Abstract
Intracytoplasmic sperm injection (ICSI) has become the most commonly used method of fertilization in assisted reproductive technology. The primary reasons for its popularity stem from its effectiveness, the standardization of the procedure, which means that it can easily be incorporated into the routine practice of fertility centres worldwide, and the fact that it can be used to treat virtually all forms of infertility. ICSI is the clear method of choice for overcoming untreatable severe male factor infertility, but its (over)use in other male and non-male factor infertility scenarios is not evidence-based. Despite all efforts to increase ICSI efficacy and safety through the application of advanced sperm retrieval and cryopreservation techniques, as well as methods for selecting sperm with better chromatin integrity, the overall pregnancy rates from infertile men remain suboptimal. Treating the underlying male infertility factor before ICSI seems to be a promising way to improve ICSI outcomes, but data remain limited. Information regarding the health of ICSI offspring has accumulated over the past 25 years, and there are reasons for concern as risks of congenital malformations, epigenetic disorders, chromosomal abnormalities, subfertility, cancer, delayed psychological and neurological development, and impaired cardiometabolic profile have been observed to be greater in infants born as a result of ICSI than in naturally conceived children. However, as subfertility probably influences the risk estimates, it remains to be determined to what extent the observed adverse outcomes are related to parental factors or associated with ICSI.
Key points
-
Intracytoplasmic sperm injection (ICSI) was introduced to overcome the most severe forms of male factor infertility and has become the most frequently used method of fertilization in assisted reproductive technology (ART).
-
Existing evidence does not support ICSI in preference over in vitro fertilization (IVF) in the general non-male factor ART population; however, in couples with unexplained infertility, ICSI is associated with lower fertilization failure rates than IVF.
-
Percutaneous and open sperm retrieval methods are highly effective for harvesting sperm from men with obstructive azoospermia; open microsurgical testicular sperm retrieval has been associated with improved sperm retrieval in men with nonobstructive azoospermia.
-
Existing evidence indicates that children conceived through ICSI have an increased risk of chromosomal abnormalities, particularly those affecting sex chromosomes, compared with naturally conceived children.
-
Whether the risk of cancer is increased among children conceived using ICSI is unclear, but some evidence indicates that certain cancer types are more common in children conceived using ICSI than in naturally conceived children.
-
All efforts should be made to evaluate and treat subfertile men, both to improve the safety and efficiency of ICSI and to allow natural conception or the use of less-invasive assisted conception methods when appropriate.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Part a adapted from ref.273, Macmillan Publishers Limited, CC BY 4.0. Part d adapted from ref.274 with permission from Ass. Prof. Igor Crha, CS., Faculty of Medicine, Masaryk University, created in collaboration with Service Center for E-Learning, Faculty of Informatics, Masaryk University, Czech Republic.

Figure reproduced with permission from ref.275, Ann Van Soom.
Similar content being viewed by others
References
Palermo, G., Joris, H., Devroey, P. & Van Steirteghem, A. C. Pregnancies after intracytoplasmic injection of single spermatozoon into an oocyte. Lancet 340, 17–18 (1992).
Palermo, G. D., Neri, Q. V. & Rosenwaks, Z. To ICSI or not to ICSI. Semin. Reprod. Med. 33, 92–102 (2015).
Jain, T. & Gupta, R. Trends in the use of intracytoplasmic sperm injection in the United States. N. Engl. J. Med. 357, 251–257 (2007).
van Rumste, M. M., Evers, J. L. & Farquhar, C. M. ICSI versus conventional techniques for oocyte insemination during IVF in patients with non-male factor subfertility: a Cochrane review. Hum. Reprod. 19, 223–227 (2004).
Dyer, S. et al. International Committee for Monitoring Assisted Reproductive Technologies world report: assisted reproductive technology 2008, 2009 and 2010. Hum. Reprod. 31, 1588–1609 (2016).
Boulet, S. L. et al. Trends in use of and reproductive outcomes associated with intracytoplasmic sperm injection. JAMA 313, 255–263 (2015).
Pereira, N. Lessons learned in andrology: from intracytoplasmic sperm injection and beyond. Andrology 4, 757–760 (2016).
Tournaye, H. et al. Microsurgical epididymal sperm aspiration and intracytoplasmic sperm injection: a new effective approach to infertility as a result of congenital bilateral absence of the vas deferens. Fertil. Steril. 61, 1045–1051 (1994).
Devroey, P. et al. Normal fertilization of human oocytes after testicular sperm extraction and intracytoplasmic sperm injection. Fertil. Steril. 62, 639–641 (1994).
Silber, S. J. et al. High fertilization and pregnancy rate after intracytoplasmic sperm injection with spermatozoa obtained from testicle biopsy. Hum. Reprod. 10, 148–152 (1995).
Devroey, P. et al. Pregnancies after testicular sperm extraction and intracytoplasmic sperm injection in non-obstructive azoospermia. Hum. Reprod. 10, 1457–1460 (1995).
Chambers, G. M. et al. Population trends and live birth rates associated with common ART treatment strategies. Hum. Reprod. 31, 2632–2641 (2016).
Practice Committees of American Society for Reproductive Medicine and Society for Assisted Reproduction Technology. Intracytoplasmic sperm injection (ICSI) for non-male factor infertility: a committee opinion. Fertil. Steril. 98, 1395–1399 (2012).
Devroey, P. & Van Steirteghem, A. A review of ten years experience of ICSI. Hum. Reprod. Update 10, 19–28 (2004).
Esteves, S. C., Miyaoka, R. & Agarwal, A. An update on the clinical assessment of the infertile male. [corrected]. Clinics 66, 691–700 (2011) erratum 67, 203 (2012).
Miyaoka, R. & Esteves, S. C. Predictive factors for sperm retrieval and sperm injection outcomes in obstructive azoospermia: do etiology, retrieval techniques and gamete source play a role? Clinics 68, 111–119 (2013).
Esteves, S. C. Clinical management of infertile men with nonobstructive azoospermia. Asian J. Androl. 17, 459–470 (2015).
Esteves, S. C., Miyaoka, R., Orosz, J. E. & Agarwal, A. An update on sperm retrieval techniques for azoospermic males. Clinics 68, (Suppl.1) 99–110 (2013).
Tournaye, H. Male factor infertility and ART. Asian J. Androl 14, 103–108 (2012).
Esteves, S. C. Novel concepts in male factor infertility: clinical and laboratory perspectives. J. Assist. Reprod. Genet. 33, 1319–1335 (2016).
Esteves, S. C. et al. Critical appraisal of World Health Organization’s new reference values for human semen characteristics and effect on diagnosis and treatment of subfertile men. Urology 79, 16–22 (2012).
Babayev, S. N., Park, C. W. & Bukulmez, O. Intracytoplasmic sperm injection indications: how rigorous? Semin. Reprod. Med. 32, 283–290 (2014).
World Health Organization. WHO laboratory manual for the examination and processing of human semen. 5th edn 226 (World Health Organization, 2010).
Cissen, M. et al. Assisted reproductive technologies for male subfertility. Cochrane Database Syst. Rev. 2, CD000360 (2016).
Tournaye, H. et al. Intracytoplasmic sperm injection versus in vitro fertilization: a randomized controlled trial and a meta-analysis of the literature. Fertil. Steril 78, 1030–1037 (2002).
Shuai, H. L., Ye, Q., Huang, Y. H. & Xie, B. G. Comparison of conventional in vitro fertilisation and intracytoplasmic sperm injection outcomes in patients with moderate oligoasthenozoospermia. Andrologia 47, 499–504 (2015).
Kruger, T. F. et al. Sperm morphologic features as a prognostic factor in in vitro fertilization. Fertil. Steril 46, 1118–1123 (1986).
Kruger, T. F. et al. Predictive value of abnormal sperm morphology in in vitro fertilization. Fertil. Steril 49, 112–117 (1998).
Gunalp, S., Onculoglu, C., Gurgan, T., Kruger, T. F. & Lombard, C. J. A study of semen parameters with emphasis on sperm morphology in a fertile population: an attempt to develop clinical thresholds. Hum. Reprod. 16, 110–114 (2001).
Menkveld, R. et al. Semen parameters, including WHO and strict criteria morphology, in a fertile and subfertile population: an attempt to develop clinical thresholds. Hum. Reprod. 16, 1165–1171 (2001).
Plachot, M. et al. Outcome of conventional IVF and ICSI on sibling oocytes in mild male fator infertility. Hum. Reprod. 17, 362–369 (2002).
Hotaling, J. M., Smith, J. F., Rosen, M., Muller, C. H. & Walsh, T. J. The relationship between isolated teratozoospermia and clinical pregnancy after in vitro fertilization with or without intracytoplasmic sperm injection: a systematic review and meta-analysis. Fertil. Steril. 95, 1141–1145 (2011).
Lundin, K., Soderlund, B. & Hamberger, L. The elationship between sperm morphology and rates of fertilization, pregnancy and spontaneous abortion in an in-vitro fertilization/intracytoplasmic sperm injection programme. Hum. Reprod. 12, 2676–2681 (1997).
Osawa, Y. et al. Assessment of the dominant abnormal form is useful for predicting the outcome of intracytoplasmic sperm injection in the case of severe teratozoospermia. J. Assist. Reprod. Genet. 16, 436–442 (1999).
Dubey, A. et al. The influence of sperm morphology on preimplantation genetic diagnosis cycles outcome. Fertil. Steril. 89, 1665–1669 (2008).
Keegan, B. R. et al. Isolated teratozoospermia does not affect in vitro fertilization outcome and is not an indication for intracytoplasmic sperm injection. Fertil. Steril. 88, 1583–1588 (2007).
Esteves, S. C. & Varghese, A. C. Laboratory handling of epididymal and testicular spermatozoa: what can be done to improve sperm injection outcome. J. Hum. Reprod. Sci. 5, 233–243 (2012).
Povlsen, B. B., Aw, L. D., Laursen, R. J., Esteves, S. C. & Humaidan, P. Pregnancy and birth after intracytoplasmic sperm injection with normal testicular spermatozoa in a patient with azoospermia and tail stump epididymal sperm. Int. Braz. J. Urol. 41, 1220–12255 (2015).
Dam, A. H. et al. Globozoospermia revisited. Hum. Reprod. Update. 13, 63–75 (2007).
Rubino, P., Viganò, P., Luddi, A. & Piomboni, P. The ICSI procedure from past to future: a systematic review of the more controversial aspects. Hum. Reprod. Update 22, 194–227 (2016).
Esteves, S. C., Schneider, D. T. & Verza, S. Jr. Influence of antisperm antibodies in the semen on intracytoplasmic sperm injection outcome. Int. Braz. J. Urol. 33, 795–802 (2007).
Zini, A. et al. Antisperm antibodies are not associated with pregnancy rates after IVF and ICSI: systematic review and meta-analysis. Hum. Reprod. 26, 1288–1295 (2011).
Chamley, L. W. & Clarke, G. N. Antisperm antibodies and conception. Semin. Immunopathol. 29, 169–184 (2007).
Cissen, M. Measuring sperm DNA fragmentation and clinical outcomes of medically assisted reproduction: a systematic review and meta-analysis. PLOS One 11, e0165125 (2016).
Esteves, S. C., Sharma, R. K., Gosálvez, J. & Agarwal, A. A translational medicine appraisal of specialized andrology testing in unexplained male infertility. Int. Urol. Nephrol. 46, 1037–1052 (2014).
Majzoub, A., Esteves, S. C., Gosálvez, J. & Agarwal, A. Specialized sperm function tests in varicocele and the future of andrology laboratory. Asian J. Androl. 18, 205–212 (2016).
Spano, M. et al. Sperm chromatin damage impairs human fertility. The Danish first pregnancy planner study team. Fertil. Steril. 73, 43–50 (2000).
Giwercman, A. et al. Sperm chromatin structure assay as an independent predictor of fertility in vivo: a case-control study. Int. J. Androl. 33, e221–227 (2010).
Agarwal, A., Cho, C. L. & Esteves, S. C. Should we evaluate and treat sperm DNA fragmentation? Curr. Opin. Obstet. Gynecol. 28, 164–171 (2016).
Practice Committees of American Society for Reproductive Medicine. The clinical utility of sperm DNA integrity testing: a guideline. Fertil. Steril. 99, 673–677 (2013).
Simon, L., Zini, A., Dyachenko, A., Ciampi, A. & Carrell, D. T. A systematic review and meta-analysis to determine the effect of sperm DNA damage on in vitro fertilization and intracytoplasmic sperm injection outcome. Asian J. Androl. 19, 80–90 (2017).
Osman, A., Alsomait, H., Seshadri, S., El-Toukhy, T. & Khalaf, Y. The effect of sperm DNA fragmentation on live birth rate after IVFI or ICSI: a systematic review and meta-analysis. Reprod. Biomed. Online 30, 120–127 (2015).
Zini, A., Boman, J. M., Belzile, E. & Ciampi, A. Sperm DNA damage is associated with an increased risk of pregnancy loss after IVF and ICSI: systematic review and meta-analysis. Hum. Reprod. 23, 2663–2668 (2008).
Robinson, L. et al. The effect of sperm DNA fragmentation on miscarriage rates: a systematic review and meta-analysis. Hum. Reprod. 27, 2908–2917 (2012).
Zhao, J., Zhang, Q., Wang, Y. & Li, Y. Whether sperm deoxyribonucleic acid fragmentation has an effect on pregnancy and miscarriage after in vitro fertilization/intracytoplasmic sperm injection: a systematic review and meta-analysis. Fertil. Steril. 102, 998–1005 (2014).
Agarwal, A. et al. Clinical utility of sperm DNA fragmentation testing: practice recommendations based on clinical scenarios. Transl Androl. Urol. 5, 935–950 (2016).
Bhattacharya, S. et al. Conventional in-vitro fertilisation versus intracytoplasmic sperm injection for the treatment of non-male-factor infertility: a randomised controlled trial. Lancet 357, 2075–2079 (2001).
Johnson, L. N. C., Sasson, I. E., Sammel, M. D. & Dokras, A. Does intracytoplasmic sperm injection improve the fertilization rate and decrease the total fertilization failure rate in couples with well-defined unexplained infertility? A systematic review and meta-analysis. Fertil. Steril. 100, 704–711 (2013).
Bungum, L., Bungum, M., Humaidan, P. & Andersen, C. Y. A strategy for treatment of couples with unexplained infertility who failed to conceive after intrauterine insemination. Reprod. Biomed. Online 8, 584–589 (2004).
Foong, S. C. et al. A prospective randomized trial of conventional in vitro fertilization versus intracytoplasmic sperm injection in unexplained infertility. J. Assist. Reprod. Genet. 23, 137–140 (2006).
Tannus, S. et al. The role of intracytoplasmic sperm injection in non-male factor infertility in advanced maternal age. Hum. Reprod. 32, 119–124 (2017).
Sfontouris, I. A. et al. Live birth rates using conventional in vitro fertilization compared to intracytoplasmic sperm injection in Bologna poor responders with a single oocyte retrieved. J. Assist. Reprod. Genet. 32, 691–697 (2015).
Poseidon Group (Patient-Oriented Strategies Encompassing IndividualizeD Oocyte Number) et al. A new more detailed stratification of low responders to ovarian stimulation: from a poor ovarian response to a low prognosis concept. Fertil. Steril. 105, 1452–1453 (2016).
Humaidan, P. et al. The novel POSEIDON stratification of ‘low prognosis patients in assisted reproductive technology’ and its proposed marker of successful outcome. F1000Res 5, 2911 (2016).
Ferraretti, A. P. et al. ESHRE consensus on the definition of ‘poor response’ to ovarian stimulation for in vitro fertilization: the Bologna criteria. Hum. Reprod. 26, 1616–1624 (2011).
Artini, P. G. et al. Conventional IVF as a laboratory strategy to rescue fertility potential in severe poor responder patients: the impact of reproductive aging. Gynecol. Endocrinol. 29, 997–1001 (2013).
Zegers-Hochschild, F. et al. The international glossary on infertility and fertility care, 2017. Fertil. Steril. 108, 393–406 (2017).
Thornhill, A. R. et al. ESHRE PGD Consortium ‘best practice guidelines for clinical preimplantation genetic diagnosis (PGD) and preimplantation genetic screening (PGS)’. Hum. Reprod. 20, 35–48 (2005).
Harton, G. L. et al. ESHRE PGD Consortium/Embryology Special Interest Group—best practice guidelines for polar body and embryo biopsy for preimplantation genetic diagnosis/screening (PGD/PGS). Hum. Reprod. 26, 41–46 (2011).
Beukers, F. et al. Morphologic abnormalities in 2-year-old children born after in vitro fertilization/intracytoplasmic sperm injection with preimplantation genetic screening: follow-up of a randomized controlled trial. Fertil. Steril. 99, 408–413 (2013).
Desmyttere, S. et al. Growth and health outcome of 102 2-year-old children conceived after pre-implantation genetic diagnosis or screening. Early Hum. Dev. 85, 755–759.
Liebaers, I. et al. Report on a consecutive series of 581 children born after blastomere biopsy for preimplantation genetic diagnosis. Hum. Reprod. 25, 275–282 (2010).
Winter, C., Van Acker, F., Bonduelle, M. & Desmyttere, S. Psychosocial development of full term singletons, born after preimplantation genetic diagnosis (PGD) at preschool age and family functioning: a prospective case-controlled study and multi-informant approach. Hum. Reprod. 30, 1122–1136 (2015).
Middelburg, K. J. et al. Neurological condition of infants born after in vitro fertilization with preimplantation genetic screening. Pediatr. Res. 67, 430–434 (2010).
Winter, C. et al. Cognitive and psychomotor development of 5- to 6-year-old singletons born after PGD: a prospective case-controlled matched study. Hum. Reprod. 29, 1968–1977 (2014).
Grimstad, F. W., Nangia, A. K., Luke, B., Stern, J. E. & Mak, W. Use of ICSI in IVF cycles in women with tubal ligation does not improve pregnancy or live birth rates. Hum. Reprod. 31, 2750–2755 (2016).
Zafer, M. et al. Effectiveness of semen washing to prevent human immunodeficiency virus (HIV) transmission and assist pregnancy in HIV-discordant couples: a systematic review and meta-analysis. Fertil. Steril. 105, 645–655 (2016).
Savasi, V., Oneta, M., Parrilla, B. & Cetin, I. Should HCV discordant couples with a seropositive male partner be treated with assisted reproduction techniques (ART)? Eur. J. Obstet. Gynecol. Reprod. Biol. 167, 181–184 (2013).
Wu, M. Y. & Ho, H. N. Cost and safety of assisted reproductive technologies for human immunodeficiency virus-1 discordant couples. World J. Virol. 4, 142–146 (2015).
Esteves, S. C., Miyaoka, R. & Agarwal, A. Surgical treatment of male infertility in the era of intracytoplasmic sperm injection - new insights. Clinics 66, 1463–1478 (2011).
Strassburger, D. et al. Very low sperm count affects the result of intracytoplasmic sperm injection. J. Assist Reprod. Genet. 17, 431–436 (2000).
Mitchell, V. et al. Outcome of ICSI with ejaculated spermatozoa in a series of men with distinct ultrastructural flagellar abnormalities. Hum. Reprod. 21, 2065–2074 (2006).
Esteves, S. C. & Agarwal, A. Reproductive outcomes, including neonatal data, following sperm injection in men with obstructive and nonobstructive azoospermia: case series and systematic review. Clinics 68, 141–150 (2013).
Esteves, S. C. et al. Comparison of sperm retrieval and reproductive outcome in azoospermic men with testicular failure and obstructive azoospermia treated for infertility. Asian J. Androl. 16, 602–606 (2014).
Gosálvez, J., Lopez-Fernandez, C., Fernandez, J. L., Esteves, S. C. & Johnston, S. D. Unpacking the mysteries of sperm DNA fragmentation: ten frequently asked questions. J. Reprod. Biotechnol. Fertil. 4, 1–16 (2015).
Hamada, A., Esteves, S. C., Nizza, M. & Agarwal, A. Unexplained male infertility: diagnosis and management. Int. Braz. J. Urol. 38, 576–594 (2012).
Sakkas, D. & Alvarez, J. G. Sperm DNA fragmentation: mechanisms of origin, impact on reproductive outcome, and analysis. Fertil. Steril. 93, 1027–1036 (2010).
Avendaño, C., Franchi, A., Duran, H. & Oehninger, S. DNA fragmentation of normal spermatozoa negatively impacts embryo quality and intracytoplasmic sperm injection outcome. Fertil. Steril. 94, 549–557 (2010).
Aitken, R. J., Bronson, R., Smith, T. B. & De Iullis, G. N. The source and significance of DNA damage in human spermatozoa: a commentary on diagnostic strategies and straw man fallacies. Mol. Hum. Reprod. 19, 474–485 (2013).
Esteves, S. C. et al. Diagnostic accuracy of sperm DNA degradation index (DDSi) as a potential noninvasive biomarker to identify men with varicocele-associated infertility. Int. Urol. Nephrol. 47, 1471–1477 (2015).
Agarwal, A., Sharma, R., Harlev, A. & Esteves, S. C. Effect of varicocele on semen characteristics according to the new 2010 World Health Organization criteria: a systematic review and meta-analysis. Asian J. Androl. 18, 163–170 (2016).
Wang, Y. J., Zhang, R. Q., Lin, Y. J., Zhang, R. G. & Zhang, W. L. Relationship between varicocele and sperm DNA damage and the effect of varicocele repair: a meta-analysis. Reprod. Biomed. Online. 25, 307–314 (2012).
Agarwal, A., Hamada, A. & Esteves, S. C. Insight into oxidative stress in varicocele-associated male infertility: part 1. Nat. Rev. Urol. 9, 678–690 (2012).
Hamada, A., Esteves, S. C. & Agarwal, A. Insight into oxidative stress in varicocele-associated male infertility: part 2. Nat. Rev. Urol. 10, 26–37 (2013).
Zini, A. & Dohle, G. Are varicoceles associated with increased deoxyribonucleic acid fragmentation? Fertil. Steril. 96, 1283–1287 (2011).
Esteves, S. C., Oliveira, F. V. & Bertolla, R. P. Clinical outcome of intracytoplasmic sperm injection in infertile men with treated and untreated clinical varicocele. J. Urol. 184, 1442–1446 (2010).
Esteves, S. C., Roque, M. & Agarwal, A. Outcome of assisted reproductive technology in men with treated and untreated varicocele: systematic review and meta-analysis. Asian J. Androl. 18, 254–258 (2016).
Kirby, E. W., Wiener, L. E., Rajanahally, S., Crowell, K. & Coward, R. M. Undergoing varicocele repair before assisted reproduction improves pregnancy rate and live birth rate in azoospermic and oligospermic men with a varicocele: a systematic review and meta-analysis. Fertil. Steril. 106, 1338–1343 (2016).
Esteves, S. C., Miyaoka, R., Roque, M. & Agarwal, A. Outcome if varicocele repair in men with nonobstructive azoospermia: a systematic review and meta-analysis. Asian J. Androl. 18, 246–253 (2016).
Kovalski, N. N., de Lamirande, E. & Gagnon, C. Reactive oxygen species generated by human neutrophils inhibit sperm motility: protective effect of seminal plasma and scavengers. Fertil. Steril. 58, 809–816 (1992).
Moskovtsev, S. I., Willis, J., White, J. & Mullen, J. B. Leukocytospermia: a relationship to sperm deoxyribonucleic acid integrity in patients evaluated for male factor infertility. Fertil. Steril. 88, 737–740 (2007).
Moskovtsev, S. I. et al. Cause specific treatment in patients with high sperm DNA damage resulted in significant DNA improvement. Syst. Biol. Reprod. Med. 55, 109–115 (2009).
Barraud-Lange, V. et al. Seminal leukocytes are good samaritans for spermatozoa. Fertil. Steril. 96, 1315–1319 (2011).
Ricci, G. et al. Effect of seminal leukocytes on in vitro fertilization and intracytoplasmic sperm injection outcomes. Fertil. Steril 104, 87–93 (2015).
Agarwal, A. & Sekhon, L. H. Oxidative stress and antioxidants for idiopathic oligoasthenoteratospermia: is it justified? Indian J. Urol. 27, 74–85 (2011).
Showell, M. G. et al. Antioxidants for male subfertility. Cochrane Database Syst. Rev. 12, CD007411 (2014).
Morrison, C. D. & Brannigan, R. E. Metabolic syndrome and infertility in men. Best Pract. Res. Clin. Obstet. Gynaecol. 29, 507–515 (2015).
Kasturi, S. S., Tannir, J. & Brannigna, R. E. The metabolic syndrome and male infertility. J. Androl. 29, 251–259 (2008).
Bakos, H. W. et al. Paternal body mass index is associated with decreased blastocyst development and reduced live birth rate following assisted reproductive technology. Fertil. Steril. 95, 1700–1704 (2011).
Keltz, J. et al. Overweight men: clinical pregnancy after ART is decreased in IVF but not in ICSI cycles. J. Assist. Reprod. Genet. 27, 539–544 (2010).
Wang, X. et al. Effects of female and male body mass indices on the treatment outcomes and neonatal birth weights associated with in vitro fertilization/intracytoplasmic sperm injection treatment in China. Fertil. Steril. 106, 460–466 (2016).
Le, W., Su, S. H., Shi, L. H., Zhang, J. F. & Wu, D. L. Effect of male body mass index on clinical outcomes following assisted reproductive technology: a meta-analysis. Andrologia 48, 406–424 (2016).
Dabaja, E. A. & Schlegel, P. N. Medical treatment of male infertility. Transl Andol. Urol. 3, 9–16 (2014).
Fraietta, R., Zylberstejn, D. S. & Esteves, S. C. Hypogonadotropic hypogonadism revisited. Clinics 68, 81–88 (2013).
Schlegel, P. N. Aromatase inhibitors for male infertility. Fertil. Steril. 98, 1359–1362 (2012).
Hussein, A., Ozgok, Y., Ross, L. & Niederberger, C. Clomiphene administration for cases of nonobstructive azoospermia: a multicenter study. J. Androl. 26, 787–791 (2005).
Reifsnyder, J. E., Ramasamy, R., Husseini, J. & Schlegel, P. N. Role of optimizing testosterone before microdissection testicular sperm extraction in men with nonobstructive azoospermia. J. Urol. 188, 535–536 (2012).
Shiraishi, K., Ohmi, C., Shimabukuro, T. & Matsuyama, H. Human chorionic gonadotrophin treatment prior to microdissection testicular sperm extraction in non-obstructive azoospermia. Hum. Reprod. 27, 331–339 (2012).
Ramasamy, R., Stahl, P. J. & Schlegel, P. N. Medical therapy for spermatogenic failure. Asian J. Androl. 14, 57–60 (2012).
Gudeloglu, A., Brahmbhatt, J. V. & Parekattil, S. J. Medical management of male infertility in the absence of a specific etiology. Semin. Reprod. Med. 32, 313–318 (2014).
Garg, H. & Kumar, R. Empirical drug therapy for idiopathic male infertility: what is the new evidence? Urology 86, 1065–1075 (2015).
Attia, A. M., AbouSetta, A. M. & Al-Inany, H. G. Gonadotrophins for idiopathic male factor subfertility. Cochrane Database Syst. Rev. 23, CD005071 (2013).
Baccetti, B. et al. Effect of follicle-stimulating hormone on sperm quality and pregnancy rate. Asian J. Androl. 6, 133–137 (2004).
Caroppo, E., Niederberger, C., Vizziello, G. M. & D’Amato, G. Recombinant human follicle stimulating hormone as a pretreatment for idiopathic oligoasthenoteratozoospermic patients undergoing intracytoplasmic sperm injection. Fertil. Steril. 80, 1398–1403 (2003).
Colacurci, N. et al. Recombinant human FSH reduces sperm DNA fragmentation in men with idiopathic oligoasthenoteratozoospermia. J. Androl. 33, 588–593 (2012).
Simoni, M. et al. Treatment with human, recombinant FSH improves sperm DNA fragmentation in idiopathic infertile men depending on the FSH receptor polymorphism p. N680S: a pharmacogenetic study. Hum. Reprod. 31, 1960–1969 (2016).
Patel, N. & Kashanian, J. A. Thyroid dysfunction and male reproductive physiology. Semin. Reprod. Med. 34, 356–360 (2016).
Krassas, G. E. et al. A prospective controlled study of the impact of hyperthyroidism on reproductive function in males. J. Clin. Endocrinol. Metab. 87, 3667–3671 (2002).
Krajewska-Kulak, E. & Sengupta, P. Thyroid function in male infertility. Front. Endocrino. 13, 174 (2013).
Singh, P., Singh, M., Cugati, G. & Singh, A. K. Hyperprolactinemia: an often missed cause of male infertility. J. Hum. Reprod. Sci. 4, 102–103 (2011).
Glazer, C. H. et al. Risk of diabetes according to male factor infertility: a register-based cohort study. Hum. Reprod. 9, 1–8 (2017).
Esteves, S. C., Schertz, J. C., Verza, Jr, S., Schneider, D. T. & Zabaglia, S. F. A comparison of menotropin, highly-purified menotropin and follitropin alfa in cycles of intracytoplasmic sperm injection. Reprod. Biol. Endocrinol. 7, 111 (2009).
Henkel, R. R. & Schill, W. B. Sperm preparation for ART. Reprod. Biol. Endocrinol. 1, 108 (2003).
Schneider, D., Feijo, C., Verza, Jr, S. & Esteves, S. Effectiveness of sperm washing by discontinuous density gradient centrifugation to remove antibodies bound to the sperm membrane. Med. Express. 1, 123–126 (2014).
Esteves, S. C., Sharma, R. K., Thomas, Jr, A. J. & Agarwal, A. Effect of swim-up sperm washing and subsequent capacitation on acrosome status and functional membrane integrity of normal sperm. Int. J. Fertil. Womens Med. 45, 335–341 (2000).
Rappa, K. L. et al. Sperm processing for advanced reproductive technologies: Where are we today? Biotechnol. Adv. 34, 578–587 (2016).
Said, T. M. & Land, J. A. Effects of advanced selection methods on sperm quality and ART outcome: a systematic review. Hum. Reprod. Update 17, 719–733 (2011).
Simon, L., Ge, S. Q. & Carrell, D. T. Sperm selection based on electrostatic charge. Methods Mol. Biol. 927, 269–278 (2013).
Aitken, R. J. et al. Electrophoretic sperm isolation: optimization of electrophoresis conditions and impact on oxidative stress. Hum. Reprod. 26, 1955–1964 (2011).
Chan, P. J., Jacobson, J. D., Corselli, J. U. & Patton, W. C. A simple zeta method for sperm selection based on membrane charge. Fertil. Steril. 85, 481–486 (2006).
Nasr Esfahani, M. H., Deemeh, M. R., Tavalaee, M., Sekhavati, M. H. & Gourabi, H. Zeta sperm selection improves pregnancy rate and alters sex ratio in male factor infertility patients: a double-blind, randomized clinical trial. Int. J. Fertil. Steril. 10, 253–260 (2016).
Stoffel, M. H. et al. Density and distribution of anionic sites on boar ejaculated and epididymal spermatozoa. Histochem. Cell Biol. 117, 441–445 (2002).
Gil, M., Sar-Shalom, M., Melendez Sivira, Y., Carreras, R. & Checa, M. A. Sperm selection using magnetic activated cell sorting (MACS) in assisted reproduction: a systematic review and meta-analysis. J. Assist Reprod. Genet. 30, 479–485 (2013).
Simopoulou, M. et al. Improving ICSI: a review from the spermatozoon perspective. Syst. Biol. Reprod. Med. 62, 359–371 (2016).
McDowell, S. et al. Advanced sperm selection techniques for assisted reproduction. Cochrane Database Syst. Rev. 10, CD010461 (2014).
Romany, L. et al. Removal of anexin V – positive sperm cells for intracytoplasmic sperm injection in ovum donation cycles does not improve reproductive outcome: a controlled and randomized trial in unselected males. Fertil. Steril. 102, 1567–1575 (2014).
Sakkas, D. Novel technologies for selecting the best sperm for in vitro fertilization and intracytoplasmic sperm injection. Fertil. Steril. 99, 1023–1029 (2013).
Bech-Fruchter, R., Shalev, E. & Weiss, A. Clinical benefit using sperm hyaluronic acid binding technique in ICSI cycles: a systematic review and meta-analysis. Reprod. Biomed. Online. 32, 286–298 (2016).
Vanderzwalmen, P. et al. Blastocyst development after sperm selection at high magnification is associated with size and number of nuclear vacuoles. Reprod. Biomed. Online 17, 617–627 (2008).
Knez, K., Zorn, B., Tomazevic, T., Vrtacnik-Bokal, E. & Virant-Klun, I. The IMSI procedure improves poor embryo development in the same infertile couples with poor semen quality: a comparative prospective randomized study. Reprod. Biol. Endocrinol. 9, 123 (2011).
Berkovitz, A. et al. How to improve IVF-ICSI outcome by sperm selection. Reprod. Biomed. Online 12, 634–638 (2006).
Setti, A. S. et al. Intracytoplasmic morphologically selected sperm injection is beneficial in cases of advanced maternal age: a prospective randomized study. Eur. J. Obstet. Gynecol. Reprod. Biol. 171, 286–290 (2013).
Setti, A. S. et al. Twelve years of MSOME and IMSI: a review. Reprod. Biomed. Online 27, 338–352 (2013).
Teixeira, D. M. et al. Regular (ICSI) versus ultra-high magnification (IMSI) sperm selection for assisted reproduction. Cochrane Database Syst. Rev. 7, CD010167 (2013).
Bradley, C. K. et al. Intervention improves assisted conception intracytoplasmic sperm injection outcomes for patients with high levels of sperm DNA fragmentation: a retrospective analysis. Andrology 4, 903–910 (2016).
Esteves, S. C., Miyaoka, R. & Agarwal, A. Sperm retrieval techniques for assisted reproduction. Int. Braz. Urol. 37, 570–583 (2011).
Esteves, S. C. et al. Reproductive potential of men with obstructive azoospermia undergoing percutaneous sperm retrieval and intracytoplasmic sperm injection according to the cause of obstruction. J. Urol. 189, 232–237 (2013).
Deruyver, Y., Vanderschueren, D. & Van der Aa, F. Outcome of microdissection TESE compared with conventional TESE in non-obstructive azoospermia: a systematic review. Andrology 2, 20–24 (2014).
Esteves, S. C. & Agarwal, A. Re: sperm retrieval rates and intracytoplasmic sperm injection outcomes for men with non-obstructive azoospermia and the health of resulting offspring. Asian J. Androl. 16, 642 (2014).
Esteves, S. C. Microdissection testicular sperm extraction (micro-TESE) as a sperm acquisition method for men with nonobstructive azoospermia seeking fertility: operative and laboratory aspects. Int. Braz. J. Urol. 39, 440 (2013).
Esteves, S. C., Verza, Jr. S. et al. in Practical Manual of In Vitro Fertilization (eds Nagy, Z. P., Varghese, A. C., Agarwal A.) 207–220 (Springer, New York, 2012).
Endo, Y. et al. Simple vitrification for small numbers of human spermatozoa. Reprod. Biomed. Online. 24, 301–307 (2012).
Coetzee, K., Ozgur, K., Berkkanoglu, M., Bulut, H. & Isikli, A. Reliable single sperm cryopreservation in Cell Sleepers for azoospermia management. Andrologia 48, 203–210 (2016).
Van Peperstraten, A., Proctor, M. L., Johnson, N. P. & Philipson, G. Techniques for surgical retrieval of sperm prior to intra-cytoplasmic sperm injection (ICSI) for azoospermia. Cochrane Database Syst Rev. 16, CD002807 (2008).
Van Wely, M., Barbey, N., Meissner, A., Repping, S. & Silber, S. J. Live birth rates after MESA or TESE in men with obstructive azoospermia: is there a difference? Hum. Reprod. 30, 761–766 (2015).
Ohlander, S., Hotaling, J., Kirshenbaum, E., Niederberger, C. & Eisenberg, M. L. Impact of fresh versus cryopreserved testicular sperm upon intracytoplasmic sperm injection pregnancy outcomes in men with azoospermia due to spermatogenic dysfunction: a meta-analysis. Fertil. Steril. 101, 344–349 (2014).
Meijerink, A. M. et al. Prediction model for live birth in ICSI using testicular extracted sperm. Hum. Reprod. 31, 1942–1951 (2016).
Vozdova, M., Heracek, J., Sobotka, V. & Rubes, J. Testicular sperm aneuploidy in non-obstructive azoospermic patients. Hum. Reprod. 27, 2233–2239 (2012).
Greco, E. et al. Efficient treatment of infertility due to sperm DNA dmage by ICSI with testicular spermatozoa. Hum. Reprod. 20, 226–230 (2005).
Esteves, S. C., Sánchez-Martín, F., Sánchez-Martín, P., Schneider, D. T. & Gosálvez, J. Comparison of reproductive outcome in oligozoospermic men with high sperm DNA fragmentation undergoing intracytoplasmic sperm injection with ejaculated and testicular sperm. Fertil. Steril. 104, 1398–1405 (2015).
Moskovtsev, S. I. et al. Testicular spermatozoa have statistically significantly lower DNA damage compared with ejaculated spermatozoa in patients with unsuccessful oral antioxidant treatment. Fertil. Steril. 93, 1142–1146 (2010).
Moskovtsev, S. I. et al. A comparison of ejaculated and testicular spermatozoa aneuploidy rates in patients with high sperm DNA damage. Syst. Biol. Reprod. Med. 58, 142–148 (2012).
Mehta, A., Bolyakov, A., Schlegel, P. N. & Paduch, D. A. Higher pregnancy rates using testicular sperm in men with severe oligospermia. Fertil. Steril. 104, 1382–1387 (2015).
Esteves, S. C., Roque, M. & Garrido, N. Use of testicular sperm for intracytoplasmic sperm injection in men with high sperm DNA fragmentation: a SWOT analysis. Asian J. Androl. 20, 1–8 (2018).
Esteves, S. C., Roque, M., Bradley, C. K. & Garrido, N. Reproductive outcomes of testicular versus ejaculated sperm for intracytoplasmic sperm injection among men with high levels of DNA fragmentation in semen: systematic review and meta-analysis. Fertil. Steril. 108, 456–467 (2017).
Abhyankar, N., Kathrins, M. & Niederberger, C. Use of testicular versus ejaculated sperm for intracytoplasmic sperm injection among men with cryptozoospermia: a meta-analysis. Fertil. Steril. 105, 1469–1475 (2016).
Pabuccu, E. G., Caglar, G. S., Tangal, S., Haliloglu, A. H. & Pabuccu, R. Testicular versus ejaculated spermatozoa in ICSI cycles of normozoospermic men with high sperm DNA fragmentation and previous ART failures. Andrologia 49, https://doi.org/10.1111/and.12609 (2017).
Zini, A., Bach, P. V., Al-Malki, A. H. & Schlegel, P. N. Use of testicular sperm for ICSI in oligozoospermic couples: how far should we go? Hum. Reprod. 32, 7–13 (2017).
Vloeberghs, V., Verheyen, G. & Tournaye, H. Intracytoplasmic spermatid injection and in vitro maturation: fact or fiction? Clinics 68, 151–156 (2013).
Ogura, A., Yanagimachi, R. & Usui, N. Behaviour of hamster and mouse round spermatid nuclei incorporated into mature oocytes by electrofusion. Zygote 1, 1–8 (1993).
Goswami, G., Singh, S. & Devi, M. G. Successful fertilization and embryo development after spermatid injection: a hope for nonobstructive azospermic patients. J. Hum. Reprod. Sci. 8, 175–177 (2015).
Vanderzwalmen, P. et al. Fertilization of an oocyte microinseminated with a spermatid in an in-vitro fertilization programme. Hum. Reprod. 10, 502–503 (1995).
Tesarik, J., Mendoza, C. & Testart, J. Viable embryos from injection of round spermatids into oocyte. N. Engl. J. Med. 333, 525 (1995).
Fischel, S., Aslam, I. & Tesarik, J. Spermatid conception: a stage too early, or a time too soon? Hum. Reprod. 11, 1371–1375 (1996).
Practice Committees of American Society for Reproductive Medicine and Society for Assisted Reproduction Technology. Round spermatid nucleus injection (ROSNI). Fertil. Steril. 90, S199–201 (2008).
Tanaka, A. et al. Fourteen babies born after round spermatid injection into human oocytes. Proc. Natl Acad. Sci. USA 112, 14629–14634 (2015).
Aitken, R. J. & De Iuliis, G. N. Origins and consequences of DNA damage in male germ cells. Reprod. Biomed. Online 14, 727–733 (2007).
Krawetz, S. A. Paternal contribution: new insights and future challenges. Nat. Rev. Genet. 6, 633–642 (2005).
Hamada, A. J., Esteves, S. C. & Agarwal, A. A comprehensive review of genetics and genetic testing in azoospermia. Clinics 68 (Suppl. 1), 39–60 (2013).
Kumar, M., Kumar, K., Jain, S., Hassan, T. & Dada, R. Novel insights into the genetic and epigenetic paternal contribution to the human embryo. Clinics 68 (Suppl. 1), 5–14 (2013).
Lewis, S. E. & Aitken, R. J. DNA damage to spermatozoa has impacts on fertilization and pregnancy. Cell Tissue Res. 322, 33–41 (2005).
Terada, Y., Luetjens, C. M., Sutovsky, P. & Schatten, G. Atypical decondensation of the sperm nucleus, delayed replication of the male genome, and sex chromosome positioning following intracytoplasmic human sperm injection (ICSI) into golden hamster eggs: does ICSI itself introduce chromosomal anomalies? Fertil. Steril. 74, 454–460 (2000).
Van Der Westerlaken, L. A., Helmerhorst, F. M., Hermans, J. & Naaktgeboren, N. Intracytoplasmic sperm injection: position of the polar body affects pregnancy rate. Hum. Reprod. 14, 2565–2569 (1999).
Coates, A. et al. Use of suboptimal sperm increases the risk of aneuploidy of the sex chromosomes in preimplantation blastocyst embryos. Fertil. Steril. 104, 866–872 (2015).
Pandey, S., Shetty, A., Hamilton, M., Bhattacharya, S. & Maheshwari, A. Obstetric and perinatal outcomes in singleton pregnancies resulting from IVF/ICSI: a systematic review and meta-analysis. Hum. Reprod. Update 18, 485–503 (2012).
Hansen, M., Kurinczuk, J. J., Milne, E., de Klerk, N. & Bower, C. Assisted reproductive technology and birth defects: a systematic review and meta-analysis. Hum. Reprod. Update 19, 330–353 (2013).
Qin, J. et al. Assisted reproductive technology and risk of congenital malformations: a meta-analysis based on cohort studies. Arch. Gynecol. Obstet. 292, 777–798 (2015).
Wen, J. et al. Birth defects in children conceived by in vitro fertilization and intracytoplasmic sperm injection: a meta-analysis. Fertil. Steril. 97, 1331–1337 (2012).
Rimm, A. A., Katayama, A. C. & Katayama, K. P. A meta-analysis of the impact of IVF and ICSI on major malformations after adjusting for the effect of subfertility. J. Assist Reprod. Genet. 28, 699–705 (2011).
Massaro, P. A., MacLellan, D. L., Anderson, P. A. & Romao, R. L. Does intracytoplasmic sperm injection pose an increased risk of genitourinary congenital malformations in offspring compared to in vitro fertilization? A systematic review and meta-analysis. J. Urol. 193, 1837–1842 (2015).
Rossi, A. C. & D’Addario, V. Neonatal outcomes of assisted and naturally conceived twins: systematic review and meta-analysis. J. Perinat Med. 39, 489–493 (2011).
Zhu, J. L., Basso, O., Obel, C., Bille, C. & Olsen, J. Infertility, infertility treatment, and congenital malformations: Danish national birth cohort. BMJ 333, 679AE (2006).
Kissin, D. M. et al. Association of assisted reproductive technology (ART) treatment and parental infertility diagnosis with autism in ART-conceived children. Hum. Reprod. 30, 454–465 (2015).
Tollervey, J. R. & Lunyak, V. V. Epigenetics: judge, jury and executioner of stem cell fate. Epigenetics 7, 823–840 (2012).
Geiman, T. M. & Robertson, K. D. Chromatin remodeling, histone modifications, and DNA methylation-how does it all fit together? J. Cell. Biochem. 87, 117–125 (2002).
Bunkar, N., Pathak, N., Lohiya, N. K. & Mishra, P. K. Epigenetics: a key paradigm in reproductive health. Clin. Exp. Reprod. Med. 43, 59–81 (2016).
Hogg, K. & Western, P. S. Refurbishing the germline epigenome: Out with the old, in with the new. Semin. Cell Dev. Biol. 45, 104–113 (2015).
Odom, L. N. & Segars, J. Imprinting disorders and assisted reproductive technology. Curr. Opin. Endocrinol. Diabetes Obes. 17, 517–522 (2010).
Gosden, R., Trasler, J., Lucifero, D. & Faddy, M. Rare congenital disorders, imprinted genes, and assisted reproductive technology. Lancet 361, 1975–1977 (2003).
Kobayashi, H. et al. Aberrant DNA methylation of imprinted loci in sperm from oligospermic patients. Hum. Mol. Genet. 16, 2542–2551 (2007).
de Waal, E. et al. Gonadotropin stimulation contributes to an increased incidence of epimutations in ICSI-derived mice. Hum. Mol. Genet. 21, 4460–4472 (2012).
Hartmann, S., Bergmann, M., Bohle, R. M., Weidner, W. & Steger, K. Genetic imprinting during impaired spermatogenesis. Mol. Hum. Reprod. 12, 407–411 (2006).
Marques, C. et al. Abnormal methylation of imprinted genes in human sperm is associated with oligozoospermia. Mol. Hum. Reprod. 14, 67–74 (2008).
Kobayashi, H. et al. DNA methylation errors at imprinted loci after assisted conception originate in the parental sperm. Eur. J. Hum. Genet. 17, 1582–1591 (2009).
Marques, C. et al. Methylation defects of imprinted genes in human testicular spermatozoa. Fertil. Steril. 94, 585–594 (2010).
Boissonnas, C. et al. Specific epigenetic alterations of IGF2-H19 locus in spermatozoa from infertile men. Eur. J. Hum. Genet. 18, 73–80 (2010).
Gomes, M. V., Huber, J., Ferriani, R. A., Amaral Neto, A. M. & Ramos, E. S. Abnormal methylation at the KvDMR1 imprinting control region in clinically normal children conceived by assisted reproductive technologies. Mol. Hum. Reprod. 15, 471–477 (2009).
Kanber, D., Buiting, K., Zeschnigk, M., Ludwig, M. & Horsthemke, B. Low frequency of imprinting defects in ICSI children born small for gestational age. Eur. J. Hum. Genet. 17, 22–29 (2009).
Tierling, S. et al. Assisted reproductive technologies do not enhance the variability of DNA methylation imprints in human. J. Med. Genet. 47, 371–376 (2010).
King, J. L. et al. Skewed X inactivation and IVF-conceived infants. Reprod. Biomed. Online 20, 660–663 (2010).
Turan, N. et al. Inter- and intra-individual variation in allele-specific DNA methylation and gene expression in children conceived using assisted reproductive technology. PLOS Genet. 6, e1001033 (2010).
Wong, E. C., Hatakeyama, C., Robinson, W. P. & Ma, S. DNA methylation at H19/IGF2 ICR1 in the placenta of pregnancies conceived by in vitro fertilization and intracytoplasmic sperm injection. Fertil. Steril. 95, 2524–2526.e3 (2011).
Li, L. et al. Evaluation of DNA methylation status at differentially methylated regions in IVF-conceived newborn twins. Fertil. Steril. 95, 1975–1979 (2011).
Feng, C. et al. General imprinting status is stable in assisted reproduction-conceived offspring. Fertil. Steril. 96, 1417–1423.e9 (2011).
Oliver, V. F. et al. Defects in imprinting and genome-wide DNA methylation are not common in the in vitro fertilization population. Fertil. Steril. 97, 147–153 (2012).
Rancourt, R. C., Harris, H. R. & Michels, K. B. Methylation levels at imprinting control regions are not altered with ovulation induction or in vitro fertilization in a birth cohort. Hum. Reprod. 27, 2208–2216 (2012).
Puumala, S. E. et al. Similar DNA methylation levels in specific imprinting control regions in children conceived with and without assisted reproductive technology: a cross-sectional study. BMC Pediatr. 12, 33 (2012).
Hiura, H. et al. Characterization of DNA methylation errors in patients with imprinting disorders conceived by assisted reproduction technologies. Hum. Reprod. 27, 2541–2548 (2012).
Nelissen, E. C. et al. Placentas from pregnancies conceived by IVF/ICSI have a reduced DNA methylation level at the H19 and MEST differentially methylated regions. Hum. Reprod. 28, 1117–1126 (2013).
Sakian, S. et al. Altered gene expression of H19 and IGF2 in placentas from ART pregnancies. Placenta 36, 1100–1105 (2015).
Melamed, N., Choufani, S., Wilkins-Haug, L. E., Koren, G. & Weksberg, R. Comparison of genome-wide and gene-specific DNA methylation between ART and naturally conceived pregnancies. Epigenetics 10, 474–483 (2015).
Vincent, R. N., Gooding, L. D., Louie, K., Chan Wong, E. & Ma, S. Altered DNA methylation and expression of PLAGL1 in cord blood from assisted reproductive technology pregnancies compared with natural conceptions. Fertil. Steril. 106, 739–748.e3 (2016).
Mehdi, M. et al. Aneuploidy rate in spermatozoa of selected men with severe teratozoospermia. Andrologia 44 (Suppl. 1), 139–143 (2012).
Hassold, T. et al. Human aneuploidy: incidence, origin, and etiology. Environ. Mol. Mutag. 28, 167–175 (1996).
Morales, C. et al. Cytogenetic study of spontaneous abortions using semi-direct analysis of chorionic villi samples detects the broadest spectrum of chromosome abnormalities. Am. J. Med. Genet. A 146A, 66–70 (2008).
Griffin, D. K., Hyland, P., Tempest, H. G. & Homa, S. T. Safety issues in assisted reproduction technology: should men undergoing ICSI be screened for chromosome abnormalities in their sperm? Hum. Reprod. 18, 229–235 (2003).
Kushnir, V. A. & Frattarelli, J. L. Aneuploidy in abortuses following IVF and ICSI. J. Assist Reprod. Genet. 26, 93–97 (2009).
Magli, M. C. et al. Paternal contribution to aneuploidy in preimplantation embryos. Reprod. Biomed. Online 18, 536–542 (2009).
Rodrigo, L. et al. Testicular sperm from patients with obstructive and nonobstructive azoospermia: aneuploidy risk and reproductive prognosis using testicular sperm from fertile donors as control samples. Fertil. Steril. 95, 1005–1012 (2011).
Bingol, B., Abike, F., Gedikbasi, A., Tapisiz, O. L. & Gunenc, Z. Comparison of chromosomal abnormality rates in ICSI for non-male factor and spontaneous conception. J. Assist Reprod. Genet. 29, 25–30 (2012).
Ghoraeian, P., Mozdarani, H., Aleyasin, A. & Alizadeh-Nili, H. Frequency of sex chromosomal disomy in spermatozoa of normal and oligozoospermic Iranian patients and its effects on fertilisation and implantation rates after ICSI. Andrologia 45, 46–55 (2013).
Mau Kai, C. et al. Reduced serum testosterone levels in infant boys conceived by intracytoplasmic sperm injection. J. Clin. Endocrinol. Metab. 92, 2598–2603 (2007).
Jensen, T. K. et al. Fertility treatment and reproductive health of male offspring: a study of 1,925 young men from the general population. Am. J. Epidemiol. 165, 583–590 (2007).
Belva, F. et al. Semen quality of young adult ICSI offspring: the first results. Hum. Reprod. 31, 2811–2820 (2016).
Belva, F. et al. Reproductive hormones of ICSI-conceived young adult men: the first results. Hum. Reprod. 32, 439–446 (2017).
Belva, F. et al. Serum reproductive hormone levels and ultrasound findings in female offspring after intracytoplasmic sperm injection: first results. Fertil. Steril. 107, 934–939 (2017).
Andersson, A. M., Jorgensen, N., Frydelund-Larsen, L., Rajpert-De Meyts, E. & Skakkebaek, N. E. Impaired Leydig cell function in infertile men: a study of 357 idiopathic infertile men and 318 proven fertile controls. J. Clin. Endocrinol. Metab. 89, 3161–3167 (2004).
Lightfoot, T. J. & Roman, E. Causes of childhood leukaemia and lymphoma. Toxicol. Appl. Pharmacol. 199, 104–117 (2004).
Raimondi, S., Pedotti, P. & Taioli, E. Meta-analysis of cancer incidence in children born after assisted reproductive technologies. Br. J. Cancer 93, 1053–1056 (2005).
Hargreave, M., Jensen, A., Toender, A., Andersen, K. K. & Kjaer, S. K. Fertility treatment and childhood cancer risk: a systematic meta-analysis. Fertil. Steril. 100, 150–161 (2013).
Williams, C. L. et al. Cancer risk among children born after assisted conception. N. Engl. J. Med. 369, 1819–1827 (2013).
Sundh, K. J. et al. Cancer in children and young adults born after assisted reproductive technology: a Nordic cohort study from the Committee of Nordic ART and Safety (CoNARTaS). Hum. Reprod. 29, 2050–2057 (2014).
Reigstad, M. M. et al. Risk of cancer in children conceived by assisted reproductive technology. Pediatrics 137, e20152061 (2016).
Källén, B. et al. Cancer risk in children and young adults conceived by in vitro fertilization. Pediatrics 126, 270–276 (2010).
Bay, B., Mortensen, E. L. & Kesmodel, U. S. Assisted reproduction and child neurodevelopmental outcomes: a systematic review. Fertil. Steril. 100, 844–853 (2013).
Pinborg, A. et al. Why do singletons conceived after assisted reproduction technology have adverse perinatal outcome? Systematic review and meta-analysis. Hum. Reprod. Update 19, 87–104 (2013).
Carson, C. et al. Cognitive development following ART: effect of choice of comparison group, confounding and mediating factors. Hum. Reprod. 25, 244–252 (2010).
Meijerink, A. M. et al. Behavioral, cognitive, and motor performance and physical development of five-year-old children who were born after intracytoplasmic sperm injection with the use of testicular sperm. Fertil. Steril. 106, 1673–1682.e5 (2016).
Tsai, C. C. et al. Clinical outcomes and development of children born after intracytoplasmic sperm injection (ICSI) using extracted testicular sperm or ejaculated extreme severe oligo-astheno-teratozoospermia sperm: a comparative study. Fertil. Steril. 96, 567–571 (2011).
Sandin, S., Nygren, K. G., Iliadou, A., Hultman, C. M. & Reichenberg, A. Autism and mental retardation among offspring born after in vitro fertilization. JAMA 310, 75–84 (2013).
Ilioi, E. C. & Golombok, S. Psychological adjustment in adolescents conceived by assisted reproduction techniques: a systematic review. Hum. Reprod. Update 21, 84–96 (2015).
Spangmose, A. L. et al. Academic performance in adolescents born after ART-a nationwide registry-based cohort study. Hum. Reprod. 32, 447–456 (2017).
Balayla, J. et al. Neurodevelopmental outcomes after assisted reproductive technologies. Obstet. Gynecol. 129, 265–272 (2017).
Guo, X. Y. et al. Cardiovascular and metabolic profiles of offspring conceived by assisted reproductive technologies: a systematic review and meta-analysis. Fertil. Steril. 107, 622–631 (2017).
Leary, C., Leese, H. J. & Sturmey, R. G. Human embryos from overweight and obese women display phenotypic and metabolic abnormalities. Hum. Reprod. 30, 122–132 (2015).
Ebner, T. et al. Quantitative and qualitative trophectoderm grading allows for prediction of live birth and gender. J. Assist Reprod. Genet. 33, 49–57 (2016).
Pontesilli, M. et al. Subfertility and assisted reproduction techniques are associated with poorer cardiometabolic profiles in childhood. Reprod. Biomed. Online 30, 258–267 (2015).
Ceelen, M. et al. Cardiometabolic differences in children born after in vitro fertilization: follow-up study. J. Clin. Endocrinol. Metab. 93, 1682–1688 (2008).
Belva, F. et al. Are ICSI adolescents at risk for increased adiposity? Hum. Reprod. 27, 257–264 (2012).
Belva, F. et al. Blood pressure in ICSI-conceived adolescents. Hum. Reprod. 27, 3100–3108 (2012).
Gkourogianni, A. et al. Plasma metabolomic profiling suggests early indications for predisposition to latent insulin resistance in children conceived by ICSI. PLOS One 9, e94001 (2014).
van der Steeg, J. W. et al. Obesity affects spontaneous pregnancy chances in subfertile, ovulatory women. Hum. Reprod. 23, 324–328 (2008).
Malvezzi, H. et al. Sperm quality after density gradient centrifugation with three commercially available media: a controlled trial. Reprod. Biol. Endocrinol. 12, 121 (2014).
The Center of Assisted Reproduction. Embryological procedures. Masaryk University http://www.ivfbrno.cz/en/embryological-procedures/t1046 (2018).
Van Soom, A. et al. Epigenetics and the periconception environment in ruminants. Proc. Belg. R. Acad. Med. 2, 1–23 (2013).
Review criteria
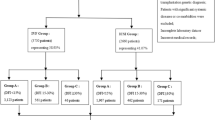
An extensive search of studies examining the relationship between intracytoplasmic sperm injection and male infertility was performed using PubMed and MEDLINE. The start and end dates for the search were January 2006 and February 2017, respectively. The overall strategy for study identification and data extraction was based on the following key words: “assisted reproductive technology”, “intracytoplasmic sperm injection”, “male infertility”, “pregnancy outcomes”, and “children”, with the filters “humans” and “English language”. Using the aforementioned criteria, 209 relevant articles were identified. Data that were solely published in conference or meeting proceedings, websites, or books were not included. Citations dated outside the search dates were included only if they provided conceptual content.
Author information
Authors and Affiliations
Contributions
S.C.E. designed the manuscript, helped in data interpretation and coordination, and drafted the manuscript. M.R., G.B., and T.H. participated in the acquisition of data and drafted the manuscript. P.H. helped in data interpretation and coordination and drafted and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Esteves, S.C., Roque, M., Bedoschi, G. et al. Intracytoplasmic sperm injection for male infertility and consequences for offspring. Nat Rev Urol 15, 535–562 (2018). https://doi.org/10.1038/s41585-018-0051-8
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41585-018-0051-8
This article is cited by
-
Second ejaculation produces good quality sperm and blastocyst and decreases the rate of unexpected ICSI cycle: a propensity score-matched analysis
Middle East Fertility Society Journal (2024)
-
Sperm Preparation with Microfluidic Sperm Sorting Chip May Improve Intracytoplasmic Sperm Injection Outcomes Compared to Density Gradient Centrifugation
Reproductive Sciences (2024)
-
CCDC28A deficiency causes sperm head defects, reduced sperm motility and male infertility in mice
Cellular and Molecular Life Sciences (2024)
-
Clinical outcome of different embryo transfer strategies after late rescue ICSI procedure: a 10-year total fertilisation failure cohort study
BMC Pregnancy and Childbirth (2023)
-
Male infertility
Nature Reviews Disease Primers (2023)