Abstract
Viral respiratory tract infections are the main causative agents of the onset of infection-induced asthma and asthma exacerbations that remain mechanistically unexplained. Here we found that deficiency in signaling via type I interferon receptor led to deregulated activation of group 2 innate lymphoid cells (ILC2 cells) and infection-associated type 2 immunopathology. Type I interferons directly and negatively regulated mouse and human ILC2 cells in a manner dependent on the transcriptional activator ISGF3 that led to altered cytokine production, cell proliferation and increased cell death. In addition, interferon-γ (IFN-γ) and interleukin 27 (IL-27) altered ILC2 function dependent on the transcription factor STAT1. These results demonstrate that type I and type II interferons, together with IL-27, regulate ILC2 cells to restrict type 2 immunopathology.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
References
Gause, W.C., Wynn, T.A. & Allen, J.E. Type 2 immunity and wound healing: evolutionary refinement of adaptive immunity by helminths. Nat. Rev. Immunol. 13, 607–614 (2013).
Hoyler, T. et al. The transcription factor GATA-3 controls cell fate and maintenance of type 2 innate lymphoid cells. Immunity 37, 634–648 (2012).
Spits, H. et al. Innate lymphoid cells–a proposal for uniform nomenclature. Nat. Rev. Immunol. 13, 145–149 (2013).
Diefenbach, A., Colonna, M. & Koyasu, S. Development, differentiation, and diversity of innate lymphoid cells. Immunity 41, 354–365 (2014).
McKenzie, A.N., Spits, H. & Eberl, G. Innate lymphoid cells in inflammation and immunity. Immunity 41, 366–374 (2014).
Halim, T.Y. et al. Group 2 innate lymphoid cells are critical for the initiation of adaptive T helper 2 cell-mediated allergic lung inflammation. Immunity 40, 425–435 (2014).
Monticelli, L.A. et al. Innate lymphoid cells promote lung-tissue homeostasis after infection with influenza virus. Nat. Immunol. 12, 1045–1054 (2011).
Barlow, J.L. & McKenzie, A.N. Type-2 innate lymphoid cells in human allergic disease. Curr. Opin. Allergy Clin. Immunol. 14, 397–403 (2014).
Lambrecht, B.N. & Hammad, H. The immunology of asthma. Nat. Immunol. 16, 45–56 (2015).
Yoo, J.K., Kim, T.S., Hufford, M.M. & Braciale, T.J. Viral infection of the lung: host response and sequelae. J. Allergy Clin. Immunol. 132, 1263–1276, quiz 1277 (2013).
Hansel, T.T., Johnston, S.L. & Openshaw, P.J. Microbes and mucosal immune responses in asthma. Lancet 381, 861–873 (2013).
Edwards, M.R., Bartlett, N.W., Hussell, T., Openshaw, P. & Johnston, S.L. The microbiology of asthma. Nat. Rev. Microbiol. 10, 459–471 (2012).
Wark, P.A. et al. Asthmatic bronchial epithelial cells have a deficient innate immune response to infection with rhinovirus. J. Exp. Med. 201, 937–947 (2005).
Edwards, M.R. et al. Impaired innate interferon induction in severe therapy resistant atopic asthmatic children. Mucosal Immunol. 6, 797–806 (2013).
García-Sastre, A. Induction and evasion of type I interferon responses by influenza viruses. Virus Res. 162, 12–18 (2011).
Barik, S. Respiratory syncytial virus mechanisms to interfere with type 1 interferons. Curr. Top. Microbiol. Immunol. 372, 173–191 (2013).
Feng, Q., Langereis, M.A. & van Kuppeveld, F.J. Induction and suppression of innate antiviral responses by picornaviruses. Cytokine Growth Factor Rev. 25, 577–585 (2014).
Jain, S. et al. Hospitalized patients with 2009 H1N1 influenza in the United States, April-June 2009. N. Engl. J. Med. 361, 1935–1944 (2009).
Terai, M. et al. Early induction of interleukin-5 and peripheral eosinophilia in acute pneumonia in Japanese children infected by pandemic 2009 influenza A in the Tokyo area. Microbiol. Immunol. 55, 341–346 (2011).
Seo, S.U. et al. Type I interferon signaling regulates Ly6Chi monocytes and neutrophils during acute viral pneumonia in mice. PLoS Pathog. 7, e1001304 (2011).
Chang, Y.J. et al. Innate lymphoid cells mediate influenza-induced airway hyper-reactivity independently of adaptive immunity. Nat. Immunol. 12, 631–638 (2011).
Reynolds, L.A., Filbey, K.J. & Maizels, R.M. Immunity to the model intestinal helminth parasite Heligmosomoides polygyrus. Semin. Immunopathol. 34, 829–846 (2012).
Brickshawana, A., Shapiro, V.S., Kita, H. & Pease, L.R. Lineage−Sca1+c-Kit−CD25+ cells are IL-33-responsive type 2 innate cells in the mouse bone marrow. J. Immunol. 187, 5795–5804 (2011).
Mjösberg, J. et al. The transcription factor GATA3 is essential for the function of human type 2 innate lymphoid cells. Immunity 37, 649–659 (2012).
Trinchieri, G. Type I interferon: friend or foe? J. Exp. Med. 207, 2053–2063 (2010).
Gupta, S., Jiang, M. & Pernis, A.B. IFN-α activates Stat6 and leads to the formation of Stat2:Stat6 complexes in B cells. J. Immunol. 163, 3834–3841 (1999).
Huber, J.P. & Farrar, J.D. Regulation of effector and memory T-cell functions by type I interferon. Immunology 132, 466–474 (2011).
Diefenbach, A. et al. Type 1 interferon (IFNα/β) and type 2 nitric oxide synthase regulate the innate immune response to a protozoan parasite. Immunity 8, 77–87 (1998).
Barlow, J.L. et al. IL-33 is more potent than IL-25 in provoking IL-13-producing nuocytes (type 2 innate lymphoid cells) and airway contraction. J. Allergy Clin. Immunol. 132, 933–941 (2013).
Murray, P.J. et al. Macrophage activation and polarization: nomenclature and experimental guidelines. Immunity 41, 14–20 (2014).
Duffield, J.S., Lupher, M., Thannickal, V.J. & Wynn, T.A. Host responses in tissue repair and fibrosis. Annu. Rev. Pathol. 8, 241–276 (2013).
Kumamoto, Y. et al. CD301b+ dermal dendritic cells drive T helper 2 cell-mediated immunity. Immunity 39, 733–743 (2013).
Murakami, R. et al. A unique dermal dendritic cell subset that skews the immune response toward Th2. PLoS ONE 8, e73270 (2013).
Motomura, Y. et al. Basophil-derived interleukin-4 controls the function of natural helper cells, a member of ILC2s, in lung inflammation. Immunity 40, 758–771 (2014).
Sweeney, C.M. et al. IL-27 mediates the response to IFN-beta therapy in multiple sclerosis patients by inhibiting Th17 cells. Brain Behav. Immun. 25, 1170–1181 (2011).
García-Sastre, A. et al. The role of interferon in influenza virus tissue tropism. J. Virol. 72, 8550–8558 (1998).
Price, G.E., Gaszewska-Mastarlarz, A. & Moskophidis, D. The role of α/β and γ interferons in development of immunity to influenza A virus in mice. J. Virol. 74, 3996–4003 (2000).
Blazejewska, P. et al. Pathogenicity of different PR8 influenza A virus variants in mice is determined by both viral and host factors. Virology 412, 36–45 (2011).
Kernbauer, E., Ding, Y. & Cadwell, K. An enteric virus can replace the beneficial function of commensal bacteria. Nature 516, 94–98 (2014).
Rankin, L.C. et al. The transcription factor T-bet is essential for the development of NKp46+ innate lymphocytes via the Notch pathway. Nat. Immunol. 14, 389–395 (2013).
Sciumé, G. et al. Distinct requirements for T-bet in gut innate lymphoid cells. J. Exp. Med. 209, 2331–2338 (2012).
Klose, C.S. et al. A T-bet gradient controls the fate and function of CCR6-RORγt+ innate lymphoid cells. Nature 494, 261–265 (2013).
Hunter, C.A. & Kastelein, R. Interleukin-27: balancing protective and pathological immunity. Immunity 37, 960–969 (2012).
Moro, K. et al. Interferon and IL-27 antagonize the function of group 2 innate lymphoid cells and type 2 innate immune responses. Nat. Immunol. 10.1038/ni.3309 (23 November 2015).
Kumar, A. & Ghosh, B. A single nucleotide polymorphism (A → G) in intron 3 of IFNγ gene is associated with asthma. Genes Immun. 9, 294–301 (2008).
Pinto, L.A. et al. STAT1 gene variations, IgE regulation and atopy. Allergy 62, 1456–1461 (2007).
Nakao, F. et al. Association of IFN-γ and IFN regulatory factor 1 polymorphisms with childhood atopic asthma. J. Allergy Clin. Immunol. 107, 499–504 (2001).
Kroegel, C. et al. Interferon-alphacon-1 treatment of three patients with severe glucocorticoid-dependent asthma. Effect on disease control and systemic glucocorticosteroid dose. Respiration 73, 566–570 (2006).
Gaush, C.R. & Smith, T.F. Replication and plaque assay of influenza virus in an established line of canine kidney cells. Appl. Microbiol. 16, 588–594 (1968).
Ruest, A., Michaud, S., Deslandes, S. & Frost, E.H. Comparison of the Directigen flu A+B test, the QuickVue influenza test, and clinical case definition to viral culture and reverse transcription-PCR for rapid diagnosis of influenza virus infection. J. Clin. Microbiol. 41, 3487–3493 (2003).
Ward, C.L. et al. Design and performance testing of quantitative real time PCR assays for influenza A and B viral load measurement. J. Clin. Virol. 29, 179–188 (2004).
Flaczyk, A. et al. IL-33 signaling regulates innate and adaptive immunity to Cryptococcus neoformans. J. Immunol. 191, 2503–2513 (2013).
Kaufman, G.N. et al. Intravenous immunoglobulin attenuates airway hyperresponsiveness in a murine model of allergic asthma. Clin. Exp. Allergy 41, 718–728 (2011).
Maazi, H. et al. ICOS:ICOS-ligand interaction is required for type 2 innate lymphoid cell function, homeostasis, and induction of airway hyperreactivity. Immunity 42, 538–551 (2015).
Acknowledgements
We thank J.L. Gommerman (University of Toronto) for Ifnar1−/− (Ifnar1tm1Agt) mice; D. Xue and G.A. Kaufman for help with AHR measurements; and B. Charbonneau for technical support. Supported by the Canadian Institutes of Health Research (J.H.F. and C.U.D.; MOP-114972 for the J.H.F. laboratory; postdoctoral fellowship for C.U.D.; MOP-89821 operating funds for S.M.V.), the Canadian Foundation of Innovation (Leaders Opportunity Fund infrastructure grant for the J.H.F. laboratory), the German National Academy of Sciences Leopoldina (C.U.D.), The American Association of Immunologists Careers in Immunology Fellowship Program (J.H.F. and C.U.D.) and Canada Research Chair in Host Responses to Virus Infections (S.M.V.).
Author information
Authors and Affiliations
Contributions
C.U.D. and J.H.F. designed the conceptual framework of the study, designed experiments and wrote the paper; C.U.D., C.D.A.M. and B.C.M. designed and performed experiments and analyzed data; M.R. and M.S. performed experiments with human ILC2 cells and helped to design and interpret experiments; A.P.M. and I.L.K. provided H. polygyrus, performed infections and helped to design and interpret experiments; J.P. and S.M.V. provided influenza virus and helped to design and interpret experiments; M.M.E. and D.M. provided STAT4-mutant mice; J.-F.G. provided reagents and expertise for experiments with IL-27; S.T.Q. provided STAT1-deficient BM; B.D.M. provided equipment and expertise for AHR measurements; K.L.M. provided IRF9-deficient BM; A.M.G. provided STAT1- and STAT2-deficient BM; and all authors provided input throughout the study and the writing of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Integrated supplementary information
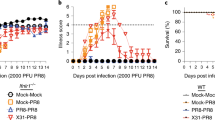
Supplementary Figure 1 Wild-type and Ifnar1−/− mice recover from infection with a low dose of IAV equally well.
(a,b) WT and Ifnar1-/- mice (five age- and sex-matched animals per group) were either mock treated with PBS as a control or infected with 20 PFU of influenza virus. (a) Survival and (b) body weight loss were monitored throughout the course of infection. (c) Pulmonary expression of the non-structural 1 (Ns1) gene of influenza was determined by qRT-PCR 5, 10 and 15 days post infection. The bars represent the mean ± standard deviation of each cohort. Data are representative of two independent experiments; n.d., not detectable. (d-g) WT and Ifnar1-/- mice (three to seven age- and sex-matched animals per group) were either mock treated with PBS or infected intranasally with 20 PFU of influenza virus. Five days post infection lungs were perfused with PBS and the pulmonary expression levels of (d) IL1b, (e) Tnf and (f) Ccl2 were determined by qRT-PCR, and (g) the numbers of inflammatory monocytes were determined by flow cytometry. Data are representative of three independent experiments. The bars represent the mean ± standard deviation of triplicates of each cohort. The asterisks indicate statistically significant differences (*, p ≤ 0.05; **, p ≤ 0.01; ***, p ≤ 0.001). (h) WT and Ifnar1-/- mice (three to seven age- and sex-matched animals per group) were either mock treated with PBS or infected intranasally with 20 PFU of influenza virus. At indicated time points post infection lungs were perfused with PBS, homogenized, and the IL-33 content was determined by ELISA. Data are representative of two independent experiments. The bars represent the mean ± standard deviation of triplicates of each cohort. One-way ANOVA test including the Bonferroni’s multiple comparison was used to analyze statistical significance.
Supplementary Figure 2 IFNAR1 deficiency results in elevated innate and adaptive type 2 immunity upon infection with H. polygyrus.
(a,b) WT and Ifnar1-/- mice (three to five age- and sex-matched animals per group) were either mock treated with PBS as control (co) or infected with H. polygyrus (H. poly., 200 larvae/mouse). Counts of (a) neutrophils, eosinophils and (b) group 2 innate lymphoid cells (ILC2) in the lamina propria of the small intestine and (c) IgG1 and (d) IgE levels in sera of mice were determined five days post-infection (p.i.). Data are representative of two independent experiments. The asterisks indicate statistically significant differences (*, p ≤ 0.05; **, p ≤ 0.01).
Supplementary Figure 3 Isolation and ex vivo expansion of mouse BM-derived ILC2 cells.
(a) Schematic representation of isolation and ex vivo expansion of murine bone marrow-derived group 2 innate lymphoid cells. (b) Bone marrow cells were stained for Sca-1, CD117 (c-Kit), CD25, and for lineage markers (TCRβ, TCRγδ, CD3ɛ, Gr-1, CD11b, TER-119, B220, NK1.1, CD5, CD11c) and lineage-negative Sca-1+c-Kit-CD25+ group 2 innate lymphoid cells were enriched by flow cytometric cell sorting. (c) Purity and (d) expression of CD127, T1/ST2, ICOS, KLRG1, CD90.2 and Gata3 of sorted bone marrow-derived ILC2 was analyzed by flow cytometry. Cells were then cultured in the presence of IL-2, IL-7, IL-25, IL-33 (all at 50 ng/ml), and TSLP (20 ng/ml) for 15 days. Cells were given fresh medium and cytokines every two days and split into multiple wells when necessary to avoid excessive crowding, yielding an increase in ILC2 numbers of approximately 500-fold. The resulting cells were then seeded in fresh medium and allowed to rest in IL-2 and IL-7 (both at 10 ng/ml) for two days. Medium was removed from wells and rested cells were stimulated as necessary for up to five days.
Supplementary Figure 4 Type I interferon–mediated inhibition of the proliferation and cytokine production of ILC2 cells occurs independently of iNOS and STAT6.
Bone marrow cells from WT, inducible nitric oxide synthase (iNos)-deficient or Stat6-deficient mice were stimulated for five days in medium as a control or with IL‐7 and IL-33 (both at 10 ng/ml). IFN-β (25 or 500 U/ml) was added to some wells, as indicated. Proliferation of cells was measured by alamarBlue assay and cytokine production was assessed by ELISA of cell culture supernatants. The bars represent the mean ± standard deviation of triplicates of each cohort. Data are representative of three independent experiments. RFU, relative fluorescence units; n.d., not detectable; ns, not statistically significant (p > 0.05). The asterisks indicate statistically significant differences (*, p ≤ 0.05; **, p ≤ 0.01; ***, p ≤ 0.001).
Supplementary Figure 5 Type I interferon restrains mouse ILC2 cells.
(a,b) Sorted and expanded bone marrow-derived ILC2 from WT mice were stimulated for five days with IL‐7 and IL-33 (both at 10 ng/ml) only (black bars) or with IL‐7 and IL-33 (both at 10 ng/ml) in combination with IFN-β (500 U/ml; red bars). (a) IFN-β was added at different time points (0h, 24h, 48h and 72h) and left in the culture until supernatants were taken. (b) IFN-β was added at the beginning of the culture (0h) and at different time points (not removed, 24h, 48h and 72h) cells were washed and re-seeded with IL‐7 and IL-33 (both at 10 ng/ml) only until supernatants were taken. Five days after culture proliferation of cells was measured by alamarBlue assay and cytokine production was determined by ELISA. The percentages of reduction due to the addition of IFN-β are shown in brackets above the red bars. Data are representative of two independent experiments. (c) Sorted and expanded bone marrow-derived ILC2 from WT mice were stimulated for three days with medium only, or with IL‐7 and IL-33 (both at 10 ng/ml). IFN-β (25 or 500 U/ml) was added to some wells as indicated. GATA3 expression was determined by intracellular flow cytometry staining and histograms and the ratio of the GATA3 mean fluorescence intensities (MFI) to the MFI of the internal isotype control stainings are shown. Data are representative of three independent experiments. (d) Sorted and expanded bone marrow-derived ILC2 from WT mice were stimulated for five days with IL‐7 and IL-33 (both at 10 ng/ml) only (black bars) or with IL‐7 and IL-33 (both at 10 ng/ml) in combination with IFN-β (500 U/ml; red bars). IFN-β was added at the beginning of the culture (0h) and at different time points (24h, 48h and 72h) cells were washed and re-seeded with IL‐7 and IL-33 (both at 10 ng/ml) only until supernatants were taken. Five days after culture GATA3 expression was determined by intracellular flow cytometry staining and the ratio of the GATA3 MFI to the MFI of the internal isotype control stainings are shown. Data are representative of two independent experiments. The bars represent the mean ± standard deviation of triplicates of each cohort. The asterisks indicate statistically significant differences (*, p ≤ 0.05; **, p ≤ 0.01; ***, p ≤ 0.001). RFU, relative fluorescence units.
Supplementary Figure 6 Type I interferon restrains IL-33-mediated inflammation.
(a) Schematic model of cytokine administration protocol. WT mice (five age- and sex-matched animals per group) were challenged intranasally with PBS as control, IFNβ, IL-33, or IL-33 + IFN-β for three consecutive days. 24 hours after the last treatment pulmonary expression of (b) Il6, (c) Ccl17, (d) Ccl22, (e) Chi3l3, (f) Fn1 and (g) Ccl24 was determined by qRT-PCR. Data are representative of two independent experiments. (h,i) WT mice (five age- and sex-matched animals per group) were challenged intranasally with phosphate buffered saline (PBS) as a control, IFN-β, IL-33, or IL-33 + IFN-β for three consecutive days. 24 hours after the last treatment pulmonary cytokine expression and cellular composition of lungs were analyzed. (h) Expression of cell surface CD11c of pulmonary eosinophils was determined by flow cytometry. After setting singlet gate, viable eosinophils were further defined as SiglecF+CD11c-. The frequencies of eosinophils are highlighted in the red gates. (i) The mean fluorescence intensities (MFI) of cell surface CD11c expression by eosinophils are shown. The bars represent the mean ± standard deviation of each cohort. Data are representative of two independent experiments. The asterisks indicate statistically significant differences (*, p ≤ 0.05; **, p ≤ 0.01; ***, p ≤ 0.001).
Supplementary Figure 7 IFN-γ-mediated inhibition of the proliferation and cytokine production of ILC2 cells occurs independently of STAT2, IRF9, IFNAR, STAT4, T-bet, iNOS and STAT6.
Bone marrow cells from (a) WT and Stat2-/-, (b) WT and Irf9-/-, (c) WT and Ifnar1-/-, (d) WT and Stat4-mutant, (e) WT and Tbx21-/-, (f) WT, iNos-/- and Stat6-/- mice were stimulated for five days in medium as a control or with IL‐7 and IL-33 (both at 10 ng/ml). IFN-γ (5 or 20 ng/ml) was added to some wells, as indicated. Proliferation of cells was measured by alamarBlue assay, cytokine production was determined by ELISA of cell culture supernatants. The bars represent the mean ± standard deviation of triplicates of each cohort. Data are representative of three independent experiments. RFU, relative fluorescence units; n.d., not detectable; ns, not statistically significant (p > 0.05). The asterisks indicate statistically significant differences (*, p ≤ 0.05; **, p ≤ 0.01; ***, p ≤ 0.001).
Supplementary Figure 8 Type II interferon restrains IL-33-mediated inflammation.
Wild type (WT) C57BL/6 mice (five age- and sex-matched animals per group) were challenged intranasally with PBS as control, IFN-γ, IL-33, or IL-33 + IFN-γ for three consecutive days. 24 hours after the last treatment pulmonary expression of (a) Il6, (b) Ccl17, (c) Ccl22, (d) Chi3l3, (e) Fn1 and (f) Ccl24 was determined by qRT-PCR. The bars represent the mean ± standard deviation of each cohort. Data are representative of two independent experiments. The asterisks indicate statistically significant differences (*, p ≤ 0.05; **, p ≤ 0.01; ***, p ≤ 0.001).
Supplementary information
Supplementary Text and Figures
Supplementary Figures 1–8 and Supplementary Tables 1 and 2 (PDF 1799 kb)
Rights and permissions
About this article
Cite this article
Duerr, C., McCarthy, C., Mindt, B. et al. Type I interferon restricts type 2 immunopathology through the regulation of group 2 innate lymphoid cells. Nat Immunol 17, 65–75 (2016). https://doi.org/10.1038/ni.3308
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ni.3308
This article is cited by
-
A diversity of novel type-2 innate lymphoid cell subpopulations revealed during tumour expansion
Communications Biology (2024)
-
Evaluation of serum levels of interferon beta and nucleotide binding and oligomerization domain 2 gene polymorphism in children with cough asthma phenotype: a case–control study
Egyptian Pediatric Association Gazette (2023)
-
The modulation of pulmonary group 2 innate lymphoid cell function in asthma: from inflammatory mediators to environmental and metabolic factors
Experimental & Molecular Medicine (2023)
-
HIF-PHD inhibitor regulates the function of group2 innate lymphoid cells and polarization of M2 macrophages
Scientific Reports (2023)
-
Solar ultraviolet B radiation promotes α-MSH secretion to attenuate the function of ILC2s via the pituitary–lung axis
Nature Communications (2023)