Abstract
We conducted this population-based cohort study by linking several databases to explore the role of socioeconomic position for accessing and keeping antihypertensive drug therapy. A total of 71 469 patients, residents in the city of Milan (Italy) aged 40–80 years, who received an antihypertensive drug during 1999–2002 were followed for 1 year starting from the first dispensation. Socioeconomic position and drug prescriptions were respectively obtained from tax registry and outpatient prescription database. The effect of socioeconomic characteristics on standardized incidence rate (SIR) of new users of antihypertensive agents, odds ratio (OR) of using combined antihypertensive agents and non-antihypertensive drugs and hazard ratio (HR) of discontinuing antihypertensive therapy were estimated after adjustment for potential confounders. SIRs were 3.7 and 4.2 per 1000 person-months among persons at the lowest and intermediate income, respectively, and 2.4 and 3.0 among immigrants and Italians, respectively. Compared to persons at the highest income, those at the lowest income had increased chances of starting with combined antihypertensive drugs (OR: 1.1; 95% confidence intervals (CIs): 1.0, 1.2), and of using drugs for heart failure (OR:1.5; CIs:1.3, 1.6) and diabetes (OR: 1.7; CIs: 1.6, 1.9). Compared with Italians, non-western immigrants had increased chances of starting with combined antihypertensive agents (OR: 1.2; CIs: 1.0, 1.3), of using drugs for heart failure (OR: 1.2; CIs: 1.0, 1.4) and for diabetes (OR: 1.8; CIs: 1.6, 2.1), and of interrupting antihypertensive therapy (HR: 1.1; 95% CIs: 1.0, 1.2). Despite the universal health coverage of the Italian National Health Service (NHS), social disparities affect accessing and keeping antihypertensive therapy.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Fields LE, Burt VL, Cutler JA, Hughes J, Roccella EJ, Sorlie P . The burden of adult hypertension in the United States 1999–2000: a rising tide. Hypertension 2004; 44: 398–404.
van Rossum CTM, van de Mheen H, Witteman JCM, Hofman A, Mackenbach JP, Grobbee DE . Prevalence, treatment, and control of hypertension by sociodemographic factors among the Dutch elderly. Hypertension 2000; 35: 814–821.
Primatesta P, Poulter NR . Hypertension management and control among English adults aged 65 years and older in 2000 and 2001. J Hypertens 2004; 22: 1093–1098.
Swaby P, Wilson E, Swaby S, Sue-Ho R, Pierre R . Chronic disease control and compliance—the HOPE worldwide Jamaica experience. West Indian Med J 2001; 50 (Suppl. 1): 51–53.
Czarnecka D, Pawelec M, Kopacz E, Kloch M . Socioeconomical status of life and regularity of intake of medicines among hypertensive patients. Przegl Lek 2006; 63: 633–636.
Morris AB, Li J, Kroenke K, Bruner-England TE, Young JM, Murray MD . Factors associated with drug adherence and blood pressure control in patients with hypertension. Pharmacotherapy 2006; 26: 483–492.
Stroupe KT, Teal EY, Tu W, Weiner M, Murray MD . Association of refill adherence and health care use among adults with hypertension in an urban health care system. Pharmacotherapy 2006; 26: 779–789.
Hyre AD, Krousel-Wood MA, Muntner P, Kawasaki L, DeSalvo KB . Prevalence and predictors of poor antihypertensive medication adherence in an urban health clinic setting. J Clin Hypertens (Greenwich) 2007; 9: 179–186.
Morenoff JD, House JS, Hansen BB, Williams DR, Kaplan GA, Hunte HE . Understanding social disparities in hypertension prevalence, awareness, treatment, and control: the role of neighborhood context. Soc Sci Med 2007; 65: 1853–1866.
Petrelli A, Gnavi R, Marinacci C, Costa G . Socioeconomic inequalities in coronary heart disease in Italy: a multilevel population-based study. Soc Sci Med 2006; 63: 446–456.
Atkinson AB, Rainwater L, Smeeding TM . Income Distribution in OECD Countries. OECD: Paris, 1995.
Esteve J, Benhamou E, Raymond L . Statistical Methods in Cancer research. Vol. IV. Descriptive Epidemiology. IARC Scientific Publications No 128. International Agency for Research on Cancer: Lyon, France, 1994.
Marubini E, Valsecchi MG . Analysing Survival Data from Clinical Trials and Observational Studies. John Wiley & Sons: New York, 1995.
Schneider S, Mohnen S, Schiltenwolf M . Are rich people healthier? Representative epidemiological data on socioeconomic group-specific disease prevalences among adults in Germany. Dtsch Med Wochenschr 2006; 131: 1998–2003.
Kuper H, Adami HO, Theorell T, Weiderpass E . Psychosocial determinants of coronary heart disease in middle-aged women: a prospective study in Sweden. Am J Epidemiol 2006; 164: 349–357.
Banks J, Marmot M, Oldfield Z, Smith JP . Disease and disadvantage in the United States and in England. JAMA 2006; 295: 2037–2045.
Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G et al. The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). 2007 Guidelines for the Management of Arterial Hypertension. J Hypertens 2007; 25: 1105–1187.
Lip GYH, Barnett AH, Bradbury A, Cappuccio FP, Gill PS, Hughes E et al. Ethnicity and cardiovascular disease prevention in the United Kingdom: a practical approach to management. J Hum Hypertens 2007; 21: 183–211.
Agyemang C, Bhopal R . Is the blood pressure of people from African origin adults in the UK higher or lower than that in European origin white people? A review of cross-sectional data. J Hum Hypertens 2003; 17: 523–534.
Gushulak B . Healthier on arrival? Further insight into the ‘healthy immigrant effect’. Can Med Assoc J 2007; 176: 1439–1440.
Agyemang C, Bhopal RS . Is the blood pressure of South Asian adults in the UK higher or lower than in the European white adults? A review of cross-sectional data. J human Hypertens 2002; 16: 739–751.
Van Wijk BLG, Klungel OH, Heerdink ER, de Boer A . Rate and determinants of 10-year persistence with anti-hypertensive drugs. J Hypertens 2005; 23: 2101–2107.
Mazzaglia G, Mantovani L, Sturkenboom MC, Filippi A, Trifirò G, Cricelli C et al. Patterns of persistence with antihypertensive medications in newly diagnosed hypertensive patients in Italy: a retrospective cohort study in primary care. J Hypertens 2005; 23: 2093–2100.
Erkens JA, Panneman MMJ, Klungel OH, van den Boom G, Prescott MF, Herings RMC . Differences in antihypertensive drug persistence associated with drug class and gender: a PHARMO study. Pharmacoepidemiol Drug Saf 2005; 14: 795–803.
Burke TA, Sturkenboom MC, Lu S-E, Wentworth CE, Lin Y, Rhoads GG . Discontinuation of hypertensive drugs among newly diagnosed hypertensive patients in UK general practice. J Hypertens 2006; 24: 1193–1200.
Elliott WJ, Plauschinat CA, Skrepnek GH, Gause D . Persistence, adherence, and risk of discontinuation associated with commonly prescribed antihypertensive drug monotherapies. J Am Board Fam Med 2007; 20: 72–80.
Conrad P . The meaning of medications: another look at compliance. Soc Science and Med 1985; 20: 29–37.
van Dijk L, Heerdink ER, Somai D, van Dulmen S, Sluijs EM, de Ridder DT et al. Patient risk profiles and practice variation in nonadherence to antidepressants, antihypertensives and oral hypoglycemics. BMC Health Serv Res 2007; 7: 51.
Cable G . Income, race, and preventable hospitalizations: a small area analysis in New Jersey. J Health Care Poor Underserved 2002; 13: 66–80.
van der Meer JBW, van den Bos J, Mackenbach JP . Socioeconomic differences in the utilization of health services in a Dutch population: the contribution of health status. Health Policy 1996; 37: 1–18.
van der Heyden JHA, Demarest S, Tafforeau J, van Oyen H . Socioeconomic differences in the utilization of health services in Belgium. Health Policy 2003; 65: 153–165.
Fernandez de la Hoz K, Leon DA . Self-perceived health status and inequalities in use of health services in Spain. Int J Epidemiol 1996; 25: 593–603.
Dunlop S, Coyte P, McIsaac W . Socio-economic status and the utilisation of physicians' services: results from the Canadian National Population Health Survey. Soc Sci Med 2000; 51: 123–133.
McIsaac W, Goel V, Naylor D . Socio-economic status and visits to physicians by adults in Ontario, Canada. J Health Serv Res Policy 1997; 2: 94–102.
Burstrom B . Increasing inequalities in health care utilisation across income groups in Sweden during the 1990s? Health Policy 2002; 62: 117–129.
Choo PW, Rand CS, Inui TS, Ting Lee M-L, Canning C, Platt R . A cohort study of possible risk factors for over-reporting of antihypertensive adherence. BMC Cardiovascular Disorders 2001; 1: 6.
Poluzzi E, Strahinja P, Vargiu A, Chaibrando G, Silvani MC, Motola D et al. Initial treatment of hypertension and adherence to therapy in general practice in Italy. Eur J Clin Pharmacol 2005; 61: 603–609.
Acknowledgements
This study was supported by the Italian Minister of the Education, University and Research grants (‘Fondo d'Ateneo per la Ricerca’ portion, years 2005 and 2006, and PRIN portion, protocol n° 2005068001, year 2005).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Corrao, G., Zambon, A., Parodi, A. et al. Do socioeconomic disparities affect accessing and keeping antihypertensive drug therapy? Evidence from an Italian population-based study. J Hum Hypertens 23, 238–244 (2009). https://doi.org/10.1038/jhh.2008.84
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhh.2008.84
Keywords
This article is cited by
-
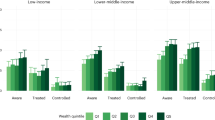
Socio-economic inequalities in the use of drugs for the treatment of chronic diseases in Italy
International Journal for Equity in Health (2022)
-
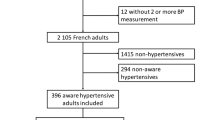
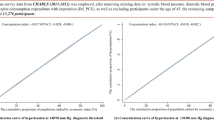
Treatment and adherence to antihypertensive therapy in France: the roles of socioeconomic factors and primary care medicine in the ESTEBAN survey
Hypertension Research (2021)
-
Adherence of Elderly Patients with Cardiovascular Disease to Statins and the Risk of Exacerbation of Chronic Obstructive Pulmonary Disease: Evidence from an Italian Real-World Investigation
Drugs & Aging (2018)
-
Drug use profile in outpatient children and adolescents in different Italian regions
BMC Pediatrics (2013)