Abstract
Background
Alveolar capillary dysplasia with misalignment of pulmonary veins (ACD/MPV) is a lethal congenital lung disorder associated with heterozygous variants in the FOXF1 gene or its regulatory region. Patients with ACD/MPV unnecessarily undergo invasive and expensive treatments while awaiting a diagnosis. The aim of this study was to reduce the time to diagnose ACD/MPV by developing a targeted next-generation sequencing (NGS) panel that detects FOXF1 variants.
Methods
A FOXF1-targeted NGS panel was developed for detection of mutations and large genomic alterations and used for retrospective testing of ACD/MPV patients and controls. Results were confirmed with Sanger sequencing and SNP array analysis.
Results
Each amplicon of the FOXF1-targeted NGS panel was efficiently sequenced using DNA isolated from blood or cell lines of 15 ACD/MPV patients and 8 controls. Moreover, testing of ACD/MPV patients revealed six novel and six previously described pathogenic or likely pathogenic FOXF1 alterations.
Conclusion
We successfully designed a fast and reliable targeted genetic test to detect variants in the FOXF1 gene and its regulatory region in one run. This relatively noninvasive test potentially prevents unnecessary suffering for patients and reduces the use of futile and expensive treatments like extra-corporeal membrane oxygenation.
Impact
-
FOXF1-targeted NGS potentially prevents ACD/MPV patients from unnecessary suffering and expensive treatments.
-
FOXF1-targeted NGS potentially reduces the number of misdiagnosis in ACD/MPV patients.
-
Retrospective testing of ACD/MPV patients using FOXF1-targeted NGS revealed six novel pathogenic or likely pathogenic variants.
Similar content being viewed by others
Introduction
Patients with alveolar capillary dysplasia with misalignment of pulmonary veins (ACD/MPV) unnecessarily undergo invasive and expensive treatments while awaiting a diagnosis. Patients with this rare and lethal congenital lung disorder usually present shortly after birth with respiratory distress caused by therapy-resistant pulmonary hypertension (PH) and insufficient oxygen uptake. In addition, 80% of the patients suffer from malformations in the gastrointestinal, urogenital or cardiovascular system.1 Currently, ACD/MPV can only be confirmed by histological examination of the lung, which is characterized by alveolar septal thickening, reduced numbers of alveolar capillaries, peripheral arterial wall hypertrophy and, in most patients, misaligned pulmonary veins (MPV).1,2 Although most neonatologists and pediatric pulmonologists are aware of this disorder, ACD/MPV is not always recognized timely and patients receive multiple futile therapies directed at the PH such as antihypertensive pharmacotherapy and extra-corporeal membrane oxygenation (ECMO). If necessary, additional surgeries are carried out for co-malformations. Due to the risks of an open lung biopsy, especially during anticoagulation while on ECMO, it takes several days to weeks before the decision is made to take a biopsy. Moreover, retrospective studies have shown that most patients are diagnosed post-mortem by autopsy1,3,4,5 and there is a high probability that many patients are not diagnosed at all. While histology is the gold standard for diagnosis of ACD/MPV, increased availability of noninvasive genetic testing makes it possible to obtain a genetic diagnosis in infants with respiratory failure and severe pulmonary hypertension, especially in the setting of congenital anomalies. To minimize the unnecessary suffering for both patients and parents, as well as reducing the use of ineffective, expensive and futile therapies, this study was aimed at developing a fast and specific genetic test to shorten the time between hospitalization and diagnosing ACD/MPV.
ACD/MPV is primarily caused by haploinsufficiency of Forkhead Box F1 (FOXF1), which is a transcription factor that plays a role in early embryonic lung development.6,7 Genomic alterations detected in ACD/MPV patients are either point mutations or indels in the FOXF1 gene or large copy number variations (CNVs) involving the gene or its 60-kilobase pair (kb) regulatory region.7,8,9,10 Therefore, genetic testing of ACD/MPV patients requires a combination of Sanger sequencing with SNP array or array comparative genomic hybridization (aCGH). To detect the different ACD/MPV variants in one run, whole-genome sequencing (WGS) can be used. However, this technique is expensive and provides an excessive amount of information about the whole genome, which takes a long time to be analyzed and might lead to incidental findings. Furthermore, whole-exome sequencing (WES) is not sufficient to detect CNVs in the regulatory region and the same applies to the available NGS panels that include the FOXF1 gene.11 In this study, we present a new targeted next-generation sequencing (NGS) panel to identify variants associated to ACD/MPV in one run. This testing method is fast, cost-effective and prevents unwanted incidental findings in other regions of the genome. Further, by routine testing of DNA samples from ACD/MPV patients, new genomic alterations involving the FOXF1 locus could be identified which contributes to the knowledge on the complex pathogenesis of ACD/MPV.
Methods
Sample collection
Blood samples, cell lines and formalin-fixed and paraffin-embedded (FFPE) lung tissues of patients with histologically confirmed ACD/MPV were collected from the Sophia Children’s Hospital—Erasmus University Medical Center Rotterdam, the Radboudumc Amalia Children’s Hospital Nijmegen, the VU University Medical Center Amsterdam, the Hospital for Sick Children Toronto, the University Hospitals Leuven and the Charles University and General University Hospital in Prague. Blood samples of age-matched controls without ACD/MPV were collected from the Sophia Children’s Hospital—Erasmus University Medical Center Rotterdam. In this study, we only used bodily material that was previously obtained for diagnostic purposes. All samples were anonymized before genetic testing was performed. Before the start of the study, the research proposal was reviewed and approved by the Daily Board of the Medical Ethics Committee (METC) Erasmus University Medical Center Rotterdam, The Netherlands.
NGS with the ACD/MPV panel
A specific ACD/MPV panel was designed with the Ion Ampliseq Designer 6.0 (ThermoFisher Scientific, Waltham, MA, USA) and included 157 amplicons targeted at the FOXF1 gene and its regulatory region. To enable detection of CNVs, 119 amplicons were designed to cover selected single nucleotide polymorphisms (SNPs) with a minor allele frequency (MAF) above 0.4.12 The majority of these 119 SNPs were selected in and around the FOXF1 gene and its regulatory region, with a distance of 50−500 base pairs (bp) between the SNPs. The other SNPs were located across the remaining parts of chromosome 16 with a distance of approximately 2−4 megabase pairs (Mb). For the detection of single nucleotide substitutions and small deletions or duplications in the FOXF1 gene, 38 overlapping amplicons were designed that together cover the FOXF1 gene. The final library was constructed with the AmpliSeq Library Kit 2.0 (ThermoFisher Scientific), according to the manufacturer’s instructions. The sequences and coverages were analyzed with the Ion S5 XL Sequencing System and the Torrent Suite Software v5.6 (ThermoFisher Scientific) as described previously.13 Due to the high GC-content, the first 6 bp at the start of exon 1 could not be covered by amplicons, as well as a 187 bp strech in the 3′ untranslated region (UTR). These regions were additionally sequenced with Sanger sequencing.
Staining
The pathologists affiliated to the providing hospitals confirmed ACD/MPV by histological examination of lung tissue at the time of diagnosis. To review the diagnosis of patients without FOXF1 alterations, an additional immunohistochemical staining was performed with hematoxylin-eosin (HE) and CD31 (JC70 clone) (Cell Marque, Rocklin, CA, USA) at the Department of Pathology of the Erasmus Medical Center. The staining was performed with ready-to-use antibodies on a Benchmark Ultra system, using an Ultraview Dab kit for visualization (all from Ventana Medical Systems, Oro Vally, AZ, USA).
DNA isolation
To isolate DNA from skin fibroblasts or FFPE lung tissues, the QIAamp DNA Mini Kit (Qiagen, Hilden, Germany) was used according to the manufacturer’s instructions. For DNA isolation from FFPE lung tissue, 8−10 sections of 10 µm were pretreated with xylene to remove the paraffin and with sodium thiocyanate to permeabilize the tissue. To isolate DNA from blood, the Chemagic DNA Blood Kit special (PerkinElmer chemagen Technology, Baesweiler, Germany), the Gentra Puregene Blood Kit (Qiagen) or the “Salting out” method14 was used. DNA concentrations were measured with the Quant-iT Picogreen assay kit (ThermoFisher Scientific) according to the manufacturer’s instructions.
Variant analysis
Single nucleotide substitutions, small deletions and small duplications were identified with the Variant Caller v5.6 plugins (ThermoFisher Scientific) and summarized in Variant Caller Files. Variants were notated as potential disease causing variants if they were present in more than 30% of the sequencing reads and located in one of the exons, the 3′ UTR or the 5′ UTR. Variants were excluded if they have been reported with an MAF above 1% in the 1000 Genomes-, UCSC common SNP 151-, ExAc-, GONL-, ESP-, gnomAD- or SwissProt Variants databases. Additionally, the FOXF1 gene was manually checked for variants with the Integrative Genomic Viewer.15 Variants were described as recommended by the Human Genome Variation Society16 and classified according to the guidelines of the American College of Medical Genetics and Genomics.17 For classification, the following in silico prediction algorithms were used: PolyPhen-2, MutationTaster, SIFT Align Protein Sequences, PANTHER and GeneSplicer. If parental DNA was available, it was used for Sanger sequencing to determine whether the variants arose de novo or were inherited from one of the parents.
CNV analysis
CNVs were identified by analyzing the percentages of sequencing reads per amplicon and allele frequencies of the common SNPs, using the Torrent Suite Software v5.6 (ThermoFisher Scientific) and Microsoft Excel (2010). Allele frequencies of the SNPs were obtained from the Variant Caller Files. A deletion was identified if multiple consecutive amplicons contained a lower percentage of reads than other samples, combined with loss of heterozygosity. A gain was called if multiple consecutive amplicons contained higher read percentages combined with an allelic imbalance. The coordinates of the CNVs are based on the 3′-end and the 5′-end of the amplicons that are located upstream and downstream of the amplicons with altered read counts. The CNVs were classified according to the joint consensus recommendation of the American College of Medical Genetics and Genomics (ACMG) and the Clinical Genome Resource (ClinGen) for interpretation and reporting of CNVs.18 If parental DNA was available, it was used for SNP array to determine on which allele the CNV arose.
Confirmation of the NGS results
The presence of small variants located in the FOXF1 gene was confirmed with Sanger sequencing using the 3730xl DNA Analyzer (Applied Biosystems, ThermoFisher Scientific) with custom-designed primers (primer sequences available upon request). Sequences were aligned and compared with the reference sequences GRCh37/hg19 from the Ensemble genome database (ENSG00000103241), using SeqScape Software v3.0 (Applied Biosystems, ThermoFisher Scientific). CNVs were confirmed with SNP array using the Infinium Global Screening Array v1.0 (Illumina, San Diego, CA, USA). Array results were analyzed with Nexus Software 9.0 (BioDiscovery, El Segundo, CA, USA).
Results
Sample collection
In total, we collected blood or skin fibroblasts of eight controls and 15 ACD/MPV patients (Table 1). The characteristic finding of misalignment of the pulmonary veins (MPV) was present in all these patients, except for patient 5. Control 1 was a sibling of ACD/MPV patient 3 and had several congenital malformations but no ACD/MPV. Controls 2 and 3 were neonates that suffered from congenital alveolar dysplasia (CAD). The five other controls were anonymous controls with normal lung histology. Furthermore, we collected 18 FFPE lung tissue samples of deceased ACD/MPV patients of whom no blood or cell lines were stored.
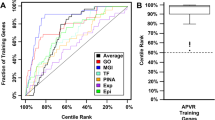
Identification of FOXF1 variants using targeted NGS
If DNA samples isolated from blood or cell lines were used, each amplicon of the NGS panel (Fig. 1) was sequenced more than ten times and the mean coverage per amplicon was above 1716. All genomic alterations found with the NGS panel corresponded to the genomic alterations found with Sanger sequencing and SNP array, indicating a sensitivity and specificity of 100% compared to current available techniques. In 11 (73%) of the 15 DNA samples isolated from blood or cell lines, we detected heterozygous FOXF1 alterations classified as pathogenic (P) or likely pathogenic (LP) (Table 1). Six of them were single nucleotide substitutions, small deletions or small duplications located in the first FOXF1 exon. The remaining five variants were CNVs of which one encompassed both the FOXF1 gene and its regulatory region, and four encompassed only the regulatory region. Two of the identified FOXF1 variants (g.86544531G > A, p.(Gly119Asp) and g.86544866_86544873del, p.(Ala231Argfs*61)) have been previously described by Sen et al.19 in other ACD/MPV patients (Table 1).
Since skin fibroblasts and blood samples of previously diagnosed ACD/MPV patients are limited, we also included four ACD/MPV patients of whom DNA was already tested with Sanger sequencing and aCGH in collaboration with the group of Stankiewicz in 201319,20 (Table 1). With the ACD/MPV NGS panel we confirmed the findings of the studies in 2013. However, in 2013, we included additional Sanger sequencing to investigate the exact breakpoints of the CNVs; therefore, the coordinates of the CNVs differ slightly from the results we show here (patients 3 and 4 of Table 1).20 Further, we showed in 2013 that these CNVs were located on the maternal allele.20 To investigate whether the other CNVs identified with the NGS panel were also located on the maternal allele, we performed SNP array on parental DNA. Indeed, the CNVs in patients 9 and 11 were also located on the maternal allele. Of patient 10, there was no parental DNA available for allele identification (Table 1).
In one patient we only detected a likely benign (LB) variant, and in three patients we could not detect any FOXF1 variants, neither by SNP array or Sanger sequencing. To make sure that these patients were not misdiagnosed, lung samples were re-examined by a specialized pathologist of the Erasmus University Medical Center who again confirmed ACD/MPV (Fig. 2).
Hematoxylin−eosin (top row) and CD31 staining on lung tissue of an age-matched control (a−c) and two ACD/MPV patients (d−f; g−i). ACD/MPV lung tissues demonstrate misalignment of pulmonary veins (MPV; asterisks) and disordered capillary networks in alveolar septa. In the DNA of ACD/MPV patient P_003854 (d−f), a deletion involving the FOXF1 regulatory region was found. In the DNA of ACD/MPV patient P_003890 (g−i), no FOXF1 alteration was found. Br bronchiole, arrows arterioles. Scale bars: 1 mm (a); 100 µm (c).
In one of the eight control samples, we detected two variants that were classified as LB. There were no FOXF1 alterations found in the other seven control samples.
To investigate whether this test can also be used when only FFPE tissue is available, we tested 18 DNA samples isolated from FFPE lung tissue. The use of these samples resulted in a large variability of sequencing depths between amplicons and between samples. Therefore, the read percentages could not be compared to each other and CNV analysis was not possible (Supplemental Fig. S1 (online)). Furthermore, multiple amplicons showed a low read depth (<10 reads) with the result that the FOXF1 gene was not fully sequenced in four samples. However, in one sample we could confirm a previously described mutation19 and in another sample we detected one novel mutation (Supplemental Table S1 (online)). Both mutations were confirmed with Sanger sequencing.
Discussion
In this study, our aim was to develop a new targeted NGS panel to detect genomic alterations associated with ACD/MPV which has the potential to reduce the time to diagnose ACD/MPV in clinical practice. Retrospective testing of ACD/MPV patients and controls showed that the panel works efficiently with DNA isolated from fresh tissue and resulted in identification of six novel and six previously described FOXF1 alterations classified as pathogenic or likely pathogenic.
Two of the previous described FOXF1 alterations were identified in other ACD/MPV patients. Interestingly, the clinical presentations differed between patients carrying the same mutation. For instance, patient 5 from the current study needed ECMO therapy directly at the start of symptoms, while the patient described by Sen et al. (patient 26) survived for 21 days without ECMO therapy.19 Furthermore, the patient from our study suffered from a bilateral hydronephrosis whereas the patient described by Sen et al.19 suffered from a megaduodenum, pyloric stenosis and an annular pancreas. In accordance with previous studies, these observations suggest that the severity of ACD/MPV and the extent of accompanying malformations cannot be correlated to specific FOXF1 variants.1,6 Recently, Szafranski et al.21 reported that the phenotypical differences might be caused by the presence or absence of rare single nucleotide variants located in the FOXF1 enhancer, which could result in different expressions of FOXF1. Furthermore, it has been suggested that parental imprinting of FOXF1 modulates FOXF1 expression.20,22 In line with earlier studies, the CNVs identified in the current study were located on the maternal allele and support that at least the regulatory region of FOXF1 is paternally imprinted.
Stated turn-around times for available FOXF1 genetic studies are generally longer than 2−3 weeks, in contrast to the 72 h for our approach using the NGS panel (Fig. 3a). Currently, ACD/MPV patients receive life supportive care and invasive treatments for several days to weeks while awaiting a diagnosis1 (Fig. 3b, left segment). By testing DNA isolated from a small blood sample with the NGS ACD/MPV panel, the time between hospitalization and diagnosis can be shortened (Fig. 3b, middle segment). The ACD/MPV panel is especially effective when a likely pathogenic or pathogenic alteration is found. This gives clinicians the chance to confirm the diagnosis earlier with lung biopsy and allows clinicians to better inform and counsel the parents.22 In the majority of patients, an earlier diagnosis leads to earlier treatment withdrawal and thus, reduces the use of invasive and expensive treatments like ECMO therapy.23 For exceptional ACD/MPV cases with an atypical less severe phenotype, lung transplantation might be an option.24,25 Based on the patient’s condition, one could argue to omit the lung biopsy if a likely pathogenic or pathogenic FOXF1 alteration is detected. Since the genotype−phenotype correlation is still not fully understood, we recommend to histologically confirm the diagnosis. Hopefully, future studies will clarify the mechanisms behind the genotype−phenotype relation with the result that eventually, genetic testing could obviate the need for a lung biopsy (Fig. 3b, right segment).
Illustration of the NGS steps within 72 h (a) Implementation of NGS with the ACD/MPV panel potentially reduces the time between hospitalization and diagnosis (b). LP likely pathogenic, P pathogenic, No LP/P all variants that are not classified as pathogenic or likely pathogenic, including variants of unknown significance, LT lung transplantation.
Given that ACD/MPV is a rare cause of PH in newborns, we recommend to continue therapy if there are no variants identified that can be classified as likely pathogenic or pathogenic (Fig. 3b, middle and right segment). However, our findings show that the absence of FOXF1 alterations does not always exclude ACD/MPV. Four of the 15 (27%) histologically confirmed ACD/MPV patients were negative for pathogenic or likely pathogenic FOXF1 alterations, even with additional testing by Sanger sequencing and SNP array. Since we are not the first group to describe ACD/MPV patients without pathogenic alterations in the FOXF1 region,9 these results suggest that the pathogenesis of ACD/MPV might involve epigenetic changes or genetic changes in other genes or regulatory regions. Therefore, a lung biopsy should still be performed if symptoms progress over time, especially when a variant of uncertain significance is found. In the absence of a FOXF1 alteration, further genome wide testing can contribute to the search for other genes or regulatory regions involved in the pathogenesis of ACD/MPV.
Additional to the care-related beneficial aspects of the ACD/MPV panel, it is also a cost-effective technique. For testing of DNA with the ACD/MPV panel, the Erasmus Medical Center charges 900 € whereas for the combination of Sanger sequencing and SNP array, 1700 € is charged. Although WGS is not yet available as a standard diagnostic test, the charges for diagnostic WGS will certainly exceed the charges for WES (1800 €). Furthermore, each extra day of hospitalization at a neonatal intensive care unit that can be prevented by an earlier diagnosis can save up to thousands of euros.22
Clearly, there are some limitations to the present study. First of all, because of the low incidence of ACD/MPV, our approach was retrospective to infants already identified as having ACD/MPV through histopathologic analysis of lung tissue, rather than demonstrating prospectively that we provide a rapid diagnostic test. However, the results of this study can be the starting point for a prospective study that investigates the impact of the ACD/MPV panel on the patient’s quality of life, the diagnostic yield, and the cost-effectiveness. Another limitation would be that the current study focused solely on detection of FOXF1 variants whereas the phenotype of ACD/MPV overlaps with the phenotypes of other congenital lung disorders. Based on the successful results of the current study, we are expanding the panel by adding more genes and loci so that other congenital lung disorders can be diagnosed without the need for additional WGS. Furthermore, by using an updated version of the Ion Ampliseq Designer, the GC-rich regions that were uncovered in the current ACD/MPV panel can be included in the expanded panel.
In this study, DNA samples isolated from FFPE tissues worked not as efficient as DNA isolated from fresh tissue. It has been shown that DNA fragmentation and degradation are higher in FFPE tissues than fresh tissues and that they increase after longer storage.26,27 In this study, only three of the 18 FFPE lung samples were processed after 2009, including one of the samples in which a mutation was identified. Presumably, as shown in previous studies, the use of more recently fixed FFPE tissues will result in more efficient sequencing.13 Furthermore, other tissues like spleen or liver may provide better results than lung tissue.
To summarize, we developed a FOXF1-targeted NGS panel to detect mutations and deletions associated with ACD/MPV and showed that the panel works efficiently with DNA isolated from fresh tissues like blood. To our knowledge, this is the first NGS panel that targets both the FOXF1 gene and the enhancer region in the same run. Therefore, this test is able to detect CNVs in the noncoding enhancer region without the need for expensive and time-consuming whole-genome approaches. Although the current study is based on retrospective testing of ACD/MPV patients, the results suggest that the panel can be used for relatively noninvasive and quick screening for FOXF1 alterations in future ACD/MPV patients. Thereby, it has the potential to increase the diagnostic yield and reduce the use of futile and high-cost techniques like ECMO therapy. Moreover, once the correlation between FOXF1 alterations and ACD/MPV is well-defined, an invasive lung biopsy might no longer be needed to confirm ACD/MPV.
References
Slot, E. et al. Alveolar capillary dysplasia with misalignment of the pulmonary veins: clinical, histological, and genetic aspects. Pulm. Circ. 8, 2045894018795143 (2018).
Kool, H., Mous, D., Tibboel, D., de Klein, A. & Rottier, R. J. Pulmonary vascular development goes awry in congenital lung abnormalities. Birth Defects Res. C Embryo Today 102, 343–358 (2014).
Al-Hathlol, K. et al. Alveolar capillary dysplasia. Report of a case of prolonged life without extracorporeal membrane oxygenation (ECMO) and review of the literature. Early Hum. Dev. 57, 85–94 (2000).
Inwald, D., Brown, K., Gensini, F., Malone, M. & Goldman, A. Open lung biopsy in neonatal and paediatric patients referred for extracorporeal membrane oxygenation (ECMO). Thorax 59, 328–333 (2004).
Sen, P., Thakur, N., Stockton, D. W., Langston, C. & Bejjani, B. A. Expanding the phenotype of alveolar capillary dysplasia (ACD). J. Pediatr. 145, 646–651 (2004).
Stankiewicz, P. et al. Genomic and genic deletions of the FOX gene cluster on 16q24.1 and inactivating mutations of FOXF1 cause alveolar capillary dysplasia and other malformations. Am. J. Hum. Genet. 84, 780–791 (2009).
Dharmadhikari, A. V., Szafranski, P., Kalinichenko, V. V. & Stankiewicz, P. Genomic and epigenetic complexity of the FOXF1 locus in 16q24.1: implications for development and disease. Curr. Genomics 16, 107–116 (2015).
Seo, H., Kim, J., Park, G. H., Kim, Y. & Cho, S. W. Long-range enhancers modulate Foxf1 transcription in blood vessels of pulmonary vascular network. Histochem. Cell Biol. 146, 289–300 (2016).
Szafranski, P. et al. Pathogenetics of alveolar capillary dysplasia with misalignment of pulmonary veins. Hum. Genet. 135, 569–586 (2016).
Szafranski, P. et al. Narrowing the FOXF1 distant enhancer region on 16q24.1 critical for ACDMPV. Clin. Epigenet. 8, 112 (2016).
National Center for Biotechnology Information. USNLoM, Genetic Testing Registry. https://www.ncbi.nlm.nih.gov/gtr/conditions/C0031190/ (13 February 2020).
Genomes Project, C. et al. A global reference for human genetic variation. Nature 526, 68–74 (2015).
Smit, K. N. et al. Combined mutation and copy-number variation detection by targeted next-generation sequencing in uveal melanoma. Mod. Pathol. 31, 763–771 (2018).
Miller, S. A., Dykes, D. D. & Polesky, H. F. A simple salting out procedure for extracting DNA from human nucleated cells. Nucleic Acids Res. 6, 1215 (1988).
Thorvaldsdottir, H., Robinson, J. T. & Mesirov, J. P. Integrative Genomics Viewer (IGV): high-performance genomics data visualization and exploration. Brief. Bioinform. 14, 178–192 (2013).
Den Dunnen, J. T. HGVS recommendations for the description of sequence variants: 2016 update. Hum. Mutat. 37, 564–569 (2016).
Richards, S. et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet. Med. 17, 405–424 (2015).
Riggs, E. R. et al. Technical standards for the interpretation and reporting of constitutional copy-number variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics (ACMG) and the Clinical Genome Resource (ClinGen). Genet. Med. 22, 245–257 (2020).
Sen, P. et al. Novel FOXF1 mutations in sporadic and familial cases of alveolar capillary dysplasia with misaligned pulmonary veins imply a role for its DNA binding domain. Hum. Mutat. 34, 801–811 (2013).
Szafranski, P. et al. Small noncoding differentially methylated copy-number variants, including lncRNA genes, cause a lethal lung developmental disorder. Genome Res. 23, 23–33 (2013).
Szafranski, P. et al. Association of rare non-coding SNVs in the lung-specific FOXF1 enhancer with a mitigation of the lethal ACDMPV phenotype. Hum. Genet. 138, 1301–1311 (2019).
Swaggart, K. A. et al. Making a genetic diagnosis in a level IV neonatal intensive care unit population: who, when, how, and at what cost? J. Pediatr. 213, 211–217.e4 (2019).
Houmes, R. J. et al. Risk and relevance of open lung biopsy in pediatric ECMO patients: the Dutch experience. J. Pediatr. Surg. 52, 405–409 (2017).
Edwards, J. J. et al. Histopathologic and genetic features of alveolar capillary dysplasia with atypical late presentation and prolonged survival. J. Pediatr. 210, 214–219 e212 (2019).
Towe, C. T., et al. Infants with atypical presentations of alveolar capillary dysplasia with misalignment of the pulmonary veins who underwent bilateral lung transplantation. J. Pediatr. 194, 158–164.e1 (2018).
Watanabe, M. et al. Estimation of age-related DNA degradation from formalin-fixed and paraffin-embedded tissue according to the extraction methods. Exp. Ther. Med. 14, 2683–2688 (2017).
Wong, S. Q. et al. Sequence artefacts in a prospective series of formalin-fixed tumours tested for mutations in hotspot regions by massively parallel sequencing. BMC Med. Genomics 7, 23 (2014).
Acknowledgements
We thank the VU University Medical Center Amsterdam and the Charles University and General University Hospital Prague for their contribution to our sample collection. Further, we thank the Friends from Sophia Foundation for their support and, we thank the Royal Netherlands Academy of Arts and Sciences for the Ter Meulen Grant. We received financial support from The Friends from Sophia Foundation and The Royal Netherlands Academy of Arts and Sciences.
Author information
Authors and Affiliations
Contributions
A.d.K., R.J.R. and D.T. designed the study. A.v.H., M.P. and A.D. provided samples. Experiments were performed by E.S., R.v.M., F.M. and J.H.v.d.T. Data were analyzed and interpreted by E.S., R.v.M., J.H.v.d.T., A.d.K., H.J.D., and R.J.R. E.S. wrote the manuscript and A.v.H., A.d.K., R.J.R., H.J.D., and D.T. critically commented and edited the manuscript. All authors had final approval of the submitted and published versions.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Slot, E., von der Thüsen, J.H., van Heijst, A. et al. Fast detection of FOXF1 variants in patients with alveolar capillary dysplasia with misalignment of pulmonary veins using targeted sequencing. Pediatr Res 89, 518–525 (2021). https://doi.org/10.1038/s41390-020-0931-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-0931-5