Abstract
Background:
Active surveillance (AS) is an increasingly important attempt to avoid overtreatment of patients who harbor clinically insignificant disease while offering curative treatment to those in whom disease is reclassified as higher risk after an observation period and repeat biopsy. We aim to evaluate the diagnostic performance of magnetic resonance imaging (MRI) in predicting upgrading on confirmatory biopsy in men with low-risk prostate cancer (PCa) on AS.
Methods:
We searched the PubMed for pertinent studies up to November 2014. We used standard methods recommended for meta-analyses of diagnostic test evaluations. The analysis was based on a summary receiver operating characteristic (SROC) curve. Meta-regression analysis was used to assess the effects of some confounding factors on the results of the meta-analysis. The potential presence of publication bias was tested using the Deeks’ funnel plots.
Results:
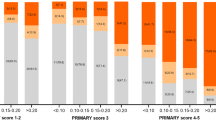
Seven studies provided the diagnostic data on MRI and AS of PCa, comprising 1028 patients. The pooled estimates of MRI on disease reclassification among AS candidates were as follows: sensitivity, 0.69 (95% confidence interval (CI), 0.44–0.86); specificity, 0.78 (95% CI, 0.53–0.91); positive likelihood ratio, 3.1 (95% CI, 1.6–6.0); negative likelihood ratio, 0.40 (95% CI, 0.23–0.70); and diagnostic odds ratio, 8 (95% CI, 4–16). The P-value for heterogeneity was <0.001. We found that the SROC curve is positioned toward the desirable upper left corner of the curve, and the area under the curve was 0.79 (95% CI, 0.76–0.83). For a pretest probability of 0.20, the corresponding positive predictive value (PPV) was 0.44 and the negative predictive value (NPV) was 0.91. MRI may reveal an unrecognized significant lesion in 33.27% of patients, and biopsy of these areas reclassified 14.59% of cases as no longer fulfilling the criteria for AS. In addition, when no suspicious disease progression (66.34%) was identified on MRI, the chance of reclassification on repeat biopsy was extremely low at 6.13%.
Conclusions:
MRI, especially multiparametric (MP)-MRI, has a moderate diagnostic accuracy as a significant predictor of disease reclassification among AS candidates. The high NPV and specificity for the prediction of biopsy reclassification upon clinical follow-up suggest that negative prostate MRI findings may support a patient remaining under AS. Although the PPV and sensitivity for the prediction were relatively low, the presence of a suspicious lesion >10 mm lesion may suggest an increased risk for disease progression.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Jemal A, Siegel R, Ward E, Hao Y, Xu J, Murray T et al. Cancer statistics. 2008 CA Cancer J Clin 2008; 58: 71–96.
Sanda MG, Dunn RL, Michalski J, Sandler HM, Northouse L, Hembroff L et al. Quality of life and satisfaction with outcome among prostate cancer survivors. N Engl J Med 2008; 358: 1250–1261.
Ukimura O, Faber K, Gill IS . Intraprostatic targeting. Curr Opin Urol 2012; 22: 97–103.
Warlick C, Trock BJ, Landis P, Epstein JI, Carter HB . Delayed versus immediate surgical intervention and prostate cancer outcome. J Natl Cancer Inst 2006; 98: 355–357.
Klotz L, Zhang L, Lam A, Nam R, Mamedov A, Loblaw A . Clinical results of long-term follow-up of a large, active surveillance cohort with localized prostate cancer. J Clin Oncol 2010; 28: 126–131.
NCCN Guidelines and Clinical Resources. Updated Prostate Cancer Guidelines, vs 2.2014. National Comprehensive Cancer Network. Available at http://www.nccn.org/professionals/physician_gls/pdf/prostate.pdf. Accessed April 2014.
Porten SP, Whitson JM, Cowan JE, Cooperberg MR, Shinohara K, Perez N et al. Changes in prostate cancer grade on serial biopsy in men undergoing active surveillance. J Clin Oncol 2011; 29: 2795–2800.
Tosoian JJ, Trock BJ, Landis P, Feng Z, Epstein JI, Partin AW et al. Active surveillance program for prostate cancer: an update of the Johns Hopkins experience. J Clin Oncol 2011; 29: 2185–2190.
Ross AE, Loeb S, Landis P, Partin AW, Epstein JI, Kettermann A et al. Prostate-specific antigen kinetics during follow-up are an unreliable trigger for intervention in a prostate cancer surveillance program. J Clin Oncol 2010; 28: 2810–2816.
Loeb S, Carter HB, Berndt SI, Ricker W, Schaeffer EM . Complications after prostate biopsy: data from SEER-Medicare. J Urol 2011; 186: 1830–1834.
Fujita K, Landis P, McNeil BK, Pavlovich CP . Serial prostate biopsies are associated with an increased risk of erectile dysfunction in men with prostate cancer on active surveillance. J Urol 2009; 182: 2664–2669.
Zhang J, Hricak H, Shukla-Dave A, Akin O, Ishill NM, Carlino LJ et al. Clinical stage T1c prostate cancer: evaluation with endorectal MR imaging and MR spectroscopic imaging. Radiology 2009; 253: 425–434.
Shukla-Dave A, Hricak H, Kattan MW, Pucar D, Kuroiwa K, Chen HN et al. The utility of magnetic resonance imaging and spectroscopy for predicting insignificant prostate cancer: an initial analysis. BJU Int 2007; 99: 786–793.
Delongchamps NB, Beuvon F, Eiss D, Flam T, Muradyan N, Zerbib M et al. Multiparametric MRI is helpful to predict tumor focality, stage, and size in patients diagnosed with unilateral low-risk prostate cancer. Prostate Cancer Prostatic Dis 2011; 14: 232–237.
Whiting P, Rutjes AW, Reitsma JB, Bossuyt PM, Kleijnen J . The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol 2003; 3: 25.
Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB et al. QUADAS-2 Group. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 2011; 155: 529–536.
Glas AS, Lijmer JG, Prins MH, Bonsel GJ, Bossuyt PM . The diagnostic odds ratio: a single indicator of test performance. J Clin Epidemiol 2003; 56: 1129–1135.
Deeks JJ . Systematic reviews in health care: systematic reviews of evaluations of diagnostic and screening tests. BMJ 2001; 323: 157–162.
Tang BM, Eslick GD, Craig JC, McLean AS . Accuracy of procalcitonin for sepsis diagnosis in critically ill patients: systematic review and meta-analysis. Lancet Infect Dis 2007; 7: 210–217.
Moses LE, Shapiro D, Littenberg B . Combining independent studies of a diagnostic test into a summary ROC curve: data-analytic approaches and some additional considerations. Stat Med 1993; 12: 1293–1316.
Lijmer JG, Bossuyt PM, Heisterkamp SH . Exploring sources of heterogeneity in systematic reviews of diagnostic tests. Stat Med 2002; 21: 1525–1537.
Rutter CM, Gatsonis CA . A hierarchical regression approach to meta-analysis of diagnostic test accuracy evaluations. Stat Med 2001; 20: 2865–2884.
Deeks JJ, Macaskill P, Irwig L . The performance of tests of publication bias and other sample size effects in systematic reviews of diagnostic test accuracy was assessed. J Clin Epidemiol 2005; 58: 882–893.
Ziakas PD, Poulou LS, Voulgarelis M, Thanos L . The Gordian knot of interim 18-fluorodeoxyglucose positron emission tomography for Hodgkin lymphoma: a meta-analysis and commentary on published studies. Leuk Lymphoma 2012; 53: 2166–2174.
Dwamena BA . Evidence-based radiology: step 3—diagnostic systematic review and meta-analysis (critical appraisal). Semin Roentgenol 2009; 44: 170–179.
Vargas HA, Akin O, Afaq A, Goldman D, Zheng J, Moskowitz CS et al. Magnetic resonance imaging for predicting prostate biopsy findings in patients considered for active surveillance of clinically low risk prostate cancer. J Urol 2012; 188: 1732–1738.
Fradet V, Kurhanewicz J, Cowan JE, Karl A, Coakley FV, Shinohara K et al. Prostate cancer managed with active surveillance: role of anatomic MR imaging and MR spectroscopic imaging. Radiology 2010; 256: 176–183.
Stamatakis L, Siddiqui MM, Nix JW, Logan J, Rais-Bahrami S, Walton-Diaz A et al. Accuracy of multiparametric magnetic resonance imaging in confirming eligibility for active surveillance for men with prostate cancer. Cancer 2013; 119: 3359–3366.
Vasarainen H, Lahdensuo K, Savolainen R, Ruutu M, Taari K, Rannikko A . Diffusion-weighted magnetic resonance imaging in prostate cancer patients on active surveillance one year after diagnosis and before repeat biopsy. Scand J Urol 2013; 47: 456–461.
Margel D, Yap SA, Lawrentschuk N, Klotz L, Haider M, Hersey K et al. Impact of multiparametric endorectal coil prostate magnetic resonance imaging on disease reclassification among active surveillance candidates: a prospective cohort study. J Urol 2012; 187: 1247–1252.
Mullins JK, Bonekamp D, Landis P, Begum H, Partin AW, Epstein JI et al. Multiparametric magnetic resonance imaging findings in men with low-risk prostate cancer followed using active surveillance. BJU Int 2013; 111: 1037–1045.
Bonekamp D, Bonekamp S, Mullins JK, Epstein JI, Carter HB, Macura KJ . Multiparametric magnetic resonance imaging characterization of prostate lesions in the active surveillance population: incremental value of magnetic resonance imaging for prediction of disease reclassification. J Comput Assist Tomogr 2013; 37: 948–956.
Zamora J, Abraira V, Muriel A, Khan K, Coomarasamy A . Meta-DiSc: a software for meta-analysis of test accuracy data. BMC Med Res Methodol 2006; 6: 31.
Swets JA . Measuring the accuracy of diagnostic systems. Science 1988; 240: 1285–1293.
Siadaty MS, Shu J . Proportional odds ratio model for comparison of diagnostic tests in meta-analysis. BMC Med Res Methodol 2004; 4: 27.
Siddiqui MM, Rais-Bahrami S, Truong H, Stamatakis L, Vourganti S, Nix J et al. Magnetic resonance imaging/ultrasound-fusion biopsy significantly upgrades prostate cancer versus systematic 12-core transrectal ultrasound biopsy. Eur Urol 2013; 64: 713–719.
Da Rosa MR, Milot L, Sugar L, Vesprini D, Chung H, Loblaw A et al. A prospective comparison of MRI-US fused targeted biopsy versus systematic ultrasound-guided biopsy for detecting clinically significant prostate cancer in patients on active surveillance. J Magn Reson Imaging 2015; 41: 220–225.
Shah ZK, Elias SN, Abaza R, Zynger DL, DeRenne LA, Knopp MV et al. Performance comparison of 1.5-T endorectal coil MRI with 3.0-T nonendorectal coil MRI in patients with prostate cancer. Acad Radiol 2015; 22: 467–474.
Cabrera AR, Coakley FV, Westphalen AC, Lu Y, Zhao S, Shinohara K et al. Prostate cancer: is inapparent tumor at endorectal MR and MR spectroscopic imaging a favorable prognostic finding in patients who select active surveillance? Radiology 2008; 247: 444–450.
van As NJ, de Souza NM, Riches SF, Morgan VA, Sohaib SA, Dearnaley DP et al. A study of diffusion-weighted magnetic resonance imaging in men with untreated localised prostate cancer on active surveillance. Eur Urol 2008; 56: 981–987.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflicts of interst.
Rights and permissions
About this article
Cite this article
Guo, R., Cai, L., Fan, Y. et al. Magnetic resonance imaging on disease reclassification among active surveillance candidates with low-risk prostate cancer: a diagnostic meta-analysis. Prostate Cancer Prostatic Dis 18, 221–228 (2015). https://doi.org/10.1038/pcan.2015.20
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pcan.2015.20
This article is cited by
-
Imaging for prostate cancer: reimbursements
Abdominal Radiology (2020)
-
MRI in active surveillance: a critical review
Prostate Cancer and Prostatic Diseases (2019)
-
The role of Prostate Imaging Reporting and Data System score in Gleason 3 + 3 active surveillance candidates enrollment: a diagnostic meta-analysis
Prostate Cancer and Prostatic Diseases (2019)
-
Role of multiparametric magnetic resonance imaging for patients under active surveillance for prostate cancer: a systematic review with diagnostic meta-analysis
Prostate Cancer and Prostatic Diseases (2019)
-
ProPSA and the Prostate Health Index as predictive markers for aggressiveness in low-risk prostate cancer—results from an international multicenter study
Prostate Cancer and Prostatic Diseases (2017)