Abstract
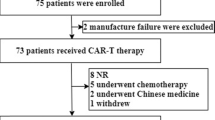
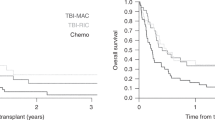
Relapsed/refractory Philadelphia chromosome-positive acute lymphoblastic leukemia (r/r Ph+ ALL) has an extremely poor prognosis. Chimeric antigen receptor T-cell (CART) therapy has acquired unprecedented efficacy in B-cell malignancies, but its role in the long-term survival of r/r Ph+ ALL patients is unclear. We analyzed the effect of CART on 56 adults with r/r Ph+ ALL who accepted split doses of humanized CD19-targeted CART after lymphodepleting chemotherapy. 51/56 (91.1%) achieved complete remission (CR) or CR with inadequate count recovery (CRi), including 38 patients with negative minimal residual disease (MRD) tested by bone marrow BCR-ABL1 copies. Subsequently, 30/51 CR/CRi patients accepted consolidative allogeneic haematopoietic stem cell transplantation (alloHSCT). Their outcomes were compared with those of 21/51 contemporaneous patients without alloHSCT. The 2-year overall survival (OS) and leukemia-free survival (LFS) of CR/CRi patients with alloHSCT were significantly superior to those without alloHSCT (58.9%, CI 49.8–68.0% vs. 22.7%, CI 12.7–32.7%, p = 0.005; 53.2%, CI 43.6–62.8% vs. 18.8%, CI 9.2–28.4%, p = 0.000, respectively). Multivariate analysis revealed that alloHSCT and MRD-negative post-CART were the independent prognostic factors for OS and LFS. CART therapy is highly effective for r/r Ph+ ALL patients, and consolidative alloHSCT could prolong their OS and LFS.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Moorman AV, Harrison CJ, Buck GAN, Richards SM, Secker-Walker LM, Martineau M, et al. Karyotype is an independent prognostic factor in adult acute lymphoblastic leukemia (ALL): analysis of cytogenetic data from patients treated on the Medical Research Council (MRC) UKALLXII/Eastern Cooperative Oncology Group (ECOG) 2993 trial. Blood. 2007;109:3189–97.
Fielding AK, Rowe JM, Buck G, Foroni L, Gerrard G, Litzow MR, et al. UKALLXII/ECOG2993: addition of imatinib to a standard treatment regimen enhances long-term outcomes in Philadelphia positive acute lymphoblastic leukemia. Blood. 2014;123:843–50.
Thomas DA, Faderl S, Cortes J, O’Brien S, Giles FJ, Kornblau SM, et al. Treatment of Philadelphia chromosome-positive acute lymphocytic leukemia with hyper-CVAD and imatinib mesylate. Blood. 2004;103:4396–407.
Bassan R, Rossi G, Pogliani EM, Bona ED, Angelucci E, Cavattoni I, et al. Chemotherapy-phased imatinib pulses improve long-term outcome of adult patients with Philadelphia chromosome-positive acute lymphoblastic leukemia: Northern Italy Leukemia Group protocol 09/00. J Clin Oncol. 2010;28:3644–52.
Tanguy-Schmidt A, Rousselot P, Chalandon Y, Cayuela JM, Hayette S, Vekemans MC, et al. Long-term follow up of the imatinib GRAAPH-2003 study in newly diagnosed patients with de novo Philadelphia chromosome-positive acute lymphoblastic leukemia: a GRAALL study. Biol Blood Marrow Transplant. 2013;19:150–5.
Chalandon Y, Thomas X, Hayette S, Cayuela J-M, Abbal C, Huguet F, et al. Randomized study of reduced-intensity chemotherapy combined with imatinib in adults with Ph-positive acute lymphoblastic leukemia. Blood. 2015;125:3711–9.
Saußele S, Richter J, Hochhaus A, Mahon FX. The concept of treatment-free remission in chronic myeloid leukemia. Leukemia. 2016;30:1638–47.
Kim DY, Joo YD, Lim SN, Kim SD, Lee JH, Lee JH, et al. Nilotinib combined with multiagent chemotherapy for newly diagnosed Philadelphia-positive acute lymphoblastic leukemia. Blood. 2015;126:746–56.
Jabbour E, Kantarjian H, Ravandi F, Thomas D, Huang XL, Faderl S. et al. Combination of hyper-CVAD with ponatinib as first-line therapy for patients with Philadelphia chromosome-positive acute lymphoblastic leukaemia: a single-centre, phase 2 study. Lancet Oncol. 2015;16:1547–55.
Soverini S, De Benedittis C, Papayannidis C, Paolini S, Venturi C, Iacobucci I, et al. Drug resistance and BCR-ABL kinase domain mutations in Philadelphia chromosome-positive acute lymphoblastic leukemia from the imatinib to the second-generation tyrosine kinase inhibitor era: the main changes are in the type of mutations, but not in the frequency of mutation involvement. Cancer. 2014;120:1002–9.
Rambaldi A, Ribera JM, Kantarjian HM, Dombret H, Ottmann OG, Stein AS, et al. Blinatumomab compared with standard of care for the treatment of adult patients with relapsed/refractory Philadelphia chromosome–positive B-precursor acute lymphoblastic leukemia. Cancer. 2020;126:304–10.
Brentjens RJ, Davila ML, Riviere I, Park J, Wang X, Cowell LG, et al. CD19-targeted T cells rapidly induce molecular remissions in adults with chemotherapy-refractory acute lymphoblastic Leukemia. Sci Transl Med. 2013;5:177ra38.
Davila ML, Riviere L, Wang X, Bartido S, Park J, Curran K, et al. Efficacy and toxicity management of 19-28z CAR T cell therapy in B cell acute lymphoblastic leukemia. Sci Transl Med. 2014;6:224ra25.
Kansagra AJ, Frey NV, Bar M, Laetsch TW, Carpenter PA, Savani BN, et al. Clinical utilization of chimeric antigen receptor T cells in B cell acute lymphoblastic leukemia: an expert opinion from the European Society for Blood and Marrow Transplantation and the American Society for Blood and Marrow Transplantation. Biol Blood Marrow Transplant. 2019;25:e76–85.
Mohty M, Gautier J, Malard F, Aljurf M, Bazarbachi A, Chabannon C. et al. CD19 chimeric antigen receptor-T cells in B-cell leukemia and lymphoma: current status and perspectives. Leukemia. 2019;33:2767–78.
Gardner R, Wu D, Cherian S, Fang M, Hanafi LA, Finney O, et al. Acquisition of a CD19-negative myeloid phenotype allows immune escape of MLL-rearranged B-ALL from CD19 CAR-T-cell therapy. Blood. 2016;127:2406–10.
Zhu YM, Wu Z, Tan YP, Du YY, Liu Z, Ou RM, et al. Anti-CD19 chimeric antigen receptor T-cell therapy for adult Philadelphia chromosome-positive acute lymphoblastic leukemia: two case reports. Medicine. 2016;95:e5676.
Park JH, Riviere I, Gonen M, Wang X, Senechal B, Curran KJ. et al. Long-term follow-up of CD19 CAR therapy in acute lymphoblastic leukemia. N Engl J Med. 2018;378:449–59.
Jiang H, Li C, Yin P, Guo T, Liu L, Xia L, et al. Anti-CD19 CAR-T therapy bridging to allo-HSCT for relapsed/refractory B-cell acute lymphoblastic leukemia: an open-label pragmatic clinical trial. Am J Hematol. 2019;94:1113–22.
Pan J, Yang JF, Deng BP, Zhao XJ, Zhang X, Lin YH. et al. High efficacy and safety of low-dose CD19-directed CAR-T cell therapy in 51 refractory or relapsed B acute lymphoblastic leukemia patients. Leukemia.2017;31:2587–93.
Zhang C, Kong PY, Li S, Chen T, Ni X, Li Y. et al. Donor-derived CAR-T Cells serve as a reduced-intensity conditioning regimen for haploidentical stem cell transplantation in treatment of relapsed/refractory acute lymphoblastic leukemia: case report and review of the literature. J Immunother.2018;41:306–11.
Litzow MR, Fielding AK, Luger SM, Paietta E, Ofran Y, Rowe JM, et al. The evolving role of chemotherapy and hematopoietic cell transplants in Ph-positive acute lymphoblastic leukemia in adults. Bone Marrow Transplant. 2017;52:1592–8.
Yang F, Zhang J, Zhang XY, Tian ML, Wang JJ, Kang LQ. et al. Delayed remission following sequential infusion of humanized CD19- and CD22-modified CAR-T cells in a patient with relapsed/refractory acute lymphoblastic leukemia and prior exposure to murine-derived CD19-directed CAR-T cells. OncoTargets Ther. 2019;12:2187–91.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J, et al. 1994 Consensus conference on acute GVHD grading. Bone Marrow Transplant. 1995;15:825–8.
Sullivan KM, Shulman HM, Storb R, Weiden PL, Witherspoon RP, McDonald GB, et al. Chronic graft-versus-host disease in 52 patients: adverse natural course and successful treatment with combination immunosuppression. Blood. 1981;57:267–76.
McDonald GB. How I treat acute graft-versus-host disease of the gastrointestinal tract and the liver. Blood. 2016;127:1544–50.
Flowers MED, Martin PJ. How we treat chronic graft-versus-host disease. Blood. 2015;125:606–15.
Neelapu SS, Tummala S, Kebriaei P, Wierda W, Gutierrez C, Locke FL, et al. Chimeric antigen receptor T-cell therapy assessment and management of toxicities. Nat Rev Clin Oncol. 2018;15:47–62.
Eide CA, Zabriskie MS, Stevens SLS, Antelope O, Vellore NA, Than H, et al. Combining the allosteric inhibitor asciminib with ponatinib suppresses emergence of and restores efficacy against highly resistant BCR-ABL1 mutants. Cancer Cell. 2019;36:431–43.e5.
Pemovska T, Johnson E, Kontro M, Repasky GA, Chen J, Wells P, et al. Axitinib effectively inhibits BCR-ABL1(T315I) with a distinct binding conformation. Nature. 2015;519:102–5.
Fei F, Lim M, Schmidhuber S, Moll J, Groffen J, Heisterkamp N. Treatment of human pre-B acute lymphoblastic leukemia with the Aurora kinase inhibitor PHA-739358 (Danusertib). Mol Cancer. 2012;11:42.
Martinelli G, Boissel N, Chevallier P, Ottmann O, Gökbuget N, Topp MS. et al. Complete hematologic and molecular response in adult patients with relapsed/refractory Philadelphia chromosome-positive B-precursor acute lymphoblastic leukemia following treatment with blinatumomab: results from a phase II, single-arm, multicenter study. J Clin Oncol. 2017;35:1795–802.
Ravandi F, Jorgensen JL, Thomas DA, O’Brien S, Garris R, Faderl S, et al. Detection of MRD may predict the outcome of patients with Philadelphia chromosome–positive ALL treated with tyrosine kinase inhibitors plus chemotherapy. Blood. 2013;122:1214–21.
Short NJ, Jabbour E, Sasaki K, Patel K, O’Brien SM, Cortes JE, et al. Impact of complete molecular response on survival in patients with Philadelphia chromosome–positive acute lymphoblastic leukemia. Blood. 2016;128:504–7.
Jabbour E, Short NJ, Jorgensen JL, Yilmaz M, Ravandi F, Wang SA, et al. Differential impact of minimal residual disease negativity according to the salvage status in patients with relapsed/refractory B-cell acute lymphoblastic leukemia. Cancer. 2017;123:294–302.
Gaipa G, Cazzaniga G, Valsecchi MG, Panzer-Grumayer R, Buldini B, Silvestri D, et al. Time point-dependent concordance of flow cytometry and realtime quantitative polymerase chain reaction for minimal residual disease detection in childhood acute lymphoblastic leukemia. Haematologica. 2012;97:1582–93.
Stow P, Key L, Chen X, Pan Q, Neale GA, Coustan-Smith E, et al. Clinical significance of low levels of minimal residual disease at the end of remission induction therapy in childhood acute lymphoblastic leukemia. Blood. 2010;115:4657–63.
Hovorkova L, Zaliova M, Venn NC, Bleckmann K, Trkova M, Potuckova E. et al. Monitoring of childhood ALL using BCR-ABL1 genomic breakpoints identifies a subgroup with CML-like biology. Blood.2017;129:2771–81.
Hunger SP. CML in blast crisis: more common than we think? Blood. 2017;129:2713–4.
McClellan JS, Dove C, Gentles AJ, Ryan CE, Majeti R. Reprogramming of primary human Philadelphia chromosome-positive B cell acute lymphoblastic leukemia cells into nonleukemic macrophages. Proc Natl Acad Sci USA. 2015;112:4074–9.
Gu B, Wu X, Chen G, Ma X, Jin Z, Tang X, et al. Haploidentical allogeneic hematopoietic stem cell transplantation compared to matched unrelated transplantation for Philadelphia chromosome-positive acute lymphoblastic leukemia. Leuk Res. 2017;59:41–6.
Wang Y, Liu QF, Xu LP, Liu KY, Zhang XH, Ma X, et al. Haploidentical versus matched-sibling transplant in adults with Philadelphia-negative high-risk acute lymphoblastic leukemia: a biologically phase III randomized study. Clin Cancer Res. 2016;22:3467–76.
Turtle CJ, Hanafi L-A, Berger C, Gooley TA, Cherian S, Hudecek M, et al. CD19 CAR-T cells of defined CD4: CD8 composition in adult B cell ALL patients. J Clin Investig. 2016;126:2123–38.
Maude SL, Laetsch TW, Buechner J, Rives S, Boyer M, Bittencourt H, et al. Tisagenlecleucel in children and young adults with B-cell lymphoblastic leukemia. N Engl J Med. 2018;378:439–48.
Acknowledgements
This work was supported by National Natural Science Foundation of China (81730003 and 81700204), Priority Academic Program Development of Jiangsu Higher Education Institutions (PAPD), Jiangsu Medical Outstanding Talents Project (JCRCA2016002), Jiangsu Provincial Key Medical Center (YXZXA2016002), Innovation Capability Development Project of Jiangsu Province (BM2015004), and National Key R&D Program of China (2017YFA0104502, 2017ZX09304021).
Author information
Authors and Affiliations
Contributions
Conception and design: BG, XM, DPW. Collection and assembly of data: BYS, XZ. Patient care: all coauthors. Data analysis and interpretation: BG, BYS, XZ, XM, DPW. Paper writing: BG, DPW. Final approval of paper: all coauthors.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Gu, B., Shi, BY., Zhang, X. et al. Allogeneic haematopoietic stem cell transplantation improves outcome of adults with relapsed/refractory Philadelphia chromosome-positive acute lymphoblastic leukemia entering remission following CD19 chimeric antigen receptor T cells. Bone Marrow Transplant 56, 91–100 (2021). https://doi.org/10.1038/s41409-020-0982-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-020-0982-6
This article is cited by
-
Safety and efficacy of CD22 and CD19 CAR-T bridging auto-HSCT as consolidation therapy for AYA and adult B-ALL
Blood Cancer Journal (2023)
-
Feasibility of in vivo CAR T cells tracking using streptavidin–biotin-paired positron emission tomography
European Journal of Nuclear Medicine and Molecular Imaging (2022)
-
Efficacy and safety of CD19 CAR-T cell therapy for acute lymphoblastic leukemia patients relapsed after allogeneic hematopoietic stem cell transplantation
International Journal of Hematology (2022)