Abstract
Introduction
Idiopathic pulmonary fibrosis (IPF) is a progressive, debilitating interstitial lung disease. Two antifibrotics, pirfenidone and nintedanib, are available for IPF treatment. Pirfenidone is available as 267 mg capsules and, more recently, as 267 mg and 801 mg tablets. The aim of this study was to examine the perceived benefits of the 801 mg formulation on patient quality of life (QoL), IPF management and pill burden.
Methods
Forty-seven patients with IPF and 170 healthcare professionals (HCPs; 150 physicians in France, Germany, Spain and the USA and 20 nurses in the USA) completed online questionnaires comprising 67 and 61 questions, respectively. Eligible patients had experience switching from the 267 mg pirfenidone tablet or capsule formulations to the 801 mg tablet formulation, and eligible HCPs were experienced in managing this switch. Questions included single and multiple responses and scalar questions with responses on a 7-point Likert scale.
Results
Patients received the 267 mg formulation for a median (range) of 6.0 (2.0–40.0) months prior to switching to the 801 mg formulation. Higher percentages of patients reported satisfaction with the 801 mg versus the 267 mg formulation for its convenience (64 vs. 17%) and number of dosage units (70 vs. 2%). More patients reported good emotional well-being on the 801 mg versus the 267 mg formulation (51 vs. 21%), and fewer patients reported missing a dose of pirfenidone (21 vs. 30%). More HCPs perceived high patient adherence with the 801 mg versus the 267 mg formulation (57 vs. 37%). Overall, 33% of physicians had experienced switching patients back to the 267 mg formulation.
Conclusion
Patients and HCPs consistently favoured the 801 mg formulation across multiple domains, including convenience, patient QoL and adherence. The 801 mg formulation may provide an alternative to the 267 mg formulation in patients established on the recommended daily dose of pirfenidone.
Similar content being viewed by others
Why carry out this study? |
Pirfenidone is an antifibrotic approved for the treatment of idiopathic pulmonary fibrosis (IPF), a progressive, debilitating interstitial lung disease with poor prognosis and limited treatment options. |
Pirfenidone was initially available as a 267 mg capsule, administered as three capsules three times a day to achieve the recommended maintenance dose. The more recently available 801 mg tablet formulation allows patients to take fewer dosage units per day. |
This survey was conducted to examine the perceived benefits of the 801 mg pirfenidone tablet formulation versus the 267 mg formulation to patients with IPF and healthcare professionals involved in the care of patients with IPF. |
What was learned from the study? |
Patients and healthcare professionals perceived benefits of the 801 mg tablet formulation versus the 267 mg formulation across multiple domains, including patient quality of life, pill burden, adherence to therapy and practical management of patients with IPF. |
The 801 mg pirfenidone tablet formulation may provide a convenient and valuable treatment option to patients established on the recommended daily maintenance dose of pirfenidone, particularly in patients who are concerned about pill burden. |
Introduction
Idiopathic pulmonary fibrosis (IPF) is the most common type of idiopathic interstitial lung disease (ILD) and is associated with progressive scarring of the lung interstitium and irreversible loss of lung function [1]. The clinical course of IPF is chronic, progressive and invariably fatal. Without treatment, the 5-year survival rate ranges from 20 to 30% [1, 2]. The combination of a poor prognosis and a severe symptom burden results in impaired quality of life (QoL), with patients facing both the physical limitations and the psychological impact of the disease [3]. Therefore, it has been suggested that optimisation of health-related QoL should be integrated with, and complementary to, treatments targeting lung function and survival [4, 5].
Currently, two antifibrotics, pirfenidone and nintedanib, are approved for the treatment of IPF [6,7,8,9]. Both drugs have been shown to significantly reduce lung function decline versus placebo over 52 weeks in patients with IPF [10, 11]. First-line treatment choice should be determined based on factors that include patient preference, medical history, concomitant medications and lifestyle [12]. Pirfenidone is available as 267 mg capsules and, more recently, as 267 mg and 801 mg tablets [7, 13]. The 801 mg formulation can be administered as one tablet three times daily, offering patients who are established on the recommended maintenance dose of 2403 mg/day the opportunity to reduce their pill burden compared with the 267 mg formulation [7]. Initial evidence from a qualitative study of 49 patients with IPF suggested that the 801 mg pirfenidone tablet was well tolerated and acceptable to patients [14].
Here, we present the results of a questionnaire-based study of patients with IPF and healthcare professionals (HCPs) that aimed to examine the perceived benefits of the 801 mg pirfenidone tablet formulation compared with the 267 mg formulation in terms of patient QoL, pill burden, adherence to therapy and practical management of IPF.
Methods
Study Design and Participants
Between February and April 2018, patients with IPF and HCPs involved in the care of patients with IPF (physicians and nurses) were asked to fill in an online questionnaire that took approximately 25 min to complete. There were different versions of the questionnaire for patients and HCPs, comprising 67 and 61 questions, respectively (Electronic Supplementary Material [ESM] S1). Participants were recruited from France, Germany, Spain and the USA. Each questionnaire was available in French, German, Spanish and English, with all responses pre-coded as numbers, so translation was not required. The questionnaires were quantitative and designed to collect information regarding the treatment of IPF with the 267 mg and 801 mg formulations of pirfenidone. The online questionnaires were developed by ELMA Research (London, UK), an independent market research agency, on behalf of F. Hoffmann-La Roche, Ltd. (Basel, Switzerland). The participants were made aware that this study was sponsored by a pharmaceutical company. Patients and HCPs were not paired in order to avoid selection bias.
Patients with experience of switching from pirfenidone 267 mg capsules or tablets (hereafter referred to as the 267 mg formulation) to the 801 mg tablet formulation were recruited by referral letters distributed by their physician (ESM S1). After receiving the referral letter, patients contacted local study recruiters by email if they wished to participate. The physicians making patient referrals were contacted through a letter that explained the objectives of the study (ESM S1) and were not necessarily taking part in the survey themselves. Patients could be included in the study if they were aged > 18 and < 90 years, had received a confirmed IPF diagnosis from a qualified medical doctor and were undergoing treatment with pirfenidone.
Responses were collected from physicians and nurses experienced in managing patients switching from the pirfenidone 267 mg formulation to the 801 mg tablet formulation. Physicians and nurses were recruited from market research panels and selected to cover a variety of regional geographical areas within the respective countries.
All participants provided voluntary, written informed consent to data collection and use (including publication), based upon a clear understanding of the purpose of the data collection. The questionnaire was performed, and ethical issues were addressed, following the Code of Conduct of the European Pharmaceutical Market Research Association (EphMRA) [15]. As indicated by Article 3.4 of the EphMRA Code of Conduct, this market research study did not require Clinical Research Ethics Committee or Independent Review Board approval. No patient-identifiable data were collected, and all patients remained anonymous throughout the study. All patients and HCPs received a small cash incentive for participation in the research.
Questionnaires
A copy of each questionnaire (patient and HCP) is provided in ESM S1. Questions included a mixture of single and multiple responses, as well as scalar questions which required respondents to select a score on a 7-point Likert scale. The patient questionnaire collected data on: sociodemographic characteristics; IPF severity and symptoms; impact of the disease on QoL; treatment history; experience of the 267 mg pirfenidone formulation; experience of the switch from the 267 mg formulation to the 801 mg tablet formulation; and experience of the 801 mg tablet regimen. The questionnaires designed for the physicians and nurses collected data on: medical speciality; expertise in managing patients with IPF; patient caseload; experience in managing patients receiving the pirfenidone 267 mg formulation; experience in managing the switch from the 267 mg formulation to the 801 mg tablet formulation; and experience with long-term use of the 801 mg tablet regimen.
Data Analysis
All data are presented descriptively as mean (standard deviation [SD]), median (range) or percentage of valid cases. All percentages presented for responses scored on the 7-point Likert scales refer to the pooled total of scores of 6 and 7. No statistical comparisons were performed due to the observational study design.
Results
Patient Demographics
A total of 47 patients with IPF completed the questionnaire (France, n = 7; Germany, n = 10; Spain, n = 10; USA, n = 20); of these, 94% of patients had received a diagnosis of IPF ≥ 12 months ago, with a median (range) time since diagnosis of 33.0 (6.0–105.0) months (Table 1). The most frequently reported symptoms of IPF were persistent dry cough (77%), fatigue (77%) and shortness of breath (72%). All (100%) patients confirmed that they were currently receiving pirfenidone. The median (range) duration of treatment with the 267 mg formulation prior to switching to the 801 mg tablet formulation was 6.0 (2.0−40.0) months. The median (range) duration of treatment with the 801 mg tablet formulation prior to participation in the questionnaire was 5.0 (1.0−25.0) months. Approximately one-third (34%) of patients were receiving oxygen therapy. Other concomitant therapies included low-dose glucocorticoids and N-acetylcysteine (Table 1).
Physician Demographics
A total of 150 physicians completed the questionnaire (France, n = 35; Germany, n = 35; Spain, n = 30; USA, n = 50; Table 2). Over 90% of physicians in France (100%), Germany (94%) and Spain (93%) reported specialising in respiratory medicine compared with 74% in the USA. The remainder of physicians reported working in internal medicine with an interest in lung disease (France 0%; Germany 6%; Spain 7%; USA 26%). Nearly all respondents were involved in the diagnosis (97%), treatment initiation of any pharmacological therapy (97%) and ongoing treatment management (100%) in patients with IPF. The median (range) patient caseload was 50.0 (11.0–450.0) patients (Table 2). The median (range) experience of participating physicians in prescribing and managing antifibrotics was 50.0 (3.0–131.0) months (Table 2).
Nurse Demographics
A total of 20 respiratory nurses completed the questionnaire (Table 3), all of whom were based in the USA due to lack of willing respondents in the other participating countries (Table 3). Approximately half (45%) of respondents were involved in the diagnosis of patients with IPF. Nearly all respondents were involved in treatment initiation of any pharmacological therapy (90%) and ongoing treatment management (100%) of patients with IPF. The median (range) patient caseload was 55.0 (15.0–300.0) patients (Table 3). The median (range) experience reported by participating nurses of managing patients treated with antifibrotics was 74.5 (25.0–124.0) months (Table 3). Of the respiratory nurses who responded, 75% reported that they routinely joined the first conversation held between patients and physicians regarding the pirfenidone 801 mg tablet formulation.
Patient Experiences with the 801 mg Pirfenidone Tablet Formulation
A higher percentage of patients were satisfied with the convenience of the 801 mg tablet formulation (64 vs. 17%) and with its ease of storage, transportation and convenience of dosing with other concomitant therapies versus the 267 mg formulation (Fig. 1a). In addition, more patients were satisfied with the 801 mg versus the 267 mg formulation in terms of number of dosage units (70 vs. 2%), dosing frequency (51 vs. 11%) and ease of swallowing (64 vs. 26%; Fig. 1b).
Percentage of patients reporting satisfactiona with the 267 mg capsule and tablet and 801 mg tablet pirfenidone formulations across multiple domains: a convenience and lifestyle, b dosing and administration. aPercentage of patients who selected 6 or 7 on a 7-point Likert scale ranging from 0 (extremely dissatisfied) to 7 (extremely satisfied); bpercentage of patients who selected 6 or 7 on a 7-point Likert scale ranging from 0 (extremely inconvenient) to 7 (extremely convenient)
Fewer patients reported missing a dose of pirfenidone with the 801 mg tablet formulation versus the 267 mg formulation (21 vs. 30%). Furthermore, fewer patients treated with the 801 mg formulation considered the pirfenidone treatment to be a practical burden versus those treated with the 267 mg formulation (4 vs. 17%, on a scale from “not a burden at all” to “a significant burden”). A greater percentage of patients treated with the 801 mg formulation were comfortable with the notion of long-term pirfenidone treatment versus those treated with the 267 mg formulation (62 vs. 15%, on a scale from “extremely uncomfortable” to “extremely comfortable”).
With regard to QoL, following the switch to the 801 mg tablet formulation 28% of patients agreed that they felt less stigmatised (i.e. unfairly regarded as a result of their IPF) and 26% felt more in control of their IPF symptoms (both on a scale from “completely disagree” to “completely agree”). A greater percentage of patients reported enjoyment of life (53 vs. 34%, on a scale from “I was not able to enjoy life at all” to “I was able to enjoy life to the fullest”) and good emotional well-being (51 vs. 21%, on a scale from “not good at all” to “very good”) while receiving the 801 mg formulation versus the 267 mg formulation.
Physician and Nurse Experiences with the 801 mg Pirfenidone Tablet Formulation
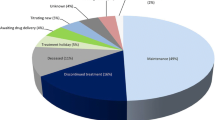
A greater percentage of physicians perceived the 801 mg tablet formulation to be more convenient than the 267 mg formulation, both for themselves (45 vs. 37%) and for their patients (40 vs. 26%; Fig. 2a). More physicians perceived that patient treatment adherence was high with the 801 mg formulation versus the 267 mg formulation (53 vs. 33%; Fig. 2b). Moreover, a higher percentage of nurses were satisfied with the convenience of the 801 mg formulation in terms of fit with patient daily routine (80 vs. 50%) and with pill burden versus the 267 mg formulation (65 vs. 40%, both on a scale from “extremely dissatisfied” to “extremely satisfied”).
Percentage of physicians reporting satisfactiona with the 267 mg capsule and tablet and 801 mg tablet pirfenidone formulations across multiple domains: a convenience and lifestyle, b dosing and administration. aPercentage of physicians who selected 6 or 7 on a 7-point Likert scale ranging from 0 (extremely dissatisfied) to 7 (extremely satisfied); bpercentage of physicians who selected 6 or 7 on a 7-point Likert scale ranging from 0 (extremely inconvenient) to 7 (extremely convenient); cpercentage of physicians who selected 6 or 7 on a 7-point Likert scale ranging from 0 (extremely low) to 7 (extremely high)
On a scale from “not easy at all” to “extremely easy”, 58% of physicians reported that the experience of switching from the 267 mg pirfenidone formulation to the 801 mg formulation was easy. Patients were maintained on the 267 mg formulation for a median (range) time of 7.2 (2.9–14.1) months prior to switching to the 801 mg formulation. The percentage of physicians who had ever reverted patients back to the 267 mg formulation was 33%, of whom 72% cited tolerability as the main reason. No data were collected on how easy HCPs perceived it to be to reduce the dose temporarily once patients were on the 801 mg formulation.
A higher percentage of HCPs (physicians and nurses) were satisfied with their experience of managing patients with the 801 mg versus the 267 mg formulation (58 vs. 44%, on a scale from “extremely dissatisfied” to “extremely satisfied”). However, the percentage of HCPs perceiving treatment as a practical burden for their patients was similar for the 801 mg and 267 mg formulations (31 and 29%, respectively, on a scale from “not a burden at all” to “a significant burden”). Furthermore, a higher percentage of HCPs (physicians and nurses) were satisfied with the 267 mg formulation versus the 801 mg formulation in terms of the perceived ease of swallowing for their patients (35 vs. 25%, on a scale from “extremely dissatisfied” to “extremely satisfied”).
Most HCPs (physicians and nurses) perceived that the pirfenidone 801 mg tablet formulation was able to meet the needs of their patients in terms of independence and treatment adherence (Fig. 3).
Physician and nurse perspectives of the impact of the 267 mg capsule and tablet and 801 mg tablet pirfenidone formulations on clinical practice and patient quality of life. Healthcare professionals (HCPs; physicians and nurses) were asked to “indicate how well the following statements describe your experience treating/managing IPF” on a 7-point Likert scale ranging from 0 (not well at all) to 7 (very well). HCPs provided a separate answer for the pirfenidone 267 mg formulation and the pirfenidone 801 mg formulation. Data are expressed as percentage of physicians and nurses who responded with a 6 or 7 on the Likert scale. IPF Idiopathic pulmonary fibrosis
Discussion
Our results show that the 801 mg tablet formulation of pirfenidone offers a number of perceived benefits to patients with IPF compared with the 267 mg capsule or tablet formulation. Patients and HCPs consistently favoured the 801 mg formulation across multiple domains, including perceptions of patient QoL, pill burden, adherence to therapy and practical management of patients with IPF.
The 801 mg pirfenidone tablet formulation was developed to provide an alternative to the 267 mg capsule for patients with IPF who are established on the recommended daily maintenance dose of 2403 mg/day. The two formulations have been shown to be bioequivalent [13], but it is possible that the reduced pill burden associated with the 801 mg formulation may have benefits in terms of adherence and QoL in patients with IPF. Real-world evidence has shown that patients with IPF have a high burden of comorbidities and concomitant medications [16,17,18]; therefore, a simplified pirfenidone dosing regimen may help reduce this burden. An increased number of prescribed daily dose units of medication has been shown to be associated with poorer adherence in patients with a range of conditions [19,20,21], and poor adherence to medications has been found to result in reduced QoL and poorer treatment outcomes [19]. The aim of our quantitative questionnaire-based study was to collect patient and HCP perspectives on the perceived benefits of the 801 mg pirfenidone tablet formulation versus the 267 mg formulations across various domains, including QoL and treatment adherence.
Results from the questionnaires indicate that the respondents, both patients and HCPs, perceived the 801 mg tablet formulation of pirfenidone to be more convenient than the 267 mg formulation for many reasons, including ease of storage and transportation, convenience of dosing with concomitant therapies, number of dosage units, dosing frequency and ease of swallowing. Similarly, a higher percentage of respiratory nurses were satisfied with the 801 mg formulation in terms of integration into the daily patient routine and pill burden compared with the 267 mg formulation. These findings are consistent with results from a recent qualitative telephone survey conducted in 49 patients with IPF who were undergoing the switch from the 267 mg capsule to the 801 mg tablet formulation of pirfenidone [14], where patients reported a positive experience with the latter as a result of the reduced number of dosage units. Taken together, these findings suggest that the 801 mg tablet formulation of pirfenidone may offer a promising alternative to patients who are established on pirfenidone therapy and concerned about pill burden.
As highlighted above, pill burden is related to treatment adherence [19,20,21]. Therefore, our finding that fewer patients reported missing a dose of pirfenidone with the 801 mg formulation compared with the 267 mg formulation was expected. This result was also reflected in the HCP responses, with a greater percentage of HCPs perceiving good treatment adherence with the 801 mg formulation versus the 267 mg formulation. Interestingly, the improvement in perceived adherence with the 801 mg formulation was greater among HCPs than among patients (20 vs. 9% improvement, respectively). Although patients and physicians were not paired and it is possible that these differences in adherence occurred by chance, it is also possible that this discrepancy is related to the nature of questionnaire-based research. Adherence was not objectively measured in our survey, and we relied upon subjective reports from patients and HCPs. Consequently, it is possible that patients felt more comfortable admitting that they had missed doses of their medication in the anonymous setting of the questionnaire and that if we had surveyed patients during face-to-face consultations, we might have found improved adherence similar to that perceived by the physicians we surveyed. Whether the adherence can be improved with the 801 mg pirfenidone tablet formulation should be explored further in studies whose designs are more objective.
In addition to observing different perceptions of adherence, we also observed different perceptions between HCPs and patients regarding the practical burden of the pirfenidone formulations and the ease of swallowing. Whereas more patients perceived the 267 mg pirfenidone formulation to be a practical burden compared with the 801 mg formulation (17 vs. 4%, respectively), HCPs did not appear to perceive any difference between the two formulations in this regard (29 vs. 31%, respectively). In addition, more patients were satisfied with the ease of swallowing the 801 mg formulation compared with the 267 mg formulation (64 vs. 26%, respectively), whereas more HCPs were satisfied with the ease of swallowing the 267 mg formulation compared with the 801 mg formulation (35 vs. 25%, respectively). Therefore, our results indicate that patients already on therapy may feel less burdened by their IPF treatment than their physicians perceive them to be. This finding suggests that further research may be required to explore both the benefits and the burden perceived by patients treated with the 801 mg formulation in clinical practice. Patient beliefs have been shown to influence treatment adherence in other therapy areas [22], and a greater awareness among HCPs for the beliefs and perceptions of patients regarding their treatment could ultimately aid the optimisation of patient care and maximisation of uptake of both new and pre-existing therapeutic options made available to patients.
The findings of our survey also provide insight on the relative contributions of physicians and nurses to the management of patients with IPF. In particular, our results have highlighted the geographical disparities in the role of the respiratory nurse. All of the nurse respondents in this study were based in the USA, where the role of the ILD specialist nurse is well established and involves providing patient education, helping patients to manage their symptoms and delivery of support groups [23, 24]. We were unable to recruit nurses involved in the care of patients with IPF from other countries due to a lack of possible respondents selected by market research panels. This is an interesting finding in itself, highlighting that although the European IPF Patient Charter recommends that ILD specialist nurses should be included in multidisciplinary teams responsible for the care of patients with IPF [5], this is not yet the reality in several countries. This could be due to low overall numbers of ILD nurses, restriction of ILD nurses to specialised centres and funding limitations. As highlighted by a qualitative survey of patients [25], both physicians and nurses play a meaningful role in the care of patients with IPF, and further efforts must be made to integrate ILD specialist nurses into the clinical team. These efforts are already becoming apparent, with some countries, such as Spain, introducing specific ILD training programmes aimed at nurses. Although these initiatives are in their early stages, it is hoped that these targeted opportunities will demonstrate benefits to patients with IPF in the near future.
As with all surveys, our study had some inherent limitations. For example, selection bias must be considered—to be switched to the 801 mg pirfenidone formulation, patients had to be established on the recommended daily maintenance dose of pirfenidone. Furthermore, patients were established on the 801 mg formulation for a minimum duration of 1 month prior to participating in the questionnaire. Therefore, patients who initiated the 801 mg formulation and subsequently discontinued it within a short timeframe would not have been included in this questionnaire and so the benefits of the 801 mg formulation observed in this study might not be representative of the wider IPF population. A further source of selection bias stems from the fact that the responding HCPs were those interested in participating in the study, and nurses were only recruited from the USA. As a result, the survey population sampled here may not be representative of all HCPs managing patients with IPF around the world. Therefore, the results may not entirely reflect clinical management seen in routine practice, and larger-scale global studies would be required to confirm the results. A further limitation is that this study only evaluated the opinions and perceptions of patients and HCPs and did not formally evaluate the expected improvement in QoL following a switch from the 267 mg to the 801 mg pirfenidone formulation. Given its observational nature, our survey does not take into account every variable that could affect perceptions and IPF management. In addition, the physician surveys did not collect the length of time patients had received the 267 mg formulation before switching to the 801 mg formulation and, therefore, it was not possible to assess whether the duration of time initially on the 267 mg formulation had any impact on the likelihood of switching back to the 267 mg formulation. Related to this, perceptions were not collected regarding the ease of temporary dose reductions on either dose. It should also be noted that the questionnaires were designed to cover specific aspects of interest, which limits comparability with studies using standardised questionnaires. Furthermore, participants were not provided with definitions for terminology used in the survey, including “stigmatised” and “involvement in diagnosis”, which could have introduced some bias in terms of individual interpretation of the questions. Additionally, some of the questions concerned past events and, therefore, recall bias may have been introduced if respondents were relying on memory when providing an answer. Importantly, the study did not survey patients treated with nintedanib, which is delivered as one 150 mg capsule twice a day, and it is possible that the twice-daily dosing of nintedanib would have provided further benefits over the 801 mg pirfenidone formulation. However, the insights obtained from this study, in combination with further research, may aid a better understanding of the complex needs of patients with IPF and the impact of appropriate disease management on their QoL.
Conclusions
Our survey gathered information on the perceived impact of the 801 mg tablet formulation of pirfenidone on IPF management from patients with IPF, physicians and nurses. Patients and HCPs perceived benefits of the 801 mg tablet formulation across multiple domains, including perceptions of patient QoL, pill burden, adherence to therapy and practical management of patients with IPF. To conclude, our results suggest that the 801 mg tablet formulation may provide a convenient and valuable treatment option in patients established on the recommended daily maintenance dose of pirfenidone, in particular by providing a possible resolution for individuals who are concerned about pill burden.
References
Kreuter M. Pirfenidone: an update on clinical trial data and insights from everyday practice. Eur Respir Rev. 2014;23:111–7.
Ley B, Collard HR, King TE Jr. Clinical course and prediction of survival in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2011;183:431–40.
Duck A, Spencer LG, Bailey S, Leonard C, Ormes J, Caress AL. Perceptions, experiences and needs of patients with idiopathic pulmonary fibrosis. J Adv Nurs. 2015;71:1055–65.
van Manen MJ, Geelhoed JJ, Tak NC, Wijsenbeek MS. Optimizing quality of life in patients with idiopathic pulmonary fibrosis. Ther Adv Respir Dis. 2017;11:157–69.
Bonella F, Wijsenbeek M, Molina-Molina M, et al. European IPF patient charter: unmet needs and a call to action for healthcare policymakers. Eur Respir J. 2016;47:597–606.
European Medicines Agency. Summary of Product Characteristics—Ofev (nintedanib). 2018. http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/medicines/003821/human_med_001834.jsp&mid=WC0b01ac058001d124. Accessed 30 Aug 2019.
European Medicines Agency. Summary of Product Characteristics—Esbriet (pirfenidone). 2018. http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/medicines/002154/human_med_001417.jsp&mid=WC0b01ac058001d124. Accessed 30 Aug 2019.
U.S. Food and Drug Administration. Summary review of regulatory action—Esbriet®. 2014. http://www.accessdata.fda.gov/drugsatfda_docs/nda/2014/022535Orig1s000SumR.pdf. Accessed 30 Aug 2019.
Food and Drug Administration. Summary review of regulatory action—Ofev®. 2014. http://www.accessdata.fda.gov/drugsatfda_docs/nda/2014/205832Orig1s000SumR.pdf. Accessed 30 Aug 2019.
Noble PW, Albera C, Bradford WZ, et al. Pirfenidone for idiopathic pulmonary fibrosis: analysis of pooled data from three multinational phase 3 trials. Eur Respir J. 2016;47:243–53.
Richeldi L, du Bois RM, Raghu G, et al. Efficacy and safety of nintedanib in idiopathic pulmonary fibrosis. N Engl J Med. 2014;370:2071–82.
Kreuter M, Bonella F, Wijsenbeek M, Maher TM, Spagnolo P. Pharmacological treatment of idiopathic pulmonary fibrosis: current approaches, unsolved issues, and future perspectives. Biomed Res Int. 2015;2015:329481.
Pan L, Belloni P, Ding HT, Wang J, Rubino CM, Putnam WS. A pharmacokinetic bioequivalence study comparing pirfenidone tablet and capsule dosage forms in healthy adult volunteers. Adv Ther. 2017;34:2071–82.
Morris H, Marshall T, Zakis K, et al. Introducing a new formulation of pirfenidone to reduce tablet burden for the IPF patient: Is it tolerable? Is it easy to take? What do our patients think? Eur Respir J. 2018;62(Suppl 62):PA4782. https://doi.org/10.1183/13993003.congress-2018.PA4782
European Pharmaceutical Market Research Association (EphMRA). Code of Conduct. 2017. https://www.ephmra.org/media/1785/ephmra-2017-code-of-conduct-october-2017.pdf. Accessed 30 Aug 2019.
Wuyts WA, Dahlqvist C, Slabbynck H, et al. Baseline clinical characteristics, comorbidities and prescribed medication in a real-world population of patients with idiopathic pulmonary fibrosis: the PROOF registry. BMJ Open Respir Res. 2018;5:e000331.
Jo HE, Glaspole I, Grainge C, et al. Baseline characteristics of idiopathic pulmonary fibrosis: analysis from the Australian Idiopathic Pulmonary Fibrosis Registry. Eur Respir J. 2017;49:1601592.
Behr J, Kreuter M, Hoeper MM, et al. Management of patients with idiopathic pulmonary fibrosis in clinical practice: the INSIGHTS-IPF registry. Eur Respir J. 2015;46:186–96.
World Health Organization. Adherence to long-term therapies: Evidence for action. 2003. http://apps.who.int/iris/bitstream/10665/42682/1/9241545992.pdf. Accessed 30 Aug 2019.
Claxton AJ, Cramer J, Pierce C. A systematic review of the associations between dose regimens and medication compliance. Clin Ther. 2001;23:1296–310.
Schroeder K, Fahey T, Ebrahim S. How can we improve adherence to blood pressure-lowering medication in ambulatory care? Systematic review of randomized controlled trials. Arch Intern Med. 2004;164:722–32.
Horne R. Compliance, adherence, and concordance: implications for asthma treatment. Chest. 2006;130:65S–72S.
Lindell KO, Olshansky E, Song MK, et al. Impact of a disease-management program on symptom burden and health-related quality of life in patients with idiopathic pulmonary fibrosis and their care partners. Heart Lung. 2010;39:304–13.
Mason W, McLaughlin S, Dedopoulos S, et al. Real-world comprehensive disease management of patients with idiopathic pulmonary fibrosis. Current Respir Med Rev. 2019;15:4–15.
Russell AM, Ripamonti E, Vancheri C. Qualitative European survey of patients with idiopathic pulmonary fibrosis: patients’ perspectives of the disease and treatment. BMC Pulm Med. 2016;16:10.
Acknowledgements
The authors would like to thank the study participants for their involvement in this research. The authors confirm that patients were not involved in the design of this study or in the dissemination of results.
Funding
Sponsorship for this study and the journal’s Rapid Service Fee were funded by F. Hoffmann-La Roche, Ltd. All authors had full access to all the data in this study and take complete responsibility for the integrity of the data and accuracy of the data analysis.
Medical Writing, Editorial and Other Assistance
Editorial assistance in the preparation of this article was provided by Chiara Degirolamo, PhD, Luca Giacomelli, PhD, and Aashni Shah, of Polistudium, Milan, Italy. Support for this assistance was funded by ELMA Research. Additional medical writing support was provided by Catherine Stanton, of CMC AFFINITY, McCann Health Medical Communications, funded by F. Hoffmann-La Roche, Ltd.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Lisa H. Lancaster reports research grants, prior advisory board, and disease-state education from Genentech; research grants and disease-state education from Boehringer Ingelheim; research grants from Celgene and Novartis; research grants and consulting fees from Bellerophon and Galapagos; and consulting fees from Magnolia Therapeutics and Theravance, outside of the submitted work. Claudia Valenzuela has received speaker fees from Boehringer Ingelheim and F. Hoffmann-La Roche, Ltd. and advisory board fees from Galapagos. Wendi Mason has received personal fees from Genentech (a subsidiary of F. Hoffmann-La Roche, Ltd) and Boehringer Ingelheim, outside of the submitted work. Claus Neurohr has received honoraria for lectures and/or consultancy from Actelion, Bayer, Boehringer Ingelheim, F. Hoffmann-La Roche, Ltd., GSK and United Therapeutics. Elena Ripamonti is the CEO and co-founder of ELMA Research, a market research company, which received funding to perform the research presented in this manuscript. Klaus-Uwe Kirchgaessler is an employee of F. Hoffmann-La Roche, Ltd. Vincent Cottin reports personal fees and non-financial support from Actelion; grants, personal fees and non-financial support from Boehringer Ingelheim; personal fees from Bayer/MSD; personal fees from Gilead; personal fees from Novartis; grants, personal fees and non-financial support from Roche; personal fees from Sanofi; personal fees from Promedior; personal fees from Celgene; personal fees from Galapagos; and personal fees from Galecto, outside of the submitted work.
Compliance with Ethics Guidelines
The survey was performed, and ethical issues were addressed, following the Code of Conduct of the European Pharmaceutical Market Research Association (EphMRA) [15]. As indicated by the Article 3.4 of the EphMRA Code of Conduct, this market research study did not require Clinical Research Ethics Committee or Independent Review Board approval.
Data Availability
Qualified researchers may request access to individual patient-level data through the clinical study data request platform (https://www.clinicalstudydatarequest.com). Further details on Roche’s criteria for eligible studies are available at https://clinicalstudydatarequest.com/Study-Sponsors/Study-Sponsors-Roche.aspx. Further details on Roche’s Global Policy on the Sharing of Clinical Information and how to request access to related clinical study documents are available at https://www.roche.com/research_and_development/who_we_are_how_we_work/clinical_trials/our_commitment_to_data_sharing.htm.
Open Access
This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced digital features
To view enhanced digital features for this article go to https://doi.org/10.6084/m9.figshare.11871381.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Lancaster, L.H., Valenzuela, C., Mason, W. et al. Patients’ and Healthcare Professionals’ Experiences of Idiopathic Pulmonary Fibrosis Treatment with the Pirfenidone 801 mg Tablet Formulation: A Multinational Survey. Pulm Ther 6, 93–105 (2020). https://doi.org/10.1007/s41030-020-00111-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41030-020-00111-y