Key summary points
To develop an easy-to-use delirium risk assessment score (DRAS) to establish if a patient admitted to a hospital is at risk of getting delirium.
AbstractSection FindingsOur delirium risk assessment score (DRAS) based on the admission interview showed that risk of delirium based on predisposing risk factors can be assessed easily without elaborate cognitive testing and/or laboratory results and therefore less stressful for the patient. The DRASs as good as or somewhat better than other risk assessment scores are not developed for one specific population.
AbstractSection MessageBecause there is still a lack of knowledge, competence and awareness regarding delirium, understanding delirium risk factors helps clinicians, patients and caregivers in targeting non-pharmacological and pharmacological interventions aimed at lessening its burden.
Abstract
Purpose
Development and validation of a delirium risk assessment score. Predisposing risk factors for delirium were used, which are easily assessed at hospital admission without additional clinical or laboratory testing.
Methods
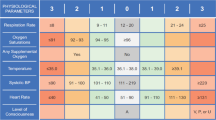
A systematic literature search identified ten risk factors: acute admission, alcohol use > 4 units/day, cognitive impairment, ADL impairment, age > 75 years, earlier delirium, hearing/vision problems, number of medication ≥ 5, number of morbidities > 2 and male. The DRAS was developed in a mixed patient population (N = 842) by the use of univariate and multivariate analyses and -2 log-likelihood calculation to weigh the risk factors. Based on the sensitivity and specificity, a cutoff score was calculated. The validation was performed in 3 cohorts (N = 408, N = 186, N = 365). In cohort 3, the DRAS was compared (AUC, sensitivity and specificity) to 3 instruments (Inouye, Kalisvaart, VMS rules).
Results
The delirium incidence was 31.8%, 20.3%, 15.6% and 15.1%. All risk factors were independently predictive for delirium, except male. The multivariate analyses excluded morbidities. The final DRAS consists of 8 items; acute admission, cognitive impairment, alcohol use (3 points), ADLimpairment/mobilityproblems (2 points), higher age, earlier delirium, hearing/vision problems, and medication (1 point). The total score is 15 points and at a cut-of score of 5 or higher the patient is at risk of developing a delirium. The cutoff was at 5 or more points, AUC: 0.76 (95% CI 0.72–0.79), sensitivity 0.77, specificity 0.60. Validation cohorts AUC was 0.75 (95% CI 0.96–0.81), 0.76 (95% CI 0.70–0.83) and 0.78 (95% CI 0.70–0.87), sensitivity 0.71, 0.67 and 0.89 and specificity 0.70, 0.72 and 0.60. The comparison revealed the highest AUC for the DRAS.
Conclusion
Based on an admission interview, the delirium risk can be easily evaluated using the DRAS shortlist score of predisposing risk factors for delirium in older inpatients.

Similar content being viewed by others
References
Dyer CB, Ashton CM, Teasdale TA (1995) Postoperative delirium. Arch Intern Med 155:461–465
Galanakis P, Bickel H, Gradinger R, Von Gumppenberg S, Förstl H (2001) Acute confusional state in the elderly following hip surgery: incidence, risk factors and complications. Int J Geriatr Psychiatry 16(4):349–355
Lindesay J, Rockwood K, Rolfson D (2002) The epidemiology of delirium. In: Lindesay J (eds) Delirium in old age, Oxford University Press, Oxford, pp 27–50
McCusker J, Cole M, Abrahamowicz M, Primeau F, Belzile E (2002) Delirium predicts 12-month mortality. Arch Intern Med 162:457–463
Witlox J, Eurelings LS, de Jonghe JF, Kalisvaart KJ, Eikelenboom P, van Gool WA (2010) Delirium in elderly patients and the risk of post discharge mortality, institutionalization, and dementia: a meta-analysis. JAMA 304(4):443–451
Inouye SK, Charpentier PA (1996) Precipitating factors for delirium in hospitalized elderly persons. Predictive model and interrelationship with baseline vulnerability. JAMA 275(11):852–857
Inouye SK (1999) Predisposing and precipitating factors for delirium in hospitalized older patients. Dement Geriatr Cogn Disord 10(5):393–400
Cole MG, McCusker J, Bellavance F, Primeau FJ, Bailey RF, Bonnycastle MJ et al (2002) Systematic detection and multidisciplinary care of delirium in older medical inpatients: a randomized clinical trial. CMAJ 167:753–759
Inouye SK, Viscoli CM, Horwitz RI, Hurst LD, Tinetti ME (1993) A predictive model for delirium in hospitalized elderly medical patients based on admission characteristics. Ann Intern Med 119:474–481
Morandi A, Davis D, Taylor JK, Bellelli G, Olofsson B, Kreisel S, Teodorczuk A, Kamholz B, Hasemann W, Young J, Agar M, de Rooij SE, Meagher D, Trabucchi M, MacLullich AM (2013) Consensus and variations in opinions on delirium care: a survey of European delirium specialists. Int Psychogeriatr 25(12):2067–2075
Yaghmour SM, Gholizadeh L (2016) Review of Nurses’ knowledge of delirium, dementia and depression (3Ds): systematic literature review. J Nurs 6:193–203
Kristiansen S, Konradsen H, Beck M (2019) Nurses’ experiences of caring for older patients afflicted by delirium in a neurological department. J Clin Nurs 28(5–6):920–930
Verloo H, Goulet C, Morin D, Von Gunten A (2016) Association between frailty and delirium in older adult patients discharged from hospital. Clin Interv Aging 11:55–63
Quinlan N, Marcantonio ER, Inouye SK, Gill TM, Kamholz B, Rudolph JL (2011) Vulnerability: the crossroads of frailty and delirium. J Am Geriatr Soc 59(Suppl 2):S262–S268
Lindroth H, Bratzke L, Purvus S, Brown R, Coburn M, Mrkobrada M et al (2018) Systematic review of prediction models for delirium in the older adult inpatient. BMJ Open 8(4):e019223
Kalisvaart KJ, Vreeswijk R, de Jonghe JF, van der Ploeg T, van Gool WA, Eikelenboom P (2006) Risk factors and prediction of postoperative delirium in elderly hip-surgery patients: implementation and validation of a medical risk factor model. J Am Geriatr Soc 54(5):817–822
Marcantonio ER, Goldman L, Mangione CM, Ludwig LE, Muraca B, Haslauer CM et al (1994) A clinical prediction rule for delirium after elective noncardiac surgery. JAMA 271(2):134–139
Rudolph JL, Jones RN, Levkoff SE, Rockett C, Inouye SK, Sellke FW et al (2009) Derivation and validation of a preoperative prediction rule for delirium after cardiac surgery. Circulation 119:229–236
Vochteloo AJ, Moerman S, van der Burg BL, de Boo M, de Vries MR, Niesten DD et al (2011) Delirium risk screening and haloperidol prophylaxis program in hip fracture patients is a helpful tool in identifying high-risk patients, but does not reduce the incidence of delirium. BMC Geriatr 11(11):39
Koster S, Oosterveld FG, Hensens AG, Wijma A, van der Palen J (2008) Delirium after cardiac surgery and predictive validity of a risk checklist. Ann Thorac Surg 86(6):1883–1887
Praktijkgids Kwetsbare ouderen (online). Available at www.vmszorg.nl
Fortes-Filho SQ, Apolinario D, Melo JA, Suzuki I, Sitta Mdo C, Garcez Leme LE (2016) Predicting delirium after hip fracture with a 2-min cognitive screen: prospective cohort study. Age Ageing 45(5):713–717
Freter S, Dunbar M, Koller K, MacKnight C, Rockwood K (2015) Risk of pre-and post-operative delirium and the delirium elderly at risk (DEAR) tool in hip fracture patients. Can Geriatr J. 18(4):212–216
Douglas VC, Hessler CS, Dhaliwal G, Betjemann JP, Fukuda KA, Alameddine LR et al (2013) The AWOL tool: derivation and validation of a delirium prediction rule. J Hosp Med. 8(9):493–499
Scholz AF, Oldroyd C, McCarthy K, Quinn TJ, Hewitt J (2016) Systematic review and meta-analysis of risk factors for postoperative delirium among older patients undergoing gastrointestinal surgery. Br J Surg 103(2)
Raats JW, Steunenberg SL, de Lange DC, van der Laan L (2016) Risk factors of post-operative delirium after elective vascular surgery in the elderly: a systematic review. Int J Surg 35:1–6
Van Meenen LC, van Meenen DM, de Rooij SE, ter Riet G (2014) Risk prediction models for postoperative delirium: a systematic review and meta-analysis. J Am Geriatr Soc 62(12):2383–2390
Ahmed S, Leurent B, Sampson FL (2014) Risk factors for incident delirium among older people in acute hospital medical units: a systematic review and meta-analysis. Age Aging 43(3):326–333
Vasilevskis EE, Han JH, Hughes CG, Ely EW (2012) Epidemiology and risk factors for delirium across hospital settings. Best Pract Res Clin Anaesthesiol 26(3):277–287
Oh ES, Li M, Fafowora TM, Inouye SK, Chen CH, Rosman LM, Lyketsos CG, Sieber FE, Puhan MA (2015) Preoperative risk factors for postoperative delirium following hip fracture repair: a systematic review. Int J Geriatr Psychiatry 30(9):900–910
Lindesay J, Rockwood K, Macdonald A (2002) The causes of delirium, in Delirium in old age. Oxford University Press, Oxford
Laurila JV, Laakkonen ML, Tilvis RS, Pitkala KH (2008) Predisposing and precipitating factors for delirium in a frail geriatric population. J Psychosom Res 65(3):249–254
Folstein MF, Folstein SE, McHugh PR (1975) «Mini-mental state». A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Knaus WA, Draper EA, Wagner DP et al (1985) APACHE II: a severity of disease classification system. Crit Care Med 13:818–829
Kalisvaart KJ, de Jonghe JF, Bogaards MJ, Vreeswijk R, Egberts TC, Burger BJ et al (2005) Haloperidol prophylaxis for elderly hip-surgery patients at risk for delirium: a randomized placebo- controlled study. J Am Geriatr Soc 53(10):1658–1666
Hetherington R (1954) The Snellen chart as a test of visual acuity. Psychol Forsch 24:349–357
Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI (1990) Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med 1990 113(12):941–948
van den Boogaard M, Pickkers P, Slooter AJ, Kuiper MA, Spronk PE, van der Voort PH, van der Hoeven JG, Donders R, van Achterberg T, Schoonhoven L (2012) Development and validation of PRE-DELIRIC (PREdiction of DELIRium in ICU patients) delirium prediction model for intensive care patients: observational multicentre study. BMJ 9(344):e420
Fan H, Ji M, Huang J, Yue P, Yang X, Wang C, Ying W (2019) Development and validation of a dynamic delirium prediction rule in patients admitted to the Intensive Care Units (DYNAMIC-ICU): a prospective cohort study. Int J Nurs Stud 93:64–73
Kat MG, Vreeswijk R, de Jonghe JFM, van der Ploeg T, van Gool WA, Eikelenboom P, Kalisvaart KJ (2008) Long-term cognitive outcome of delirium in elderly hip surgery patients. Dement Geriatr Cogn Disord 26(1):1–8
Woodford HJ, George J (2007) Cognitive assessment in the elderly: a review of clinical methods. QJM 100:469–484
Acknowledgements
We would like to thank Karlijn van Stralen (MSc. PhD) of the Spaarne Gasthuis Academy for her help with the statistical calculations and the editing of the article during the process of writing.
Funding
The current study did not receive any grant or financial support.
Author information
Authors and Affiliations
Contributions
RV and KK conceived and designed the study. RV and IK are responsible for obtaining the data. RV, KK, AM were involved in the analysis and interpretation of data. RV, KK and AM drafted the manuscript. The study was supervised by KK and AM. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interests.
Ethical approval
The studies were done in accordance with the Declaration of Helsinki and the guidelines on good clinical practice. Approval was obtained from the Advies Commissie Locale Uitvoerbaarheid (ACLU), the local committee of the METC of our hospital.
Informed consent
All patients and relatives were informed verbally. Patients and/or relatives gave their verbal consent for obtaining the data.
Data availability statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vreeswijk, R., Kalisvaart, I., Maier, A.B. et al. Development and validation of the delirium risk assessment score (DRAS). Eur Geriatr Med 11, 307–314 (2020). https://doi.org/10.1007/s41999-019-00287-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-019-00287-w