Introduction
Health, treatment, and the impact of medical interventions on health lie at the heart of medical and demographic history (McKeown Reference McKeown1970; Woods Reference Woods2007). One of the few ways to study these issues in a historical context is to explore the impact that health interventions have had on the life chances of the individuals concerned. Death is a rather robust health indicator that does not leave much room for changing definitions over time or space and has the advantage that it covered the whole population and that its registration was institutionalized in many countries long before it was normal to report morbidity (Ryan Johansson Reference Ryan Johansson1991).
Whereas in the earliest studies on the effect of medical intervention on mortality, rather crude methods were used (such as visual inspection of time trends in mortality before and after the date at which effective medical measures became available), later on more advanced statistical methods were used. This allowed quantitative estimates of changes in mortality coinciding with the introduction of antibiotics and vaccines or the provision of better-qualified medical personnel (Lazuka Reference Lazuka2018; Lorentzon and Pettersson-Lidbom Reference Lorentzon and Pettersson-Lidbom2021; Van Wijhe et al. Reference Van Wijhe, McDonald, de Melker, Postma and Wallinga2016).
Information on the mortality of the medical profession and of their family members might also be used as a historical “critical test for medical knowledge and practice” (Woods Reference Woods1996). The underlying assumption of this approach is that doctors have the most medical knowledge and that they apply this knowledge to themselves, to their families, and their patients; thus, the mortality of members of the medical profession and of their families is “a yardstick against which others can be compared” (Woods Reference Woods2000: 230).
The secular increase in life expectancy in the Western world from the last quarter of the nineteenth century until the 1930s was largely caused by the decline in infant and child mortality. It is therefore important to study whether and how medical care for infants and children has played a role in this process.Footnote 1
Already in the 1920s several studies were published in which the authors tried to find out whether the children of medical doctors experienced lower mortality, being considered indicative of knowledge about good health practices by their parents (Emerson Reference Emerson1924; Anonymous 1924; Lennox Reference Lennox1924). These studies were based on questionnaires for a small number of families, did not refer to a specific time window, and gave conflicting results.
In the early 1990s Preston and Haines (Reference Preston and Haines1991) and Ewbank and Preston (Reference Ewbank, Preston, Caldwell, Findley, Caldwell, Santow, Cosford, Braid and Broers-Freeman1990) studied the topic in a more thorough way. They made use of the Public Use Samples of the US censuses of 1900 and 1910 and, through indirect techniques, derived estimates of child mortality (death before age 5) for the years 1895 and 1905 (and with other data until 1924) for physicians and surgeons. These estimates were based on information on the number of children married women had borne and the number of those children who had survived to the time of the census. Comparable measures were derived for England and Wales from the Census of Marriage and Fertility in 1911 (Preston and Haines Reference Preston and Haines1991).
The outcome of the comparison of the mortality of children of medical doctors with those from other families was negative for the USA; groups which could be expected to have had lower mortality because of better awareness of good hygienic practices and closer connection to networks of professional expertise did not, in fact, enjoy a substantial mortality advantage. The mortality of offspring of doctors was only six per cent below the national average. Preston and Haines (Reference Preston and Haines1991: 206–7) were aware that the relatively high mortality seen among the children of medical professionals in the USA reflected in part the lower standards of admission into these groups at the time. The comparative mortality advantage of professionals in England and Wales was much higher, attributable to their comparative economic advantage, partly reflecting the greater success of England’s professional societies in restricting access to the professions (Preston, and Haines Reference Preston and Haines1991: 187–88). By comparing the American circumstances with those of other societies, Preston and Haines (Reference Preston and Haines1991: 177) believed that more insight could be given into factors relevant for the pattern of child mortality, such as the relative social and economic standing of different social groups, differences in childcare practices, and the disease environment. Kunitz (Reference Kunitz1991: 235) argued that the USA and UK were both exceptional cases and thus not very suitable as models for the interpretation of the role of medicine. Mackenbach (Reference Mackenbach2020: 112) also considered the British experience as not generalizable, considering that England’s cause-of-death composition was different from that in many other European countries. McKeown (Reference McKeown1970) had already stated earlier that the effect of medical practice had to be investigated in countries where the timing of industrialization and patterns of practice were different from those in the UK. It thus makes sense to try to repeat Preston and Haines’ analysis for other European countries.
In our paper, we focus on the mortality of infants and children in the families of medical practitioners in the Netherlands. As in other countries, infant and childhood mortality declined in the Netherlands from the 1870s on, due to a combination of changes in infant care, partly driven by cultural change (breastfeeding, modern hygienic practices) and the start of large-scale public sanitation (see, for example, Morel Reference Morel, Schofield, Reher and Bideau1991; Preston and Haines Reference Preston and Haines1991).Footnote 2 Medical doctors there were convinced that they had played a decisive role in the decline of infant and child mortality. “As far as the decrease in the mortality of children is concerned, and in particular that of children below age one, it certainly is not a bold proposition when I assume that we might in these figures also observe the positive effect of the advice and prescriptions for the treatment and diet of young children, abundantly given in recent years by the medical profession,” wrote one doctor (Van Vollenhoven Reference Van Vollenhoven1894). Another one argued: “It is obvious that the lives of many children have been saved due to the fact that the spread of the medical profession over the Netherlands is at present much wider than was the case twenty years ago” (Bruinsma Reference Bruinsma1905).
Our approach differs from the Preston and Haines study in various aspects. We do not use a standardized mortality ratio based on indirect estimates, but calculate actual death rates separately for infants and young children. Our study is not restricted to the mortality of children whose mothers survived until the census but covers all children born regardless of the survival status of the mother. This ensures that no bias is introduced by the correlation of the mother’s and children’s survival chances (Condran Reference Condran1994). We do not limit ourselves to the situation in the last decade of the nineteenth and the first decades of the twentieth century but focus on the whole period during which the mortality decline took place from the 1850s on. Finally, we distinguish between groups of medical practitioners, which differ in the kind of education and training that they had received.
We reconstructed the life histories of the offspring of a group of Dutch medical professionals who were practicing in a high-mortality region in the country between 1850 and 1922. In this period infant mortality declined from 182 per 1000 live births to 84, and child mortality from 125 per 1000 one-year-old children to 37 per 1000. The data therefore allow us to go back to a period in which medical professionals had to deal with very high infant and child mortality. The period 1850–1922 was also a very important transitional period in the history of medical training, the medical profession, and medical science. During this period a new regulation of medical authority and medical education took place, allowing us to compare the experience of various groups of medical practitioners, distinguished by the medical training that they had received (university graduates versus non-graduates) and by the basis of medical knowledge (‘traditional’ versus ‘biomedicine’) (Aulbers Reference Aulbers, Aulbers and Bremer1995; Houwaart Reference Houwaart, Aulbers and Bremer1995). At the end of the nineteenth century, the discovery of the microbiological origin of many diseases not only allowed more targeted advice on how to prevent infection, but was also a springboard for the development of prophylactics such as vaccinations, and therapies such as immune sera and antibiotics (Léonard Reference Léonard and Salomon-Bayet1986; Porter Reference Porter1997: 245–303). An excellent data source is available for the period that we study, namely the population register, which makes it possible to study various factors that may have influenced the level of infant and child mortality in the medical professional’s family.
We will focus on two questions:
-
Were medical practitioners working in the period between 1850 and 1922 able to lower the level of their children’s mortality below the levels of children coming from groups comparable to them as far as socioeconomic and educational status is concerned?
-
Were medical professionals who had received a more thorough theoretical medical training or who had been trained in more recent periods better able to reduce the mortality of their offspring than colleagues with a more practical training or less recent graduation?
Before starting to answer these questions, we discuss the position of the Dutch medical professional in the nineteenth century, paying particular attention to the changes that took place in their training and organization. Then we briefly present information on the question whether medical men indeed took the responsibility for the medical care of their children. Finally, we discuss the research plan, the period and area that we are studying, and the sources used for this study.
The medical profession in the Netherlands
Two particular years mark the development of the medical profession in the Netherlands during the nineteenth century: 1818, when an enactment reorganized the medical laws that had been passed during the French occupation; and 1865, the year in which the government established new legislation concerning medical practice and public health inspection.
The 1818 law regulating the issuing of medical licenses created a clear legal boundary separating the unqualified from the qualified practitioners. It also reinforced an already existing division within the medical profession between academic or university and non-academic or non-university-trained practitioners. The two groups were medical doctors separately licensed by the universities, and the non-academic group (sometimes referred to as “the second medical order”) “licensed” or otherwise recognized by provincial committees composed of the “most skilled and experienced men” such as medical doctors (Van Lieburg Reference Van Lieburg1983). The 1818 law also confirmed the already existing division in the spheres of practice of the medical profession between internal medicine, obstetrics, and surgery. Finally, the law differentiated according to the location of the practice: town, countryside, or ship.
The university-trained medical professionals pursued a purely theoretical study at one of the then three Dutch universities, and subsequently became doctors without any clinical training. To graduate, university-trained doctors were required to write a dissertation in one of three disciplines: internal medicine, obstetrics, or surgery. They received the title respectively of medicinae doctor, artis obstetriciae doctor, or chirurgiae doctor. University-trained doctors were allowed to practice in towns as well as in the countryside. They diagnosed complaints, prescribed treatments, attended, and advised in particular the upper middle class, often after having passed a period as doctor in the municipal health services for the poor and mostly settled in the towns.
The non-graduate doctors (here referred to as the second medical order) acquired the skills and knowledge needed to pass the examination via an apprenticeship in an existing practice or by attending one of the six clinical schools established by the state to improve the clinical training of the non-graduate doctors. They were required to pass an examination before a local departmental or provincial committee. Three categories of practitioners in internal medicine were distinguished: the stads-heelmeester (town surgeon), the plattelands-heelmeester (country surgeon), and the scheeps-heelmeester (naval surgeon). Non-university-trained obstetric practitioners were formally divided into plattelands vroedmeester (rural man-midwife) and stads-vroedmeester (town man-midwife), but they had the same qualifications (ibid.). They mostly took care of the poor, in particular in the countryside. Own experience and study of the experiences of colleagues were the basis of their practice.
The quality of the practical training and theoretical knowledge of the non-university medical practitioners differed considerably. The six clinical schools nominally offered a four-year program with a strong emphasis on clinical training but only the schools of Rotterdam and Amsterdam were of a high level and could even be ranked above the university medical departments. The students of the other clinical schools and those people who had prepared themselves for the examination via an apprenticeship in an existing practice compared less favorably with the aforementioned group.
A distinct group were the officieren van gezondheid (military health officers), who had graduated at the military health school in Utrecht after four years of study. The school existed until 1865 and derived its value from the fact that in addition to offering a sound basis in theory, the institute offered practical-clinical education. In their comings and goings, the officers were not hindered by the old separation between internal medicine and surgery. They served in hospitals that functioned more or less as modern hospitals and were actively involved in preventive medicine (Kerkhoff Reference Kerkhoff and de Moulin1988). Whereas the judgment about the naval surgeons was generally very negative, the military medical school was considered an excellent medical training institution and the military health officers were a highly valued part of the medical profession. The medical health officers could after a certain period in office start a practice as country or city surgeon, whereas for a license as man-midwife an additional exam had to be passed. During a large part of the nineteenth century, medical health officers (among which many were Germans) were responsible for almost all medical care in the Malay Archipelago (Kerkhoff Reference Kerkhoff, van Heteren, de Knecht-van Eekelen and Poulissen1989).
The medical profession as a whole ranked rather high but the prestige of the various groups of medical professionals differed widely. Those holding a doctor’s degree stood clearly above other medical professionals. Their prestige was above all determined by the societal consensus on the priority of intellectual over physical work (Frijhoff Reference Frijhoff1983), their academic education and knowledge of Latin, and the standing of the houses to which they were called and not so much a consequence of their better knowledge or skills. They predominantly came from the highest layers of the lower middle class and the bourgeoisie, and generally earned a higher income (Goudsmit Reference Goudsmit1978: 29). A large part of non-university-trained medical practitioners also originated from the petty or wealthier bourgeoisie, but their economic situation fluctuated and it required a lot of energy to earn a decent living (Van Lieburg Reference Van Lieburg1985; De Man Reference De Man1902). In the end of the period under study, from the 1890s on, the study of medicine opened to new classes, which were not used to sending their sons into academia, but this opening was still mainly restricted to the middle class.
From the 1850s on, the government tried to bring order into the variety of licenses available to the medical profession. In many respects the situation was considered as an abuse: the level of medical knowledge as such was low, and there was criticism on the purely theoretical character of the university training, on the low scientific level of the training in the clinical schools, and the insufficient control on the examinations and the organization of medical care (Verdoorn Reference Verdoorn1965: 84–94; Van Lieburg Reference Van Lieburg1983, Reference Van Lieburg1985). This ultimately led in 1865 to a new regulation of the medical profession and authority, dubbed the Medical Practitioners Act. This law made an end to the large differences in medical training and qualification of the various categories of medical practitioners. It implied an uniformization of medical training, to be given only at universities, and of medical competence, as the dichotomy between internal medicine and obstetrics and surgery was abolished. All medical students would be required henceforth to pass a state examination consisting of theoretical and clinical practical parts, which conveyed the right to the title of arts (doctor) and authority to practice in all fields of medicine (internal medicine, surgery, and obstetrics). The requirements for the examination could be met only by attending the universities of Utrecht, Leyden and Groningen, or the Atheneum Illustre in Amsterdam, which in 1876 was elevated to the University of Amsterdam. Medical education therefore became completely localized in the universities. It was explicitly laid down that the state examination in internal medicine, obstetrics, and surgery had to consist of a theoretical and a clinical practical part. This last element required sufficient proof of clinical practical knowledge acquired at the bedside and in performing surgical and obstetric operations. The establishment of a state examination committee imposed in the years 1865–1885 a uniform opinion on both the level and the nature of the knowledge of the candidates from the various medical schools. It promoted the practical-clinical training and skills using the new achievements of physics and chemistry and forced the definitive introduction of clinical education at the universities (Van Lieburg Reference Van Lieburg and Frijhoff1990: 97).
In the first years after the passing of the act, many tried to get a license as arts – especially those who had already practiced medicine for a long time. The examination rooms were filled with town surgeons, country surgeons, and military health officers. After some years, only university graduates like bachelors of medicine and doctors of medicine took the exams.
Shortly after the Medical Practitioners Act was introduced, medicine also gradually started to acquire a new theoretical basis: instead of a jumble of symptom-oriented and speculative ideas, new theories became more prominent, theories generated and validated by experimental science and characterized by universalized diagnostic and therapeutic categories, leading to changes in practical and clinical medicine. From the key years 1876–1885 onwards, a gap became visible between the young medical practitioners who were henceforth taught by groups of microbiologists, professors and graduates who were on Pasteur’s side, and the elderly whose studies were entirely pre-Pasteur. From the 1880s onwards, medical journals, reference works, and medical textbooks increasingly showed Pasteurian convictions (Léonard Reference Léonard and Salomon-Bayet1986: 156).
Comparisons over time of the effect of medical expertise on the life chances of infants and children are very complex. There is a change in the disease panorama from one in which environmental conditions were a very important factor, to one in which congenital diseases became more relevant. Important changes took place in the medical training and gradually a new group replaced the old groups of medical practitioners. Old medical doctrines were substituted by the Pasteurian inspired theories. All these transitions were complex and they cannot be pinpointed to a specific point in time (Salomon-Bayet Reference Salomon-Bayet and Salomon-Bayet1986). Thus, the passage of time and the changes in the training and qualification of the medical profession are crucial elements in our study; they are key to the research question whether medical practitioners who had a better and more recent medical training were better able to reduce the mortality of their offspring than less qualified colleagues.
Was the father the family doctor?
Before presenting the data, an important issue has to be discussed, namely the question whether medical practitioners indeed took responsibility of the medical care of their own children. Most medical men indeed treat the members of their own family, in particular their children (Lens Reference Lens1984; Rennert et al. Reference Rennert, Hagoel, Epstein and Shifroni1990: 96–98). In 1847 the Code of Ethics of the American Medical Association stated that: “…the natural anxiety, the solicitude which he [the physician] experiences at the sickness of a wife, a child, or anyone who by ties of consanguinity is rendered peculiarly dear to him, tend to obscure his judgment, and produce timidity and irresolution in his practice” (La Puma, and Priest Reference La Puma and Priest1992: 1810). Thus, children often did not benefit when treated by their father (McSherry Reference McSherry1988; Wasserman et al. Reference Wasserman, Hassuk, Young and Land1989; La Puma et al. Reference La Puma, Stocking, LaVoie and Darling1991; Dusdieker et al. Reference Dusdieker, Murph, Murph and Dungy1993).
First-hand historical accounts such as diaries and autobiographies, collections of letters, and books written by children and spouses of medical practitioners about their growing up give an impression of the complaints and illnesses for which the help of the father in his role as medical expert was called upon. These personal documents show that Dutch medical practitioners in the nineteenth and early twentieth century indeed took the responsibility for the medical care of their children and that they did not eschew taking even the most drastic measures when they considered that necessary. Documents illustrate that they indeed attended the delivery of their wife’s children and had the main responsibility for the outcome (Verkade Reference Verkade1982: 105). Life-threatening operations of own family members are mentioned several times, for example in the autobiography of Albert Willem van Renterghem, a military health officer and arts (Van Renterghem Reference Van Renterghem1924: 190–91). Many personal documents show that many medical practitioners continuously and kept a strict eye on the health of their children. Sometimes, against the opinion of the strong religious community in which they lived, they vaccinated their own children (Allebé Reference Allebés.a.; Perneel Reference Perneel2000: 105). Documents show that medical men as fathers in an early stage identified infectious diseases and tried to apply strict norms regarding social contacts and the isolation of their children (Van Renterghem Reference Van Renterghem1924: 153). Various personal accounts made mention of the way in which medical practitioners monitored the health of their children. In case of illness, they checked regularly whether the body temperature of their children had increased and boiled the milk they gave their children (Hellema Reference Hellema2017). Frederik van Eeden, (1860–1932) medical doctor and novelist left many ego-documents and very detailed personal diaries showing a continuous vigilance concerning the health of his young children (Van Eeden Reference Van Eeden1971). Documents also provide proof that medical practitioners as fathers strongly encouraged the breastfeeding of their children (Wijgchel Reference Wijgchel1973: 140–45). In case of emergency, fathers as doctors resorted to techniques with which they did not have much experience, such as tracheotomy in case of croup (Van Renterghem Reference Van Renterghem1924: 484–85). We may thus conclude that fathers with a medical training indeed acted as the family doctor, which could be beneficial for the survival rates of their own children compared to children from other (comparable) social classes, as we hypothesize in our first research question.
Data collection
To test whether the life chances of the children of the various groups of medical practitioners differed significantly from each other and from those of children born within families of which the head did not have a medical background, a complete reconstruction of the reproductive history of the medical practitioner’s family and the survival status of his children and those of a comparable group without a medical background is needed.
We first constructed a database with information on medical practitioners, practicing in the Netherlands at any time during the period 1850–1922. In the next stage, the selected medical professionals were identified in the municipal population registers to collect information on their personal characteristics and those of their families. In stage 3, the vital registration system and other sources were used to check for missing, incomplete, or inconsistent information. In stage 4, we used data on children born in families from other social classes; that allowed us to find out whether or not the specific knowledge and capacities of the medical practitioners had a decreasing effect on the mortality of their children, compared to the children from parents who lacked that specific knowledge and capacities.
Given the time-consuming data-collection process, we focused our study on the medical profession practicing at least once in their career in the western part of the country. Map 1 shows the administrative boundaries of this region as well as the level of infant mortality in each municipality in the period 1841–1860.
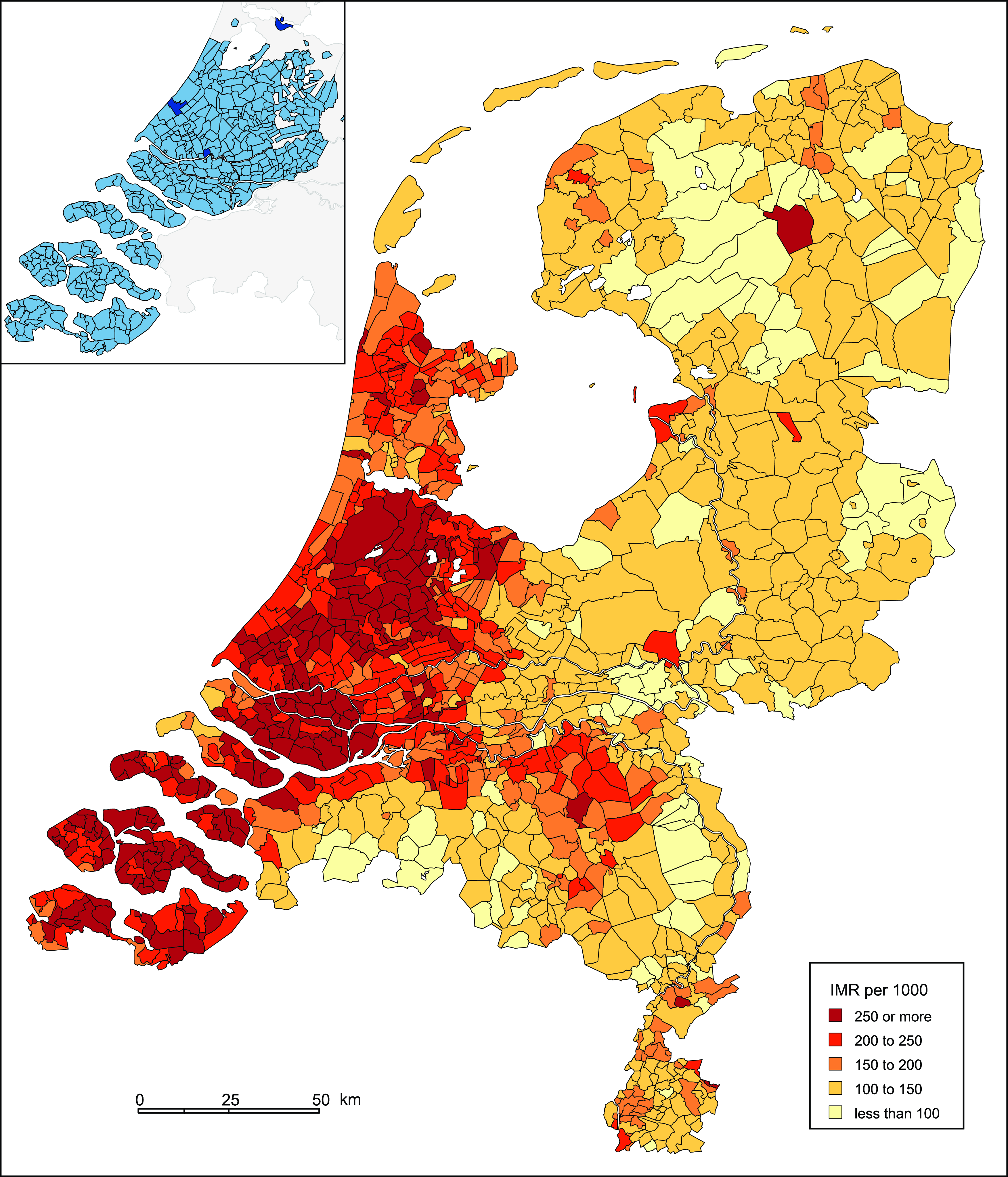
Map 1. Infant mortality rates (per 1000 live births) per municipality, Netherlands, 1840-61, and map inset with selected western municipalities for medical practitioners. Source: Ekamper and Van Poppel (Reference Ekamper and van Poppel2008). Note: digital geometry from NLGis (Boonstra Reference Boonstra2007).
Until around 1880 this part of the country had the highest infant mortality rates (IMRs): in large parts of the western Netherlands, infants had a one in four chance of dying within the first year of life.Footnote 3 After 1880 this regional pattern changed considerably and in the 1930s these regions had the lowest IMRs. The high levels of IMR as well as the rapid change in its value make the area an interesting study region, as it offered medical practitioners the chance to have a real effect on the life chances of the newborns. In the chosen part of the country, the absolute and relative number of medical practitioners was also much higher than in other regions. The better economic situation, leading to a substantial demand for medical services, and the fact that universities and former clinical schools were nearly all located in the west explain this unequal distribution of doctors over the regions (Verdoorn Reference Verdoorn1965: 122–24). It is also suggested that the mental climate here corresponded more with the cultural needs and the social aspirations of a substantial part of the profession (Rutten Reference Rutten1985: 156–57). And, last but not least, the process of medicalization, the “increasing frequency of contact with doctors, (…) and the growing authority of doctors over the behavior of the sick” (Riley Reference Riley2001: 87), started earlier in the western part of the country. If the medical profession played a role in the decrease of infant and child mortality at all, one might expect to see evidence of that in this area in the first place.
For our study, we selected 2827 medical practitioners born between 1805 and 1890 practicing in the selected region at any moment between 1850 and 1905. This information is provided by (bi-annual) provincial and state medical registers, listing all officially recognized medical practitioners by place of residence. The first register that we used applied to 1851, the last one to 1903. For each individual medical practitioner, the registers recorded surnames, initials, university and non-university degrees, and dates and places of examination. To complete the information on the medical training of the selected medical professionals, we could make use of the database of the medical professions in the Netherlands in the period 1450–1950 developed by Van Lieburg (Reference Van Lieburg2011), containing information on some 185,000 practicing medical professionals.
Only those medical practitioners were selected who had graduated or had passed at least one medical examination after 1848. In this way we could ensure that we only included doctors who were at the start of their medical and family career around 1850, a year that marked the beginning of our main source of information, the population register. Doctors who started practicing after 1903 were not included, mainly for practical reasons. The same applied to the very small number of female medical professionals who mostly remained unmarried.
The majority of the selected medical practitioners had at least once in their career practiced in the larger cities of Amsterdam, Rotterdam, and The Hague. Around 14% of the medical professionals in our sample had graduated in the decade before 1867 and another 20% even before 1857; these persons thus had completed their medical training before the new legislation concerning medical practice came into effect. Another 10% completed training under the new system but before the year in which medical education became completely localized in the universities. The fourth group (20%) consisted of those medical practitioners that were trained before the new medical ideas and new techniques of hygiene based on it spread throughout the medical profession and the universities. Around 36% had completed their training after 1890, the year that we can consider as the start of the period of biomedicine. Around 62% of the medical sample consisted of men who had graduated as arts; 13% had graduated as doctor of medicine whereas 18% had been trained outside the university (second medical order). Health officers took 7%.
There is a strong overlap between the various categories of medical practitioners that can be distinguished according to their level of qualification and medical training and the period of graduation. This of course complicates any analysis in which we focus on time-effects in the relation between medical training and infant and childhood mortality. Furthermore, a non-negligible number of medical practitioners could be labeled in more than one category, which complicates the analysis further. For example, persons having a qualification as non-university medical practitioner could later on in their life have graduated at the university as arts. We decided to use only their first qualification in our analysis.
The municipal population registers were the main source of information on the birth, death, and marriage of the medical professionals, their spouses, and their children. Municipal population registers combine census listings with vital registration in an already linked format for the entire population from 1850 to 1939. They make it possible to track persons down from household to household and from place to place. They not only contain static information, such as date of birth and sex, but also information on demographic events taking place in the family. Thus, date and place of birth, relation to the head of the household, sex, marital status, occupation, and religion were recorded for each household member (Thomas Reference Thomas and Thomas1938). The life courses of families and individuals can thus, in principle, be followed in detail over a long period of time. Many medical men worked only temporarily in a municipality – especially during the start of their career – and many of them thus had to be followed as they moved to a new place of residence in search of a better position. We thus had to consult population registers for all the places where the medical professionals had resided during their career. We collected information on the complete reproductive history of medical practitioners from the moment of marriage until the wife had reached age 50, whereas the life histories of all their children were followed at least until they had reached age 12. For all members of the family, we collected information on sex, religion, place and date of birth, place and date of death, and place and date of marriage. For those children and parents for which we did not have a date of death, we determined a date of last observation based on the date of last departure from the municipality or on the date of marriage of the child. Children in first and second marriages of the husband were included but children from earlier marriages of the wife were not. Furthermore, the very small number of children born before marriage, even those who acquired a legitimate status later in life by a marriage between the mother and “father” were excluded.
Population registers do not contain information on stillbirths, and deaths during the first days of life were sometimes not recorded completely either. For that reason, the vital registration system had to be checked to find out whether (live and stillborn) children were missing in the population register. As an additional check, sometimes genealogical sources were consulted. All in all, we found information on about 8300 births, of which a date of death could be determined for around 90% – whereas for the rest, we only had a date of last observation.
To find out whether the special medical knowledge and skills over and above their generally higher level of education and higher-level income had an effect on their children’s death risks, we had to compare the life chances of the children of the medical practitioners with those of the population at large. To do this, we used information from the Historical Sample of the Netherlands (HSN), a database with information on the complete life histories of a national random sample of the 1812–1922 birth cohorts in the Netherlands (Mandemakers Reference Mandemakers2001). These sampled individuals are followed from cradle to grave. We use here information on 52,300 children born between 1850 and 1922. Ages at death or, when missing, ages at last observation were based on death certificates, marriage certificates, population registers, personal record cards, and personal record lists of the sampled individuals (Mandemakers Reference Mandemakers2019). As the HSN sample does not contain stillbirths, we excluded them from the sample of the medical practitioners in comparisons with the HSN data.
To ascertain to which social group the families in the control group belonged, we used information on the father’s occupation as given in the birth certificate of the sampled individuals. We coded the occupational titles according to the HISCO classification system (Van Leeuwen and Maas Reference Van Leeuwen and Maas2011; Mandemakers et al. Reference Mandemakers, Muurling, Maas, Van de Putte, Zijdeman and Lambert2013), which was then stratified according to the Social Power coding scheme developed by Van de Putte and Miles (Reference Van de Putte and Miles2005). We also used as alternative classification the condensed HISCLASS system (Van Leeuwen and Maas Reference Van Leeuwen and Maas2011). A large portion of the children (33%) were born to unskilled workers’ families; another 32% to medium-skilled or lower-skilled families; and 14% to farmers’ families.Footnote 4
When medical practitioners practiced in a region where infant mortality was very high, their children also ran higher risks. To take these very large regional differences in account, we linked each individual child from the reference group and the HSN sample to the IMR as observed in their municipality of birth and relevant time period (Ekamper and Van Poppel Reference Ekamper and van Poppel2008). Therefore, we had to eliminate from the medical practitioners sample all children born outside the Netherlands, which resulted in around 6.6 percent of all births.
Tables 1 and 2 compare some characteristics of the (children of the) medical profession with that of the reference group. Table 3 presents some additional characteristics available for the children of medical doctors only. We had information on 52,300 children from the HSN and a total of 8,290 children born to families of medical practitioners in the Netherlands between 1850 and 1922. Infant mortality was 173 per 1000 in the first and 109 per 1000 in the second group and early childhood mortality was respectively 103 and 58 per 1000 one-year-old children. Remarkably, enough boys had a survival advantage in the medical practitioners group in both the youngest age groups. The geographical background of the children of the medical profession was completely different from that of the reference group. Provinces in the western part of the country – the region long characterized by high IMR – were overrepresented in the medical sample (87% versus 53% in the HSN sample).
Table 1. Descriptive statistics of the children of medical practitioners born in the Netherlands and the Historical Sample of the Netherlands, 1850–1922
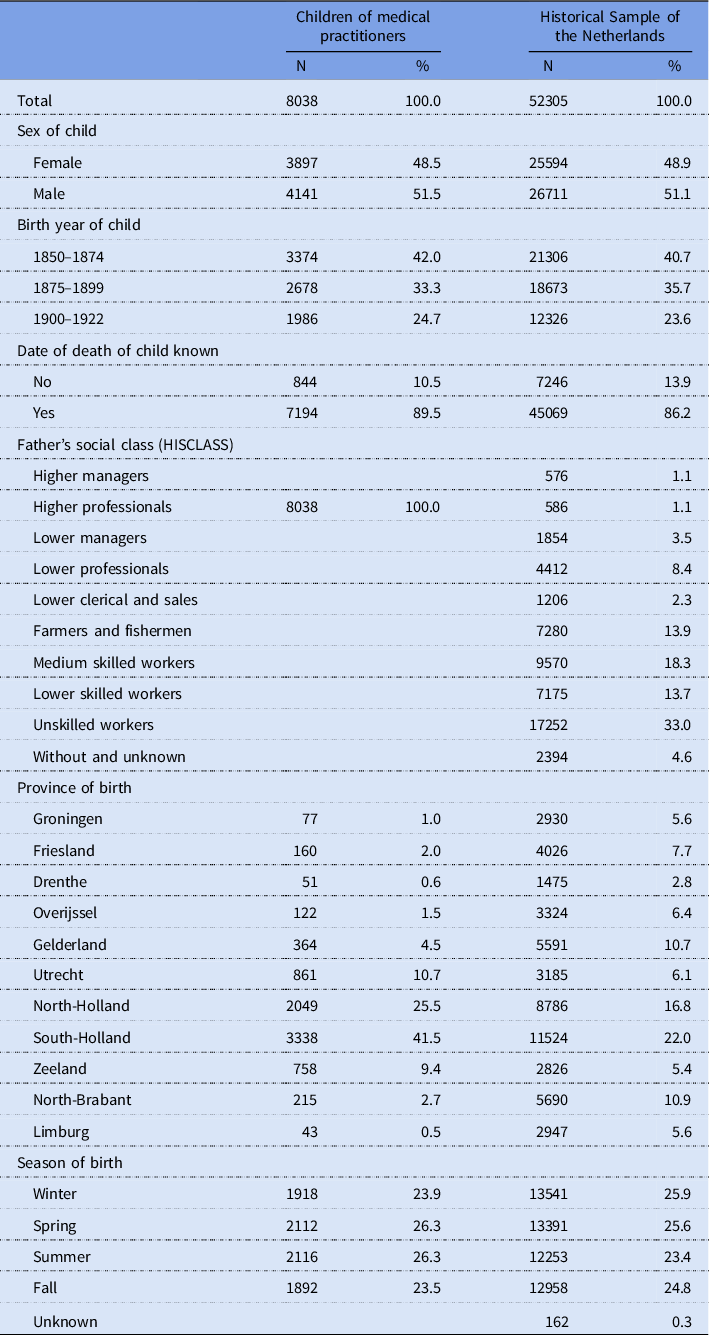
Source: Own medical doctors database, Historical Sample of the Netherlands (HSN).
Notes: Excluding children born abroad and stillbirths; children from medical practitioners were excluded from the Historical Sample of the Netherlands data.
Table 2. Infant and early childhood mortality among children of medical practitioners born in the Netherlands and in the Historical Sample of the Netherlands, 1850–1922
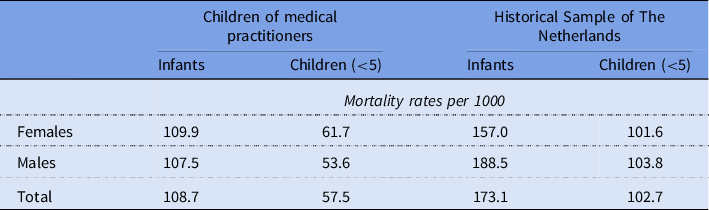
Source: Own medical doctors database, Historical Sample of the Netherlands (HSN).
Table 3. Additional descriptive statistics available for the children of medical practitioners only, the Netherlands, 1850–1922
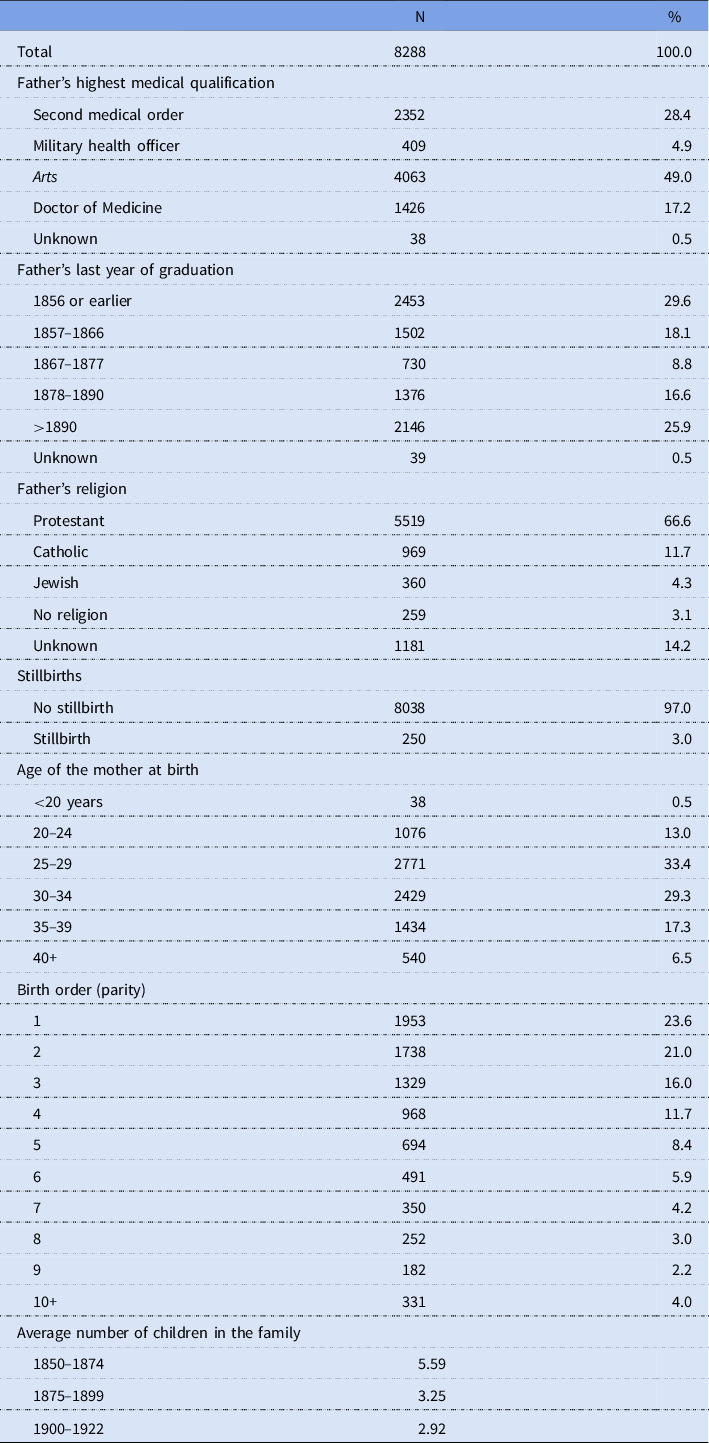
Source: Own medical doctors database.
Note: Including stillbirths and excluding children born abroad.
Comparing the mortality of children of medical practitioners with that of the general population
To answer our first research question on whether medical practitioners were able to lower the level of their children’s mortality below the levels of children coming from other (including socio-economically comparable) groups, we merged the two databases. We estimated death risks for the various social classes, with the medical practitioners group as a whole as one separate class. Compared to other social groups, children born to a medical professional’s family might have had some specific traits (such as age of the mother at birth, religion) which in themselves could have had an effect on the mortality risks of their children. Disentangling these effects is not possible at this time, as this information is not yet available for a large part of the HSN sample. We had information on the age at birth of the father of the children, a variable that shows a very strong overlap with that of the age of the mother at the birth of the child.
We use Cox proportional hazards regression models (Cox, and Oakes Reference Cox and Oakes1984) to compare the death risks of children of medical practitioners with those of the general population and to examine the impact of the father’s medical training on the risk of the child dying. The Cox proportional hazards model is a robust model that can deal with survival time and censored data and allows us to estimate the effects of a set of covariates on the death rate. Since our data on the children of medical practitioners includes all children of the families, children of the same family will share family-related covariates. We take the multilevel nature of these clustered data into account by extending the models to Cox proportional hazards models with shared frailty, which accounts for the unobserved heterogeneity by including the family-level shared frailty (Wienke Reference Wienke2011; Austin Reference Austin2017). The regression equations were estimated separately for the infancy period (from birth through the end of the first year of life) and the childhood period (from age one to age five). There are technical and substantive reasons behind this division. At the beginning of life, genetic and familial factors (the constitution at birth, age of the mother, breastfeeding) are more important as factors affecting the health of children whereas social, economic, and environmental factors (knowledge about health and nutrition, hygiene, economic situation) are more important at later ages. Failing to take this variation into account can produce misleading results (Van Norren and Van Vianen Reference Van Norren and van Vianen1986; Oris et al. Reference Oris, Derosas, Breschi, Bengtsson, Campbell and Lee2004).
The strength of the effect of a variable is expressed in terms of relative risks. For categorical variables, this relative risk expresses the increase or decrease in the death rate compared to the reference categories. For instance, a relative risk of 1.25 for a period of birth implies that for this birth cohort there is a (1.25−1)×100 percent = 25 percent higher death rate than for the reference period of birth.
All models incorporate covariates affecting the mortality risks of the child via maternal factors (indirectly measured via age of the father at the birth of the child), via individual characteristics of the child (sex), and via the climatological (season of birth) and ecological situation in which the child is born (IMR of municipality of birth and province of birth, to capture a more encompassing level of mortality). To separate time trends and spatial differences in infant mortality, we included both the national IMR and the detrended municipal IMR’s by demeaning the municipal IMR’s by the period national averages. To tell whether the effect of the regional IMR variation was weaker for children of medical practitioners we also included interaction of medical practitioners with the regional IMR variation in the models. In addition to that, the year of birth of the child and province of birth were included to take into account other structural environmental developments in the age groups concerned. All variables except IMR have been classified as categorical variables. All models were estimated using R version 4.2.2.
The results of the comparison of the medical profession as a whole with various other social groups are presented in Table 4 for the infancy as well as for the early childhood period. We focus only on those variables that are directly relevant to our research question, that is, the role of social class and time. We compare the medical profession both with all the various other social groups and with the higher socioeconomic groups only. We control for the sex of the child, season of birth, province of birth, and age of the father at birth.
Table 4. Hazard ratios from Cox proportional hazards regression models with shared frailty for survival of children from medical practitioners in infancy (<1 year) and early childhood (1–4 years) compared to the Historical Sample of The Netherlands
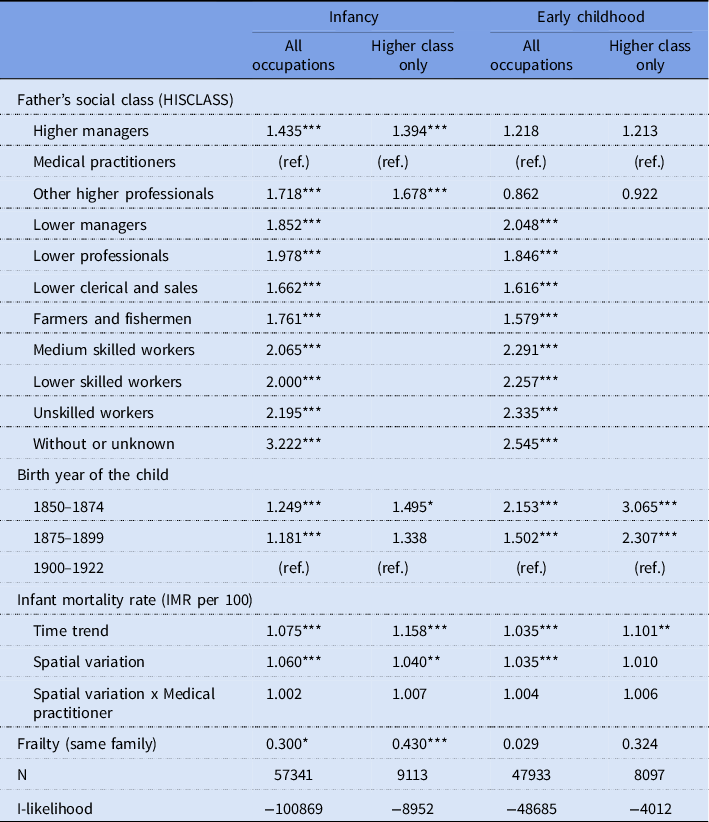
Source: Own medical doctors database, Historical Sample of the Netherlands (HSN).
Notes: All models also controlled for sex of child, season of birth, province of birth, and age of father at birth; children from medical practitioners were excluded from the Historical Sample of the Netherlands data.
* p < .10.
** p < .05.
*** p < .01.
The most important question for us, our first research question, was whether the medical profession had a favorable position compared with other socioeconomic groups. That appeared indeed to be the case as far as infant mortality was concerned. Children born to families of medical professionals did much better than children born in all layers of society – even compared with children born in the group of which they themselves were part, namely the higher professionals (HISCLASS) and the elite (SOCPO). Infants born in these groups (medical doctors’ families excluded) had around 40% (SOCPO classification) and 70% respectively higher death risks than infants born to a medical professional’s family. Children born to workers’ families (whatever their degree of skill) ran the risk of dying within their first year that was in general two times higher than their counterparts born to families of medical professionals. This applied to the HISCLASS (see Table 4) as well as the SOCPO classification (see Appendix Table A1). Children of farmers and fishermen, but also those whose father was member of the middle class, had a 70 to 90 percent higher risk of dying in their first year of life than children born to a medical family. In general, more or less comparable results were found for both social class classifications, delivering proof that it was not the classification that caused this pattern. For early childhood mortality the differences were, as far as the middle and working classes were concerned, not much different. Remarkably, however, the higher professionals and the elite were in this respect on equal footing with the medical practitioners. Excess mortality among low and unskilled laborers and among farmers, however, remained very high.
In line with the expectations, we observed in Table 4 a very strong time effect. Children born during the period 1850–1874 had a 25% higher infant mortality risk than children born after 1900, and the time effect was even higher for the survival of children after age one. This time effect was even stronger if we look at the children from the higher socioeconomic classes only. Thus, the mortality decline had been stronger among children born in a medical practitioner’s family or other higher socioeconomic class families than in the general population. The mortality “regime,” both the infant mortality level time trend and the spatial variation in the infant mortality by place of birth of the child, had very strong and significant effects on the death risks of children, especially for the infants. For example, a HR of 1.075 implies that when the municipal IMR increased by one unit (for example from 20 to 21 per 100 live births) the death risk of children would increase by 7.5 percent. A 5 percentage point increase of IMR in a municipality would thus lead to a 44% (1.0755) increase in the death risk of children. However, the IMR spatial variation effect was not different for children from medical practitioners compared to others (interaction effect HR’s close to 1).
Comparing children’s death risks within the group of medical practitioners
It stands to reason that the training the medical professionals had received and the period in which they had studied determined to a large degree the kind of medical knowledge that they had acquired and whether or not they had systematically been exposed to the latest medical insights and interventions. To answer our second research question, whether these differences between medical practitioners affect the survival chances of their children, Table 5 presents outcomes on the death risks of the children of the various groups of the medical profession. As this part of the analysis is focused only on medical practitioners, we have more information available than was the case in Table 4. In addition to the sex of the child, we were able to use the age of the mother at the birth of the child; and we also controlled for the parity of the child and the religion of the father, two variables that were very relevant in the nineteenth-century Dutch context for the survival prospects of the child (Walhout and Van Poppel Reference Walhout, van Poppel and Walhout2019). We also included children recorded as stillbirths, as around one third of them had been born alive, but had died before a birth certificate had been made up.
Table 5. Hazard ratios from Cox proportional hazards regression models with shared frailty for survival of children from medical practitioners in infancy (<1 year) and early childhood (1–4 years) by fathers’ highest medical qualification and period of latest graduation
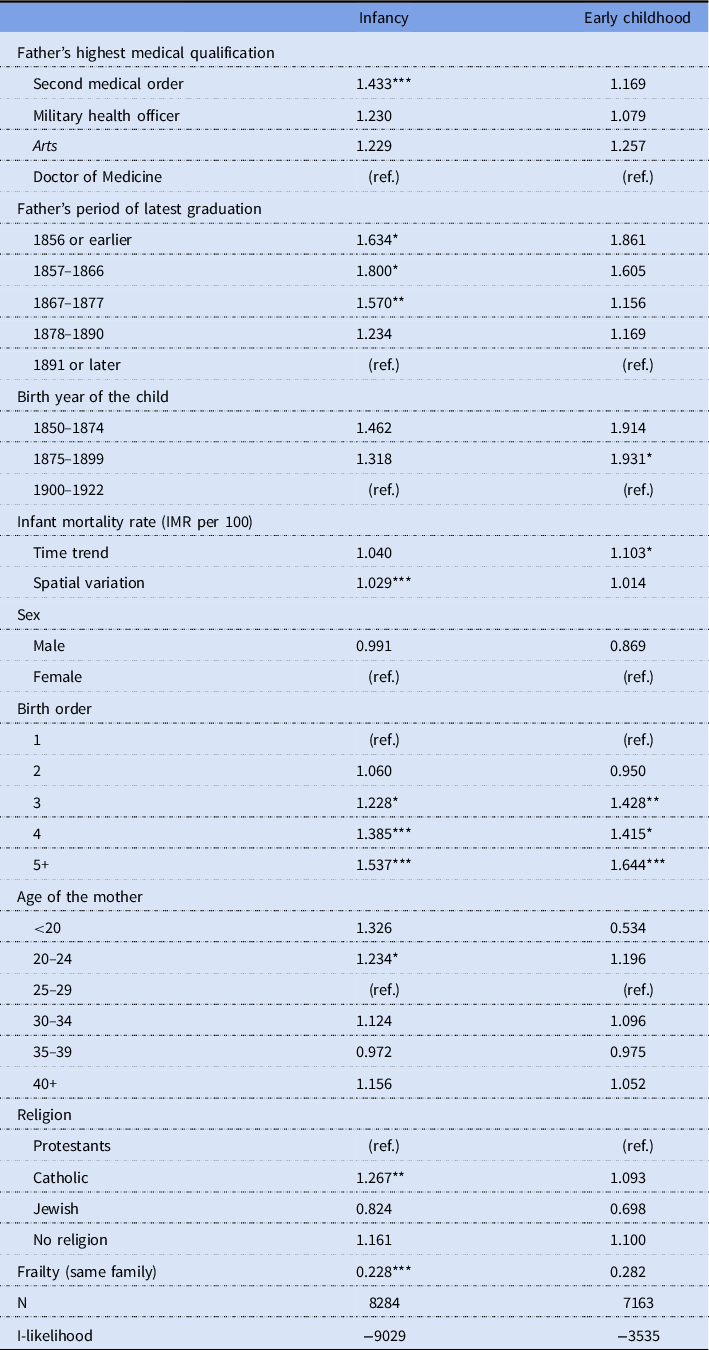
Source: Own medical doctors database.
Note: All models also controlled for province of birth and season of birth.
* p < .10.
** p < .05.
*** p < .01.
Table 5 indeed shows some remarkable outcomes. First of all, the passage of time, measured by the period of birth of the child, is in line with the group of children from the higher socioeconomic classes and stronger than for the group of children as a whole, but except for early childhood mortality of children born 1875–1899 not significant. Secondly, for the survival prospects of the child in its first year of life, which kind of medical qualification their father had certainly played a role: death rates of children from the medical practitioners with the highest medical qualification, the university-trained medical doctors, were lowest, slightly better than those from the arts group and the military health officers, and statistically significant and much better than children of medical practitioners with the lowest medical qualification, the members of the second medical order. One has to realize that children of medical doctors were more frequently born in the earliest period and nonetheless had better survival chances.
The period of graduation of the medical professionals had a strong significant effect on the survival of their children. Children born to fathers who had graduated before 1867 had almost double the death risks in the first year of life compared to children born in families in which the father had graduated after 1890. Again, a relatively strong effect on the survival of infants was found of the local mortality regime. A HR of 1.029 implies that when IMR increased by one unit, the death risk of children of medical practitioners would increase by 2.9 percent; an increase in IMR of 11 points, which could happen when, for example, in 1841–1860 a doctor moved from The Hague to Gouda, would theoretically increase the death risk of a medical practitioner’s child by 37% (1.02911).
For children who had survived age one, effects of medical qualification were in the same direction but much smaller than for infants. Graduation period effects for children whose fathers graduated before 1867, with much higher death risks, were similar to infants. However, none of the effects for early childhood mortality at age 1–4 years were significant. It is clear that Table 5 gives a distorted picture of the effects of medical training on the mortality of infants and children. That is due to the strong interrelatedness between the level of medical qualification (after 1867, all new medical professionals were university trained), the period in which the medical professional graduated (all new medical professionals from 1867 on have the same qualification) and the period of birth of the child. In addition, the more recently children were born, the higher the chance that they were born to families of recent graduates, that is, in the university-trained medical profession. Given the general time trends of IMR and ECMR in the Netherlands, this has an effect on the outcomes as well. It is hard to find a solution for this problem. One way to counter it, at least partially, is to do a sensitivity analysis by repeating the analysis by alternately excluding the period of birth of the child and the period of graduation to test for the impact of the omitted variables on the effects of the remaining variables. The results of this exercise are given in Table 6.
Table 6. Hazard ratios from Cox proportional hazards regression models with shared frailty for survival of children from medical practitioners in infancy (<1 year) and early childhood (1–4 years) by fathers’ highest medical qualification and period of latest graduation, with exclusion of one of the time variables
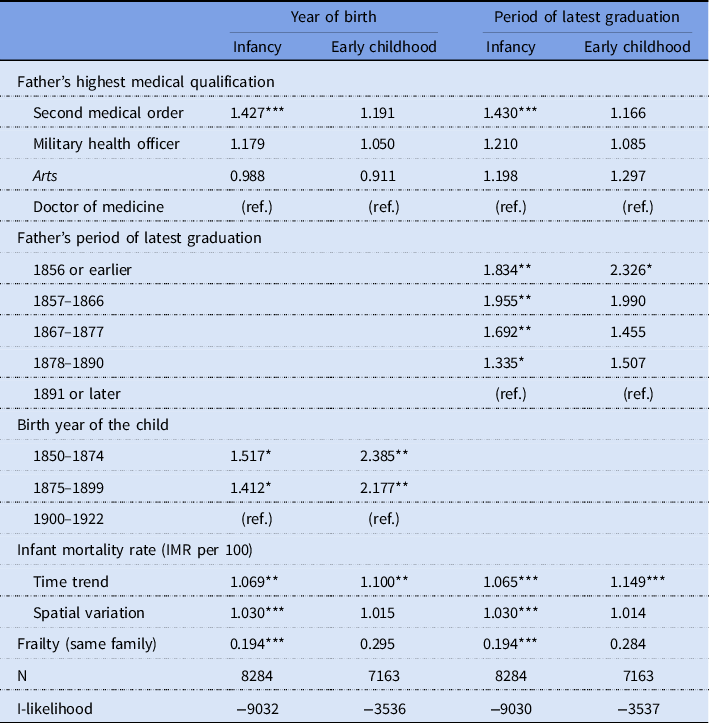
Source: Own medical doctors database.
Note: All models also controlled for sex of child, birth order, age of the mother, religion, season of birth, and province of birth.
* p < .10.
** p < .05.
*** p < .01.
When the period of graduation is excluded, the level of medical qualification still shows an effect: children of medical doctors with their purely theoretical medical training still show higher and statistically significant survival prospects in their first year of life than children from the second medical order. Children from health officers still show an unfavorable position, but children from artsen did different and had even a smaller though not statistically significant HR. Thus, if only the birth year of the child was entered into the equation instead of period of graduation, period of birth had much stronger effects on the death rates of infants and children, capturing part of the left out period of graduation effect from the model in Table 5; children born before 1875 had a 50% higher death risk in their first year of life than that of children born after 1899. For death risk in early childhood, the effects were even stronger. The effect of the local mortality regime remained at the same level.
If alternately the period of qualification was entered into the equation instead of the birth year of the child, the effects of the qualification period were much stronger and in the expected direction. The more recent the study period of the medical practitioners, the lower the chances of their children dying in the first year of life and in the early childhood period. Compared with the children of medical practitioners graduating in 1891 or later, the death risks of children of which the fathers had graduated before 1867 were almost double. Children of doctors graduating in the years 1867–1877 did do slightly better. In general, for infants the difference between the first and last period of graduation was smaller than for children in the early childhood ages. Thus, as medical professionals were able to study medicine in a period in which biomedicine was gaining ascendancy over traditional medicine, their children were directly profiting from this development. All in all, the sensitivity analyses confirm the effects of the period of birth of the child and the period of graduation from Table 5.
Discussion
Our statistical analysis has shown that the offspring of medical practitioners as a whole did have better survival prospects than children born to families without a father with a medical background. This also applied when the death risks of the children of medical practitioners were compared with those of comparable high-status groups. This is the more telling because medical practitioners were overrepresented in regions with high infant mortality levels. The results of a more refined analysis within the medical profession provided evidence that when medical men had effective medical knowledge, measured by the period of graduation and the highest level of medical training reached, the positive effects on the survival of their children were stronger.
For a part the favorable position of the children of the medical doctors was due to the fact that the income and wealth of the university-trained doctors was higher than that of the second medical order (Van Lieburg Reference Van Lieburg1983). This last group, in particular when living in the countryside, had to be content with a “simple life style and a low income.” The medical doctors indeed generally lived in better quality housing: they were rarely plagued by overcrowding, lack of ventilation, inadequate water supply and sewage, and bad arrangements for cooking and storage of food. Servants could keep their homes clean, risks of transmission were lower as overcrowding was less common, and they were able to isolate the sick with lower risks of smallpox, typhus, typhoid, and phthisis as the result (Burnett Reference Burnett, Schofield, Reher and Bideau1991).
It was not only infant mortality that was reduced in doctor’s families; there was also a decline in child mortality across father’s period of graduation. National data confirm that at ages above year one, mortality decline was strong and started even earlier than mortality in the first year of life. Acute respiratory diseases, convulsions (usually the effect of a respiratory or gastrointestinal illness), acute digestive diseases (such as enteritis and diarrhea), and infectious diseases such as measles, scarlet fever, diphtheria, whooping cough, smallpox were the dominant causes of death of children aged 1–14 years. These were also the causes that were responsible for the strong decline of child mortality between 1875 and 1920 (Wolleswinkel-Van den Bosch et al. Reference Wolleswinkel-Van den Bosch, Looman, van Poppel and Mackenbach1997). Direct effects of medical practice partly contributed to mortality decline in this age group. Smallpox had been greatly reduced through vaccination since the beginning of the 19th century and became more effective when in the 1870s a system of compulsory vaccination became effective. Immunization against diphtheria became available in the 1890s. Together with tracheostomy – that is, creating an opening in the neck to place a tube into the child’s windpipe – it substantially reduced mortality from diphtheria in the first decades of the 20th century (Van Wijhe et al. Reference Van Wijhe, McDonald, de Melker, Postma and Wallinga2016). In the 1900s, the ability of the medical profession to diagnose illnesses correctly was aided as chemical and bacteriological tests for micro-organisms that had been identified as disease-causing became available. Yet it was mainly preventive measures and recommendations to treat sick children that reduced the death risks of young children. Doctors strongly recommended to keep the child from being exposed to infective organisms, and to avoid contacts with sick people and their clothing. This implied isolation and quarantine. For all these causes of death we found indeed evidence in our qualitative sources that the medical doctors in our study recommended and applied these measures.
A factor that might have been relevant for the lower mortality of doctors’ children, in particular death from childhood infections, is fertility control. When families became smaller, the likelihood of transmission of infection within the family became smaller, which reduced the incidence of infectious diseases. It probably also reduced case fatality, because a lower force of infection led to a higher age of infection, when children were less vulnerable. Moreover, chances were higher that children were breastfed for longer periods. For the medical practitioners, we controlled the models for the effect of parity and it turned out that indeed the first and second born children were less vulnerable than higher parity children.
Preston and Haines (Reference Preston and Haines1991: 208) explained the absence of a substantial mortality advantage of children of medical practitioners in the late nineteenth century in the USA by the fact that “Infectious disease processes, which were principally responsible for the foreshortening of life, were still poorly understood by most physicians; few effective technologies based upon the new understandings had been developed; those technologies which were developed had been slow to diffuse; and the assumption of public responsibility for such private matters as child death was still incomplete and often ineffective.” The Dutch case proved that, indeed, when the above-mentioned conditions were met, that is, in the last decades of the nineteenth and the first decades of the twentieth century, the children of medical doctors were in a more favorable position. In the 1890s Pasteur’s new techniques of hygiene began to spread throughout the population: a light diet consisting entirely of milk during the first months of its life, prohibition of feeding porridge, daily baths, the use of boiled milk and boiled water to make baby food, and washing hands before beginning to breastfeed (De Knecht-van Eekelen Reference De Knecht-van Eekelen1984: 90–165; Morel Reference Morel, Schofield, Reher and Bideau1991: 211; Van Heteren Reference Van Heteren, de Blécourt, Frijhoff and Gijswijt-Hofstra1993).
However, even before that time, children of Dutch doctors fared better. Morel (ibid.: 196) argued that even before the Pasteurian revolution in medicine, medical men began to intervene in the area of childbirth, early infancy and the care of sick children, leading to such innovations as stricter hygiene, more regular feeding schedules, discouragement of swaddling, the propagation of vaccination, and the gradual introduction of artificial foods in order to avoid the problems associated with abrupt weaning (ibid.: 204–05). Given the outstanding role that medical practitioners played in the propagation of these cultural changes, and their involvement in private societies and welfare clinics, which propagated modern behavior among the population, and given their role as writer of treatises on infant care and personal hygiene, it is likely that these advocates of the medical profession also adhered to these principles in their home environment (De Knecht-van Eekelen Reference De Knecht-van Eekelen1984; Van Heteren Reference Van Heteren, de Blécourt, Frijhoff and Gijswijt-Hofstra1993).
Children born to families of doctors who had received their training after 1890 – besides the effect of being born late in the period studied – had better chances of surviving infancy and childhood than the offspring of doctors who had received training earlier in the nineteenth century. Many doctors adopted the new insights and new methods regarding the health of children rather late in the game. Digby (Reference Digby1994) argued that these new ideas not only ran counter to the intellectual traditions of the doctors, but, particularly for older practitioners, might also have impinged on their self-image as skilled healers. A clear example of such an attitude can be found in the autobiography of the country surgeon Jan Adam Geill, who was part of our sample. He explained his decision to retire in 1909 after having practiced for more than 50 years as follows: “The many worries that I always had about my patients and the sleepless night that I had to experience as an obstetrician were sufficient reasons to bless the moment that my career ended. The more so because contact with my three sons caused a complete loss of my former firm self-confidence, and for that reason it was high time to resign my office. They were experienced in percussion, auscultation, chemistry and the microscope, enabling them to identify illnesses mathematically and to link a certain rock-solid medical procedure to it. These splendid sciences were completely unfamiliar to me at that time; my own routines in treating patients now filled me with distrust and I therefore considered it advisable to retire” (Geill Reference Geill1909: 27).
A medical practice could hardly function for an unmarried man, for the role that the doctor’s wife played in the daily household and medical routine was extremely important. In very few doctor’s families the doctors’ spouse worked outside the house. Whereas during the period 1812–1910 less than half of lower-skilled and unskilled workers in and outside the agricultural sector stopped working at the time of marriage around 90 percent of women marrying a husband from the highest social class (such as the medical doctors) did so (Van Poppel et al. Reference Van Poppel, van Dalen and Walhout2009). Of course this could have had survival advantages for the child. The uninterrupted presence of the mother would allow her to breastfeed her children and also had a positive effect on hygiene, such as hand-washing, cleaning of the house, the quality of food served to children, and prevention of accidents at home (Preston, and Haines Reference Preston and Haines1991: 27–36; De Beer Reference De Beer2001: 75). Most medical practitioners will have been away from their family for most of the daylight hours, and the care of their children was thus almost entirely in the hand of the mother and servant(s). Thus, the domestic health practice of individual women was probably a more salient factor in children’s mortality than the presence of a father who happened to be a healthcare practitioner. Wives might even have viewed their husband as ill-qualified for dealing with their own offspring, while in turn, medical practitioners viewed children, including their own, as particularly difficult subjects. In many historical and developing countries there is a much greater maternal than paternal involvement in children’s health-related care (Cleland Reference Cleland2010). Qualitative sources such as diaries and autobiographies written by children and wives of medical practitioners also provide proof of that. An example is the case of Christina Hendrika Josephina Sloot, the wife of Gerardus Petrus Timotheus Kortenhorst (1846–1903), a doctor in our sample. His son described his mother’s role in the following way. “My mother was (…) a cordate doctor’s wife, who did not mind - when my father was far away in the country assisting a woman in childbirth - to observe his office hours and, if necessary, to bandage a wound. Furthermore, she and not my father was the family doctor for the children. So it happened that we got through measles, chicken pox and a mild case of scarlet fever without my father knowing anything about it…” (Kortenhorst, Reference Kortenhorsts.a.: 213).
Our study focused for a large part on a region that for a long period was characterized by very high infant mortality. That made it also for medically educated people difficult to escape the high death risks, as became visible in the strong effect that the local infant mortality level had on the death risks of the doctor’s children. After all, in a mortality regime dominated by variation in the incidence of infectious diseases, location in a spatially structured disease environment (presence of effective sewerage, treated water) mattered more for mortality outcomes than the advantages or disadvantages dependent upon the status of an individual. Because medical practitioners intermingled freely with their patients and other lower strata members such as servants, they could not stay isolated from them, the consequence of which could be that the mortality risks of their children were seriously affected. This might in particular have played a role in the higher mortality of the non-university medical practitioners.
Mackenbach (Reference Mackenbach2020: 107) argued that the population health impact of medical care is determined by three factors. The first is the availability of effective treatments, as resulting from scientific breakthroughs and other more general advances. The second is coverage of the relevant patient groups, as determined by the diffusion of the innovation among medical professionals and by the patients’ access to the healthcare system. The third is the quality of application, which is dependent on training, experience and guideline adherence of professionals and on patient compliance. Over time and place, each of these three factors have changed. In particular the second factor has been important in downplaying the role of medicine in the decline in infant and child mortality. Medical practitioners could in principle give valuable preventive hygienic advice based on the practical experience that wrong feeding patterns, impure drinking water, absence of vaccination, untidiness, and poor housing conditions went hand in hand with diseases. The medical culture strongly opposed the kinds of healthcare that were popular among the population at large, such as, trusting on the assistance of witchdoctors, patron saints, and the use of home remedies. Yet very often, even when children were quite sick, parents did not appeal to medical practitioners for help (Rutten Reference Rutten1986: 256–58). Many parents seriously doubted whether medical treatment for infants could have any positive effects, as their experience showed that it had had little success in curing infants of diseases. The lower classes in the countryside in particular were convinced that “nothing can be done for sick children.” This lack of confidence stemmed in part from the fact that many parents were unfamiliar with how doctors worked. “After all, the poor little sheep cannot tell what is hurting him” and “They do not have a hatch in their body through which the doctors can see what is hurting them, so [even] doctors can only guess what is wrong with the child.” Thus, it is no wonder that before they called the doctor, parents preferred to call upon family members, neighbors and friends who had experience with sick children (Barentsen Reference Barentsen1922; Franken Reference Franken1929: 6).
Acknowledgments
We are very grateful to Prof. Mart van Lieburg for providing us with the medical education data from his database of the medical professions in the Netherlands in the period 1450–1950.
Appendix A
Table A1. Hazard ratios from Cox proportional hazards regression models with shared frailty for survival of children from medical practitioners in infancy (<1 year) and early childhood (1–4 years) compared to the Historical Sample of the Netherlands
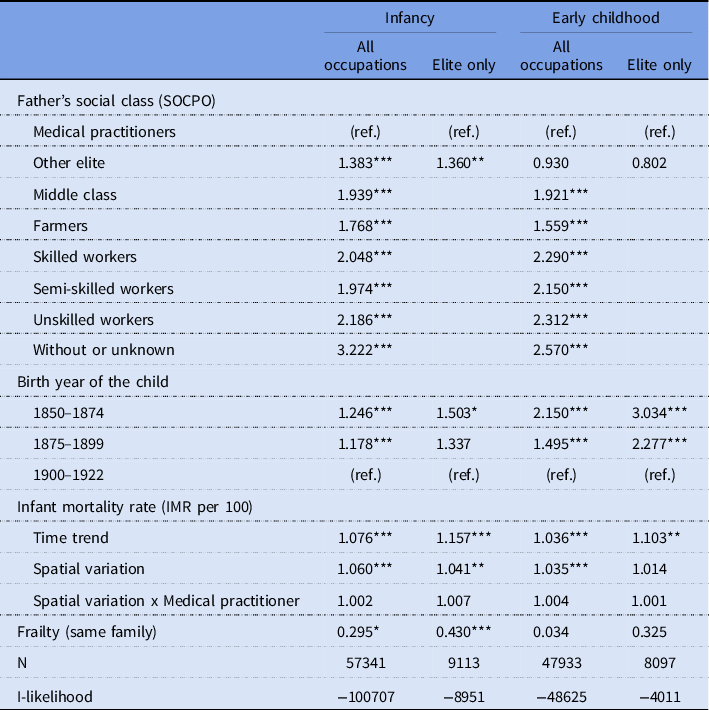
Source: Own medical doctors database, Historical Sample of the Netherlands (HSN).
Notes: All models also controlled for sex of child, season of birth, province of birth, and age of father at birth; children from medical practitioners were excluded from the Historical Sample of the Netherlands data.












