Abstract
Study design
Psychometric study.
Objective
The aim of the study was to translate and culturally adapt the MSISQ-15 into Italian and to administer it to individuals with a spinal cord injury (SCI).
Setting
Rome’s Wheelchair Rugby Team and three spinal units in Italy.
Methods
Translation and validation of the MSISQ-15 were performed based on international guidelines. The questionnaire, which was in a paper and online format, was administered with the Short Form-12 Health Survey (SF-12) and the Spinal Cord Independence Measure Self-Report.
Results
Sixty-five participants were recruited. Internal consistency coefficient of MSISQ-15 scale, assessed by Cronbach’s alpha, was 0.75. Test–retest reliability interclass correlations was, for example, 0.86. The construct validity was calculated and showed statistically significant results in relation to the mental health status investigated with the SF-12.
Conclusions
The MSISQ-15 is a valid, reliable, and useful questionnaire for investigating how often the symptoms of an SCI interfere with a person’s satisfaction or sexual activity.
Similar content being viewed by others
Introduction
Depending on the extent of the damage, people with spinal cord injury (SCI) report perceiving different stimuli and sensations [1, 2]. In the past, the topic of sexuality was underexplored in the field of neurology because of the taboo surrounding it; however, it is now increasingly being studied in the literature [1, 3]. As evidenced by nurses in a study conducted in the Netherlands, sexuality is linked with discomfort characterized by shame, inadequate knowledge, and the thought that sexuality is not important after an SCI [4, 5]. Today, the sexual sphere is considered a priority after an SCI because when a disability or chronic illness overrides sexuality or sexual activity, the image of the individual changes. Patients must face this aspect of their lives in order to redefine their sexuality and themselves. After an SCI, men perceive themselves as less masculine and women feel less attractive and comfortable with themselves [3, 4]. These feelings may be heightened by modern culture, which espouses the myth of bodily perfection and traditional masculine norms [6]. Moreover, the SCI might have an impact on fertility in men and result in pregnancy-related problems in women [7]. Given these concerns, those interviewed in many studies about sexuality and disability state they want more education about sexual intimacy and having children after an SCI for themselves and their partners [3, 8]. By understanding the physiological changes that occur after this type of injury, care teams can work to redefine patients’ lives by improving their sexual quality of life [7]. To achieve this aim, it is fundamental to assess sexuality holistically, taking into account mental and social factors, rather than just the symptom [9]. Exploring literature, the Multiple Sclerosis Intimacy and Sexuality Questionnaire (MSISQ-15) is the most accurate and most commonly employed tool for the purpose of analyzing sexuality holistically and it has already been used in population with SCI with excellent results (Cronbach’s alpha >0.8 and intraclass correlation coefficient >0.8). The tool was developed in 2006 with 19 items [10] and reduced to 15 in 2013 in US [11], in 2014 was validated in Persian [12], in 2015 in Brazilian Portuguese [13], and in 2018 in Dutch in a population with SCI [14]. All versions showed positive results for reliability and validity. Moreover, the cross-cultural adaptation process is important when an instrument is used in a different language, setting and time to reduce the risk of introducing bias into a study. In studies where a phenomenon is measured indirectly with questionnaires, comparison of results between cultures and groups may be a challenge. In particular comparison will be difficult if the adaptation process has been flawed. It is therefore important that each item is adapted appropriately. Therefore, it is important to adapt it to and validate it in the Italian context so that it can be introduced into clinical practice, authors decided to validate the 15-item version for because it is shorter and because already used in a sample with SCI. The MSISQ-15 is divided into three domains: (1) primary sexual dysfunctions, which include the symptoms resulting from neurological alterations that directly affect sexual function (alteration of genital sensation, erectile dysfunction, orgasmic dysfunction, decrease in vaginal lubrication, and libido reduction); (2) secondary sexual dysfunctions, which include symptoms that derive from the pathology and indirectly affect sexual function (muscle constriction, spasticity, bladder and bowel dysfunction, and pain or discomfort in nongenital areas of the body); and (3) tertiary sexual dysfunctions include all the psychological, emotional, social, and cultural aspects of the pathology that have an impact on sexual function (feeling less virile/feminine or less attractive, concern about partner satisfaction, and general insecurity about their sexuality). The aforementioned domains are analyzed through 15 items to be answered by assigning a value from 1 (never) to 5 (always). The total score ranges from 15 to 75 points: the higher the score, the greater the impact the damaging event has on the person’s sexuality.
In short, the objective of this study is to translate, culturally adapt, and measure the psychometric properties of the MSISQ-15 within the Italian population by administering it to individuals with an SCI.
Methods
The present study was conducted by health professionals from Sapienza University of Rome and the Rehabilitation and Outcome Measures Assessment Association [14,15,16,17,18,19,20,21,22,23,24,25]. After receiving permission from the developers of the original MSISQ-15 (see Appendix 1), the instrument was translated from English into Italian using the Translation and Cultural Adaptation of Patient Reported Outcomes Measures–Principles of Good Practice guideline [26]. The reliability and construct validity of the culturally adapted scale were assessed following the “Consensus-Based Standards for the Selection of Health Status Measurement Instruments” COnsensus-based Standards for the selection of health Measurement INstruments (COSMIN) checklist [27].
Data collection
The sampling method consisted in recruiting all the eligible participants who met the inclusion criteria. The population was recruited from Rome’s Wheelchair Rugby Team and three spinal units in Italy. The study aims and procedures were explained to all the eligible individuals, and those interested in participating signed the informed consent before being included in the study. Based on the previous versions of the questionnaire, the inclusion criteria for our population were as follows: people with an SCI, who have been sexually active for at least 6 months, and who speak Italian fluently. The exclusion criteria included psychiatric or cognitive impairment evaluated by clinical screening. The questionnaire was administered twice, first with the Short Form-12 Health Survey (SF-12) and the Spinal Cord Independence Measure Self-Reported (SCIM SR), and the second administration occurred 3 days later.
Instruments
The MSISQ-15 is a self-report measure initially designed to assess satisfaction with and the influence of symptoms on sexual activity over a 6-month period for patients with multiple sclerosis [10]. Only later was it also considered useful for the evaluation of people with an SCI due to the similarity of the symptoms in the two different clinical conditions (Cronbach’s alpha >0.8 and intraclass correlation coefficient >0.8) [28].
The SF-12 is a self-administered questionnaire developed in the United States based on the original SF-36 [29]. The questionnaire examines a person’s physical and mental health through 12 items and showed to be valid in its Italian version [25].
The SCIM SR, derived directly from the SCIM III [26], is a self-administered scale questionnaire for people with an SCI, consisting of 19 items that investigate the basic activities of daily life: self-care (nutrition, hygiene and personal care, dressing), respiration management, sphincter control, and mobility (in bed and transfers). Depending on clinical relevance, the score for each item can vary from 0 to 100: the higher the score, the greater the person’s autonomy. SCIM SR showed to be valid in its Italian version [30].
Data analysis
Following COSMIN guidelines [27], in order to assess the psychometric properties of the Italian version of the MSISQ-15 [14], the internal consistency was evaluated through the Cronbach’s alpha coefficient, whose value, to be considered acceptable, must be >0.7. The stability was assessed by comparing the results from the first administration with the results from the second; the intraclass correlation coefficient was calculated and considered acceptable for values >0.7. Finally, Pearson’s correlation coefficient was calculated to detect the correlations among the MSISQ-15, SF-12, and SCIM SR and determine its construct validity. Evaluation of construct validity requires that the correlations of the measure be examined in regard to variables that are known to be related to the construct (purportedly measured by the instrument being evaluated or for which there are theoretical grounds for expecting it to be related) [31]. Therefore, the construct validity in this study was evaluated not only in association with the SCIM, to assess whether the scores of the two instruments increased linearly, but also with the SF-36. It was decided to evaluate the association between the scores obtained by the participants in assessing their sexual dysfunction through the MSISQ-15 and those obtained in assessing their physical and mental health through the SF-12. Both scales ask people to score themselves based on their symptoms and health and it exists theoretical grounds for expecting sexual dysfunction and quality of life to be related [5]. The Pearson correlation coefficient can be interpreted as follows: 0 indicates no linear relationship; +1/−1 indicates a perfect linear positive/negative relationship; values between 0 and 0.3 (0 and −0.3) indicate a weak linear positive (negative) relationship through a shaky linear rule; values ranging from 0.3 to 0.7 (−0.3 and −0.7) indicate a moderate positive (negative) linear relationship through a fuzzy-firm linear rule; and values between 0.7 and 1.0 (−0.7 and −1.0) indicate a strongly positive (negative) linear relationship through a firm linear rule. The significance level was set at a p value less than or equal to 0.05. All statistical analyses were performed using IBM-SPSS version 23.0.
Results
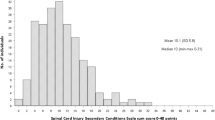
The linguistic and cultural adaptation of the MSISQ-15 is presented in Appendix 2. According to data from the Gruppo Italiano Studio Epidemiologico Mielolesioni study, the incidence of SCI is estimated to be 2500 cases per year with a prevalence of 60,000–70,000 cases for a population of 60 million in Italy [32]. Among the 103 recruited participants, 65 met the inclusion criteria and were included in the study, of these, the firsts 25 participated in the subsequent retest. Table 1 reports the participants’ demographic characteristics. The statistical analysis found the Cronbach’s alpha value for the total score to be >0.7 (see Table 2), demonstrating that the MSISQ-15 has excellent internal consistency and there is a strong interrelationship among the items. Moreover, Table 2 shows all the items are relevant from the analysis of Cronbach’s alpha if Item deleted. As revealed in Table 3, the value of the intraclass correlation coefficient between the test and retest was >0.7 for 8 of the 15 items; therefore, these items alone show the instrument has excellent stability for a delivery time of 3 days.
Construct validity was evaluated using Pearson’s correlation analysis to determine the associations among the MSISQ-15, SF-12, and SCIM SR. In Table 4, the minus sign indicates that the scales have an inversely proportional correlation: for the MSISQ-15 (whose score ranges from 15 to 75), a value near 0 shows that the person never has the symptoms investigated, while on the SCIM SR (score 0–100), a value close to 0 shows that the lesion is so significant as to cause complete dependence. Although this correlation exists, from a statistical point of view, it does not have any statistically valid meaning. The only statistically significant correlation is between the MSISQ-15 and mental health (whose evaluation is carried out with the SF-12).
Discussion
It is important for the development of clinical practice and research that practical and appropriate measures are universally accepted; this would allow comparisons and met analysis of high quality randomized controlled trials of people with this ever-increasing injury. The aim of the study was to validate the Italian version of the MSISQ-15. Therefore, after the translation and cultural adaptation of the questionnaire into Italian, the MSISQ-15 was administered to people with an SCI based on the inclusion criteria. From the statistical analysis, it appears that the MSISQ-15 scale has optimal internal consistency. Moreover, all the items are relevant since, if any items were eliminated, the value of alpha would decrease, accordingly diminishing the internal consistency. In terms of the Dutch version of the questionnaire, when we only consider its administration to people with an SCI, it shows good internal consistency only for the second and the third domains, not for the first. This is probably a result of the smaller Dutch sample (43 people). In the current study, the stability has a value of 0.91 for the total score of the scale, and therefore, it is statistically significant. However, in the analysis of each individual item, 8 items out of 15 took on a value of >0.7 (see Table 3). This result is probably a consequence of the discrete variability of the scores to be inserted (from 1 to 5); in fact, the average scores obtained for the test and retest present a minimum difference. Moreover, the results of this study are also affected by the small number of participants (n = 25) that took the retest. In the Dutch version of the questionnaire, a total of 102 people (with multiple sclerosis and SCI) completed the retest, leading to statistically significant results for all the items.
Concerning construct validity in this study, the statistical analysis showed that the MSISQ-15 has a statistically significant correlation with mental health (SF-12). This result shows that when the frequency of sexual disorder increases, the negative perception that people have of their mental health also increases. Therefore, in terms of the individual’s capacity to face the sexual act, the mental health component of self-esteem is an important factor.
Limitations
Finally, the study has some limitations. One of these concerns the small sample size: although it reached the minimum value to validate this instrument (>49 participants), the number of participants who took the retest (25 participants) should be improved in future studies in order to examine its stability. Another limitation is related to the inability to extract correlations among the participants’ characteristics because of small sample size. Particularly, it is expected that individuals with paraplegia and tetraplegia have different issues, particularly in terms of sexual activities. Further studies should analyze differences in respondent with tetraplegia and paraplegia.
In fact, as reported by developers a limitation of the MSISQ-15 is that the primary, secondary, and tertiary domains do not necessarily differentiate between specific and nonspecific sexual dysfunction. Thus, the scale is an overall measure of sexual dysfunction not specific for a SCI population. The tool itself have some limitation, item 7: “Feeling of being less virile or less feminine // Feeling less masculine or feminine” introduces a heterosexist bias. The understanding and interpretation of the answers to this item are possible only from a heterosexist and androcentric perspective, based on a binary and linear vision of sexuality. The item, in fact, presupposes that there is a direct and linear correspondence between the sex attributed to birth (binary), gender identity, and sexual orientation. That is, a cisgender vision of sexuality. This bias interfere with the interpretation of non-cisgender (transsexual) or homosexual or bisexual or intersexual people with SCI. Future studies should consider a revision of that item.
Conclusion
In conclusion, the Italian version of the MSISQ-15 has been proven to be a valid and reliable overall measure for investigating sexuality from both a physical and psychological point of view in people with an SCI. For the first time, it is possible to determine how often the symptoms of an SCI affect the sexual sphere, thus allowing for an improved understanding of the possible problems in all functional areas of a person’s life. The results will promote the improvement of the quality of rehabilitative interventions to contribute in increasing the quality of life in sexual area of an individual with an SCI. However, in order to address specific sexual dysfunction it is recommendable to match the results of MSQS-15 with other specific measures. For example, to assess the urogenital function the use of the MSISQ-15 could be combined with the Qualiveen [33].
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Di Benedetto P, Franceschini M, Lotta S. Riabilitazione dei traumi vertebro-midollari. Italy: Minerva Medica; 1994.
Federici S, Artegiani F, Pigliautile M, Antonelli P, Diotallevi D, Ritacco I, et al. Enhancing psychological sexual health of people with spinal cord injury and their partners in an Italian unipolar spinal unit: a pilot data study. Front Psychol. 2019;10:754.
Fritz HA, Dillaway H, Lysack CL. “Don’t Think Paralysis Takes Away Your Womanhood”: sexual intimacy after spinal cord injury. Am J Occup Ther. 2015;69:6902260030p1-10.
Sakellariou D, Sawada Y. Sexuality after spinal cord injury: the Greek male’s perspective. Am J Occup Ther. 2006;60:311–9.
Pascual A, Wighman A, Littooij EC, Janssen TWJ. Sexuality as part of rehabilitation? A qualitative study on the perceptions of rehabilitation nurses on discussing patient sexuality during clinical rehabilitation. Disabil Rehabil. 2019:1–8. https://doi.org/10.1080/09638288.2019.1670271. [Epub ahead of print].
Aikman K, Oliffe JL, Kelly MT, McCuaig F. Sexual health in men with traumatic spinal cord injuries: a review and recommendations for primary health-care providers. Am J Mens Health. 2018;12:2044–54.
Stoffel JT, Van der Aa F, Wittmann D, Yande S, Elliott S. Fertility and sexuality in the spinal cord injury patient. World J Urol. 2018;36:1577–85.
Thrussell H, Coggrave M, Graham A, Gall A, Donald M, Kulshrestha R, et al. Women’s experiences of sexuality after spinal cord injury: a UK perspective. Spinal Cord. 2018;56:1084–94.
Ricciardi R, Szabo CM, Poullos AY. Sexuality and spinal cord injury. Nurs Clin North Am. 2007;42:675-84; viii-ix.
Christopherson JM, Moore K, Foley FW, Warren KG. A comparison of written materials vs. materials and counselling for women with sexual dysfunction and multiple sclerosis. J Clin Nurs. 2006;15:742–50.
Foley FW, Zemon V, Campagnolo D, Marrie RA, Cutter G, Tyry T, et al. The Multiple Sclerosis Intimacy and Sexuality Questionnaire— re-validation and development of a 15-item version with a large US sample. Mult Scler. 2013;19:1197–203.
Mohammadi K, Rahnama P, Montazeri A, Foley FW. The multiple sclerosis intimacy and sexuality questionnaire-19: reliability, validity, and factor structure of the Persian version. J Sex Med. 2014;11:2225–31.
Silva RA, Olival GS, Stievano LP, Toller VB, Jordy SS, Eloi M, et al. Validation and cross-cultural adaptation of sexual dysfunction modified scale in multiple sclerosis for Brazilian population. Arq Neuropsiquiatr. 2015;73:681–7.
Noordhoff TC, Scheepe JR, ‘t Hoen LA, Sluis TAR, Blok BFM. The Multiple Sclerosis Intimacy and Sexuality Questionnaire (MSISQ-15): validation of the Dutch version in patients with multiple sclerosis and spinal cord injury. Neurourol Urodyn. 2018;37:2867–74.
Galeoto G, Scialpi A, Grassi ML, Berardi A, Valente D, Tofani M, et al. General sleep disturbance scale: translation, cultural adaptation, and psychometric properties of the Italian version. Cranio—J Craniomandib Pr. 2019;11:1–9.
Nobilia M, Culicchia G, Tofani M, De Santis R, Savona A, Guarino D, et al. Italian version of the jebsen-taylor hand function test for the assessment of hand disorders: a cross-sectional study. Am J Occup Ther. 2019;73:7303205080p1–p6.
Berardi A, Dhrami L, Tofani M, Valente D, Sansoni J, Galeoto G. Cross-cultural adaptation and validation in the Italian population of the wolf motor function test in patients with stroke. Funct Neurol. 2018;33:229–53.
Galeoto G, Sansoni J, Valenti D, Mollica R, Valente D, Parente M, et al. The effect of physiotherapy on fatigue and physical functioning in chronic fatigue syndrome patients: a systematic review. Clin Ter. 2018;169:e184–8.
Dattoli S, Colucci M, Soave MG, De Santis R, Segaletti L, Corsi C, et al. Evaluation of pelvis postural systems in spinal cord injury patients: outcome research. J Spinal Cord Med. 2018;43:185–92.
Galeoto G, Iori F, De Santis R, Santilli V, Mollica R, Marquez MA, et al. The outcome measures for loss of functionality in the activities of daily living of adults after stroke: a systematic review. Top Stroke Rehabil. 2019;26:236–45.
Ruggieri M, Palmisano B, Fratocchi G, Santilli V, Mollica R, Berardi A, et al. Validated fall risk assessment tools for use with older adults: a systematic review. Phys Occup Ther Geriatr. 2018;36:331–53.
Puledda F, Viganò A, Celletti C, Petolicchio B, Toscano M, Vicenzini E, et al. A study of migraine characteristics in joint hypermobility syndrome a.k.a. Ehlers–Danlos syndrome, hypermobility type. Neurol Sci. 2015;36:1417–24.
Tofani M, Galeoto G, Cazzetta D, Berardi A, Sansoni J, Valente D. Validation of the pediatric evaluation of disability inventory in an Italian population with autism spectrum disorder: a cross-sectional study. Clin Ter. 2019;170:e460–4.
Berardi A, Galeoto G, Guarino D, Marquez MA, De Santis R, Valente D, et al. Construct validity, test-retest reliability, and the ability to detect change of the Canadian occupational performance measure in a spinal cord injury population. Spinal cord Ser cases. 2019;5:52.
Berardi A, Biondillo A, Màrquez MA, De Santis R, Fabbrini G, Tofani M, et al. Validation of the short version of the Van Lieshout test in an Italian population with cervical spinal cord injuries: a cross-sectional study. Spinal Cord. 2018;29:52.
Wild D, Grove A, Martin M, Eremenco S, McElroy S, Verjee-Lorenz A, et al. Principles of good practice for the translation and cultural adaptation process for patient-reported outcomes (PRO) measures: report of the ISPOR task force for translation and cultural adaptation. Value Health. 2005;8:94–104.
Mokkink LB, de Vet HCW, Prinsen CAC, Patrick DL, Alonso J, Bouter LM, et al. COSMIN risk of bias checklist for systematic reviews of patient-reported outcome measures. Qual Life Res. 2018;27:1171–9.
Noordhoff TC, Scheepe JR, ‘t Hoen LA, Sluis TAR, Blok BFM. The Multiple Sclerosis Intimacy and Sexuality Questionnaire (MSISQ-15): validation of the Dutch version in patients with multiple sclerosis and spinal cord injury. Neurourol Urodyn. 2018;37:2867–74.
Kodraliu G, Mosconi P, Groth N, Carmosino G, Perilli A, Gianicolo EA, et al. Subjective health status assessment: evaluation of the Italian version of the SF-12 Health Survey. Results from the MiOS Project. J Epidemiol Biostat. 2001;6:305–16.
Bonavita J, Torre M, China S, Bressi F, Bonatti E, Capirossi R, et al. Validation of the Italian version of the spinal cord independence measure (SCIM III) self-report. Spinal Cord. 2016;54:553–60.
Strauss ME, Smith GT. Construct validity: advances in theory and methodology. Annu Rev Clin Psychol. 2009;5:1–25.
Baricich A, Amico AP, Zampolini M, Gimigliano F, Cisari C, Fiore P. People with spinal cord injury in Italy. Am J Phys Med Rehabil. 2017;96(2 Suppl 1):S80–2. https://doi.org/10.1097/PHM.0000000000000573.
Bonniaud V, Bryant D, Pilati C, Menarini M, Lamartina M, Guyatt G, et al. Italian version of Qualiveen-30: cultural adaptation of a neurogenic urinary disorder-specific instrument. Neurourol Urodyn. 2011;30:354–9.
Acknowledgements
We acknowledge those who participated in the surveys; their collective expertise greatly informed the development of the Italian version of the MSISQ-15.
Author information
Authors and Affiliations
Contributions
AB, GG, MAM: conceived and/or designed the work that led to the submission, acquired data, and/or played an important role in interpreting the results. MM, MT: drafted or revised the manuscript. DV: approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The authors certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. Informed consent was obtained from all participants for being included in the study. Institutional Review Board approval was not required because the administration of these tool was part of the usual process of assessment of these individuals in clinical practice, the research involved the analysis of data collected such that individual subjects cannot be identified in any way.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Monti, M., Marquez, M.A., Berardi, A. et al. The Multiple Sclerosis Intimacy and Sexuality Questionnaire (MSISQ-15): validation of the Italian version for individuals with spinal cord injury. Spinal Cord 58, 1128–1133 (2020). https://doi.org/10.1038/s41393-020-0469-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-020-0469-8