Abstract
The development of molecularly targeted anticancer therapies has resulted in a paradigm shift in the clinical drug development process. Phase 1 studies now routinely incorporate pharmacodynamic biomarker endpoints, specifically to evaluate whether a targeted therapy has the desired impact on its target and whether this leads to clinical benefit. Non-invasive molecular imaging using positron emission tomography (PET) has shown promise in this setting, in particular where target modulation directly impacts on glucose metabolism or cell proliferation. In this review, we discuss the challenges in identifying PET biomarkers of target modulation by a novel targeted therapy in the preclinical setting and in their translation into the clinical setting.
Similar content being viewed by others
Introduction
Recent years have seen tremendous advances in understanding of the molecular mechanisms by which cancers develop and progress [1]. The development of drugs targeting these molecular processes is changing the face of modern oncology [2]. The majority of targeted therapies either interferes with key signal transduction pathway proteins, or interacts with cell surface receptors or antigens. The specificity of these drugs for their target generally means that their clinical use is associated with better tolerability than is shown by cytotoxic therapies still in general use.
Although promising, the development of molecularly targeted therapies in oncology has resulted in a paradigm shift in the clinical drug development process due to the significant challenges in obtaining reimbursement for targeted cancer therapeutics [3]. Rather than being drugs used in every patient with a particular cancer, molecular targeted drugs will generally have a smaller market since the relevant target may be present in only a small proportion of patients with a given form of cancer. Because of this and the enormous costs of drug development, pharmaceutical companies are seeking to make early strategic decisions regarding ongoing clinical development of targeted therapies. Therefore, in addition to the traditional safety and pharmacokinetics endpoints, phase I protocols are increasingly incorporating pharmacodynamic analyses to determine whether a drug has the desired impact on its target (proof of mechanism) and whether this leads to clinical benefit (proof of concept) [4].
While proof of mechanism has traditionally involved analysis of a putative biomarker in pre- and post-treatment biopsies, there are significant barriers in obtaining robust and adequately powered tissue biomarker results in clinical trials. These include the unwillingness of subjects to undergo repeated biopsies for research purposes, the inaccessibility of lesions, biopsy sampling errors due to tumour heterogeneity, and inadequate biopsy samples [5]. The development of imaging biomarkers has the potential to overcome many of these limitations.
Although reduction in tumour dimensions on computed tomography (CT) or magnetic resonance imaging is often used as surrogate for treatment efficacy, many targeted therapies exert their effects through inhibition of tumour cell proliferation, resulting in tumour stabilisation rather than regression. Thus, according to the response evaluation criteria in solid tumours (RECIST) [6], growth arrest indicates stable disease rather than response. In addition, even when regression does occur, it may be a late phenomenon. The use of more appropriate pharmacodynamic biomarkers of tumour response to these drugs has therefore been recognised as essential to guide the clinical evaluation of these agents.
Molecular imaging
Molecular imaging involves the use of agents or techniques that enable visualisation of physiological or biological processes in an intact organism. In contrast to tissue biomarker studies, molecular imaging is non-invasive and easily repeated, overcoming the significant issues associated with tissue collection and quality. Although a wide range of molecular imaging modalities exist, in this review we focus on the use of positron emission tomography (PET) for defining target modulation in the early evaluation of novel targeted therapies in oncology.
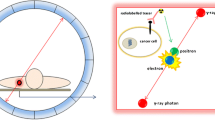
PET is a tomographic imaging modality that utilises molecules labelled with positron-emitting radioisotopes to evaluate biological phenomena in cancer. Isotopes such as 15O, 11C, 13N and 18F can be incorporated into various small molecules and drugs. The rapid decay of these agents, ranging from a couple of minutes to a couple of hours, allows sensitive imaging at early time points after administration. Larger biomolecules including peptides and antibodies may take longer to clear from the circulation and therefore require imaging to be performed at later time points. Various radiometals are suitable for labelling such agents and include 68Ga, 64Cu, and 89Zr with a half-life of decay ranging from an hour to several days.
There are many tracers with the potential to make PET the preferred imaging modality in oncology [7]. However, [18F]-fluorodeoxyglucose (FDG) is the most commonly used agent in oncological practice. Its use is based on Warburg’s fundamental observation that augmented aerobic glycolysis is a hallmark of cancer cells [8, 9]. FDG uptake reflects the combined effects of vascularity (delivery of FDG to the cell), glucose transporter expression, the activity of hexokinase as the initial rate-limiting enzyme of glycolysis, and the metabolic rate of the cell. The high sensitivity and specificity of FDG PET imaging have facilitated its widespread use for staging and monitoring of tumour response to therapy in both clinical and research settings [10–12].
Imaging cell proliferation
Tumour growth is characterised by unrestrained cell division and tumour cells therefore have higher rates of proliferation than normal cells. The PET tracer, 3′-deoxy-3′-[18F]fluoro-L-thymidine (FLT) is a thymidine analogue used to assess cell proliferation [13, 14]. It is taken up into the cell by the nucleoside salvage pathway transporters, predominantly by the family of equilibrative nucleoside transporters. Once inside the cell FLT is phosphorylated in the cytosol by thymidine kinase-1 (TK1) generating FLT monophosphate, which is not a substrate for further metabolism and so becomes trapped in the cell. As thymidine kinase expression is cell cycle regulated, increasing from late G1 and reaching maximal levels in the S-phase before being degraded during mitosis [15, 16], an FLT signal depends on cell proliferation and therefore represents an indirect PET tracer of cell proliferation. This is further supported by correlation of FLT uptake with other biomarkers of cell proliferation such as Ki-67 [17–19].
However, recent studies have also shown that modulation of FLT uptake may reflect changes in expression of the nucleoside transporters resulting from alterations in cellular use of salvage and de novo pathways for nucleotide production. Indeed, anticancer drugs that inhibit key enzymes in the de novo DNA synthesis pathway result in increased cellular FLT uptake due to the cells switching to use the salvage pathway for thymidine production [20, 21].
FLT PET imaging has shown some promise in the assessment of early response to conventional and targeted therapies [22], including docetaxel in breast cancer [23], chemoradiotherapy in head and neck cancer [24, 25], and gefitinib in lung adenocarcinoma [26]. Its use in this setting, however, remains controversial with several studies demonstrating no correlation between changes in FLT uptake and morphologic tumour response [27–29].
Challenges in identifying imaging biomarkers of target modulation in the preclinical setting
While an ideal imaging biomarker would directly demonstrate that a drug modulates its target, there are significant fiscal and regulatory impediments to the development of target-specific imaging biomarkers in oncology [7]. Therefore, in practice, imaging biomarkers rely on identification of common downstream phenotypic changes that occur as a consequence of target modulation. As most anti-tumour drugs ultimately exert their effects by impairing tumour metabolism or cell proliferation, studies to identify imaging biomarkers of response often focus on the evaluation of FDG PET and FLT PET scans. Where proof of mechanism can be demonstrated using PET, the same imaging biomarker may also be useful as a proof-of-concept biomarker, if it can be shown to predict tumour response to the drug. Preclinical studies play an important role in demonstrating that target modulation is indeed associated with changes in imaging biomarkers, and that these are, in turn, predictive of tumour response.
Continual technological advances over the past 15 years have facilitated the development of high-resolution preclinical PET systems, which provide a powerful platform for translational research [30]. Preclinical tumour models have become increasingly sophisticated in recent years. Moving beyond xenografts generated from human cell lines grown in culture, there is now a vast array of genetically engineered mouse models (GEMMs) with spontaneous tumour development recapitulating the genomic background of human cancers. Another important advance has been the development of the technique of patient-derived xenografts (PDX) in which patient tumour tissue is directly implanted into and then passaged through mice [31]. PDX models faithfully recapitulate the heterogeneity and biology of the clinical specimen from which they were obtained, thereby overcoming a significant limitation of traditional cell culture-based xenografts [32].
While FDG and FLT are the most commonly used PET tracers for evaluating novel targeted therapies, they present some limitations as regards translation between the preclinical and clinical settings that need to be considered when performing biomarker studies to identify imaging surrogates for target modulation. In contrast to patient tumours, many tumour xenografts exhibit low baseline FDG uptake. As a result, identifying a preclinical xenograft model with a signal-to-noise ratio sufficient for assessing drug-induced changes in uptake can be challenging, particularly when a specific tumour genotype is required for drug activity (e.g. expression of a mutant form of a target kinase). In contrast, tumours arising in GEMMs (e.g. Kras G12D; Pten del mouse model of ovarian cancer [33], and the TH-MYCN mouse model of neuroblastoma (Wood, Cullinane, Hicks et al., unpublished data) more faithfully reflect FDG uptake in the clinical setting with respect to the imaging phenotype.
The biodistribution of FLT differs significantly between mice and humans (Fig. 1). In humans, FLT accumulates in the highly proliferative bone marrow compartment, is metabolised through the liver, and has relatively low tumour uptake compared to FDG. Conversely, mice demonstrate significantly higher plasma levels of thymidine than do humans, have little basal bone marrow FLT uptake, and excrete FLT unchanged in the urine without significant hepatic uptake [34, 35]. FLT uptake in tumour xenografts is inversely related to the intrinsic tumour thymidine concentration, which, when coupled with the high rate of proliferation typically associated with human xenografts, results in a high proportion of human xenografts with high basal FLT uptake in mice. In contrast, tumours arising in GEMMs and syngeneic tumour models generally show low FLT uptake, presumably due to their relatively high intratumour thymidine levels.
Variable biodistribution of FDG and FLT in mouse and human FDG PET (left) and FLT PET (right) images of a mouse bearing a 2008 ovarian tumour (top) and a human ovarian cancer patient (bottom). Arrows indicate the position of the 2008 tumour. FDG uptake into preclinical tumour models is generally less robust than FLT uptake (top panels). In contrast, a pattern of high FDG and low FLT uptake is frequently observed in human tumours (lower panels). The characteristic FLT uptake into liver and bone marrow in humans is not observed in the mouse (right panels). Substantial FDG uptake into the harderian gland behind the eye is observed in mice (color figure online)
In preclinical imaging biomarker studies, the higher signal-to-noise ratio associated with FLT may lead to more striking drug-induced changes than are seen with FDG [36, 37] (Fig. 1), but may misinform translation into the clinical environment. Therefore, careful consideration of the differences between these tracers in the preclinical versus clinical settings is required when selecting a PET tracer for early clinical biomarker evaluation.
Challenges in extrapolating findings from preclinical studies to the clinical domain
Preclinical imaging biomarker studies have two key objectives. The first is to define the association between a tissue biomarker that directly measures the effect of the drug on its target and the imaging biomarker. In practice, while a cohort of tumour-bearing mice is subjected to longitudinal PET imaging, tumours are, at the same time, harvested from a parallel cohort for ex vivo biomarker analysis and testing of correlations between the different biomarkers investigated. The second aim is to explore the impact of different drug doses and schedules to define the relationship between drug exposure and the tissue and imaging biomarkers. Achievement of these key goals in preclinical studies will indicate the optimal drug dose and schedule, as well as the optimal PET tracer and imaging time for evaluation in clinical trials.
Where preclinical studies support the association between an imaging biomarker and an appropriate tissue biomarker of target modulation, further investigation of this association in early clinical development of the compound is warranted. These proof-of-mechanism biomarker studies are typically performed in an expanded cohort of patients once the maximum tolerated dose of the drug has been determined in a Phase 1 study. The patient population in which the study is performed must have tumours in which the expression of the drug target is relevant. This usually requires screening of patient tumours for expression of the appropriate target, for example a mutant kinase such as BRAFV600E in melanoma patients for evaluation of type 1 BRAF inhibitors or ALK-positive tumours for drugs such as crizotinib. In rare cases, where a tumour is driven by a single oncogene such as BCR-ABL in chronic myeloid leukaemia, selection of patients with this disease is sufficient for evaluation of inhibitors of the oncogenic protein. These studies must also be adequately powered to demonstrate a significant difference between pre- and post-treatment biomarker analyses, where one exists. Typically, these studies involve 15–30 patients [38–40]. However, the existence of a logical link between tumour biology and preclinical proof-of-concept and clinical proof-of-mechanism studies does not guarantee that these imaging biomarkers will be successfully introduced into clinical therapeutic response assessment. Below we describe examples in which the successful identification and evaluation of imaging biomarkers for proof of mechanism of novel targeted therapies in the preclinical and clinical settings have been achieved; however, these biomarkers have not yet entered daily clinical practice.
FDG PET as an imaging biomarker in oncogene-driven tumours
Imatinib
Gastrointestinal stromal tumour (GIST) is a rare tumour characterised by activation of the c-KIT oncogene [41]. In vitro studies using cell lines expressing the activating mutations in c-KIT found in GIST revealed that the small molecule KIT inhibitor, imatinib, causes a rapid reduction in cellular uptake of the glucose analogue, 2-deoxyglucose. Furthermore in vivo, imatinib therapy resulted in a rapid reduction in FDG uptake and membrane expression of GLUT-1 [42]. The direct association between imatinib and, in subsequent studies, nilotinib [43] treatment and inhibition of glucose uptake therefore supported the use of FDG PET in proof-of-mechanism studies of drugs targeting this receptor. In the clinical setting, FDG uptake into GISTs that express imatinib-sensitive mutations in c-KIT is significantly reduced within 48 h of imatinib therapy, consistent with the ability of the drug to modulate its target. Despite this powerful molecular imaging signal of drug effectiveness, CT remains the most common modality for assessing response following modification of RECIST criteria to reduce the misclassification of response in comparison to FDG PET. The so-called Choi criteria were established to reconcile the observation that some patients who demonstrated apparent progression according to RECIST had a complete metabolic response on FDG PET and had a favourable prognosis [44]. This phenomenon has since been called “pseudoprogression”. The ability of these revised CT criteria to approximate the findings on FDG PET, which was used as the validating gold standard, has been considered sufficient to allow CT to remain the preferred modality for response assessment in most clinical situations.
Vemurafenib
Activating mutations in the BRAF oncogene are known to occur in approximately 50 % of malignant melanoma cases. As B-Raf signalling promotes cell proliferation and survival through the mitogen-activated protein kinase (MAPK) pathway, several mutant B-Raf kinase inhibitors including vemurafenib and dabrafenib have been developed. In vitro studies suggest that activation of the MAPK signalling pathway by mutant BRAF impacts on several pathways regulating glucose metabolism, including the liver kinase B1–AMP-activated protein kinase (LKB1–AMPK1) energy sensor pathway and GLUT-1 expression [45, 46]. Extracellular signal-related kinase (ERK), which functions downstream of B-Raf, phosphorylates the tumour suppressor LKB1, which leads to uncoupling of the LKB1–AMPK1 complex such that LKB1 is no longer able to activate AMPK, thereby promoting cell growth, proliferation and survival in conditions of energy stress [45]. ERK also phosphorylates a number of transcription factors that regulate the expression of the glucose transporter GLUT-1 [46, 47]. Together, these findings suggest that FDG PET may be an indirect readout of B-Raf inhibitor-mediated MAPK pathway inhibition.
In the preclinical setting, treatment of BRAFV600E mutant melanoma models with vemurafenib indeed led to a rapid reduction in FDG uptake, supporting the hypothesis that FDG PET is a useful pharmacodynamic marker of BRAF inhibition [48] (Fig. 2). Further, it was shown that development of resistance is associated with restoration of FDG uptake [49].
Preclinical and clinical PET imaging of early tumour response to therapy FDG PET images of Balb/c nude mice bearing BRAFV600E mutant LOX-IMVI tumours imaged at baseline and 1 day following combination therapy with the BRAF inhibitor PLX-4720 (top panels). FDG PET images of a melanoma patient with a BRAFV600E mutant tumour responding to the BRAF inhibitor vemurafenib (bottom panels). Baseline uptake of FDG is typically higher in melanoma in patients than preclinical melanoma models but both demonstrate the concept of early metabolic response following modulation of signalling through the involved oncogenic pathway
FDG PET has also been investigated as an imaging biomarker following vemurafenib therapy in two early-phase clinical studies. Bollag et al. [50] demonstrated a major reduction in FDG uptake following 14 days of treatment with vemurafenib. McArthur et al. [40] also performed FDG PET imaging in 31 patients prior to and on day 15 of vemurafenib therapy and all showed a metabolic response according to prospectively defined criteria. As this study was performed in patients at different dose levels, the results also provide insight into the relationship between plasma levels and target inhibition.
Together, these data suggest that FDG PET is a robust clinical imaging marker of inhibition of BRAFV600E mutant melanoma (Fig. 2). Nevertheless, a metabolic response was not necessarily associated with tumour regression on subsequent CT. Thus, it appears that target modulation may be a necessary, but sometimes insufficient, condition for therapeutic response. This leaves in question whether monitoring of therapeutic response to BRAF inhibitors should be performed by early FDG PET, potentially allowing a change in treatment or dose escalation in non-responders, or should simply continue to be evaluated by morphological imaging, using CT later during treatment.
FLT PET as an imaging biomarker for target inhibition by a CDK4/6 inhibitor
FLT has been successfully evaluated as a biomarker of target inhibition and response to a number of targeted therapies, in particular compounds that directly impact on the cell cycle. Progression through the cell cycle requires co-ordinated interaction between the cyclins and their partner proteins, the cyclin dependent kinases (CDKs). Upon binding to cyclin D1, CDK4 drives G1 cell cycle progression through its phosphorylation of Rb, which leads to release of the E2F transcription factor and expression of S-phase genes [51–53]. Deregulation of the CDK4/cyclin D/Rb pathway occurs commonly in cancer through amplification of cyclin D, mutational activation of CDK4 or loss of the negative regulator, p16 [54]. CDK4 has therefore been identified as a target for therapeutic intervention in cancer. Consistent with its mechanism of action, the CDK4/6 inhibitor PD-0332991 induced arrest in the G1 phase of the cell cycle in p16-null MDA-MB-231 cells in vitro [35]. FLT PET was therefore investigated as an imaging biomarker in preclinical proof-of-mechanism studies for this agent. Target modulation by PD-0332991 following treatment of the MDA-MB-231 xenograft model was demonstrated by hypophosphorylation of Rb in tumour tissue and this correlated closely with inhibition of FLT uptake [35]. Drug-induced changes in FLT uptake were also correlated with other tissue markers of cell proliferation, including bromodeoxyuridine, Ki-67 and TK-1 expression. These results strongly support the use of FLT PET in early clinical studies to demonstrate proof of mechanism for this cell cycle-specific targeted agent.
FLT PET has been explored as an imaging biomarker in early clinical studies to evaluate PD-0332991 in the setting of mantle cell lymphoma, which exhibits the t(11;14)(q13;q32) translocation and aberrant B cell expression of cyclin D1 [39]. A substantial reduction in FLT, but not FDG, uptake was observed in tumours at an early time point during therapy in the majority of patients and this correlated well with reduction in Rb phosphorylation and Ki-67-positive cells. Together, these findings provide proof of mechanism of this drug in the clinical setting. Nevertheless, FLT PET has not yet entered clinical practice for the monitoring of any form of therapy.
Conclusion
To date, FDG and FLT have been the key PET tracers evaluated as imaging biomarkers of target modulation in the field of oncology. As discussed, there have been a number of cases in which these tracers have proven to be markers of target inhibition and to be predictive of tumour response. Nevertheless, despite its recognized limitations, morphologic imaging remains the dominant technology for therapeutic response assessment. It needs to be recognized, however, these agents are at best indirect markers of target inhibition by a drug. Although specific PET tracers that directly inform target modulation by novel targeted drugs may provide a means of demonstrating proof of mechanism and thus expedite drug development in the future, unless existing molecular imaging techniques such as FDG and FLT become accepted for clinical therapeutic response assessment of targeted agents, there will continue to be a strong disincentive for the development of such tracers.
References
Hanahan D, Weinberg RA (2011) Hallmarks of cancer: the next generation. Cell 144:646–674. doi:10.1016/j.cell.2011.02.013
Thompson CB (2009) Attacking cancer at its root. Cell 138:1051–1054. doi:10.1016/j.cell.2009.09.002
Jonsson B (2013) Technology assessment for new oncology drugs. Clin Cancer Res 19:6–11. doi:10.1158/1078-0432.CCR-12-1819
Spinella DG (2009) Biomarkers in clinical drug development: realizing the promise. Biomark Med 3:667–669. doi:10.2217/bmm.09.61
Thomas A, Rajan A, Lopez-Chavez A, Wang Y, Giaccone G (2013) From targets to targeted therapies and molecular profiling in non-small cell lung carcinoma. Ann Oncol 24:577–585. doi:10.1093/annonc/mds478
Therasse P, Eisenhauer EA, Verweij J (2006) RECIST revisited: a review of validation studies on tumour assessment. Eur J Cancer 42:1031–1039. doi:10.1016/j.ejca.2006.01.026
Hicks RJ, Hofman MS (2012) Is there still a role for SPECT-CT in oncology in the PET-CT era? Nat Rev Clin Oncol 9:712–720. doi:10.1038/nrclinonc.2012.188
Warburg O (1956) On the origin of cancer cells. Science 123:309–314
Warburg O, Wind F, Negelein E (1927) The metabolism of tumors in the body. J Gen Physiol 8:519–530
Kelloff GJ, Krohn KA, Larson SM, Weissleder R, Mankoff DA, Hoffman JM, Link JM, Guyton KZ, Eckelman WC, Scher HI, O’Shaughnessy J, Cheson BD, Sigman CC, Tatum JL, Mills GQ, Sullivan DC, Woodcock J (2005) The progress and promise of molecular imaging probes in oncologic drug development. Clin Cancer Res 11:7967–7985. doi:10.1158/1078-0432.CCR-05-1302
Poeppel TD, Krause BJ, Heusner TA, Boy C, Bockisch A, Antoch G (2009) PET/CT for the staging and follow-up of patients with malignancies. Eur J Radiol 70:382–392. doi:10.1016/j.ejrad.2009.03.051
Chen K, Chen X (2011) Positron emission tomography imaging of cancer biology: current status and future prospects. Semin Oncol 38:70–86. doi:10.1053/j.seminoncol.2010.11.005
Shields AF, Grierson JR, Dohmen BM, Machulla HJ, Stayanoff JC, Lawhorn-Crews JM, Obradovich JE, Muzik O, Mangner TJ (1998) Imaging proliferation in vivo with [F-18] FLT and positron emission tomography. Nat Med 4:1334–1336. doi:10.1038/3337
Tehrani OS, Shields AF (2013) PET imaging of proliferation with pyrimidines. J Nucl Med 54:903–912. doi:10.2967/jnumed.112.112201
Ke PY, Chang ZF (2004) Mitotic degradation of human thymidine kinase 1 is dependent on the anaphase-promoting complex/cyclosome-CDH1-mediated pathway. Mol Cell Biol 24:514–526
Li CL, Lu CY, Ke PY, Chang ZF (2004) Perturbation of ATP-induced tetramerization of human cytosolic thymidine kinase by substitution of serine-13 with aspartic acid at the mitotic phosphorylation site. Biochem Biophys Res Commun 313:587–593
Chalkidou A, Landau DB, Odell EW, Cornelius VR, O’Doherty MJ, Marsden PK (2012) Correlation between Ki-67 immunohistochemistry and 18F-fluorothymidine uptake in patients with cancer: a systematic review and meta-analysis. Eur J Cancer 48:3499–3513. doi:10.1016/j.ejca.2012.05.001
Vesselle H, Grierson J, Muzi M, Pugsley JM, Schmidt RA, Rabinowitz P, Peterson LM, Vallières E, Wood DE (2002) In vivo validation of 3′deoxy-3′-[(18)F]fluorothymidine ([(18)F]FLT) as a proliferation imaging tracer in humans: correlation of [(18)F]FLT uptake by positron emission tomography with Ki-67 immunohistochemistry and flow cytometry in human lung tumors. Clin Cancer Res 8:3315–3323
Buck AK, Schirrmeister H, Hetzel M, Von Der Heide M, Halter G, Glatting G, Mattfeldt T, Liewald F, Reske SN, Neumaier B (2002) 3-deoxy-3-[(18)F]fluorothymidine-positron emission tomography for noninvasive assessment of proliferation in pulmonary nodules. Cancer Res 62:3331–3334
Kenny LM, Contractor KB, Stebbing J, Al-Nahhas A, Palmieri C, Shousha S, Coombes RC, Aboagye EO (2009) Altered tissue 3′-deoxy-3′-[18F]fluorothymidine pharmacokinetics in human breast cancer following capecitabine treatment detected by positron emission tomography. Clin Cancer Res 15:6649–6657. doi:10.1158/1078-0432.CCR-09-1213
Perumal M, Pillai RG, Barthel H, Leyton J, Latigo JR, Forster M, Mitchell F, Jackman AL, Aboagye EO (2006) Redistribution of nucleoside transporters to the cell membrane provides a novel approach for imaging thymidylate synthase inhibition by positron emission tomography. Cancer Res 66:8558–8564. doi:66/17/8558
Weber WA (2010) Monitoring tumor response to therapy with 18F-FLT PET. J Nucl Med 51:841–844. doi:10.2967/jnumed.109.071217
Contractor KB, Kenny LM, Stebbing J, Rosso L, Ahmad R, Jacob J, Challapalli A, Turkheimer F, Al-Nahhas A, Sharma R, Coombes RC, Aboagye EO (2011) [18F]-3′Deoxy-3′-fluorothymidine positron emission tomography and breast cancer response to docetaxel. Clin Cancer Res 17:7664–7672. doi:10.1158/1078-0432.CCR-11-0783
Kishino T, Hoshikawa H, Nishiyama Y, Yamamoto Y, Mori N (2012) Usefulness of 3′-deoxy-3′-18F-fluorothymidine PET for predicting early response to chemoradiotherapy in head and neck cancer. J Nucl Med 53:1521–1527. doi:10.2967/jnumed.111.099200
Hoshikawa H, Mori T, Kishino T, Yamamoto Y, Inamoto R, Akiyama K, Mori N, Nishiyama Y (2013) Changes in (18)F-fluorothymidine and (18)F-fluorodeoxyglucose positron emission tomography imaging in patients with head and neck cancer treated with chemoradiotherapy. Ann Nucl Med 27:363–370. doi:10.1007/s12149-013-0694-8
Sohn HJ, Yang YJ, Ryu JS, Oh SJ, Im KC, Moon DH, Lee DH, Suh C, Lee JS, Kim SW (2008) [18F]Fluorothymidine positron emission tomography before and 7 days after gefitinib treatment predicts response in patients with advanced adenocarcinoma of the lung. Clin Cancer Res 14:7423–7429. doi:10.1158/1078-0432.CCR-08-0312
Soloviev D, Lewis D, Honess D, Aboagye E (2012) [(18)F]FLT: an imaging biomarker of tumour proliferation for assessment of tumour response to treatment. Eur J Cancer 48:416–424. doi:10.1016/j.ejca.2011.11.035
Pfannenberg C, Aschoff P, Dittmann H, Mayer F, Reischl G, von Weyhern C, Kanz L, Claussen CD, Bares R, Hartmann JT (2010) PET/CT with 18F-FLT: does it improve the therapeutic management of metastatic germ cell tumors? J Nucl Med 51:845–853. doi:10.2967/jnumed.109.070425
Benz MR, Czernin J, Allen-Auerbach MS, Dry SM, Sutthiruangwong P, Spick C, Radu C, Weber WA, Tap WD, Eilber FC (2012) 3′-deoxy-3′-[18F]fluorothymidine positron emission tomography for response assessment in soft tissue sarcoma: a pilot study to correlate imaging findings with tissue thymidine kinase 1 and Ki-67 activity and histopathologic response. Cancer 118:3135–3144. doi:10.1002/cncr.26630
Aide N, Visser EP, Lheureux S, Heutte N, Szanda I, Hicks RJ (2012) The motivations and methodology for high-throughput PET imaging of small animals in cancer research. Eur J Nucl Med Mol Imaging 39:1497–1509. doi:10.1007/s00259-012-2177-x
Quintana E, Shackleton M, Sabel MS, Fullen DR, Johnson TM, Morrison SJ (2008) Efficient tumour formation by single human melanoma cells. Nature 456:593–598. doi:10.1038/nature07567
Julien S, Merino-Trigo A, Lacroix L, Pocard M, Goere D, Mariani P et al (2012) Characterization of a large panel of patient-derived tumor xenografts representing the clinical heterogeneity of human colorectal cancer. Clin Cancer Res 18:5314–5328. doi:10.1158/1078-0432.CCR-12-0372
Kinross KM, Brown DV, Kleinschmidt M, Jackson S, Christensen J, Cullinane C, Hicks RJ, Johnstone RW, McArthur GA (2011) In vivo activity of combined PI3 K/mTOR and MEK inhibition in a Kras(G12D);Pten deletion mouse model of ovarian cancer. Mol Cancer Ther 10:1440–1449. doi:10.1158/1535-7163.MCT-11-0240
Shields AF (2012) PET imaging of tumor growth: not as easy as it looks. Clin Cancer Res 18:1189–1191. doi:10.1158/1078-0432.CCR-11-3198
Zhang CC, Yan Z, Li W, Kuszpit K, Painter CL, Zhang Q, Lappin PB, Nichols T, Lira ME, Affolter T, Fahey NR, Cullinane C, Spilker M, Zasadny K, O’Brien P, Buckman D, Wong A, Christensen JG (2012) [(18)F]FLT-PET imaging does not always “light up” proliferating tumor cells. Clin Cancer Res 18:1303–1312. doi:10.1158/1078-0432.CCR-11-1433
Cullinane C, Dorow DS, Jackson S, Solomon B, Bogatyreva E, Binns D, Young R, Arango ME, Christensen JG, McArthur GA, Hicks RJ (2011) Differential (18)F-FDG and 3′-deoxy-3′-(18)F-fluorothymidine PET responses to pharmacologic inhibition of the c-MET receptor in preclinical tumor models. J Nucl Med 52:1261–1267. doi:10.2967/jnumed.110.086967
McKinley ET, Smith RA, Zhao P, Fu A, Saleh SA, Uddin MI, Washington MK, Coffey RJ, Manning HC (2013) 3′-Deoxy-3′-18F-fluorothymidine PET predicts response to (V600E)BRAF-targeted therapy in preclinical models of colorectal cancer. J Nucl Med 54:424–430. doi:10.2967/jnumed.112.108456
Infante JR, Camidge DR, Mileshkin LR, Chen EX, Hicks RJ, Rischin D, Fingert H, Pierce KJ, Xu H, Roberts WG, Shreeve SM, Burris HA, Siu LL (2012) Safety, pharmacokinetic, and pharmacodynamic phase I dose-escalation trial of PF-00562271, an inhibitor of focal adhesion kinase, in advanced solid tumors. J Clin Oncol 30:1527–1533. doi:10.1200/JCO.2011.38.9346
Leonard JP, LaCasce AS, Smith MR, Noy A, Chirieac LR, Rodig SJ et al (2012) Selective CDK4/6 inhibition with tumor responses by PD0332991 in patients with mantle cell lymphoma. Blood 119:4597–4607. doi:10.1182/blood-2011-10-388298
McArthur GA, Puzanov I, Amaravadi R, Ribas A, Chapman P, Kim KB, Sosman JA, Lee RJ, Nolop K, Flaherty KT, Callahan J, Hicks RJ (2012) Marked, homogeneous, and early [18F]fluorodeoxyglucose-positron emission tomography responses to vemurafenib in BRAF-mutant advanced melanoma. J Clin Oncol 30:1628–1634. doi:10.1200/JCO.2011.39.1938
Corless CL, Fletcher JA, Heinrich MC (2004) Biology of gastrointestinal stromal tumors. J Clin Oncol 22:3813–3825. doi:10.1200/JCO.2004.05.14022/18/3813
Cullinane C, Dorow DS, Kansara M, Conus N, Binns D, Hicks RJ, Ashman LK, McArthur GA, Thomas DM (2005) An in vivo tumor model exploiting metabolic response as a biomarker for targeted drug development. Cancer Res 65:9633–9636. doi:65/21/9633
Cullinane C, Natoli A, Hui Y, Conus N, Jackson S, Brüggen J, Manley PW, McArthur GA (2010) Preclinical evaluation of nilotinib efficacy in an imatinib-resistant KIT-driven tumor model. Mol Cancer Ther 9:1461–1468. doi:10.1158/1535-7163.MCT-09-1181
Choi H, Charnsangavej C, Faria SC, Macapinlac HA, Burgess MA, Patel SR, Chen LL, Podoloff DA, Benjamin RS (2007) Correlation of computed tomography and positron emission tomography in patients with metastatic gastrointestinal stromal tumor treated at a single institution with imatinib mesylate: proposal of new computed tomography response criteria. J Clin Oncol 25:1753–1759. doi:10.1200/JCO.2006.07.3049
Zheng B, Jeong JH, Asara JM, Yuan YY, Granter SR, Chin L, Cantley LC (2009) Oncogenic B-RAF negatively regulates the tumor suppressor LKB1 to promote melanoma cell proliferation. Mol Cell 33:237–247. doi:10.1016/j.molcel.2008.12.026
Kao YS, Fong JC (2011) A novel cross-talk between endothelin-1 and cyclic AMP signaling pathways in the regulation of GLUT1 transcription in 3T3-L1 adipocytes. Cell Signal 23:901–910. doi:10.1016/j.cellsig.2011.01.016
Osthus RC, Shim H, Kim S, Li Q, Reddy R, Mukherjee M, Xu Y, Wonsey D, Lee LA, Dang CV (2000) Deregulation of glucose transporter 1 and glycolytic gene expression by c-Myc. J Biol Chem 275:21797–21800. doi:10.1074/jbc.C000023200
Søndergaard JN, Nazarian R, Wang Q, Guo D, Hsueh T, Mok S et al (2010) Differential sensitivity of melanoma cell lines with BRAFV600E mutation to the specific Raf inhibitor PLX4032. J Transl Med 8:39. doi:10.1186/1479-5876-8-39
Baudy AR, Dogan T, Flores-Mercado JE, Hoeflich KP, Su F, van Bruggen N, Williams SP (2012) FDG-PET is a good biomarker of both early response and acquired resistance in BRAFV600 mutant melanomas treated with vemurafenib and the MEK inhibitor GDC-0973. EJNMMI Res 2:22. doi:10.1186/2191-219X-2-22
Bollag G, Hirth P, Tsai J, Zhang J, Ibrahim PN, Cho H et al (2010) Clinical efficacy of a RAF inhibitor needs broad target blockade in BRAF-mutant melanoma. Nature 467:596–599. doi:10.1038/nature09454
Harbour JW, Luo RX, Dei Santi A, Postigo AA, Dean DC (1999) Cdk phosphorylation triggers sequential intramolecular interactions that progressively block Rb functions as cells move through G1. Cell 98:859–869
Sherr CJ (1995) D-type cyclins. Trends Biochem Sci 20:187–190
Lundberg AS, Weinberg RA (1998) Functional inactivation of the retinoblastoma protein requires sequential modification by at least two distinct cyclin-cdk complexes. Mol Cell Biol 18:753–761
Malumbres M, Barbacid M (2001) To cycle or not to cycle: a critical decision in cancer. Nat Rev Cancer 1:222–231. doi:10.1038/35106065
Conflict of interest
Carleen Cullinane, Benjamin Solomon and Rodney Hicks have nothing to disclose.
Ethical approval
Compliance with Ethics Guidelines.
Human and Animal studies
All studies involving animal or human subjects were performed with approval from the appropriate Peter MacCallum Cancer Centre ethics committee and therefore have been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Author information
Authors and Affiliations
Corresponding author
Additional information
Color figures online at http://link.springer.com/article/10.1007/s40336-013-0047-6
Rights and permissions
About this article
Cite this article
Cullinane, C., Solomon, B. & Hicks, R.J. Imaging of molecular target modulation in oncology: challenges of early clinical trials. Clin Transl Imaging 2, 5–12 (2014). https://doi.org/10.1007/s40336-013-0047-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40336-013-0047-6