Abstract
Resistance to chemotherapy is a principal problem in the treatment of small cell lung cancer (SCLC). We show here that SCLC is surrounded by an extensive stroma of extracellular matrix (ECM) at both primary and metastatic sites. Adhesion of SCLC cells to ECM enhances tumorigenicity and confers resistance to chemotherapeutic agents as a result of β1 integrin-stimulated tyrosine kinase activation suppressing chemotherapy-induced apoptosis. SCLC may create a specialized microenvironment, and the survival of cells bound to ECM could explain the partial responses and local recurrence of SCLC often seen clinically after chemotherapy. Strategies based on blocking β1 integrin-mediated survival signals may represent a new therapeutic approach to improve the response to chemotherapy in SCLC.
Similar content being viewed by others
Main
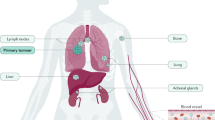
Lung cancer is the most common fatal malignancy in the developed world. Small cell lung cancer (SCLC), which constitutes 25% of all lung neoplasms, is characterized by early and widespread metastases. Etoposide is the most effective drug for use against SCLC and is commonly used in combination with doxorubicin and cyclophosphamide or platinum-based drugs1. However, despite initial sensitivity to chemotherapy, this tumor almost invariably relapses and becomes resistant to further treatment; thus, the patient 2-year survival rate remains less than 5% (ref. 2). New therapeutic strategies are urgently needed, and these will most likely result from a better understanding of the cell biology of SCLC.
The integrin family of receptors represents the main extracellular matrix (ECM) receptors. The growth and survival of untransformed epithelial and endothelial cells requires adhesion to ECM proteins. When displaced from ECM, these cells undergo apoptosis. This phenomenon is called 'anchorage dependence'. After being activated by an ECM ligand, integrins stimulate intracellular signals, which can prevent entry into the cell death program3,4. Integrins regulate many intracellular signaling pathways, such as tyrosine phosphorylation and inositol lipid metabolism5. This can lead to negative regulation of interleukin-1β converting enzyme expression6, an essential effector of apoptosis. A characteristic feature of cancer cells is their ability to grow without the requirement of adhesion to ECM. This correlates closely with tumorigenicity in animal models7. Cytoplasmic oncogenes may provide a constitutively activated signal, usually initiated by ligand-bound integrins, thereby overcoming anchorage dependence. Anchorage-independent growth is seen in vitro in SCLC cells, which grow as non-adherent, free-floating aggregates.
Some forms of chemotherapy exert their cytotoxic effects mainly by inducing apoptosis8,9. Tumor mass is a balance between cell proliferation and cell death (necrosis and apoptosis), and factors affecting this balance have a profound effect on tumor growth. Regulation of apoptosis in tumor cells remains poorly understood. However, the level of protein tyrosine kinase (PTK) activity may determine whether SCLC cells survive and proliferate or die by apoptosis10. SCLC cell growth in vitro may be sustained by multiple autocrine and paracrine loops involving calcium-mobilizing neuropeptides11. This discovery led to the development of agents to block these growth loops for use in clinical trials in patients with SCLC, for example, neuropeptide receptor antagonists such as [D-Arg6, D-Trp7,9, NmePhe8]-substance P (6–11)(ref. 12) and monoclonal antibodies against the growth factor gastrin-releasing peptide13. The aim of our study here was to determine if the local environment of SCLC cells in vivo could provide a survival signal, or block a death signal, thereby accounting for the protection of SCLC cells from chemotherapy-induced apoptosis.
SCLC cells are surrounded by ECM proteins
We determined the ECM composition of unselected SCLC specimens from pathology files by immunohistochemical staining for fibronectin (Fn), laminin (Ln), collagen IV and tenascin. Normal areas of the lung showed Ln and collagen IV localized to the basement membranes of alveoli, septae, blood vessels and bronchial glands, whereas Fn staining showed diffuse weak positivity throughout the pulmonary interstitium. No tenascin immunoreactivity was seen in normal lung. In contrast, extensive (> 50% of section area) Fn, collagen IV and tenascin staining were seen in 56%, 87% and 61% of tumors, respectively, with focal areas of immunoreactivity seen in another 35%, 9% and 39% of sections, respectively (Table 1). Fn, collagen IV (Fig. 1 ) and tenascin (not shown) were expressed mainly in areas of reactive host connective tissue, which were present as extensive areas of scarring or as stromal bands delineating packets of invasive tumor cells. Intracellular staining for Fn and Ln was seen in 26% and 16% of tumors, respectively (Fig. 1 and Table 1). In SCLC sections, the basement membranes of the alveoli were considerably thickened compared with adjacent uninvolved areas, with increased expression of Fn, Ln and collagen IV. In three cases in which matched metastatic lymph nodes were available for examination, Fn, collagen IV and tenascin immunoreactivity was as extensive there as in the primary tumors (data not shown). Thus, in vivo, SCLC cells exist in an ECM-rich environment.
SCLC cells adhere to ECM proteins through β1 integrins
We next determined the physiological relevance of these in vivo results using the classical SCLC cell lines H69, H345 and H510. Expression of individual integrin subunits on SCLC cells was homogeneous with an almost unimodal distribution. The main beta integrin expressed was β1. The alpha integrins were those known to be involved in adhesion to collagen and Ln; (α2β1, α3β1 and α6β1) and Fn; (α3β1 and αvβ1)(refs. 14–16; Table 2). These results were in agreement with those described in other SCLC cell lines17. In keeping with this, H69 cells adhered to Fn, Ln and collagen IV in a concentration-dependent manner (data not shown). Adhesion induced a profound change in SCLC cell morphology, with reorganization of the actin cytoskeleton. The cells adopted a flattened conformation and formed actin-rich filopodia (Fig. 2a), giving the appearance of differentiation to a neuron-like morphology. However, adhesion to ECM proteins had no effect on the expression of neuroendocrine markers chromogranin A, dopa-decarboxylase and neuron-specific enolase (results not shown). Adhesion was stimulated by 1 mM Mn2+ (similar results were seen with 1 mM Mg2+) and was inhibited by the function-blocking β1 antibodies P5D2 and 4B4 (Fig. 2b; similar results were obtained in H510 and H345 cells). These results demonstrate that SCLC cells adhere to Fn, Ln and collagen IV in a mostly β1 integrin-dependent manner.
a, Adhesion of H69 SCLC cells to ECM. Confocal fluorescence microscopy of cells stained with rhodamine phalloidin after 4 h of attachment to poly-L-lysine (left) or collagen IV (right). b, Effect of Mn2+ and the β1 function-blocking antibodies (β1-ve Ab) P5D2 or 4B4 on SCLC cell adhesion to laminin (Ln) fibronectin (Fn) and collagen IV (C IV). –, negative control. Data represent the mean ± s.e.m. of three to six independent experiments done in quadruplicate on duplicate plates. c, Effect of ECM proteins on chemotherapy-induced apoptosis in SCLC cells. SCLC cells were seeded in the presence of pre-coated fibronectin (P●laminin (▪) or collagen IV (♦) or in the absence of ECM (□), then increasing concentrations (horizontal axes) of chemotherapeutic agents were added. Apoptosis was determined by acridine orange or Giemsa staining. Each point represents the mean ± s.e.m. of two to four independent experiments. d, The effect of etoposide on H69 SCLC cell apoptosis in the presence of no coating matrix (–), poly-L-lysine (PLL) or collagen IV in the presence or absence of the function-blocking antibody P5D2. Each bar represents the mean ± s.e.m. of three independent experiments.
ECM protects SCLC cells from chemotherapy-induced apoptosis
The addition of the chemotherapeutic agents doxorubicin, CIS-4-sulfoethylthio-cyclophosphamide (cyclophosphamide) and etoposide induced a concentration-dependent increase in SCLC cell apoptosis, as judged by morphology, electron microscopy, acridine orange/propidium iodide staining and immunoassay of cytoplasmic histone-associated DNA fragments. Adhesion of SCLC cells to Ln, Fn or collagen IV substantially protected H69, H345 and H510 cells against the apoptosis induced by these chemotherapeutic agents, reducing both the percentage and number of cells undergoing apoptosis (Fig. 2c). For example, in H345 cells, in response to 50 μM etoposide, Fn reduced apoptosis from 75% to 14%, which corresponded to a reduction from 1.05 × 105 to 0.33 × 105 apoptotic cells (similar results were obtained with cis-platinum). Nonspecific adhesion of H69 cells to poly-L-lysine did not protect cells from etoposide-induced apoptosis. Furthermore, the addition of the β1 function-blocking antibody P5D2 abolished the ECM-mediated protection from etoposide-induced apoptosis (Fig. 2d). The addition of conditioned medium (from SCLC cells grown in the presence of collagen IV or Fn) did not protect SCLC cells adhered to poly-L-lysine from chemotherapy-induced apoptosis (data not shown). Thus, ECM-mediated protection from apoptosis was not mediated by the release of soluble autocrine growth factors. Therefore, ECM proteins acting through β1 integrins protect SCLC cells from chemotherapy-induced apoptosis.
In liquid culture, the presence of Fn stimulated a 150–200% increase in SCLC cell number. Furthermore, Fn also reduced the cytotoxicity of cyclophosphamide and cis-platinum in H345 cells (50% inhibitory concentration (IC50):1.0–200 μM and 92–450 μg/ml, respectively; (n = 3; Fig. 3a). Similarly, the presence of Ln, Fn or collagen IV substantially reduced the sensitivity of all SCLC cell lines to the cytotoxic agents doxorubicin, cis-platinum, etoposide and cyclophosphamide (results not shown). Adhesion to Fn, Ln and collagen IV had no effect on cell–cell aggregation up to 24 hours, but at later time points, a small increase in cell aggregation was seen, which was abolished by function-blocking β1 antibodies. Treating SCLC cells with either β1 function-blocking or -stimulating antibodies in the absence of ECM had no effect on SCLC cell growth, cell–cell aggregation or chemotherapy-induced apoptosis (data not shown). Tumor and transformed cells, including SCLC, are able to form colonies in agarose medium. Indeed, there is a positive correlation between the cloning efficiency of cells and the histological tumor involvement of SCLC cells18. The presence of Fn or Ln in the clonogenic assay caused a 200–300% stimulation of H69 cell colony formation (Fig. 3b). Further addition of neuropeptide growth factors bradykinin (10 nM) and galanin (50 nM) caused an additive effect. Moreover, Fn also reduced the cytotoxicity of etoposide in the clonogenic assay in H69 cells (IC50: 3.2–9.3 μg/ml; n = 2; Fig. 3c). These data indicate that in vivo β1 integrin-mediated adhesion of SCLC cells to ECM proteins around the tumor is associated with enhanced tumorigenicity and increased resistance to standard chemotherapeutic agents.
a, The chemosensitivity of H345 SCLC cells to increasing concentrations (horizontal axes) of chemotherapeutic agents was assessed in the presence (●) or absence (□) of fibronectin. Live cells were assessed by trypan blue exclusion. Data represent mean ± s.e.m. of three independent experiments done in quadruplicate in duplicate plates. b, The effect of ECM proteins laminin (Ln) and fibronectin (Fn) on H69 SCLC cell colony formation in the presence of bradykinin (BK) or galanin (Gal). The clonogenic assay was done in triplicate in two independent experiments. Data represent mean ± s.d. c, Inhibition of H69 cell colony formation by increasing concentrations (horizontal axis) of etoposide, in the presence (●) or absence (□) of fibronectin. Data represent mean (of two independent experiments done in triplicate) ± s.d.
PTK activation prevents chemotherapy-induced caspase activation
PTK activity in SCLC cells may be essential in determining whether they survive and proliferate or die by apoptosis10. Adhesion of H69 SCLC cells to Fn stimulates PTK activity in both basal cells (not treated with etoposide) and etoposide-treated cells. This effect was completely blocked by pretreatment with tyrphostin-25 (a selective PTK inhibitor) or a function-blocking β1 antibody (Fig. 4a). The presence of Fn reduced the cytotoxicity of H69 SCLC cells to etoposide, shifting the concentration-response curve to the right (IC50: 2.2–25 μg/ml). This effect was blocked by the addition of function-blocking β1 antibodies ( Fig. 4b). Addition of tyrphostin-25 (25 μM) also blocked the Fn-mediated reduction in cytotoxicity shifting the concentration-response to etoposide back to the left. As a consequence, in the presence of tyrphostin-25, the IC50 for etoposide was the same (5 μg/ml) in the presence or absence of ECM (Fig. 4b). Similar results were obtained with Ln and collagen IV (results not shown). The addition of 25 μM tyrphostin-25 to SCLC cells for 24 hours had no effect on SCLC cell adhesion to ECM (data not shown). These data show that β1 integrin-dependent resistance to chemotherapy is mediated by a PTK-dependent mechanism.
a, The effect of fibronectin on tyrosine phosphorylation in SCLC cells. H69 SCLC cells were seeded in the presence or absence of fibronectin as indicated with or without the function-blocking β1 antibody 4B4 (β1-ve Ab), tyrphostin-25 (Tyrph) or etoposide. Cell lysates were assessed by western blot analysis with antibodies against phosphotyrosine (PY20 and 4G10). The gel is representative of three independent experiments. Left margin, molecular weight markers in kDa. b, H69 SCLC cells were seeded in the absence (□) or presence of fibronectin alone (●) or fibronectin plus a function-blocking β1 antibody (♦ and discontinous line). Etoposide (concentrations, horizontal axis) and diluent (upper) or tyrphostin-25 were added, then cells were aspirated and counted. Cell number in the absence of etoposide for each condition was considered 100%. Data represent the mean ± s.e.m. of three independent experiments done in quadruplicate in duplicate plates. c, Effect of fibronectin on etoposide-induced apoptosis and caspase-3 activation. H69 cells were seeded, and etoposide, β1 blocking antibody (β1-ve Ab), tyrphostin, z-VAD or sodium orthovanadate (Na2VO3) were added to each well. Upper, apoptosis, determined by acridine orange staining; data represent mean (of three independent experiments done in triplicate) ± s.e.m. Lower, western blot analysis with antibody against pro-caspase 3; blot is representative of a parallel sample. Left margin, molecular weight markers in kDa. d, Effect of fibronectin on topoisomerase IIα (Topo II) expression in the presence and absence of etoposide and tyrphostin. Upper, western blot analysis with antibody against human topoisomerase IIα. Left margin, molecular weight markers in kDa. Lower, decantenation assay of topoisomerase IIα activity; NW, high-molecular-weight interlocking kDNA network; MC, decantenated individual DNA mini circles. Gels shown are representative of two independent experiments done in duplicate.
Several of the chemotherapeutic agents used here, including etoposide, function specifically by inhibiting the re-annealing action of topoisomerse II, resulting in DNA damage and apoptosis19. Caspase-3, one of the essential mediators of apoptosis, is activated by proteolytic cleavage of pro-caspase-3 (ref. 20). After being activated, caspase-3 cleaves the chaperone inhibitor of caspase activated deoxyribonuclease, releasing the DNAase activity, which causes DNA fragmentation in nuclei21. In H69 SCLC cells, the etoposide (25 μg/ml)-induced pro-apoptotic effect and pro-caspase-3 cleavage was completely blocked by co-incubation with either the tyrosine phosphatase inhibitor sodium vanadate (200 μM) or the broad-spectrum caspase inhibitor z-Val-Ala-DL-Asp-fluromethylketone (z-VAD; 100 μM) without affecting the level of pro-caspase-3 expression (Fig. 4c). In addition to blocking pro-caspase-3 cleavage, Fn reduced both the percent (43% to 11%) and number (4.8 × 104 to 1.45 × 104) of cells undergoing apoptosis in response to 25 μg/ml etoposide. Furthermore, the Fn-mediated protection of H69 SCLC cells from etoposide-induced apoptosis and pro-caspase-3 cleavage was abrogated by either the addition of a function-blocking β1 antibody or the PTK inhibitor tyrphostin-25 (25 μM). This tyrphostin effect was blocked by 100 μM z-VAD without affecting the level of pro-caspase-3 expression. The function-blocking β1 antibody had no effect on etoposide-induced apoptosis in the absence of Fn. Apoptosis induced by DNA damage can be suppressed by Bcl-2 (ref. 22) through a mechanism that prevents caspase-3 activation23. Adhesion to Fn or treatment with etoposide has no effect on the level of Bcl-2 expression in SCLC cells (data not shown). Adhesion to Fn or treatment with tyrphostin-25 did not substantially alter either the expression or activity of topoisomerase II in basal or etoposide-treated cells (Fig. 4d). Furthermore, treatment with z-VAD did not affect etoposide-inhibition of topoisomerase II (results not shown). Thus adhesion to Fn through β1 integrins protects SCLC cells from etoposide-induced caspase-3 activation and apoptosis by activating PTK signaling downstream of DNA damage. In addition, z-VAD prevents apoptosis at a point downstream of DNA damage, preventing activation and cleavage of pro-caspase-3 by upstream caspases.
Discussion
This study shows that SCLC, in vivo, is surrounded by an extensive stroma of ECM at both primary and secondary metastatic sites. This stroma contains, in part, Fn, Ln, collagen IV and tenascin. The extent of ECM deposition around SCLC cells in vivo has not generally been appreciated. The origin of ECM proteins in SCLC stroma is unclear, but may be the consequence of complex autocrine and paracrine interactions involving fibroblasts and other surrounding cells. SCLC cells secrete many growth factors, including insulin-like growth factor and neuropeptides such as gastrin-releasing peptide, which are mitogenic both for SCLC cells and fibroblasts24,25,26. In addition, a basal 'feeder' layer of human fibroblasts can stimulate the clonal growth of SCLC cells. Furthermore, SCLC cell lines also secrete many inflammatory cytokines and mediators involved in tissue repair (T.S., S.C.D. & R.S., unpublished results). These include TGF-β and IL-8 (an essential angiogenic factor for non-small cell lung cancer growth in nude mice27). In cultured fibroblasts, TGF-β modulates the splicing of the primary Fn transcript, leading to the production of other ECM proteins, including Ln and tenascin28,29. SCLC cell lines secrete Fn, as shown by western blot analysis (T.S. & R.C.R., unpublished results), and the detection of intracellular and pericellular staining for Fn, collagen IV, Ln and tenascin in pathological samples raises the possibility that, at least in some cases, SCLC cells may secrete these ECM proteins. ECM may also be a substrate for neovascularization30 further facilitating metastasis. Therefore, in vivo, SCLC may create a specialized environment as a consequence of autocrine and paracrine effects that, using an analogy to inflammation, likens SCLC to 'a wounding reaction' with the laying down and remodeling of ECM, growth factor release and neovascularization.
The exact function of tenascin is unclear. It is known to be an oncodevelopmental protein expressed in fetal tissue31 and in adult tissues that are actively remodeling, where it is often co-expressed with matrix metalloproteases32, supporting the idea that the local environment around SCLC is like an ongoing inflammatory reaction. Tenascin may facilitate growth factor-dependent proliferation and protect cells from apoptosis, possibly in conjunction with other ECM proteins33.
Doxorubicin, cyclophosphamide, etoposide and cis-platinum caused a concentration-dependent stimulation of apoptosis in SCLC cells. Overexpression of the multidrug resistance gene MDR1 is not common in SCLC, indicating that, unlike in other tumors, this is not an important mechanism for drug resistance in these tumors34. The binding of SCLC cells to laminin reduces the cytotoxicity of certain chemotherapeutic agents35. We have shown here that this is a general property of many ECM proteins found in increased amounts around SCLC in vivo. This occurs as a result of β1 integrin-dependent adhesion to Ln, Fn and collagen IV. Despite their anchorage independence, the binding of SCLC cells to ECM proteins confers protection from chemotherapy-induced apoptosis. Furthermore, Ln and collagen IV are the main glycoproteins of basement membranes, and induce migration, probably by haptotaxis36. This seems to be important in metastasis in many tumor cell lines. Thus, at primary and secondary metastatic sites, there seems to be a permissive environment for SCLC cell proliferation, protection from apoptosis and resistance to chemotherapy.
ECM suppression of cytotoxicity is not due to differentiation to a chemoresistant phenotype, a lower growth rate or ECM-stimulated autocrine secretion. Function-blocking β1 and function-stimulating β1 antibodies did not substantially affect SCLC cell–cell adhesion. The small increase in cell aggregation seen after prolonged contact with Fn is therefore most likely due to clonal expansion. Changes in cell–cell adhesion do not seem to be important in ECM-mediated resistance to chemotherapy. Our results indicate that the resistance to chemotherapy induced by β1-mediated adhesion to ECM is due to an increase in the level of PTK activity. However, increased intracellular tyrosine phosphorylation had no effect on etoposide-induced topoisomerase II inhibition. Thus, despite chemotherapy-induced DNA damage, ECM-mediated PTK activation blocks caspase activation, which prevents apoptosis. It is not known how integrin-stimulated PTK activation suppresses the early phase of apoptosis in SCLC cells. R-Ras and insulin-like growth factor-1, which activate phosphatidylinositol-3 kinase (PI3K), cooperatively inhibit caspase-3 activation, preventing apoptosis of BaF3 cells37. Activation of PI3K by integrins protects epithelial cells from detachment-induced apoptosis38. Integrin-stimulated PI3K activation may impinge on the nuclear response to DNA-damaging agents.
We made a retrospective analysis of available clinical case notes to determine the translational research implications of these findings. Sixteen patients 62.5 ± 2.3 years of age who had received some standard form of chemotherapy were identified; eight had no or focal Fn matrix and eight had extensive Fn matrix. They had a survival time of 11.5 ± 1.7 months (mean ± s.e.m.). There was no substantial age or sex difference between the two groups. Patients with extensive matrix around their tumors had a significantly shorter survival time from diagnosis (8.4 ± 1.7 months) than did patients with focal or no matrix (15 ± 2.6 months; mean ± s.e.m; P < 0.05, paired Student's t-test).
Our in vitro and in vivo data provide strong preliminary evidence that adhesion to ECM proteins is essential in SCLC cell resistance to chemotherapy. Cancer cells bound to ECM may escape chemotherapy-induced cell death and then, with subsequent genetic damage, drug-resistant clones are selected. This is an excellent model to explain not only SCLC behavior in vivo but also why partial responses and local recurrence of SCLC are often seen after chemotherapy. With the development of increasingly specific tyrphostins, identification of the PTKs mediating β1-integrin-dependent survival signals may provide new therapeutic strategies to improve the response of SCLC to chemotherapy.
Methods
Cell Culture.
H69, H510 and H345 cell lines from ATCC (Rockville, Maryland) were grown in RPMI 1640 medium (Sigma) supplemented with 10% (volume/volume) heat-inactivated fetal calf serum and 5 mg/ml L-glutamine in an atmosphere of 5% CO2. For experiments, cells were grown in SITA (RPMI 1640 supplemented with 30 nM selenium, 5 μg/ml insulin, 10 μg/ml transferrin and 0.25% (weight/volume) BSA). Cell viability was routinely greater than 90%, as judged by trypan blue exclusion.
Tissue immunohistochemistry.
Formalin-fixed, paraffin-embedded SCLC resection specimens from University of Edinburgh Department of Pathology files (1989–1994) were de-waxed in xylene and rehydrated through graded alcohols to water. Antigen unmasking was done by either pre-incubating sections in 0.1% trypsin, pH 7.6, at 37 °C for 15 min (for Fn, Ln and tenascin) or boiling them in a microwave oven for 15 min in 0.1 M citrate, pH 6.0 (for collagen IV). Primary antibodies against Fn (1:100 dilution; FN-3E2), Ln (1:50 dilution; LAM-89), tenascin (1:400 dilution; BC-24) and collagen IV (1:100 dilution; Col-94) were all from Sigma. Sections were processed using a Techmate 500 (Dako, Carpinteria, California). Antibody detection was done using a multilink streptavidin–biotin complex method, and visualization was achieved using a di-amino benzidine chromagen method following the manufacturer's instructions (Dako, Carpinteria, California). Slides were counterstained using Harris' hematoxylin. Negative control samples were incubated in primary antibody diluent only. All slides were reviewed independently by two people. Staining was graded on a semi-quantitative scale as no staining, focal staining or extensive (> 50% of section area) staining.
Flow cytometric analysis of integrin expression.
Cells (1 × 105) were washed in PBS containing 0.2% (weight/volume) BSA and 0.1% sodium azide (EPICS buffer), plated onto 96-well flexible assay plates and incubated at 4 °C for 30 min with integrin subunit antibodies (1:500 dilution) followed by a 30-minute incubation with species-appropriate FITC-conjugated secondary antibodies (1:40 dilution; Dako, Carpinteria, California). Cells were resuspended in EPICS buffer and analyzed by flow cytometry using an EPICS profile 2 (Coulter, Hialeah, Florida). All photomultiplier settings were standardized throughout the study. Mean fluorescence intensity arbitrary units on a log scale were recorded for each sample. The antibodies against integrin were all from Serotec unless otherwise stated: αv (13C2; M. Horton, Edinburgh, UK), α2 (AK7), α3 (11G5), α4 (HP2/1), α5 (SAM-1) and α6 (4F-10 (IgG2b)). β6 (E7P6G10P0) and β5 (PiF6) were from D. Salter (Edinburgh, UK); β4 (3E1) was from Life Technologies; β3 (PM6/13) and β2 (MHM23) were from Dako (Carpinteria, California); and β1 (mAb13) was from Becton Dickinson (San Jose, California).
Adhesion assay.
First, 96-well plates (CoStar, Cambridge, Massachusetts) were coated with 100 μl of 20 μg/ml fibronectin, 10 μg/ml laminin (Life Technologies) or 10 μg/ml collagen IV (Sigma) overnight at 4 °C and blocked with 1 mg/ml BSA (1 h at 25 °C). Then, SCLC cells (5 × 104) that had been washed twice in RPMI were added to the wells in the presence or absence of the function-blocking β1 antibodies P5D2 (10 μg/ml; P. Hughes, Scripps Research Institute) or 4B4 (10 μg/ml; Coulter, Hialeah, Florida) or 1 mM Mn2+. After 45 min of incubation at 37 °C, non-adherent cells were removed by gentle washing and adherent cells were fixed with 3% formaldehyde and stained with 1% methylene blue. After plates were washed with distilled water, 100 μl of 0.1 M HCl was added to each well and the absorbance of the resulting solution was measured at 630 nm on a plate reader (Dynatech Technologies, Chantilly, Virginia). Each condition was assayed in quadruplicate in duplicate plates.
Chemosensitivity assay.
Cells (0.5 × 105–1.0 × 105) cultured in SITA medium were seeded into 96-well microtiter plates in the presence or absence (where indicated) of 100 μl pre-coated fibronectin (20 μg/ml), laminin (10 μg/ml) or collagen IV (10 μg/ml). The cytotoxic agents platinum (cis-platinum (II) diammine dichloride), etoposide, doxorubicin (Sigma) and cyclophosphamide (CIS-4-sulfoethylthio-cyclophosphamide) (Asta Pharmaceuticals, Franfurt, Germany) were added to each well 1 h after seeding. Where indicated, function-blocking β1 antibodies (P5D2 or 4B4, both at 10 μg/ml) were added at the time of cell seeding, and etoposide and/or 25 μM tyrphostin-25 (Calbiochem. La Jolla, California) were added with the cytotoxic agent (1 h after cell seeding). Each condition was assayed in quadriplicate in duplicate plates. After 72 h, cells were either detached from the plates and aspirated and cytospun onto glass slides. Apoptotic cell populations were then assessed (described below). Live cells were determined by trypan blue exclusion, using a hemocytometer. The total cell number was determined using a Coulter counter (Coulter, Hialeah, Florida).
Assessment of SCLC cell apoptosis.
To assess apoptosis, 1 μl of an ethidium bromide (100 μg/ml)/acridine orange (100 μg/ml) (1/1 volume/volume) mixture was added to 200 μl SCLC cells, and the percentage of cells undergoing apoptosis was determined using fluorescent microscopy as described39. Apoptosis was also assessed using a Cell Detection ELISAPLUS kit following the manufacturer's instructions (Boehringer), or by staining cytospin preparations using May-Grünwald-Giemsa stain.
Clonogenic assay.
Cells (1 × 104) were suspended in a 0.3% (weight/volume) agarose/SITA mix containing neuropeptides (10 nM bradykinin or 50 nM galanin), ECM proteins (10 μg/ml laminin or 20 μg/ml fibronectin) and O–25 μg/ml etoposide. The cells were layered over a solid base of 0.5% (weight/volume) agarose in SITA containing the same additives, in 35-mm plastic dishes. Cultures were incubated in a humidified atmosphere of 5% CO2/95% air at 37 °C for 21 d, and were then stained with nitroblue tetrazolium. Colonies greater than 120 μm in diameter (16 cells) were counted using light microscopy.
Confocal microscopy.
SCLC cells (1 × 105) in SITA medium were allowed to attach for 45 min at 37 °C to glass cover slips pre-coated with 25 μg/ml poly-L-lysine or 10 μg/ml collagen IV. Unattached cells were gently removed by washing with SITA medium and attached cells were allowed to spread for 4 h. After fixation with 3% paraformaldehyde in PBS for 20 min, residual paraformaldehyde was 'quenched' using 50 mM NH4Cl/PBS. Cells were permeabilized with 0.1% Triton X-100 in PBS for 4 min and were blocked with 0.2% fish skin gelatin/PBS before being stained with rhodamine phalloidin (1:400 dilution) for 20 min at room temperature. Immunofluorescence was measured using a BioRad MRC 600 laser confocal microscope with a Zeiss 63× objective.
Immunoblotting.
To determine the effect of fibronectin on tyrosine phosphorylation, 1 × 106 H69 SCLC cells cultured in SITA medium were seeded in 6-well plates in the absence or presence of 20 μg/ml fibronectin with or without function-blocking β1 antibody (10 μg/ml 4B4). Etoposide (25 μg/ml) or tyrphostin-25 (25 μM) were added to each well 1 h after cell seeding. After 72 h, cells were aspirated and pelleted, and lysates were assessed by western blot analysis (see below) with anti-phosphotyrosine antibodies. A 50:50 mixture of PY20 (Santa Cruz Biotechnology, Santa Cruz, California) and 4G10 (Upstate Biotechnology, Lake Placid, New York) was used.
To determine the effect of fibronectin on etoposide-induced apoptosis and caspase-3 activation, H69 SCLC cells (1 × 106) cultured in SITA medium were seeded in 6-well plates. Etoposide (25 μg/ml), function-blocking β1 antibody (10 mg/ml), tyrphostin-25 (25 μM), z-Val-Ala-DL-Asp-fluromethylketone (100 μM) or sodium orthovanadate (200 μM) were added to each well 1 h after cell seeding. After 72 h of culture, apoptosis was determined by acridine orange staining (described above) and the level of pro-caspase 3 was determined by western blot analysis (see below) using an anti pro-caspase 3 antibody (CPP-32; Transduction Laboratories, Lexington, Kentucky).
For western blot analysis, cell pellets were lysed at 4 °C using standard RIPA buffer and 20 μg of protein were separated by 10% SDS–PAGE. Proteins were transferred to Hybond C nitrocellulose membranes (Amersham), and immunodetection was done using the enhanced chemiluminescence system (ECL; Amersham). The antibody against human topoisomerase IIα was from TopoGEN (Columbus, Ohio). Species-appropriate HRP-conjugated secondary antibodies were from Dako (Carpinteria, California).
Decatenation assay.
Cells (5 × 106) were cultured in SITA medium in 6-well plates in the presence or absence of 1 ml pre-coated fibronectin (20 μg/ml). Cells were allowed to 'settle' before the addition of 25 μg/ml etoposide or 25 μM tyrphostin-25. Each condition was assayed in duplicate. After 72 h, nuclear extracts were prepared as described40. Topoisomerase II activity was measured by the ATP-dependent decatenation of kDNA, in which an interlocking kDNA network is decatenated to individual DNA minicircles and small catenanes. Reaction buffer (50 mM Tris-HCI, pH 7.5, 10 mM MgCl2, 100 mM KCl, 0.5 mM EDTA, 30 μg/ml BSA, 1 mM ATP, 0.5 mM dithiothreitol and 100 μg/ml kDNA) was mixed with drug and enzymes (in that order) in a total volume of 45 μl, and the reaction mixtures were incubated for 30 min at 37 °C. The reaction was then stopped and reaction products were analyzed by agarose gel electrophoresis in 1% gels using 89 mM Tris-borate (pH 8.3) and 2 mM EDTA buffer.
References
Ihde, D., Pass, H., & Glastein, E. in Cancer: Principles and Practice of Oncology 4th edn. (eds. De Vita, V.T.Jr., Hellman, S. and Rosenberg, S.A.) 591–687 (J.B. Lippincott, Philadelphia, 1993).
Smyth, J.F. et al. The impact of chemotherapy on small cell carcinoma of the bronchus. Q. J. Med. 61, 969– 976 (1986).
Meredith, J.E. Jr., Fazeli, B. & Schwartz, M.A. The extracellular matrix as a cell survival factor. Mol. Biol. Cell 4, 953–961 (1993).
Frisch, S.M. & Francis, H. Disruption of epithelial cell-matrix interactions induces apoptosis. J. Cell Biol. 124, 619–626 (1994).
Meredith, J.E. Jr. & Schwartz, M.A. Integrins adhesion and apoptosis. Trends Cell Biol. 7, 146–150 (1997).
Boudreau, N., Sympson, C.J., Werb, Z. & Bissell, M.J. Suppression of ICE and apoptosis in mammary epithelial cells by extracellular matrix. Science 267, 891–893 (1995).
Freedman, V.H. & Shin, S. Cellular tumorigenicity in nude mice, correlation with cell growth in semi-solid medium. Cell 3, 355–359 (1974).
Smith, P.J. et al. Etoposide-induced cell cycle delay and arrest-dependent modulation of DNA topoisomerase II in small cell lung cancer cells. Br. J. Cancer 70, 914–921 ( 1994).
Aas, T. et al. Specific p53 mutations are associated with de novo resistance to doxorubicin in breast cancer patients. Nature Med. 2, 811–814 (1996).
Tallet, A. et al. Inhibition of neuropeptide-stimulated tyrosine phosphorylation and tyrosine kinase activity stimulates apoptosis in small cell lung cancer cells. Cancer Res. 56, 4255– 4263 (1996).
Sethi, T., Langdon, S., Smyth, J. & Rozengurt, E. Growth of small cell lung cancer cells: stimulation by multiple neuropeptides and inhibition by broad spectrum antagonists in vitro and in vivo. Cancer Res. 52, 2737s–2742s (1992).
Langdon, S.P., Cummings, J. & Smyth, J.F. Antagonists of mitogenic peptides. Cancer Topics 9, 10–13 ( 1994).
Kelly, M.J. et al. Antitumor activity of a monoclonal antibody directed against gastrin-releasing peptide in patients with small cell lung cancer. Chest 112, 256–261 ( 1997).
Haynes, R.O. Integrins: Versatility and signaling in cell adhesion. Cell 69, 11–25 (1992).
Elices, M.J., Urry, L.A. & Hemler, M.E. Receptor functions for the integrin VLA-3: Fibronectin, collagen and laminin binding are differentially influenced by ARG-GLY-ASP peptide and by divalent cations. J. Cell Biol. 112, 169–181 (1991).
Vogel, B.E., Tarone, G., Giancotti, F.G., Gailit, J. & Ruoslahti, E. A novel fibronectin receptor with an unexpected subunit composition (αvβ1). J. Biol. Chem. 265, 5934–5937 ( 1990).
Falcioni, R. et al. Expression of β1, β3, β4 and β5 integrins by Human Lung Carcinoma cells of different histotypes. Exp. Cell Res. 210, 113–122 ( 1994).
Carney, D.N., Gazdar, A.F. & Minna, J.D. Positive correlation between histological tumor involvement and generation of tumor cell colonies in agarose in specimens taken directly from patients with small-cell carcinoma of the lung. Cancer Res . 40, 1820–1823 ( 1980).
Giaccone, G. Small cell lung cancer and topoisomerases. Anticancer Res. 14, 269–276 (1994).
Sakahira, H., Enari, M. & Nagata, S. Cleavage of CAD inhibitor in CAD activation and DNA degradation during apoptosis. Nature 391, 96– 99 (1998).
Enari, M. et al. A caspase-activated DNAase that degrades DNA during apoptosis, and its inhibitor ICAD. Nature 391, 43– 50 (1998).
Sentman, C.L., Shutter, J.R., Hockenbery, D., Kanagawa, O. & Korsmeyer, S.J. Bcl-2 inhibits multiple forms of apoptosis but not negative selection in thymocytes. Cell 67, 879–888 (1991).
Chinnaiyan, A.M. et al. Molecular ordering of the cell death pathway. Bcl-2 and Bcl-xL function upstream of the CED-3-like apoptotic proteases. J. Biol. Chem. 271, 4573–4576 ( 1996).
Sethi, T & Rozengurt, E. Multiple neuropeptides stimulate clonal growth of small cell lung cancer: effects of bradykinin, vasopressin, cholecystokinin, galanin, and neurotensin. Cancer Res. 51, 3621–3623 ( 1991).
Bepler, G. et al. Peptides and growth factors in small cell lung cancer: production, binding sites, and growth effects. Cancer Res. Clin. Oncol. 114, 235–244 (1988).
Rozengurt, E. Neuropeptides as cellular growth factors: role of multiple signaling pathways. Eur. J. Clin. Invest. 21, 123– 134 (1991).
Arenberg, D.A. et al. Inhibition of interleukin-8 reduces tumourigenesis of human non-small cell lung cancer in SCID mice. J. Clin. Invest. 97, 2792–2802 (1996).
Borsi, L., Castellani, P., Risso, A.M., Leprini, A. & Zardi, L. Transforming growth factor-β regulates the splicing pattern of fibronectin messenger RNA precursor. FEBS Lett. 261, 175–178 (1990).
Sieweke, M.H., Thompson, N.L., Sporn, M.B. & Bissell, M.J. Mediation of wound-related Rous Sarcoma virus tumourigenesis by TGF-β. Science 48, 1656–1660 (1990).
Bloch, W. et al. β1 integrin is essential for teratoma growth and angiogenesis. J. Cell Biol. 139, 265– 278 (1997).
Nicolò, G. et al. Expression of tenascin and of the ED-B containing oncofetal fibronectin isoform in human cancer. Cell Diff. Dev. 32, 401–408 (1990).
Hedin, U., Holm, J. & Hansson, G.K. Induction of tenascin in rat arterial injury: relationship to altered smooth muscle cell phenotype. Am. J. Pathol. 139, 649–656 (1991).
Jones, P.L., Crack, J. & Rabinovitch, M. Regulation of Tenascin-C, a vascular smooth muscle cell survival factor that interacts with the αvβ3 integrin to promote epidermal growth factor receptor phosphorylation and growth. J. Cell Biol. 139, 279– 293 (1997).
Lai, S.L. et al. MDR1 gene expression in lung cancer. J. Natl. Cancer Inst. 81, 1144–1150 ( 1989).
Fridman, R. et al. Reconstituted basement membrane (matrigel) and laminin can enhance the tumorgenicity and the drug resistance of small cell lung cancer cell lines. Proc. Natl. Acad. Sci. USA 87, 6698–6702 (1990).
McCarthy, J.B., Barara, M.L., Palm, S.L., Sas, D.F. & Furcht. L.T. The role of cell adhesion proteins-laminin and fibronectin-in the movement of malignant and metastatic cells. Cancer Metastasis Rev. 4, 125–152 ( 1985).
Suzuki, J., Kaziro, Y., & Koide, H. Synergistic action of R-Ras and IGF-1 on Bcl-xL expression and caspase-3 inhibition in BaF3 cells: R-Ras and IGF-1 control distinct anti-apoptotic kinase pathways. FEBS Lett. 437, 112– 116 (1998).
Khwaja, A., Rodriguez-Viciana, P., Wennstrom, S., Warne, P.H., & Downward, J. Matrix adhesion and Ras transformation both activate a phosphoinositide 3-OH kinase and protein kinase B/Akt cellular survival pathway. EMBO J. 16, 2783– 2793 (1997).
Duke R.C. & Cohen. J.J. in Current Protocols in Immunology (eds. Coligan, J.E. et al.) 3.17.1– 3.17.16 (John Wiley & Sons, New York, 1992).
Staal, F.J.T., Roederer, M., Herzenberg L.A. & Herzenberg L.A. Intracellular thiols regulate activation of nuclear kB and transcription of human immunodeficiency virus. Proc. Natl. Acad. Sci. USA 87, 9943–9947 (1990).
Acknowledgements
We thank G. Boyd and J. Cummings (ICRF, Western General Hospital, Edinburgh, UK) for help with topoisomerase II alpha experiments, and J. Lauder and B. Simpson (Department of Pathology, University of Edinburgh) for assistance with immunohistochemistry. We also thank P. Hughes (Scripps Research Institute) for comments on the manuscript. This work was supported by the Medical Research Council UK (Clinical Training Fellowship to RCR) and the Scottish Hospital Endowment Research Trust.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sethi, T., Rintoul, R., Moore, S. et al. Extracellular matrix proteins protect small cell lung cancer cells against apoptosis: A mechanism for small cell lung cancer growth and drug resistance in vivo. Nat Med 5, 662–668 (1999). https://doi.org/10.1038/9511
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1038/9511
This article is cited by
-
Fibronectin promotes tumor angiogenesis and progression of non-small-cell lung cancer by elevating WISP3 expression via FAK/MAPK/ HIF-1α axis and activating wnt signaling pathway
Experimental Hematology & Oncology (2023)
-
DeepInsight-3D architecture for anti-cancer drug response prediction with deep-learning on multi-omics
Scientific Reports (2023)
-
Identification of ferroptosis and drug resistance related hub genes to predict the prognosis in Hepatocellular Carcinoma
Scientific Reports (2023)
-
Combination of naringenin and epicatechin sensitizes colon carcinoma cells to anoikis via regulation of the epithelial–mesenchymal transition (EMT)
Molecular & Cellular Toxicology (2023)
-
Cell fiber-based 3D tissue array for drug response assay
Scientific Reports (2022)