Abstract
The role of the immune system as an integral component of the inflammatory response in the pathophysiology of migraine remains unclear. The aim of this study was to evaluate the differences in immune system parameters (acquired immunity parameters) in patients with episodic migraine (EM) and in healthy controls. In EM patients, we aimed to determine whether the changes found in peripheral blood parameters were related to migraine severity according to the standardised MIDAS and HIT-6 tests. Forty-nine patients with EM and 50 healthy controls were included in this study. The authors compared different lymphocyte parameters obtained by multicolor flow cytometry in the EM and control groups by performing statistical tests. The relationship between the changes in peripheral blood parameters and migraine severity in EM patients was investigated using correlation and regression analysis. EM patients showed higher values than healthy controls, especially in nine parameters: relative count of lymphocytes, relative and absolute counts of CD3 T cells, relative and absolute counts of CD8 suppressor cytotoxic T cells, relative and absolute counts of CD4 + TEMRA (terminally differentiated helper T lymphocytes), absolute count of CD8 naïve T cells, and absolute count of CD19 switched memory B cells. Among the lymphocyte parameters, CD4 + TEM (effector memory helper T lymphocytes) and CD8 + TEMRA (terminally differentiated cytotoxic T lymphocytes) were statistically significantly associated with HIT-6. Patients with a CD4 + TEM value below 15 had a high probability (90%) that the HIT-6 value would be higher than 60. The results of this study show that EM patients have changes in immune system parameters measured in the peripheral blood. Changes in the abundance of CD4 + TEM could be used as a biomarker for disease severity.
Similar content being viewed by others
Introduction
Migraine is the sixth most common cause of disability worldwide, and it significantly worsens the quality of life of affected individuals and places a great economic burden on society1. An extensive European research study reported a big effect of migraine among 17.7% of men and 28.0% of women losing within 10 days of activities during a 3-month period2. Sokolovic et al.3 revealed that persons with headaches lost 10.2 workday equivalents per year (estimated from absenteeism and days with productivity reduction ≥ 50%, typically without including days with productivity reduction < 50%)3. An American study stated that, of the total $13 billion economic burden from migraine, impaired work function accounted for $5 billion and that direct medical costs only reached $1 billion4.
Intensive research in recent years has greatly increased the understanding of the pathophysiology of this disease and has contributed to the discovery of new drugs that were developed based on the knowledge of pathophysiological processes. A migraine headache is caused by the depolarisation of nociceptive trigeminal nerve fibres belonging to the trigeminovascular system. When the trigeminovascular system is stimulated, the vasoactive neurotransmitters are released from the perivascular nerve endings such as Calcitonin Gene-Related Peptide (CGRP), substance P and neurokinin A, all which cause vasodilation of the meningeal vessels and sterile perivascular neurogenic inflammation5.
The role of the immune system in the pathophysiology of migraine remains unclear6. Moskovitz first suggested the idea that local neurogenic inflammation due to the release of neuropeptides from meningeal nerves is involved in migraine7. Neurogenic inflammation occurs when vasoactive neurotransmitters, especially CGRP, release inflammatory mediators such as serotonin, histamine and prostaglandins from activated and degranulated dural mast cells. Anti-migraine drugs like sumatriptan or naratriptan can inhibit plasma protein extravasation in the dura mater8,9. On top of that, the efficacy of nonsteroidal anti-inflammatory drugs in the inhibition of dural plasma protein extravasation are additional arguments for a pathogenic role of meningeal neurogenic inflammation in migraine as well as the elevated CGRP levels that were found in plasma samples obtained from the jugular vein during a migraine attack10.
The results of a number of already published studies indicate altered immune function in migraineurs. Fidan et al. studied the role played by cytokines in migraine. They described significantly higher IL-6 levels in migraine patients11. Other studies from the last decade have shown, among other things, a reduction in CD4 + CD25 + regulatory T cells in migraine; changes in lymphocyte subsets in paediatric migraine (lower CD8 + prevalence and a higher CD4 + /CD8 + ratio in the ictal phase irrespective of migraine subtype); higher CD3, CD4, CD8 and CD19 in patients with chronic migraine compared to patients with episodic migraine; and an increased proportion of Treg CD45R0 + CD62L– and CD45R0–CD62L– cells12,13,14,15.
The purpose of this article was to evaluate the differences in immune system parameters (adaptive immunity parameters) in peripheral blood in patients with episodic migraine (EM) and in healthy controls. We also aimed to determine whether the changes found in peripheral blood parameters in EM patients were related to migraine severity according to the standardised MIDAS and HIT-6 tests and to thus find a biomarker that determines the severity of migraine.
Materials and methods
Study population
This observational study was conducted from January 2019 to May 2019. A total of 99 volunteers were enrolled in the study. Forty-nine volunteers were patients with episodic migraine. Fifty patients were healthy controls (HCs) without any comorbidities who had never experienced headaches in their life and were 18–65 years of age. All of the volunteers with EM were all patients of the Department of Neurology of the University Hospital in Hradec Králové, Czech Republic. The eligibility criteria for patients with EM included being aged 18–65 years with EM without aura based on the International Classification of Headache Disorders 3rd edition for migraine without aura16, a history of migraine without aura of at least 1 year, migraine onset prior to age 50, at least 1 migraine attack per month on average within the past 3 months and no comorbidities. During the analysis, no EM patients had used any prophylactic medication to date. The analysis (peripheral blood samples) was performed at least one week after the last episode of migraine.
All participants provided written informed consent. This study was approved by the ethics committee of the University Hospital Hradec Králové. The trial was registered under reference number 201809S18P.
Flow cytometry and haematology
The authors collected blood samples from the antecubital fossa vein into sample tubes pre-coated with EDTA anticoagulant. The blood count was performed with a Sysmex XN‐3,000. For the surface staining of lymphocytes, 50 µl of blood was added to tubes containing 5 µl of fluorochrome-labelled monoclonal antibodies. All the antibodies used and their source information and dilution factors are summarised in Supplementary Table 1.
Blood samples were incubated with antibodies for 15 min at room temperature in the dark. Then a lysis solution (OptiLyse C, Beckman Coulter) was added, and the mixture was incubated for another 10 min. Flow cytometric evaluation was conducted with a Navios 10 flow cytometer (Beckman Coulter). All the data were then assessed using Kaluza 2.1 Analysis Software (Beckman Coulter). A minimum of 30,000 events were obtained for each stain and were supplied in list mode. Multiple peripheral blood parameters were assessed as absolute and relative values. The gating strategies for the different lymphocyte subsets assessed were as follows: lymphocytes (low SSC/CD45 + +), T lymphocytes (CD3 +), B lymphocytes (CD19 +), natural killer (NK) cells (CD3-CD16 + and/or CD56 +), helper T lymphocytes (CD3 + CD4 +), cytotoxic T lymphocytes (CD3 + CD8 +), naïve helper T lymphocytes (CD3 + CD4 + CD45RA + CD62L +), terminally differentiated helper T lymphocytes—CD4 + TEMRA (CD3 + CD4 + CD45RA + CD62L-), central memory helper T lymphocytes (CD3 + CD4 + CD45RA-CD62L +), effector memory helper T lymphocytes—CD4 + TEM (CD3 + CD4 + CD45RA-CD62L-), naïve cytotoxic T lymphocytes (CD3 + CD8 + CD45RA + CD62L +), terminally differentiated cytotoxic T lymphocytes—CD8 + TEMRA (CD3 + CD8 + CD45RA + CD62L-), central memory cytotoxic T lymphocytes (CD3 + CD8 + CD45RA-CD62L +), effector memory cytotoxic T lymphocytes (CD3 + CD8 + CD45RA-CD62L-), regulatory T lymphocytes (CD3 + CD4 + CD25 + + CD127-), regulatory T lymphocytes CD45RA + (CD3 + CD4 + CD25 + + CD127-, CD45RA +), activated T lymphocytes (CD3 + CD69 +), activated B lymphocytes (CD19 + CD69 +), activated NK cells (CD3-CD56 + and/or CD16 + CD69 +), CD57-positive T lymphocytes (CD3 + CD57 +), CD57-positive NK cells (CD3-CD56 + and/or CD16 + CD57 +), naïve B lymphocytes (CD19 + IgD + CD27), non-switched memory B lymphocytes (CD19 + IgD + CD27 +), class-switched memory B lymphocytes (CD19 + IgD-CD27 +) and double-negative B lymphocytes (CD19 + IgD-CD27-). The gating strategy for the different lymphocyte subsets is presented in supplementary Figs. 1–3. The absolute values were calculated from the blood counts, and the relative values were calculated as the percentage of the population described. The data denoted with abs represent an absolute value. All methods were performed in accordance with the relevant guidelines and regulations.
MIDAS
The MIDAS is a self‐reporting instrument that was administered to the patients to measure MIDAS, headache pain intensity, and headache attack frequency. According to the total score (0–21 and more), the severity of the migraine is classified into grades I–IV (I = little or no disability, II = mild disability, III = moderate disability and IV = severe disability)17. In the study, the MIDAS score was analysed as a dichotomous variable: low to moderate levels of disability (MIDAS scores = 0–20) and severe levels of disability (MIDAS score ≥ 21).
HIT-6
The Headache Impact Test-6 (HIT-6) was developed to measure a wide spectrum of factors contributing to the burden of a headache, and it has demonstrated utility for generating quantitative and pertinent information on the impact of a headache. The disability was classified using the following two impact grades based on the HIT-6 score: little to substantial impact (HIT-6 score: 36–59) and severe impact (HIT-6 score: > 60)18,19.
Statistical analysis
A total of 49 EM patients and 50 healthy controls (HCs) were studied. First, we used t-tests (for normally distributed parameters) or a non-parametric Mann–Whitney U test with non-pooled SDs (for non-normally distributed parameters) to compare differences in the mean or median values of 52 lymphocyte characteristics (parameters) between the groups. Lilliefors normality test was used to assess whether the parameter was normally or non-normally distributed. However, for the categorical sex parameter, a chi-square test of independence was used. The Benjamini–Hochberg (B–H) procedure was used to minimise the false discovery rate. The effect size for all numerical parameters (except for sex) was assessed by Cohen's d, which is the standardised difference between group means. Cramér's V is reported for sex.
The relationships between each of the 3 EM parameters (MIDAS score, MIDAS severity and HIT-6) and each of the 52 lymphocyte characteristics within the patient group were examined first by Spearman’s correlation coefficient (rho). Next, we examined the relationships between EM parameters and lymphocyte characteristics using regression analysis. We categorised the numerical HIT-6 outcome as a binary variable with a threshold value of 60. For binary HIT-6 and MIDAS severity outcomes, we ran a series of univariate logistic regression models (with lymphocyte parameters as explanatory variables). The logarithmised MIDAS score outcome was fitted to an OLS regression model. Thereafter, the statistical significance of parameters was validated using an adjusted (multivariate) logistic (OLS) regression model with added covariates (sex and age) to reduce the (latent) possible effect of these covariates on the EM parameters. The goodness of fit of each univariate and multivariate logistic regression model (strength of association) was evaluated by the index of determination (R2) for OLS models and Nagelkerke pseudo-R2 for logistic regression models. Both correlation and regression analyses were performed on a subgroup of 44 EM patients. This group contained 44 patients who all had lymphocyte parameters measured (no missing values for any parameters) and who did not have extreme values. An extreme value was a value that is five times the interquartile range away from the median. All analyses were performed using the statistical software R (www.r-project.org/); the reported p-values are two-tailed, and a 5% significance level was chosen.
Results
Characteristics of EM patients and HC
There were 38 (77.6%) females among the EM patients and 37 (74.0%) females among the HCs; therefore, the number of females in each group was nearly identical. The EM patients were 4 years younger on average than the HC patients (EM: mean = 41. 0 (interquartile range = 18); HC: 47.5 (17)). The demographic characteristics are summarised Table 1.
Comparison of the parameters of the immune system between EM patients and the control group
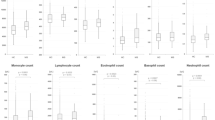
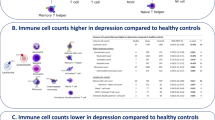
EM patients differed from healthy controls in several parameters. Table 2 shows the description and comparison of lymphocyte parameters with main changes between EM patients and healthy controls. Supplementary Table 2 shows all the parameters.
The groups differed moderately (effect size > 0.6) and with a p-value < 0.10 in 4 parameters: relative count of lymphocytes, relative and absolute number of CD3 T cells, and absolute number of CD4 + TEMRA, and the values in the EM patients were clearly higher than those in the healthy controls. In addition, other five parameters, relative number of CD4 + TEMRA and both relative and absolute numbers of CD8 T cells, absolute number of naïve CD8 T cells and the absolute number of CD19 switched memory B cells, have shown changes between EM patients and healthy subjects (Table 2).
Correlation between immune system parameters and migraine severity
Subsequently, a correlation analysis (Spearman's rho) was performed between each pair of lymphocyte parameters (52 parameters) with paraclinical tests (MIDAS, MIDAS degree and HIT-6). In the MIDAS degree, patients were divided into four groups according to the values of the MIDAS test.
Correlations were evaluated for a subgroup of 44 (out of 49) patients for whom all values were measured and whose values were not extreme (5 × the IQR from the median). Table 3 summarises the statistically significant correlations. Supplementary Table 3 reports all the correlation coefficients.
Among the lymphocyte parameters, CD4 + TEM (% of CD4 + ; rho equal to − 0.40) and CD8 + TEMRA (% of CD8 + ; rho equal to − 0.41) were negatively correlated with the HIT-6 at a 5% significance level. A negative correlation indicated that lower values of the HIT-6 occurred with higher values of these parameters. A weak correlation with a p-value < 0.10 was observed between the HIT-6 and 2 parameters, CD3 + CD57 + (% of CD3 +) (− 0.34) and Treg CD45RA + (% of Treg) (0.33).
Regression modelling of migraine severity
MIDAS degree modelling using logistic regression
For MIDAS degree regression modelling, patients were divided into two groups according to the MIDAS test values. The first subgroup included patients with MIDAS values of 1–3 (MIDAS scores = 0–20), and the second subgroup included patients with MIDAS 4 values (MIDAS score ≥ 21). The modelling was performed using logistic regression. Table 4 shows the regression analysis results (95% confidence interval, odds ratio estimates and the pseudo-R2) for the lymphocyte parameters with main changes (p value < 0.1). Supplementary Table 4 reports all the regression results.
In the group of patients with a lower MIDAS degree (1, 2 or 3), there were 26 patients (18 (69%) females) with a mean age of 42.9 years, and in the MIDAS degree 4 group, there were 18 patients (16 (88.9%) females) with a mean age of 38.5 years. None of the lymphocyte parameters explained (variability of the values) the MIDAS degree and were statistically significant (Table 4). However, 2 lymphocyte parameters, CD3 + CD57 + (p = 0.058; R2 = 0.13) and CD19 non-switched memory abs (0.095; 0.09), displayed p-values < 0.10. These parameters were not significant at a 10% significance level after adjusting for age and gender. These results (after changing the MIDAS categorisations from 4 to 2 groups) differed from the correlation results. For the 4-degree MIDAS, there were no significant parameters (Table 4).
Neither age nor gender explain the MIDAS degree. As expected, the MIDAS degree was best explained by another parameter of migraine, the HIT-6 (0.027; 0.18).
MIDAS 0–100 value modelling by a regression model (OLS)
A MIDAS value in the range of 0–100 explained (“predicted”) with p value < 0.10 1 lymphocyte parameter, CD4 + TEM (% of CD4 +) (0.068; 0.08). Age significantly explained the MIDAS numerical value (0.017; 0.13). The combination of age and NK CD69 + explained 17% of the variability.
HIT-6 modelling (categorised as < 60 and > = 60) using logistic regression
Correlation of four parameters with HIT-6 (as described in correlation analysis results) has p value < 0.10: Treg CD45RA + (% of Treg), CD4 + TEM (% of CD4 +), CD8 + TEMRA (% of CD8 +), and CD3 + CD57 + (% of CD3 +). When the outcome of the HIT-6 was categorised, the study was limited to a low number of patients with HIT-6 values up to 60. (Only 9 patients had HIT-6 values of less than 60, and 35 patients had values of 60 and more, specifically 60–74).
The absolute number of CD45RA + Treg cells for patients with HIT < 60 (25.6 (13.9)) is lower compared to patients with HIT-6 > 60 (35.2 (16.1)) (Supplementary Fig. 4A). On the contrary, CD4 + TEM are statistically significantly (P value = 0.023) augmented in patients with a lower disease severity (HIT-6 < 60; 24.6 (11.4)) vs. severe patients (HIT-6 > 60; 16.4 (9.4)) (Supplementary Fig. 4B). The same (but not statistically significant) happened for CD8 + TEMRA (HIT-6 < 60; 25.1 (18.1) vs. HIT-6 > 60; 21.4 (16.8)), and CD3 + CD57 + (HIT-6 < 60; 24.8 (20.9) vs. HIT-6 > 60; 11.8 (9.0)) (Supplementary Fig. 4C and D).
Conclusions on non-identification should be interpreted with caution because of the small number of patients CD4 + TEM values up to 20 predicted a high probability that the HIT-6 > 60 (Fig. 1).
Predicted probability of a HIT-6 value of greater than or equal to 60 based on the CD4 EM values. The blue curve shows the predicted probability (point estimator) of a HIT-6 value of greater than or equal to 60 for the range of observed CD4 EM values. The shaded (light red) area depicts the 95% confidence interval estimate of the probability.
Discussion
The objective of this study was to evaluate the differences in acquired immunity parameters in patients with EM and in healthy controls. In our study, EM patients showed higher values than healthy controls for nine parameters: the relative count of lymphocytes, relative and absolute counts of CD3 T cells, relative and absolute counts of CD8 suppressor cytotoxic T cells, relative and absolute counts of CD4 + TEMRA, absolute count of CD8 naïve T cells, and absolute count of CD19 switched memory B cells respectively.
CD4 + TEMRA are terminally differentiated effector memory lymphocytes. Terminally differentiated helper T lymphocytes have been implicated in protective immunity against pathogens20. Significantly higher values of absolute counts of terminally differentiated helper T lymphocytes compared to the healthy controls were found in our work.
CD3 abs represent the absolute value of total T cells. Their increased value is observed in both protective inflammatory response fighting infectious or cancerous diseases and harmful inflammation indicating immunopathological autoimmune diseases. Grazzi et al.14 demonstrated that CD3, CD4 and CD19 (expressed as absolute numbers) were significantly higher in patients with chronic migraine those with episodic migraine. In this work, the significant increase in absolute numbers of both CD3 T cells and CD19 B cells was observed in migraine patients compared to results for healthy controls.
CD8 abs represents the absolute value of cytotoxic/suppressor T cells. Resting naïve CD8 T cells have an astounding capacity to react to intracellular pathogens such as viruses via massive expansion and terminal differentiation into cytotoxic effector cells21. CD8 T cells are involved in the immunopathogenesis of multiple sclerosis22. Cseh et al.13 examined lymphocyte levels in paediatric migraine patients and found that the CD8 prevalence was lower in patients than in controls13. Covelli et al.23 did not observe a change in this peripheral blood parameter in migraine patients23. The present study reported an elevation in CD8 abs in migraine patients.
The mechanisms underlying migraine onset are largely unknown. The role of the immune system in migraine onset is a matter of debate. A series of clinical investigators have reported alterations in immune function in migraine patients. However, the results of this work are inconsistent with the findings of other investigators and showed that there were alterations in the immune system function in patients who were treated for EM. Therefore, the next step of this work was to determine whether the changes found in the peripheral blood parameters were related to migraine severity according to the standardised MIDAS and HIT-6 tests in EM patients.
Among the lymphocyte parameters, CD4 + TEM and CD8 + TEMRA were statistically significantly associated with HIT-6. Effector T cells play an important role in immunity against pathogenic agents24. Previous studies have noted that subjects with type 2 diabetes mellitus had elevated percentages of effector memory T cells25. CD8 + TEMRA exhibit potent effector functions, including the ability to secrete proinflammatory cytokines and cytotoxic molecules26.
CD4 + TEM seems to be a significant parameter. The key study by Sallusto and Lanzavecchia27 revealed that CD4 + TEM generated more IFNγ27. In addition, IFNγ-stimulated dendritic cell-derived exosomes decrease oxidative stress and enhance recovery from a demyelinating damage in slice cultures28. Research also indicates that there is an association between myelin integrity and susceptibility to expanding depression29. Cortical expanding depression might start intracranial neurogenic inflammation, consequently resulting in migraine headaches via subsequent activation of trigeminal afferents30,31,32. Pusic et al.33 demonstrated that interferon gamma-stimulated dendritic cell exosomes (IFNγ-DC-Exos) might decrease susceptibility to expanding depression in vivo and in vitro, which means that IFNγ-DC-Exos might be a possible therapeutic for migraine33.
In this study, the most interesting parameter appeared to be already aforementioned CD4 + TEM. The HIT-6 migraine outcome was (much) better explained by CD4 + TEM (33%) than by age (15%). On the other hand, age was better described (13% variability explained) by the outcome MIDAS 0–100 than by the best lymphocyte parameter, CD4 + TEM (8%). The combination of CD4 + TEM and age explained 17% of the variability for MIDAS and 37% of the variability for the HIT-6. The results of this work showed that lower CD4 + TEM values mean that there is an increased probability of a MIDAS score ≥ 21. The interval estimate of probability was inaccurate due to the small number of patients in the groups. For this reason, this estimate should be verified in a larger, independent sample.
In relation to the HIT-6, CD4 + TEM appear to be an important parameter. Patients with an CD4 + TEM value below 15 had a high probability (90%) of having a HIT-6 value above 60. This is an estimate of the probability. The interval estimate for this probability was 75–95%. In other words, this probability predicts that 9 out of 10 patients with CD4 + TEM < 15 will have a HIT-6 higher than 60. Results of this study show that CD4 + TEM could be a biomarker that determines the severity of migraine.
Biomarkers can be characterized as physical signs or laboratory measurements connected with a biological process possessing presumed indicative and predicative utility34. One can expect that biomarkers associated with the putative pathophysiology of migraine might possess a corresponding value as diagnostic or therapeutic indicators by detecting patients at an increased risk for migraine expansion or by predicting the efficacy of migraine interventions. At present, biomarkers connected with the elevated risk for migraine and biomarkers connected with clinical reactions to treatment are known35. Although several circulating biomarkers have been proposed as diagnostic or therapeutic tools in migraine, their identification is still a challenge for the scientific community, reflecting, at least in part, disease complexity and clinical diagnostic limitations.
The biomarkers associated with clinical responses to treatment are interesting for clinical practice. At present, CGRP represents the most promising candidate as a diagnostic and/or therapeutic biomarker as its plasma levels are elevated during a migraine attack and decrease during successful treatment36. Cernuda-Morollón et al. have shown that onabotulinumtoxinA significantly decreases CGRP levels in peripheral blood samples between attacks and measured 1 month after injection, thus confirming interictal, peripheral levels of CGRP as a potential chronic migraine biomarker37. Other treatment response biomarkers may be neurokinin A and serotonin transporter. Neurokinin A levels measured before drug administration were significantly higher in responders vs nonresponders to rizatriptan38. STin 2.12/12 genotype was identified as a significant factor increasing the odds for an inconsistent response to triptans39. CD4 + TEM may be a new biomarker, one that assesses the severity of migraine in patients without prophylactic treatment. As new prophylactic anti-migraine treatments are now available (anti-CGRP monoclonal antibodies), it is important to identify a patient early with a more severe course of migraine so that therapy is rationally selected for each patient in an effort to increase their quality of life as much as possible.
Peripheral blood immune parameters were evaluated in this study. We are aware that absolute lymphocyte counts are highly variable and may considerably change even during a day. For this reason, samples were taken approximately at the same time. We are also aware that migraineurs often suffer from comorbid atopic disorders and are exposed to chronic stress due to frequent headaches, and this stress is the cause of prolonged release of endogenous corticosteroids to cope with the potentially harmful consequences of this stress. However, the price of this regulatory effort is dampening protective capacities of the immune system. To eliminate the factors that could affect the immune system, only patients without known comorbidities and for whom migraine was their only disease were selected for this analysis.
In spite of that we have chosen 5% statistical significance level we interpret the non-significant results with p value < 0.10 because we studied many lymphocyte parameters in a relatively small sample of EM patients. The use of a high number of variables implies that by chance some of the measurements will display statistical significance. This is the reason for using a statistical test with correction for multiple comparisons. The statistical power of these tests is lower because they are much more restrictive, and this is the reason why we did not get statistical significance (p < 0.05) in the variables measured. We focused on describing our data set in order to identify a few potential biomarkers from the set of many parameters because there are no studies investigating these relationships. Our findings should be validated by another study.
Conclusions
The results of this study show that EM patients show changes in immune system parameters as determined by peripheral blood collection. CD4 + TEM appears to be an important parameter. Lower CD4 + TEM values mean that there is an increased probability of a severe disability. The CD4 + TEM may represent a potential biomarker that determines the severity of migraine. However, these results should be validated in a larger cohort of EM patients.
Abbreviations
- EM:
-
Episodic migraine
- IFNγ:
-
Interferon gamma
- CGRP:
-
Calcitonin gene-related peptide
- CD4 + TEM :
-
Effector memory helper T lymphocytes
- CD8 + TEMRA :
-
Terminally differentiated cytotoxic T lymphocytes
- CD4 + TEMRA :
-
Terminally differentiated helper T lymphocytes
References
Goadsby, P. J. et al. Pathophysiology of migraine: A disorder of sensory processing. Physiol. Rev. 97, 553–622 (2017).
Steiner, T. et al. The impact of headache in Europe: Principal results of the Eurolight project. J. Headache Pain. 15, 31 (2014).
Sokolovic, E., Riederer, F., Szucs, T., Agosti, R. & Sándor, P. S. Self-reported headache among the employees of a Swiss university hospital: Prevalence, disability, current treatment, and economic impact. J. Headache Pain. 14, 29 (2013).
Hu, X. H., Markson, L. E., Lipton, R. B., Stewart, W. F. & Berger, M. L. Burden of migraine in the United States: Disability and economic costs. Arch Intern. Med. 159, 813–818 (1999).
Pietrobon, D. & Striessnig, J. Neurobiology of migraine. Nat. Rev. Neurosci 4(5), 386–398 (2003).
Kemper, R. H., Meijler, W. J., Korf, J. & Horst, G. J. Migraine and function of the immune system: A meta-analysis of clinical literature published between 1966 and 1999. Cephalalgia 21, 549–557 (2001).
Moskowitz, M. A., Reinhard, J. F., Romero, J., Melamed, E. & Pettibone, D. J. Neurotransmitters and the fifth cranial nerve: is there a relation to the headache phase of migraine?. Lancet 2, 883–885 (1979).
Buzzi, M. G. & Moskowitz, M. A. The antimigraine drug, sumatriptan (GR43175), selectively blocks neurogenic plasma extravasation from blood vessels in dura mater. Br. J. Pharmacol. 99(1), 202–206 (1990).
Connor, H. E. et al. Naratriptan: biological profile in animal models relevant to migraine. Cephalalgia 17(3), 145–152 (1997).
Goadsby, P. J., Edvinsson, L. & Ekman, R. Vasoactive peptide release in the extracerebral circulation of humans during migraine headache. Ann. Neurol. 28(2), 183–187 (1990).
Fidan, I., Yüksel, S., Ymir, T., Irkeç, C. & Aksakal, F. N. The importance of cytokines, chemokines and nitric oxide in pathophysiology of migraine. J. Neuroimmunol. 171(1–2), 184–188 (2006).
Arumugam, M. & Parthasarathy, V. Reduction of CD4(+)CD25(+) regulatory T-cells in migraine: Is migraine an autoimmune disorder?. J. Neuroimmunol. 290, 54–59 (2016).
Cseh, A. et al. Lymphocyte subsets in pediatric migraine. Neurol. Sci. 34, 1151–1155 (2013).
Grazzi, L. et al. Evaluation of immune parameters in chronic migraine with medication overuse. Neurol. Sci. 35, 171–173 (2014).
Nurkhametova, D. et al. Purinergic profiling of regulatory T-cells in patients with episodic migraine. Front. Cell Neurosci. 12, 326 (2018).
Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders, 3rd edition. Cephalalgia. 33:629–808 (2013).
Stewart, W. F., Lipton, R. B., Dowson, A. J. & Sawyer, J. Development and testing of the migraine disability assessment (MIDAS) questionnaire to assess headache-related disability. Neurology. 56, S20–S28 (2001).
Bayliss, M. S. et al. A study of the feasibility of Internet administration of a computerized health survey: The headache impact test (HIT). Qual. Life Res. 12, 953–961 (2003).
Kosinski, M. et al. A six-item short-form survey for measuring headache impact: The HIT-6. Qual. Life Res. 12, 963–974 (2003).
Tian, Y. et al. Unique phenotypes and clonal expansions of human CD4 effector memory T cells re-expressing CD45RA. Nat. Commun. 8, 1473 (2017).
Zhang, N. & Bevan, M. J. CD8(+) T cells: Foot soldiers of the immune system. Immunity 35, 161–168 (2011).
Salou, M., Nicol, B., Garcia, A. & Laplaud, D.-A. Involvement of CD8(+) T cells in multiple sclerosis. Front. Immunol. 6, 604 (2015).
Covelli, V., Maffione, A. B., Munno, I. & Jirillo, E. Alterations of nonspecific immunity in patients with common migraine. J. Clin. Lab. Anal. 4, 9–15 (1990).
Rosenblum, M. D., Way, S. S. & Abbas, A. K. Regulatory T cell memory. Nat. Rev. Immunol. 16, 90–101 (2016).
Rattik, S. et al. Elevated circulating effector memory T cells but similar levels of regulatory T cells in patients with type 2 diabetes mellitus and cardiovascular disease. Diab. Vasc. Dis. Res. 16, 270–280 (2019).
Yap, M. et al. Expansion of highly differentiated cytotoxic terminally differentiated effector memory CD8+ T cells in a subset of clinically stable kidney transplant recipients: A potential marker for late graft dysfunction. J. Am. Soc. Nephrol. 25, 1856–1868 (2014).
Sallusto, F., Lenig, D., Förster, R., Lipp, M. & Lanzavecchia, A. Two subsets of memory T lymphocytes with distinct homing potentials and effector functions. Nature 401(6754), 708–712 (1999).
Pusic, A. D., Pusic, K. M., Clayton, B. L. & Kraig, R. P. IFNγ-stimulated dendritic cell exosomes as a potential therapeutic for remyelination. J. Neuroimmunol. 266(1–2), 12–23 (2014).
Pusic, A. D., Mitchell, H. M., Kunkler, P. E., Klauer, N. & Kraig, R. P. Spreading depression transiently disrupts myelin via interferon-gamma signaling. Exp. Neurol. 264, 43–54 (2015).
Leao, A. A. P. Spreading depression of activity in the cerebral cortex. J. Neurophysiol. 7, 359–390 (1944).
Pietrobon, D. & Moskowitz, M. A. Pathophysiology of migraine. Annu. Rev. Physiol. 75, 365–391 (2013).
Cui, Y., Kataoka, Y. & Watanabe, Y. Role of cortical spreading depression in the pathophysiology of migraine. Neurosci. Bull. 30(5), 812–822 (2014).
Pusic, K. M., Won, L., Kraig, R. P. & Pusic, A. D. IFNγ-stimulated dendritic cell exosomes for treatment of migraine modeled using spreading depression. Front. Neurosci. 13, 942 (2019).
Biomarkers Definitions Working Group. Biomarkers and surrogate endpoints: preferred definitions and conceptual framework. Clin. Pharmacol. Ther. 69(3), 89–95 (2001).
Durham, P. & Papapetropoulos, S. Biomarkers associated with migraine and their potential role in migraine management. Headache. 53(8), 1262–1277 (2013).
Ferroni, P. et al. Circulating biomarkers in migraine: New opportunities for precision medicine. Curr. Med. Chem. 26(34), 6191–6206 (2019).
Cernuda-Morollón, E. et al. OnabotulinumtoxinA decreases interictal CGRP plasma levels in patients with chronic migraine. Pain 156, 820–824 (2015).
Sarchielli, P. et al. Clinical-biochemical correlates of migraine attacks in rizatriptan responders and non-responders. Cephalalgia 26(3), 257–265 (2006).
Terrazzino, S. et al. The serotonin transporter gene polymorphism STin2 VNTR confers an increased risk of inconsistent response to triptans in migraine patients. Eur. J. Pharmacol. 641(2–3), 82–87 (2010).
Acknowledgements
This study was partially supported by MH CZ—DRO (UHHK, 00179906), by the grant projects of the Ministry of Health of the Czech Republic (FN HK 00179906) and by Charles University in Prague, Czech Republic (PROGRES Q40/15).
Author information
Authors and Affiliations
Contributions
Z.P. conceived the idea. Z.P., J.K., K.K. and M.V. designed the research and wrote the paper. O.S., L.S., B.K. and J.M. performed the research and analyzed the data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflicts of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pavelek, Z., Souček, O., Krejsek, J. et al. The role of the immune system and the biomarker CD3 + CD4 + CD45RA−CD62L− in the pathophysiology of migraine. Sci Rep 10, 12277 (2020). https://doi.org/10.1038/s41598-020-69285-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-69285-4
This article is cited by
-
Glia Signaling and Brain Microenvironment in Migraine
Molecular Neurobiology (2023)
-
Metabolic profile changes in serum of migraine patients detected using 1H-NMR spectroscopy
The Journal of Headache and Pain (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.