Studies investigating the transmission of mental health difficulties from parent to offspring increasingly focus on offspring emotion reactivity and regulation as one potential pathway through which risk is transmitted. This is as across early childhood prolonged exposure to unfavorable early-life caregiving environments, such as those involving high levels of parental psychological distress, may influence the development of maladaptive emotion reactivity and regulation in offspring (Glöggler & Pauli-Pott, Reference Glöggler and Pauli-Pott2008; Harden et al., Reference Harden, Panlilio, Morrison, Duncan, Duchene and Clyman2017). In turn, early childhood emotion reactivity and regulation play a key role in concurrent and future risk for psychological maladjustment (Eisenberg et al., Reference Eisenberg, Spinrad and Eggum2010) including internalizing and externalizing problems. Emotional reactivity and regulation in relation to environmental stimuli may involve simultaneous physiological, psychological and behavioral processes (Bridgett et al., Reference Bridgett, Burt, Edwards and Deater-Deckard2015). Although the influence of parental psychological distress on children’s behavioral emotion reactivity and regulation has been previously investigated, less is known regarding this influence on child emotion-related physiological responses, especially in early childhood. This is despite evidence indicating that children’s physiological processes may not be stable across the first years of life (Bornstein & Suess, Reference Bornstein and Suess2000) and potentially subject to various environmental influences.
In the present study we addressed this gap by focusing on the association between maternal psychological distress and both behavioral and physiological aspects of child fear-related reactivity and regulation. Subsequently, we examined whether child fear-related reactivity and regulation mediated the link between maternal psychological distress and child internalizing and externalizing problems.
The need for studies examining psychological well-being may be especially great in East Asian countries, where relatively less research on this topic has been conducted, and the mental health needs are large and growing. In fact, in Asian countries, internalizing and externalizing problems are reported more frequently compared to other countries (Magiati et al., Reference Magiati, Ponniah, Ooi, Chan, Fung and Woo2015), with up to 17% of children manifesting such difficulties (Woo et al., Reference Woo, Fung, Lee, Koh, Cai, Ng and Chan2007; Yang et al., Reference Yang, Qi, Cui, Li, Zhang, Zhou, Chen, Zhu, He and Zheng2019). This investigation is part of the effort to identify early risk factors that may contribute to the emergence of internalizing and externalizing problems. Moreover, given that maternal depressive or anxiety symptoms previously predicted later child internalizing and externalizing problems in a Singaporean sample (Soe et al., Reference Soe, Wen, Poh, Li, Broekman, Chen, Chong, Kwek, Saw, Gluckman, Meaney, Rifkin-Graboi and Qiu2016), the present investigation will contribute towards clarifying child factors that potentially mediate this pathway.
Emotion reactivity and regulation: Implications for child maladjustment
Emotional reactivity refers to one’s emotional responses to an event (Gross, Reference Gross and Gross2014). Emotion regulation refers to the internal and external processes, both implicit and effortful, which are responsible for modulating emotional responses over time and across exposures (Cole et al., Reference Cole, Martin and Dennis2004). These two constructs are conceptually disparate constructs but intertwined (Gross et al., Reference Gross, Sheppes and Urry2011). Young children who display elevated reactivity or experience emotions with elevated intensity tend to have more difficulty regulating them (Koole & Aldao, Reference Koole and Aldao2016).
As described by Gross and Jazaieri (Reference Gross and Jazaieri2014), dysfunctional patterns of emotional responses, primarily in terms of intensity or duration, or emotion regulation may influence the development of psychological maladjustment. Empirical evidence supporting this framework revealed positive associations between negatively valenced emotion reactivity and internalizing and externalizing problems in typically developing children (Eisenberg et al., Reference Eisenberg, Cumberland, Spinrad, Fabes, Shepard, Reiser, Murphy, Losoya and Guthrie2001) and adolescents (Shapero & Steinberg, Reference Shapero and Steinberg2013). Likewise, as across development emotion regulation contributes to one’s adaptability to the environment, it also predicts psychological maladjustment and the emergence of internalizing or externalizing problems (Eisenberg et al., Reference Eisenberg, Spinrad and Eggum2010; Kim & Deater-Deckard, Reference Kim and Deater-Deckard2011; Martin et al., Reference Martin, Boekamp, McConville and Wheeler2010; Quiñones-Camacho & Davis, Reference Quiñones-Camacho and Davis2018).
Besides behaviorally measured emotion reactivity and regulation, children’s risk for developing maladjustment may also be influenced by variability in the activity of the autonomic nervous system (ANS) in relation to emotional functioning (Calkins et al., Reference Calkins, Graziano and Keane2007). According to Porges’ polyvagal theory (Porges, Reference Porges2001; Porges, Reference Porges2003), the parasympathetic branch of the ANS participates in controlling physiological arousal and promoting emotion and behavior regulation, thus preserving homeostasis. Respiratory sinus arrhythmia (RSA) is commonly employed as an index of parasympathetic activity as it signals changes in heart-rate variability taking into account fluctuations in heart rate that occur naturally due to respiration (Porges, Reference Porges2007).
Three aspects of RSA (i.e., “baseline RSA”, “RSA reactivity,” and “RSA recovery”) are relevant to emotional functioning. First, high baseline RSA, reflecting high parasympathetic influence on the heart when at rest, is usually considered optimal as it may indicate low overall reactivity, or promptness for appropriate reactivity to the environment (Laborde et al., Reference Laborde, Mosley and Mertgen2018) and has been linked to more efficient emotion regulation (Beauchaine et al., Reference Beauchaine, Gatzke-Kopp, Neuhaus, Chipman, Reid and Webster-Stratton2013). Second, RSA reactivity reflects one’s response to emotional events. As the parasympathetic system withdraws to allow attending to the event, reduced RSA is anticipated during the event compared to baseline, i.e., RSA suppression. Greater RSA suppression during distress, in fact, related to higher scores in adaptive emotion regulation skills in school-aged children (Gentzler et al., Reference Gentzler, Santucci, Kovacs and Fox2009) suggesting that parasympathetic withdrawal may serve adaptive responding to distress. Regarding child maladjustment, RSA suppression during distress has been associated with both low (Calkins & Dedmon, Reference Calkins and Dedmon2000; Gentzler et al., Reference Gentzler, Santucci, Kovacs and Fox2009) and high (Calkins et al., Reference Calkins, Graziano and Keane2007; Fortunato et al., Reference Fortunato, Gatzke-Kopp and Ram2013) levels of child behavior problems but the former association was also bolstered by meta-analytic evidence (Graziano & Derefinko, Reference Graziano and Derefinko2013). This incongruity among studies highlights that interpretations of changes in ANS’ activity should incorporate contextual influences (Graziano & Derefinko, Reference Graziano and Derefinko2013). Third, RSA recovery is representative of return to baseline or to a state of alleviated arousal; parasympathetic activity is anticipated to increase and RSA to return to baseline-like levels. RSA recovery is considered adaptive as it facilitates the preservation of homeostasis when an active response to the stimulus is no longer required. Lower RSA recovery post-distress was associated with more dysregulated frustration (Santucci et al., Reference Santucci, Silk, Shaw, Gentzler, Fox and Kovacs2008). Despite its adaptive function and contrary to RSA baseline and reactivity, RSA recovery is not extensively investigated in terms of its association with child socio-emotional difficulties, especially in early childhood.
Maternal psychological distress and offspring emotion reactivity and regulation
The transmission of mental health difficulties from parent to offspring is a rather complicated process implicating both genetic and environmental influences (Hawn et al., Reference Hawn, Overstreet, Stewart and Amstadter2015). Although the genetic underpinnings of emotion reactivity and regulation are not extensively investigated, according to twin studies, up to 55% of individual differences in emotion regulation may be heritable (Hawn et al., Reference Hawn, Overstreet, Stewart and Amstadter2015). These genetic factors may also be linked to environmental factors that influence emotion regulation. In the case of maternal psychological distress, mothers with a genetic susceptibility to elevated distress may transmit this susceptibility to their offspring but also expose them to a non-optimal caregiving environment that will hinder the development of efficient emotion regulation processes. Several studies aimed at disentangling the genetic versus environmental influences in the intergenerational transmission of psychological distress. Their findings suggest that although genetic factors may play a role, maternal psychological distress may influence offspring outcomes, including emotion-related processes, largely through environmental pathways. This is as its association with said outcomes remains present when genetic factors have been accounted for (see Natsuaki et al., Reference Natsuaki, Shaw, Neiderhiser, Ganiban, Harold, Reiss and Leve2014, for a review). For instance, Ensink et al. (Reference Ensink, de Moor, Zafarmand, de Laat, Uitterlinden, Vrijkotte, Lindauer and Middeldorp2020) showed that up to 11% of the variance in mental health difficulties in middle childhood were due to maternal environmental risk, including elevated psychological distress; in contrast, genetic factors could not explain any additional variance in child mental health difficulties but were associated with the maternal environmental risk.
The substantial environmental component implicated in the influence of maternal psychological distress on child emotion reactivity and regulation is largely expressed in caregiving. According to an attachment-based coregulation framework (Laurent et al., Reference Laurent, Ablow and Measelle2012; Tronick, Reference Tronick2007), during the first years of life children learn how to navigate their own physiological and behavioral emotion-related responses and others’ emotional states through socialization processes when interacting with their caregivers (Thompson, Reference Thompson and Gross2014). In this context, coregulation describes the interactional attunement of physiological responses (Laurent et al., Reference Laurent, Ablow and Measelle2012) and synchronous affective states or behaviors between children and their caregivers (Feldman, Reference Feldman2007). With regards to fear reactivity and regulation, in particular, in the first few years of life caregiver presence seems to also have a buffering effect on infants’ distress-related physiological arousal (Hostinar et al., Reference Hostinar, Sullivan and Gunnar2014). For example, such buffering has been noted during the still-face phase of the still-face paradigm when mothers touched their infant while remaining unresponsive (Feldman et al., Reference Feldman, Singer and Zagoory2010), and in the process of initiating day care attendance (Ahnert et al., Reference Ahnert, Gunnar, Lamb and Barthel2004). The caregiver buffering effect may continue well into late childhood (e.g., Seltzer et al., Reference Seltzer, Prososki, Ziegler and Pollak2012; van Rooij et al., Reference van Rooij, Cross, Stevens, Vance, Kim, Bradley, Tottenham and Jovanovic2017). Around three years of age children start transitioning into a phase of transient exploration, wherein they are increasingly more confident in exploring situations and social interactions in unfamiliar settings on their own requiring less assistance from their caregiver in regulating fear (Callaghan et al., Reference Callaghan, Meyer, Opendak, Van Tieghem, Harmon, Li, Lee, Sullivan and Tottenham2019).
Coregulation and social buffering processes may be perturbed in mothers with elevated psychological distress, i.e., depressive mood and/or anxiety difficulties. This is as adults with elevated psychological distress experience difficulties in regulating their own reactions and emotions (Kircanski et al., Reference Kircanski, Waugh, Camacho and Gotlib2016; Schiweck et al., Reference Schiweck, Piette, Berckmans, Claes and Vrieze2019), which may also enhance inflexible responses to a distressing stimulus that over time reinforce the maintenance of anxiety or depressive mood (Cisler et al., Reference Cisler, Olatunji, Feldner and Forsyth2010). Due to their emotion regulation difficulties, parents with elevated psychological distress may be less attentive to their child’s distress signals, less available to provide or model emotional support to their children, or even exhibit negative behaviors when their child experiences distress (Borelli et al., Reference Borelli, Margolin and Rasmussen2015a; Möller et al., Reference Möller, Majdandžić and Bögels2015; Premo & Kiel, Reference Premo and Kiel2016). Perturbations in coregulation processes in the context of high maternal psychological distress may increase children’s risk for developing inefficient regulation patterns in terms of both physiology and behavior. In support of this notion, high maternal anxiety and depressive symptoms have been previously related to poor observed emotion reactivity and regulation in children across development (Glöggler & Pauli-Pott, Reference Glöggler and Pauli-Pott2008; Pauli-Pott et al., Reference Pauli-Pott, Mertesacker and Beckmann2004; Silk et al., Reference Silk, Shaw, Skuban, Oland and Kovacs2006). Yet, the direct association between aspects of maternal psychological distress and RSA during emotion-evocative tasks has been primarily investigated in school-aged children (Borelli et al., Reference Borelli, Burkhart, Rasmussen, Smiley and Hellemann2018; Borelli et al., Reference Borelli, Rasmussen, John, West and Piacentini2015b). Evidence of whether such effects are already present earlier in development are currently lacking despite findings indicating that physiological reactivity may not be stable across the first years of life (Bornstein & Suess, Reference Bornstein and Suess2000) and, thus, still malleable by environmental influences.
Offspring emotion reactivity and regulation and the transgenerational transmission of mental health risk
As offspring emotion reactivity and regulation may directly be influenced by maternal psychological distress and relate to the emergence of child internalizing or externalizing difficulties, it may to some extent mediate the transmission of mental health difficulties from parent to offspring. Some evidence for such a mediating role was documented in relation to frustration or anger reactivity and regulation during the preschool years (Halligan et al., Reference Halligan, Cooper, Fearon, Wheeler, Crosby and Murray2013) and self-reported emotion regulation in school-aged children (Suveg et al., Reference Suveg, Shaffer, Morelen and Thomassin2011). The mediating role of such emotion processes in the context of fear, however, remains largely unexplored. This is despite theoretical considerations and empirical support on the contribution of fear-related coregulatory processes to the emergence of mental health difficulties (Borelli et al., Reference Borelli, Rasmussen, John, West and Piacentini2015b; Nolte et al., Reference Nolte, Guiney, Fonagy, Mayes and Luyten2011) and previous demonstrations of the direct impact of maternal psychological distress on fear regulation in early childhood (Glöggler & Pauli-Pott, Reference Glöggler and Pauli-Pott2008).
With regards to child RSA, some evidence in school-aged children linked parental and child anxiety through child’s baseline RSA (Borelli et al., Reference Borelli, Rasmussen, John, West and Piacentini2015b). Although there is abundant evidence of links between RSA variables and child internalizing and externalizing difficulties (e.g., Graziano & Derefinko, Reference Graziano and Derefinko2013), whether child emotion-related RSA mediates the link between maternal psychological distress and child problems in early childhood remains unclear.
Current study
Building upon the existent evidence, the present study focused on two research questions. First, we investigated whether maternal psychological distress, as indicated by depressive or anxiety symptoms, would associate with physiological and behavioral reactivity and regulation in response to a novel, potentially frightening stimulus in 3.5-year-olds. As around this age, children’s exploratory behavior increases and they begin spending less time in direct contact with the caregiver, a developmentally relevant challenge is increased independence in emotion regulation. Accordingly, here we examine preschoolers’ emotion regulation skills in the absence of the mother as they encounter a potentially frightening stimulus. This allows for a window in the child’s independent emotion regulation capacity and the internalization of pertinent processes, socialized by the caregiver.
In terms of physiology we have incorporated both RSA reactivity and recovery, as they may provide constructive insight on children’s regulatory processes. Observations of child behavior during the task were also collected. We hypothesized that higher maternal distress would relate to: 1) decreased RSA suppression (i.e., decreased RSA reactivity during the task compared to baseline) indicative of decreased parasympathetic withdrawal in response to distress, and higher levels of observed reactivity between baseline and the fear-eliciting episode; 2) decreased RSA and observed recovery between the fear-eliciting episode and a return-to-baseline play phase following the fear-eliciting episode. Given the demonstrated prospective association between maternal depressive or anxiety symptoms and child internalizing and externalizing problems in our cohort (Soe et al., Reference Soe, Wen, Poh, Li, Broekman, Chen, Chong, Kwek, Saw, Gluckman, Meaney, Rifkin-Graboi and Qiu2016), our second aim was to investigate whether fear-related reactivity or regulation mediated the association between maternal psychological distress and child internalizing and externalizing problems at 48 months of age (Figure 1). Given the cross-sectional design implemented, the present study constitutes an exploratory step towards characterizing child physiology as a variable of interest in the link between maternal psychological distress and child mental health difficulties.

Figure 1. Conceptual model for the indirect association between depressive and anxiety symptoms, and child internalizing and externalizing problems through child fear reactivity or regulation.
Method
Participants
Pregnant women above 18 years of age were recruited during the first trimester of pregnancy to participate the prospective pregnancy cohort study, Growing Up in Singapore Toward Healthy Outcomes (GUSTO; Soh et al., Reference Soh, Tint, Gluckman, Godfrey, Rifkin-Graboi, Chan, Stünkel, Holbrook, Kwek, Chong and Saw2013). Recruitment took place at the Kandang Kerbau Women’s and Children’s Hospital and the National University Hospital in Singapore between June 2009 and September 2010. Demographic information was extracted from survey questionnaires administered as part of a scheduled appointment during pregnancy.
At 42 months of age, a subset of GUSTO toddlers attended a roughly 3-hour long neurocognitive testing visit. During this visit, children’s observed behavior and heart-rate data were collected during a fear-eliciting episode, administered as part of the standard testing protocol. Maternal self-reports on anxiety and depressive mood were collected during this visit. Maternal and paternal reports on child behavior problems were collected by the experimenters during a home visit at 48 months of age but were mailed to the parents in advance of that home visit.
This study focuses on a subset of 251 GUSTO children (128 girls), born from healthy singleton pregnancies (having a last-recorded Apgar score of ≥8; having birth weight ≥2000g and ≤4000g, after adjusting it for gestational age) who attended the 42-month testing visit, and had participated in the fear-eliciting episode without their caregivers present. Additional inclusion criteria were usable maternal psychological distress data during the same time-point, and usable data on child behavior problems from both parents, provided when children were 48 months old.
This study was approved by both the National Health Care Group Domain Specific Review Board (reference D/09/021) and the SingHealth Centralized Institutional Review Board (reference 2009/280/D). All parents provided informed written consent on behalf of themselves and their children before their participation and were reimbursed at the end of each visit.
Measures
Maternal psychological distress
Two aspects of psychological distress were assessed in the present study, depressive and anxiety symptoms. Maternal depressive symptoms was measured using the Beck Depression Inventory II (BDI-II; Beck et al., Reference Beck, Ward, Mendelson, Mock and Erbaugh1961). The BDI-II is a widely used measure of depressive symptoms, comprised by 21 questions, assessing mothers’ feelings during the past two weeks. Individual item scores (0-3) were summed up to a total score ranging from 0 to 63. Scores of 14 or above are indicative of at least mild depression. Within the present sample 13% reported a score of 14 (indicating presence of mild depression) or higher. Cronbach’s alpha for this questionnaire in our cohort was 0.84.
Maternal anxiety symptoms were assessed using the state anxiety sub-scale of the Spielberger State-Trait Anxiety Inventory (STAI-S) Form Y (Spielberger & Sydeman, Reference Spielberger and Sydeman1994). The STAI-S is a well-validated measure of current state-anxiety levels, comprised of 20 items. Total scores range from 20 (no anxiety) to 80. Within the present sample 30% reported a score of 40 (indicating clinically significant symptoms) or higher. Cronbach’s alpha was 0.93.
Children’s emotion reactivity and regulation
Emotion reactivity and regulation were measured during a fear-eliciting episode from the preschool version of the Laboratory Temperament Assessment Battery (Goldsmith et al., Reference Goldsmith, Reilly, Lemery, Longley and Prescott1999). The episode was video-recorded and child behaviors were coded at a later point in time by two trained raters who were blind to both maternal psychological distress variables and child behavior problem scores.
An adaptation of the “Jumping Spider” episode was administered to measure fear-related reactivity and regulation. This episode was designed to evoke fear-related responses due to unexpected events as these are considered a major source of fear in preschoolers. With this cohort we used a “Jumping Lizard” (JL), instead of a spider, as a more culturally appropriate stimulus. A detailed description of the episode administration and coding can be found in Tsotsi et al. (Reference Tsotsi, Borelli, Abdulla, Tan, Sim, Sanmugam, Tan, Chong, Qiu, Chen and Rifkin-Graboi2020). Briefly, participants received one score for each coding dimension (i.e., peak intensity of facial fear, bodily fear, vocal distress, lack of approach, withdrawal speed and distance, gaze aversion, and presence of startle) per trial for each of the four trials. An average score per dimension was calculated across the four trials. Following the four episode trials a “return-to-baseline” phase occurred, i.e. the experimenter indicated that the lizard was a toy and the child was allowed to play with it.
Interrater reliability was assessed through intra-class correlation coefficients (ICCs) using two-way mixed single measures with absolute agreement. ICCs, calculated per coding dimension, ranged between 0.81 and 0.99 for JL.
Except from startle, all average scores per dimension loaded onto an overall factor score, reflecting average fear reactivity during the four trials; this overall four-trial factor score was used in all analyses as an index of emotion reactivity (Table 1) wherein higher scores indicated greater fear reactivity. Similarly, one factor score, reflecting reactivity during the return-to-baseline phase, was calculated. Reductions in observed reactivity between the four trials and the “return-to-baseline” phase were considered to reflect efficient emotion regulation. As such, behavioral “Fear Regulation” was calculated as the difference score of JL’s return-to-baseline factor score minus the overall four-trial factor score.
Table 1. Summary of the behavior and RSA indices for fear reactivity and regulation during the Jumping Lizard episode

Heart-rate variability
Heart-rate data and respiratory activity data were collected using an ambulatory device, the Vrije Universiteit Ambulatory Monitoring System (VU-AMS, version 5fs, TD-FPP, Amsterdam, the Netherlands), and processed with the VU-DAMS software (version 2.2). The system uses three lead electrocardiograms (ECG), slightly below the right collar bone; between the two lower right ribs; and at the apex of the heart on the left lateral margin of the chest. Four lead impedance cardiograms recorded respiration (Ernst et al., Reference Ernst, Litvack, Lozano, Cacioppo and Berntson1999); these were placed at the suprasternal notch above the top of the sternum (i.e. Adam’s pit); at the xiphoid process; at the back, on the spine, at least 3cm above the level of the suprasternal notch; and at the back on the spine, at least 1cm below the level of the xiphoid process.
In order to collect RSA data, first, a primary check was performed to assess signal quality, i.e., the Q, R, S and T (QRST) deflections, comprising each heart rate waveform, and changes in impedance, and adjustments were made to the device to avoid errors or noise. Afterwards, the device was synced to computer time and disconnected from the computer, and data collection was initiated. The VU-AMS has an “event-marker’ button which was pressed to denote the start or end of an event. An event marker was recorded at the beginning and end of the baseline coloring session and of the JL episode. Additional markers were placed based on specific events within the episode (e.g., to indicate the start of the return-to-baseline phase). These markers were used to label the collected data and divide the entire HR recording into specific events. Before processing the HR recordings to calculate RSA values, the specific timings of each marker were also manually checked against each participant’s corresponding video.
The DAMS software calculates RSA in the time domain (instead of frequency) combining the ECG and respiration data using an automatic scoring algorithm. This algorithm detects the beginning and end of inspiration and expiration in each respiratory cycle and then uses this information to calculate the respiratory rate (i.e., breaths per minute). Respiration signals were filtered so that only frequencies between 0.10 and 0.40 Hz were included. RSA is calculated using a peak-valley estimation method (Grossman et al., Reference Grossman, van Beek and Wientjes1990); during each breath RSA is the difference score between the longest inter-beat-interval (IBI) during deceleration in the expiration phase (including a 1000ms delay after the end of expiration) minus the shortest IBI during heart-rate acceleration in the inspirational phase (including a 1000ms delay after the end of inspiration). When the RSA score was invalid, a score of zero was assigned to that breath. The DAMS software performs automated beat detection and runs an automated check to detect artifacts (e.g., missing ECG data), R-peaks based on QRST complexes (IBIs are then derived between two consecutive R-peaks over their distance in milliseconds), and irregular IBI’s (classified as high or moderately suspicious, designating beats that the software’s automated beat detector considers mistakes). All IBI’s labeled “highly suspicious” were manually removed. Within our sample suspicious IBI’s comprised between 0.1-0.5% of IBI’s. Additional checks of the automatically generated RSA scores were performed by visually inspecting the respiratory signals and IBI time series from the entire recording during a given event. Any breathing cycles with detected IBI artifacts (e.g., ectopic beats) were removed from further processing.
Baseline RSA data were collected during a 2.5-minute coloring session wherein children were seated and given an A4 black-and-white drawing to color. Baseline RSA was calculated as the average RSA within the 2.5 minutes. For the JL episode average RSA values were calculated and extracted for two events, i.e., the four-trial phase, and the “return-to-baseline” play phase. RSA reactivity was the physiological index of emotion reactivity, calculated as the difference score of baseline RSA minus RSA during the four-trial phase, wherein positive scores indicate RSA suppression (i.e., decreased RSA during the four-trial phase) and negative scores indicate RSA augmentation (i.e., increased RSA during the four-trial phase). RSA recovery was the physiological index of emotion regulation, calculated as the difference score of RSA during the “return-to-baseline” phase minus RSA during the four-trial phase, wherein positive scores indicate RSA augmentation (i.e., increased RSA during the “return-to-baseline” phase) and negative scores indicate RSA suppression (i.e., decreased RSA during the “return-to-baseline” play. In line with the corresponding behavioral variables, described earlier, we used one fear reactivity and one fear regulation RSA variable (Table 1). RSA reactivity scores were included as continuous in all analyses ranging from augmentation (negative values) to suppression (positive values) with higher scores reflecting higher suppression. RSA recovery scores were treated in the same way ranging from suppression (negative values) to augmentation (positive values) with higher scores reflecting higher recovery.
Child behavior problems
Reports from both parents on the Child Behavior Checklist (CBCL; Achenbach & Rescorla, Reference Achenbach and Rescorla2000) 1.5–5 years were used to measure child behavior problems. CBCL is a 99-item standardized assessment of child behavior problems with representative normative data, based on 24 societies, including Singapore. The global dimension of Internalizing Problems (36 items; score range: 0–72) includes emotional difficulties, such as anxiety, while Externalizing Problems (23 items; score range: 0–46) include negative or disruptive behaviors, such as aggression. Raw rather than T-scores (following the manual’s recommendation regarding research uses) were used in all analyses. Based on maternal reports, 17% (internalizing) and 12% (externalizing) of our participants had a T-score of 60 (i.e., the cutoff for borderline clinical range) or above. Based on paternal reports a higher percentage of participants scored a T-score of 60 or above, namely 24% for internalizing and 14% for externalizing. Cronbach’s alphas in our cohort were α = .88 (maternal) and α = .90 (paternal) for Internalizing Problems, and α = .90 (maternal) and α = .90 (paternal) for Externalizing Problems. Consistency between maternal and paternal CBCL reports was assessed through ICCs using two-way mixed average measures with absolute agreement. The ICCs were 0.62 and 0.69 for Internalizing and Externalizing Problems, respectively, indicating good consistency (Hallgren, Reference Hallgren2012). Therefore, average CBCL scores between maternal and paternal reports were used in all analyses.
Missing data
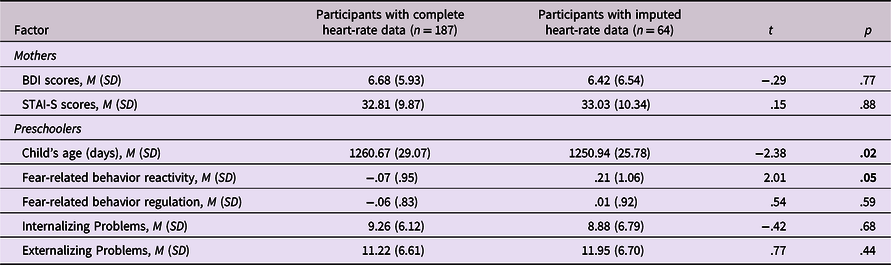
All 251 participants had completed datasets for all variables of interest besides heart-rate. Sixty-four participants had missing values for one or more RSA variables; this was due to technical problems with the heart-rate device or the software (n = 17), or heart-rate data not being collected due to lack of parental consent (n = 44) or lack of child compliance in wearing the heart-rate device (n = 3). A comparison between participants with complete heart-rate data (n = 187) and those with imputed heart-rate data (n = 64) on all other continuous variables is presented in Table 2. As Little’s Missingness-Completely-At-Random test was not significant [χ 2(814) = 871.45, p = .08], indicating missingess completely at random (Little, Reference Little1988), we implemented multiple imputation to handle the missing RSA values. Twenty imputations were generated, and pooled values were used in all subsequent analyses. As a means of validating the findings that emerged after imputing missing RSA values, the results of analyses conducted on participants with complete datasets (n = 187) are available as supplementary information.
Table 2. Comparison between participants with complete heart-rate data (n = 187) and those with imputed heart-rate data (n = 64) on other continuous variables of interest

Note. p values in bold fond are significant.
Data analytic plan
Analyses were performed using SPSS and AMOS, version 25.0. Descriptive statistics and Pearson bivariate correlations between the main study variables were conducted. The association between maternal depressive or anxiety symptoms on child fear-related variables was assessed through two sets of multivariable hierarchical linear regressions. In the first set, separate regressions were conducted for maternal BDI and STAI-S scores. Each of these variables was entered in the second step of the regression analysis after entering all the control variables in the first step. Given that maternal BDI and STAI-S scores were highly correlated in our sample, in the second set of regressions, maternal BDI and STAI-S scores were entered simultaneously in the second step. The control variables for both sets of analyses were ethnicity, maternal education (as an index of SES), birth order, and child’s age (in days) at the time of testing.
In relation to our second aim, we conducted follow-up analyses investigating whether fear-related variables would mediate the association between maternal BDI or STAI-S scores, and child internalizing and externalizing problems. This mediating effect was assessed through path analysis. In order to improve confidence interval accuracy (MacKinnon, Lockwood & Williams, Reference MacKinnon, Lockwood and Williams2004), bias-corrected bootstrapping (2000 resamples) was also implemented. Analyses were controlled for the same variables as in the linear regressions. Internalizing and externalizing scores were included simultaneously in all models with their error variances co-varied. Model fit was evaluated using multiple fit indices, namely the χ 2/df ratio wherein ratios of less than 3 indicate a good fit, the comparative fit index (CFI) and the Tucker-Lewis index (TLI), wherein values above .95 indicate a good fit, the root-mean square error of approximation (RMSEA), wherein values below 0.5 indicate a good fit, and the RMSEA-associated p value, wherein values above 0.05 indicate a good fit.
Results
Descriptive statistics
Frequency information of categorical demographic variables (ethnicity, maternal education, birth order) are presented in Table 3. Descriptive information of all continuous variables (i.e., child age in days, maternal depressive and anxiety symptoms, child fear reactivity and regulation scores, child behavior problems), and their correlations are presented in Table 4. Of note, higher RSA suppression, indicative of higher RSA reactivity, was related to higher behavioral reactivity. Significant correlations were also noted between higher behavior reactivity and lower behavior regulation, and between higher RSA reactivity (i.e., higher suppression) and higher RSA recovery.
Table 3. Frequency information for all categorical variables

Table 4. Descriptive information for all continuous variables in the total sample (n = 251), and bivariate correlations between the main predictor and outcome variables

† p < .10; *p < .05; **p < .01.
Maternal psychological distress and child emotion-related reactivity and regulation
To examine our first research question, we assessed whether maternal BDI or STAI-S scores influenced child emotion-related variables. The first hypothesis was partially supported as a significant effect of maternal BDI scores on child fear-related RSA reactivity was found (Table 5) suggesting that higher maternal depressive symptoms associated with lower fear-related RSA suppression. This effect remained significant when STAI-S scores were also included in the analysis. No influence of STAI-S scores on RSA reactivity was found. Additionally, no main effect of maternal BDI or STAI-S on fear-related behavior reactivity was observed.
Table 5. Summary of regression analyses examining the associations between maternal depressive symptoms and anxiety, and child fear reactivity and regulation separately and within the same model. In the first step of all analyses only the control variables, i.e., ethnicity, maternal education, birth order and child age at the time of testing, were included.

† p < .10, *p ≤ .05, **p ≤ 0.01.
Note. SE = Standard Error; CI = Confidence Interval.
In line with the first hypothesis, maternal BDI scores were significantly associated with fear-related RSA recovery (Table 5), partially confirming our second hypothesis; higher maternal depressive symptoms related to lower child RSA recovery. Again, this effect remained significant when STAI-S scores were also included. No effect of STAI-S scores on RSA recovery was observed. Finally, no main effect of maternal BDI or STAI-S was noted on fear-related behavior regulation.
Child fear-related reactivity and regulation between maternal psychological distress, and child internalizing and externalizing problems
In order to examine our second research question, we assessed whether an indirect effect of maternal BDI or STAI-S scores on child internalizing and externalizing problems through fear-related reactivity and regulation would be present. The first model, assessing the mediating effect of fear-related behavior reactivity, explained 14% and 9% of the variance of internalizing and externalizing problems, respectively, and yielded a good fit: χ 2/df = 0.50, CFI = 1.00, TLI = 1.05, RMSEA = .00, and RMSEA-associated p value = 1.00. Besides a significant direct effect of maternal BDI scores on child internalizing [b = .24, SE = .08, p = .00, 95%CI(0.09,0.38)] and externalizing [b = .21, SE = .08, p = .01, 95%CI(0.05,0.35)] problems, no other paths were significant (Table 6).
Table 6. Direct and indirect effects and confidence intervals of the path models on child internalizing and externalizing problems

Note. p values in bold fond are significant.
The second model, assessing the mediating effect of fear-related RSA reactivity, explained 13% and 9% of the variance of internalizing and externalizing problems, respectively, and yielded a good fit: χ 2/df = 1.99, CFI = .99, TLI = .90, RMSEA = .01, and RMSEA-associated p value = 1.00. As in the first model, a significant direct effect of maternal BDI on child internalizing and externalizing problems emerged. In addition, the negative association between maternal BDI scores and child RSA reactivity, indicating a link between higher maternal BDI scores and lower RSA suppression, was significant. No other paths were significant (Table 6).
The third model, assessing the mediating effect of fear-related behavior regulation, explained 14% and 9% of the variance of internalizing and externalizing problems, respectively, and yielded a good fit: χ 2/df = 1.04, CFI = .99, TLI = 1.00, RMSEA = .00, and RMSEA-associated p value = 1.00. Similar to the first and second models, a significant direct effect of maternal BDI on child internalizing and externalizing problems was found. No other paths were significant (Table 6).
Finally, the fourth model, assessing the mediating effect of fear-related RSA regulation, explained 14% and 11% of the variance of internalizing and externalizing problems, respectively, and yielded a good fit: χ 2/df = 1.07, CFI = 1.00, TLI = .99, RMSEA = .00, and RMSEA-associated p value = 1.00. Similar to the previous three models a significant direct effect of maternal BDI on child internalizing and externalizing problems was found. In addition, a significant negative association between maternal BDI and child RSA regulation emerged, indicating higher maternal BDI scores with lower RSA recovery. Likewise, lower child RSA recovery was associated with higher externalizing problems. The indirect effect between maternal BDI scores on child externalizing problems through child RSA regulation was also significant (Table 6). No other paths were significant.
Discussion
In the present study we sought to elucidate two gaps in the literature. First, we asked whether maternal psychological distress would associate with offspring fear-related reactivity and regulation in terms of both physiology and behavior. Second, we further examined whether offspring fear-related reactivity and regulation could be a variable of interest in explaining the previously documented association between maternal psychological distress, and child internalizing and externalizing problems.
With regards to our first question, maternal depressive, but not anxiety, symptoms were directly related to child physiological reactivity and regulation in the context of fear. Higher levels of maternal depressive symptoms were associated with smaller RSA decreases between baseline and exposure to a fear-eliciting stimulus, indicative of lower RSA suppression. This association was noted despite the fact that our examination occurred in a birth cohort sample, not selected for maternal psychological distress. Although the interpretation of RSA suppression among studies is varied, according to Porges’ polyvagal theory (Porges, Reference Porges2001; Porges, Reference Porges2003) changes in RSA denote a means of coping with distressing situations via parasympathetic withdrawal. Not surprisingly, children who are exposed to comparatively high levels of maternal depressive mood may be less prepared physiologically to deal with distress. Alternatively, they may exercise lower regulatory effort in relation to fear, perhaps as they may have developed familiarity with this feeling as a result of inefficient emotional support and socialization processes in mothers with elevated depressive symptoms. Such an interpretation would align with ideas regarding dampened reactivity to emotional challenges in depressed individuals (Rottenberg et al., Reference Rottenberg, Gross and Gotlib2005). Importantly, high maternal depressive symptoms were also associated with lower RSA recovery during the return-to-baseline period, suggestive of decreased competence in regulating the arousal post-distress. In line with Borelli et al. (Reference Borelli, Rasmussen, John, West and Piacentini2015b; Reference Borelli, Burkhart, Rasmussen, Smiley and Hellemann2018) we showed that maternal psychological distress, namely depressive symptoms, may be associated with offspring physiology during and after distress.
In the present study, maternal depressive symptoms only associated with child RSA within a fear-eliciting setting but not with child behavior. Although the effect of maternal depressive symptoms is in line with earlier evidence on fear-related behavior (Glöggler & Pauli-Pott, Reference Glöggler and Pauli-Pott2008), here we only observed this association for the pertinent RSA variables. Of note, however, greater fear-related RSA suppression, often considered to be adaptive, was associated with higher corresponding behavioral reactivity. This suggests that greater RSA decreases during the fear-eliciting task, indicating elevated arousal, may then be expressed as heightened behavior reactivity. Around 3.5 years of age, children’s emotion regulation may have not fully shifted to an internalized process, particularly when in novel, potentially frightening settings. Consequently, and in line with the idea of social buffering, when they experience elevated fear, perhaps the adaptive response is to behave intensely in order to signal their need for help in soothing. Such an interpretation would align with the coregulation framework, wherein children formulate expectations for external support based on the caregiver’s availability in different emotional contexts and increasingly internalize this information and use it in the absence of the caregiver (Calkins & Leerkes, Reference Calkins, Leerkes, Baumeister and Vohs2011). It may be relevant here as the fear-eliciting episode was administered to the children without their caregiver being present.
Moving on to our second research question, we further asked whether the association between maternal depressive symptoms and child internalizing and externalizing problems child would be mediated by fear reactivity and recovery. We found that child RSA recovery, but not reactivity, during fear concurrently mediated the association between maternal depressive symptoms and child externalizing problems. Diminished fear-related physiological recovery may be a variable of interest when investigating how mental health difficulties may be conveyed from parents to children. This finding suggests that the influence of maternal depressive symptoms on child physiology, especially in the context of fear, may yield concomitant difficulties for the child. It also resonates with well-documented difficulties in various aspects of self-regulation among children with externalizing difficulties (Eisenberg et al., Reference Eisenberg, Spinrad and Eggum2010). Although the present experimental design does not allow for causal inferences, it is conceptually consistent with earlier evidence supporting such a role for emotion-related reactivity and/or regulation in the relation between aspects of maternal psychological distress and child socio-emotional difficulties (Borelli et al., Reference Borelli, Rasmussen, John, West and Piacentini2015b; Halligan et al., Reference Halligan, Cooper, Fearon, Wheeler, Crosby and Murray2013; Maughan et al., Reference Maughan, Cicchetti, Toth and Rogosch2007; Suveg et al., Reference Suveg, Shaffer, Morelen and Thomassin2011).
Understandably the mediating effect of child physiological regulation in the association between maternal depressive symptoms and child externalizing problems may signify an interplay of genetic and environmental pathways in the intergenerational transmission of mental health difficulties. Adoption studies have, for example, revealed that birth mothers with depressive symptoms transfer some genetic risk for increased emotion reactivity (Natsuaki et al., Reference Natsuaki, Ge, Leve, Neiderhiser, Shaw, Conger, Scaramella, Reid and Reiss2010) or externalizing difficulties to their offspring (Pemberton et al., Reference Pemberton, Neiderhiser, Leve, Natsuaki, Shaw, Reiss and Ge2010). On the environmental front, depressive mood may influence the quality of caregiving. Parents who are high on depressive mood may be prone to cultivate disrupted or nonsynchronous coregulation processes (Kudinova et al., Reference Kudinova, Woody, James, Burkhouse, Feurer, Foster and Gibb2019; Woody et al., Reference Woody, Feurer, Sosoo, Hastings and Gibb2016) or exhibit unsupportive emotion socialization processes (Williams & Woodruff-Borden, Reference Williams and Woodruff-Borden2015), thus increasing children’s risk for developing inefficient emotion regulation. Such caregiving patterns may be rather marked in the context of fear or threat. Although meta-analytic evidence supports the environmental pathway of transmission for maternal depressive symptoms (Natsuaki et al., Reference Natsuaki, Shaw, Neiderhiser, Ganiban, Harold, Reiss and Leve2014), future investigations are needed to disentangle these components in relation to the mediating effect of child physiological regulation observed here. Of note, however, the environmental pathway of transmission for maternal psychological distress is important from a clinical standpoint as this pathway is modifiable by prevention programs or early interventions.
Contrary to earlier evidence assessing the influence of anxiety symptoms in mothers in the community on child RSA (Borelli et al., Reference Borelli, Rasmussen, John, West and Piacentini2015b), within our findings maternal anxiety was not linked to RSA variables for any of the episodes administered in our study. This unexpected finding may be due to other moderating factors may be at play, such as parental emotion socialization, mothers’ own parasympathetic activity or child age. For example, mothers with elevated anxiety symptoms may still experience and express adequate levels of positive affectivity, potentially alleviating the negative effect of anxiety on child physiology (Eysenck & Fajkowska, Reference Eysenck and Fajkowska2018). Age differences between the children in our study, who were only 3.5 years old, and those in earlier studies may contribute to this divergence; it may be the case that for maternal anxiety to influence child physiology a longer, cumulative exposure is necessary. Lastly, it is possible that the lack of a significant association between maternal anxiety symptoms and child RSA is due to low anxiety severity within the present community sample. Additional investigations are thus warranted, including mothers diagnosed with an anxiety disorder, in order to elucidate the nature of this association.
Despite high correlations between internalizing and externalizing problems, in the present study, this mediating effect was specific to the externalizing symptom dimension. One possible interpretation for this divergence may be that besides or concurrently with fear or distress the lack of RSA recovery following the fear-eliciting episode also reflected excitement and approach-related affect upon finding out that the lizard was actually a plastic toy. It may be that when it comes to a relatively novel experience, feelings of excitement and fear may co-occur. As elevated approach is more frequently associated with externalizing behaviors (Eisenberg et al., Reference Eisenberg, Spinrad and Eggum2010), it is possible that our results echo this mixture of positive and negative emotions. Given that child problems were assessed through parental reports, an alternative interpretation may involve the manifestation of internalizing problems in early childhood. Parents may struggle in distinguishing between the two problem dimensions as preschoolers are not yet able to fully or appropriately express internalizing problems sometimes “disguising” them as externalizing behaviors.
The present study has three main strengths. First, it is the first study that assessed both RSA reactivity and recovery during a fear-eliciting episode in the context of maternal affective difficulties within a normative sample. Although a number of studies are to date available using baseline RSA and RSA reactivity, the inclusion of RSA recovery is a most representative measure of physiological regulation. Second, the inclusion of both physiological and observational data allowed for the clarification of the links between physiology and expressed behavior. Third, as maternal depressive mood and anxiety symptoms usually co-exist, the inclusion of both symptom dimensions allowed us to investigate their unique effects on child emotion-related physiological responses.
Our study also has some limitations. First, as the predictor and mediator variables were captured at the same time-point, our study lacks a true longitudinal design. With a developmental psychopathology framework in mind a first step in exploring risk factors for the development of mental health difficulties is to investigate concurrent links between potential risk factors and mental health difficulties in the community. Hence, the concurrent associations, observed here, may be informative as a conceptual model and serve as an exploratory step towards characterizing child physiology as a variable of interest in the link between maternal psychological distress and child for child externalizing problems in a community sample. As a next step, it is critical to replicate such associations using a longitudinal design. This is as longitudinal designs are more suitable compared to cross-sectional ones for testing a model’s causal nature (Maxwell & Cole, Reference Maxwell and Cole2007; Selig & Preacher, Reference Selig and Preacher2009). Second, although the environmental component of transmitted risk from mothers to offspring could be explained based on a mother-child coregulation framework, we did not measure the interplay of physiological reactivity and regulation between mothers and their children. As these may interact with maternal affective symptoms to predict child outcomes, the inclusion of maternal physiological measures will improve our understanding of the observed associations.
In conclusion, in the present study maternal depressive symptoms related to child parasympathetic reactivity and regulation in the context of fear. Most importantly, parasympathetic regulation concurrently mediated the effect of maternal depressive symptoms on child maladjustment, namely externalizing problems. To our knowledge this study is the first to document such associations in the preschool years lending preliminary support to animal models that identified fear-related arousal as a mechanism for the transgenerational transmission of mental health.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S0954579421000936
Acknowledgments
The GUSTO study group includes Allan Sheppard, Amutha Chinnadurai, Anne Eng Neo Goh, Anne Rifkin-Graboi, Anqi Qiu, Arijit Biswas, Bee Wah Lee, Birit F.P. Broekman, Boon Long Quah, Borys Shuter, Chai Kiat Chng, Cheryl Ngo, Choon Looi Bong, Christiani Jeyakumar Henry, Claudia Chi, Cornelia Yin Ing Chee, Yam Thiam Daniel Goh, Doris Fok, E Shyong Tai, Elaine Tham, Elaine Quah Phaik Ling, Evelyn Chung Ning Law, Evelyn Xiu Ling Loo, Fabian Yap, Falk Mueller-Riemenschneider, George Seow Heong Yeo, Helen Chen, Heng Hao Tan, Hugo P S van Bever, Iliana Magiati, Inez Bik Yun Wong, Ivy Yee-Man Lau, Izzuddin Bin Mohd Aris, Jeevesh Kapur, Jenny L. Richmond, Jerry Kok Yen Chan, Joanna D. Holbrook, Joanne Yoong, Joao N. Ferreira., Jonathan Tze Liang Choo, Jonathan Y. Bernard, Joshua J. Gooley, Keith M. Godfrey, Kenneth Kwek, Kok Hian Tan, Krishnamoorthy Niduvaje, Kuan Jin Lee, Leher Singh, Lieng Hsi Ling, Lin Lin Su, Ling-Wei Chen, Lourdes Mary Daniel, Lynette P Shek, Marielle V. Fortier, Mark Hanson, Mary Foong-Fong Chong, Mary Rauff, Mei Chien Chua, Melvin Khee-Shing Leow, Michael Meaney, Mya Thway Tint, Neerja Karnani, Ngee Lek, Oon Hoe Teoh, P. C. Wong, Paulin Tay Straughan, Peter D. Gluckman, Pratibha Agarwal, Queenie Ling Jun Li, Rob M. van Dam, Salome A. Rebello, Seang-Mei Saw, See Ling Loy, S. Sendhil Velan, Seng Bin Ang, Shang Chee Chong, Sharon Ng, Shiao-Yng Chan, Shirong Cai, Shu-E Soh, Sok Bee Lim, Stella Tsotsi, Chin-Ying Stephen Hsu, Sue Anne Toh, Swee Chye Quek, Victor Samuel Rajadurai, Walter Stunkel, Wayne Cutfield, Wee Meng Han, Wei Wei Pang, Yap-Seng Chong, Yin Bun Cheung, Yiong Huak Chan and Yung Seng Lee.
Funding statement
This research is supported by the Singapore National Research Foundation under its Translational and Clinical Research (TCR) Flagship Programme and administered by the Singapore Ministry of Health’s National Medical Research Council (NMRC), Singapore- NMRC/TCR/004-NUS/2008; NMRC/TCR/012-NUHS/2014. Additional funding is provided by the Singapore Institute for Clinical Sciences, Agency for Science Technology and Research (A*STAR), Singapore, Biomedical Research Council (BMRC) Strategic Positioning Fund (SPF) [Grant ID: SPF2013/002]; the NMRC [NMRC/CBRG/0039/2013]; and the Young Investigator Award at the Singapore Institute for Clinical Sciences [SICS/YIG/2013/002].
Conflicts of interest
None.