Abstract
Venous thromboembolism (VTE) is a major cause of morbidity and mortality in patients with cancer. Primary prevention with pharmacologic agents (or mechanical methods, if anticoagulants are contraindicated) is recommended in all cancer patients hospitalized for surgical or medical reasons. The role of prophylaxis in outpatients is less certain because of the diversity of the patient populations and their cancer treatments with respect to the associated risks of VTE and bleeding. Treatment with low-molecular weight heparin is the recommended first-line approach in cancer patients with newly diagnosed VTE, and is usually continued for a minimum of 3–6 months. Other management issues that require further research include the optimum duration of anticoagulant therapy, the treatment of recurrent VTE, the role of vena cava filters, the effects of VTE and its treatment on quality of life, and the impact of anticoagulants on survival. Newer anticoagulants hold promise in providing more-effective and convenient treatment of VTE in this high-risk population, but further studies are awaited.
Key Points
-
Primary prevention with pharmacologic agents (or mechanical methods, if anticoagulants are contraindicated) is recommended in all cancer patients hospitalized for surgery or medical reasons
-
Extending prophylaxis up to 30 days after surgery should be considered in patients with additional risk factors for venous thromboembolism (VTE)
-
Routine prophylaxis in outpatients is not recommended except in selected patients, such as those receiving thalidomide-based or lenalidomide-based therapy
-
Treatment with low-molecular-weight heparin is the recommended first-line approach in cancer patients with newly diagnosed VTE
-
Treatment duration should be individualized based on the stage or extent of the cancer, the risk of recurrent VTE, the risk of serious bleeding, the clinical status and personal preference of the patient
-
Evidence for the efficacy and safety of inferior vena cava filters is very limited and they should not be used in patients who can receive anticoagulants
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Khorana AA et al. (2007) Thromboembolism is a leading cause of death in cancer patients receiving outpatient chemotherapy. J Thromb Haemost 5: 632–634
Blom JW et al. (2005) Malignancies, prothrombotic mutations, and the risk of venous thrombosis. JAMA 293: 715–722
Hutten BA et al. (2000) Incidence of recurrent thromboembolic and bleeding complications among patients with venous thromboembolism in relation to both malignancy and achieved international normalized ratio: a retrospective analysis. J Clin Oncol 18: 3078–3083
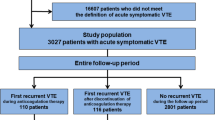
Prandoni P et al. (2002) Recurrent venous thromboembolism and bleeding complications during anticoagulant treatment in patients with cancer and venous thrombosis. Blood 100: 3484–3488
Elting LS et al. (2004) Outcomes and costs of deep venous thrombosis among patients with cancer. Arch Intern Med 164: 1653–1661
Geerts WH et al. (2004) Prevention of venous thromboembolism: The Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 126: 338S–400S
Leonardi MJ et al. (2007) A systematic review of deep venous thrombosis prophylaxis in cancer patients: implications for improving quality. Ann Surg Oncol 14: 929–936
Fricker JP et al. (1988) Low dose heparin versus low molecular weight heparin (Kabi 2165, Fragmin) in the prophylaxis of thromboembolic complications of abdominal oncological surgery. Eur J Clin Invest 18: 561–567
McLeod RS et al. (2001) Subcutaneous heparin versus low molecular-weight heparin as thromboprophylaxis in patients undergoing colorectal surgery: results of the Canadian colorectal DVT prophylaxis trial: a randomized, double-blind trial. Ann Surg 233: 438–444
ENOXACAN Study Group (1997) Efficacy and safety of enoxaparin versus unfractionated heparin for prevention of deep vein thrombosis in elective cancer surgery: a double-blind randomized multicentre trial with venographic assessment. ENOXACAN Study Group. Br J Surg 84: 1099–1103
Petrov M et al. (2007) Enoxaparin versus heparin prophylaxis for venous thromboembolism after abdominal oncologic surgery: a randomized double-blind controlled trial [abstract #668]. J Thromb Haemost 5: 668
Bergqvist D et al. (2005) Low molecular weight heparin started before surgery as prophylaxis against deep vein thrombosis: 2500 versus 5000 units in 2070 patients. Br J Surg 82: 496–501
Balibrea JL et al. (2007) Bemiparin Cooperative Study Group in Surgery for Cancer. Optimal dosing of bemiparin as prophylaxis against venous thromboembolism in surgery for cancer: an audit of practice. Int J Surg 5: 114–119
Simonneau G et al. (2006) A randomized study comparing the efficacy and safety of nadroparin 2850 IU (0.3 mL) vs. enoxaparin 4000 IU (40 mg) in the prevention of venous thromboembolism after colorectal surgery for cancer. J Thromb Haemost 4: 1693–1700
Bergqvist D et al. (2002) Duration of prophylaxis against venous thromboembolism with enoxaparin after surgery for cancer. N Engl J Med 346: 975–980
Lausen I et al. (1998) Incidence and prevention of deep venous thrombosis occurring late after general surgery: randomized controlled study of prolonged thromboprophylaxis. Eur J Surg 164: 657–663
Rasmussen MS et al. (2003) Prolonged prophylaxis with low molecular weight heparin (Dalteparin) following major abdominal surgery for malignancy. Blood 102: 56a
Agnelli G et al. (2006) A clinical outcome-based prospective study on venous thromboembolism after cancer surgery: the @RISTOS project. Ann Surg 243: 89–95
Agnelli G et al. (2005) Randomized clinical trial of postoperative fondaparinux versus perioperative dalteparin for prevention of venous thromboembolism in high-risk abdominal surgery. Br J Surg 92: 1212–1220
Lyman GH et al. (2007) American society of clinical oncology guideline: recommendations for venous thromboembolism prophylaxis and treatment in patients with cancer. J Clin Oncol 25: 1–16
Marras LC et al. (2000) The risk of venous thromboembolism is increased throughout the course of malignant glioma: an evidence-based review. Cancer 89: 640–646
Simanek R et al. (2007) Venous thromboembolism and survival in patients with high-grade glioma. Neuro-Oncology 9: 89–95
Semrad TJ et al. (2007) Epidemiology of venous thromboembolism in 9489 patients with malignant glioma. J Neurosurg 106: 601–608
Cerrato D et al. (1978) Deep vein thrombosis and low-dose heparin prophylaxis in neurosurgical patients. J Neurosurg 49: 378–381
Melon E et al. (1987) Deep venous thrombosis prophylaxis by low molecular weight heparin in neurosurgical patients. Anesthesiology 75: A214
Nurmohamed MT et al. (1996) Low molecular weight heparin and compression stockings in the prevention of venous thromboembolism in neurosurgery. Thromb Haemost 75: 233–238
Agnelli G et al. (1998) Enoxaparin plus compression stockings compared with compression stockings alone in the prevention of venous thromboembolism after elective neurosurgery. N Engl J Med 339: 80–85
Iorio A and Agnelli G (2000) Low-molecular-weight and unfractionated heparin for prevention of venous thromboembolism in neurosurgery: a meta-analysis. Arch Int Med 160: 2327–2332
Dickinson LD et al. (1998) Enoxaparin increases the incidence of postoperative intracranial hemorrhage when initiated preoperatively for deep venous thrombosis prophylaxis in patients with brain tumors. Neurosurgery 43: 1074–1081
Goldhaber SZ et al. (2002) Low rate of venous thromboembolism after craniotomy for brain tumor using multimodality prophylaxis. Chest 122: 1933–1937
MacDonald RL et al. (2003) Randomized, pilot study of intermittent pneumatic compression devices plus dalteparin versus intermittent pneumatic compression devices plus heparin for prevention of venous thromboembolism in patients undergoing craniotomy. Surg Neurology 59: 363–372
Perry JR et al. (2007) PRODIGE: A phase III randomized placebo-controlled trial of thromboprophylaxis using dalteparin low molecular weight heparin (LMWH) in patients with newly diagnosed malignant glioma [abstract#2011]. J Clin Oncol 25 (Suppl): 77s
Clarke-Pearson DL et al. (1983) Venous thromboembolism prophylaxis in gynecologic oncology: a prospective, controlled trial of low-dose heparin. Am J Obst Gynecol 145: 606–613
Clarke-Pearson DL et al. (1990) A controlled trial of two low-dose heparin regimens for the prevention of postoperative deep vein thrombosis. Obst Gynecol 75: 684–689
Einstein MH et al. (2007) Venous thromboembolism prevention in gynecologic cancer surgery: a systematic review. Gynecol Onc 105: 813–819
Borstad E et al. (1988) Comparison of low molecular weight heparin vs unfractionated heparin in gynecological surgery. Acta Obstet Gynecol Scand 67: 99–103
Kaaja R et al. (1992) Comparison of enoxaparin, a low-molecular-weight heparin, and unfractionated heparin, with or without dihydroergotamine, in abdominal hysterectomy. Eur J Obstet Gynecol Reprod Biol 47: 141–145
von Tempelhoff GF et al. (2000) Effect of low molecular weight heparin (Certoparin) versus unfractionated heparin on cancer survival following breast and pelvic cancer surgery: a prospective randomized double-blind trial. Int J Oncol 16: 815–824
Baykal et al. (2001) Comparison of enoxaparin and standard heparin in gynaecologic oncologic surgery: a randomised prospective double-blind clinical study. Eur J Gynaecol Onc 22: 127–130
Cade JF et al. (1983) Prophylaxis of venous thrombosis after major thoracic surgery. ANZ J Surg 53: 301–304
Azorin JF et al. (1997) Efficacy and tolerability of fraxiparine in the prevention of thromboembolic complications in oncologic thoracic surgery. Ann Cardiol Angeiol (Paris) 46: 341–347
Bigg SW et al. (1992) Prophylactic mini-dose heparin in patients undergoing radical retropubic prostatectomy. A prospective trial. Urology 39: 309–313
Sawczuk IS et al. (2002) Low molecular weight heparin for venous thromboembolism prophylaxis in urologic oncologic surgery. Cancer Invest 20: 889–892
Patiar S et al. (2007) Prevention of venous thromboembolism in surgical patients with breast cancer. Br J Surg 94: 412–420
Lin PP et al. (1998) Deep venous thrombosis after orthopedic surgery in adult cancer patients. J Surg Onc 68: 41–47
Clarke-Pearson DL et al. (1984) Prevention of postoperative venous thromboembolism by external pneumatic calf compression in patients with gynecologic malignancy. Obstet Gynecol 63: 92–98
Turpie AG et al. (1977) Prevention of venous thrombosis in patients with intracranial disease by intermittent pneumatic compression of the calf. Neurology 27: 435–438
Stein PD et al. (2006) Incidence of venous thromboembolism in patients hospitalized with cancer. Am J Med 1999: 60–68
Khorana AA et al. (2006) Thromboembolism in hospitalized neutropenic cancer patients. J Clin Oncol 24: 484–490
Levine M et al. (1994) Double-blind randomised trial of a very-low-dose warfarin for prevention of thromboembolism in stage IV breast cancer. Lancet 343: 886–889
Ciftci A et al. (2007) Thrombosis in patients with lung cancer and the effectiveness of low warfarin prophylaxis on patients survival [abstract #563]. J Thromb Haemost 5 (suppl 1): 563
Haas SK et al. (2005) Prevention of venous thromboembolism with low-molecular-weight heparin in patients with metastatic breast or lung cancer—results of the TOPIC Studies [abstract #OR059]. J Thromb Haemost 3 (Suppl 1): OR059
Pelzer H et al. (2007) Prospective, randomized open trial of enoxaparin in patient with advanced pancreatic cancer undergoing first-line chemotherapy [abstract #PT488]. J Thromb Haemost 5 (Suppl 2): PT488
Hirsh J (2007) Risk of thrombosis with lenalidomide and its prevention with aspirin. Chest 131: 275–277
Amin A et al. (2007) Thromboprophylaxis rates in US medical centers: success or failure? J Thromb Haemost 5: 1610–1616
Kucher et al. (2005) Electronic alerts to prevent venous thromboembolism among hospitalized patients. N Engl J Med 352: 969–971
Francis CW (2007) Prophylaxis for thromboembolism in hospitalized medical patients. N Engl Med 356: 1438–1444
Van Dongen CJ et al.: Fixed dose subcutaneous low molecular weight heparins versus adjusted dose unfractionated heparin for venous thromboembolism. Cochrane Database of Systematic Reviews 2004, Issue 4. Art. No.: CD001100. 10.1002/14651858.CD001100.pub2
Lee AYY (2003) Management of thrombosis in cancer: primary prevention and secondary prophylaxis. Br J Haematol 128: 291–302
Ageno W et al. (2002) Selecting patients for home treatment of deep vein thrombosis: the problem of cancer. Haematologica 87: 286–291
Martel N et al. (2005) Risk for heparin-induced thrombocytopenia with unfractionated and low-molecular-weight heparin thromboprophylaxis: a meta-analysis. Blood 106: 2710–2715
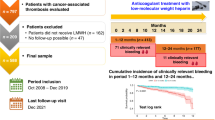
Lee AYY et al. (2003) Low-molecular-weight heparin versus a coumarin for the prevention of recurrent venous thromboembolism in patients with cancer. N Engl J Med 349: 146–153
Hull RD et al. (2006) Long-term low-molecular-weight heparin versus usual care in proximal-vein thrombosis patients with cancer. Am J Med 119: 1062–1072
Meyer G et al. (2002) Comparison of low-molecular-weight heparin and warfarin for the secondary prevention of venous thromboembolism in patients with cancer: a randomized controlled study. Arch Int Med 162: 1729–1735
Deitcher SR et al. (2006) Secondary prevention of venous thromboembolic events in patients with active cancer: enoxaparin alone versus initial enoxaparin followed by warfarin for a 180-day period. Clin Applied Thromb Hemost 12: 389–396
The van Gogh Investigators (2007) Idraparinux versus standard therapy for venous thromboembolic disease. N Engl J Med 357: 1094–1104
The PREPIC (Prevention du Risque d'Embolie Pulmonaire par Interruption Cave) randomized study (2005) Eight-year follow-up of patients with permanent vena cava filters in the prevention of pulmonary embolism. Circulation 112: 416–422
Buller HR et al. (2204) Antithrombotic therapy for venous thromboembolic disease: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 126 (3 Suppl): 401S–428S
Goerner A (1931) The influence of anticlotting agents on transplantation growth of tumor tissue. J Lab Clin Med 16: 369–372
Lebeau B et al. (1994) Subcutaneous heparin treatment increases survival in small cell lung cancer. “Petites Cellules” Group. Cancer 74: 38–45
Elias EG et al. (1975) Heparin and chemotherapy in the management of inoperable lung carcinoma. Cancer 36: 129–136
Zacharski LR et al. (1981) Effect of warfarin on survival in small cell carcinoma of the lung. Veterans Administration Study No. 75. JAMA 245: 831–835
Chahinian AP et al. (1989) A randomized trial of anticoagulation with warfarin and of alternating chemotherapy in extensive small-cell lung cancer by the Cancer and Leukemia Group B. J Clin Oncol 7: 993–1002
Altinbas M et al. (2004) A randomized clinical trial of combination chemotherapy with and without low-molecular-weight heparin in small cell lung cancer. J Thromb Haemost 2: 1266–1271
Klerk CPW et al. (2005) The effect of low molecular weight heparin on survival in patients with advanced malignancy. J Clin Oncol 23: 2130–2135
Kakkar AK et al. (2004) Low molecular weight heparin, therapy with dalteparin, and survival in advanced cancer: the fragmin advanced malignancy outcome study (FAMOUS). J Clin Oncol 22: 1944–1948
Sideras K et al. (2006) Low-molecular-weight-heparin in patients with advanced cancer: a phase 3 clinical trial. Mayo Clin Proc 81: 758–767
Zacharski LR et al. (1984) Effect of warfarin anticoagulation on survival in carcinoma of the lung colon, head and neck, and prostate. Final report of VA Cooperative Study 75. Cancer 53: 2046–2052
Maurer LH et al. (1997) Randomized trial of chemotherapy and radiation therapy with or without warfarin for limited-stage small-cell lung cancer: a Cancer and Leukemia Group B study. J Clin Oncol 15: 3378–3387
Lazo-Langner A et al. (2007) The effect of low-molecular-weight heparin on cancer survival. A systematic review and meta-analysis of randomized trials. J Thromb Haemost 5: 729–737
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Agnes YY Lee declared that she receives research funding from Pfizer. Marc Carrier declared no competing interests.
Rights and permissions
About this article
Cite this article
Carrier, M., Lee, A. Prophylactic and therapeutic anticoagulation for thrombosis—major issues in oncology. Nat Rev Clin Oncol 6, 74–84 (2009). https://doi.org/10.1038/ncponc1244
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ncponc1244
This article is cited by
-
A Prospective Observational Study to Determine Rate of Thromboprophylaxis in Oncology Patients Undergoing Abdominal or Pelvic Surgery
Indian Journal of Surgical Oncology (2021)
-
Predictors of thrombosis in testicular cancer during platinum-based chemotherapy
World Journal of Urology (2019)
-
The low-molecular-weight heparin, nadroparin, inhibits tumour angiogenesis in a rodent dorsal skinfold chamber model
British Journal of Cancer (2010)
-
Onkologische Notfälle II
Der Onkologe (2010)
-
Ältere Patienten profitieren von Primärtherapie mit Bortezomib
best practice onkologie (2010)