Abstract
While mRNA vaccines against SARS-CoV-2 are exceedingly effective in preventing symptomatic infection, their immune response features remain to be clarified. In the present prospective study, 225 healthy individuals in Japan, who received two BNT162b2 doses, were enrolled. Correlates of BNT162b2-elicited SARS-CoV-2-neutralizing activity (50% neutralization titer: NT50; assessed using infectious virions) with various determinants were examined and the potency of sera against variants of concerns was determined. Significant rise in NT50s was seen in sera on day 28 post-1st dose. A moderate inverse correlation was seen between NT50s and ages, but no correlation seen between NT50s and adverse effects. NT50s and SARS-CoV-2-S1-binding-IgG levels on day 28 post-1st dose and pain scores following the 2nd dose were greater in women than in men. The average half-life of NT50s was ~ 68 days, and 23.6% (49 out of 208 individuals) failed to show detectable neutralizing activity on day 150. While sera from elite-responders (NT50s > 1,500: the top 4% among the participants) potently to moderately blocked all variants of concerns examined, some sera with low NT50s failed to block the B.1.351-beta strain. Since BNT162b2-elicited immunity against SARS-CoV-2 is short, an additional vaccine or other protective measures are needed.
Similar content being viewed by others
Introduction
Since the emergence of coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in Wuhan, China, the disease quickly spread to the world. As of June 29, 2021, more than 180 million SARS-CoV-2-infected individuals and almost 4 million death cases have been reported in over 200 countries1,2,3,4. Since the beginning of the pandemic, researchers and pharmaceutical companies around the world have been working on developing vaccines5. Currently, more than 10 vaccines have been authorized for public use worldwide. The development of vaccines against SARS-CoV-2 was achieved time- and efficacy-wise beyond our expectations within a single calendar year from the availability of the viral sequence to the initiation of immunization of many people in several countries6,7.
Among various vaccines, two RNA vaccines (BNT162b2 and mRNA-1273/TAK-919) have been shown to be as much as 94–95% effective and safe8,9,10,11. In addition, inactivated vaccines or viral vector vaccines have also been available in certain countries and areas5,7,10,11. For example, the adenovirus-vector-based vaccine (ChAdOx1 nCoV-19/AZD1222) has reportedly achieved 62% efficacy in initial trials12. The phase 3 reports of another adenovirus-based vaccine (Ad26.COV2.S) has indicated 85% efficacy against severe disease or death13,14.
However, the recent emergence of various SARS-CoV-2 variants with mutations in the spike region is raising concerns about the efficacy of vaccines. The D614G and B.1.1.7 (alpha/N501Y) variants appear to be without antigenic escape15,16. However, the B.1.351 (beta) variant is reportedly represents a neutralization escape variant to convalescent sera17. The phase 3 results of NVX-CoV2373 (a nanoparticle, protein-based vaccine) from the United Kingdom indicated 89% efficacy with over 50% of cases attributable to the more transmissible alpha variant18. However, a phase 2b trial in South Africa showed 60% efficacy, in which approximately 90% of the endpoints occurred in subjects infected with the beta variant19,20, suggesting that the beta variant is less susceptible to antibodies elicited with the original Wuhan strain antigens, which is in the composition of all the vaccines currently being evaluated7. Another recent concern is the emergence of a B.1.617.2 (delta) variant, which was first detected in India, is now spreading around the world. This variant of concern (VOC) seems to have less susceptibility to vaccine-elicited protection and increased transmissibility beyond alpha strains21.
In the present study, we examined neutralizing activity and S1-binding-antibody response in BNT162b2-vaccinated health care workers (n = 225) in Japan. We also investigated the correlation among neutralizing activity levels, S1-binding-IgG and -IgM levels, genders, and adverse events. Decline of BNT162b2-elicited immune response and activity of the elite and moderate responders against VOCs were also investigated.
Results
Demographic characteristics and immune response in the participants
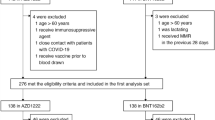
We obtained blood samples for antibody testing from a total of 225, 220, 211, 210 and 208 vaccine recipients on days 7, 28, 60, 90 and 150 post-1st dose, respectively (Table 1). Demographic characteristics of the participants are shown in Table 1. As of the time of enrollment, the average age of the participants was 41.8 years (range 21–72 years), and 69.8% of the participants were female serving as a physician, nurse, paramedical staff, or administrative staff. None of the participants was in the immunodeficient state or was receiving immunosuppressants or steroids.
We first determined the neutralizing activity against SARS-CoV-2 in sera samples taken on day 7 post-1st dose from 225 participants; however, none of the samples showed detectable neutralization activity (NT50 < 20). We then determined the neutralizing activity in samples taken on day 28 post-1st dose from 220 vaccinated participants. As shown in Fig. 1A, NT50 levels were substantially diverse among the participants: the geometric mean of NT50 values was 375.2 (range 25.6–2680.0). Very low or no correlation of the NT50 values with ages was identified (Fig. 1A: Spearman’s ρ = − 0.22; 95% CI − 0.34 to − 0.09, p = 0.001). We also examined the levels of S1-binding-IgG and -IgM levels using the HISCL system that enables quantitative and highly sensitive determination of S1-binding-IgG and -IgM levels22. The geometric mean of S1-binding-IgG values was 527.0 (range 44.6–3212.2), while that of S1-binding-IgM was 85.1 (range 10.3–1406.5). There was a high positive correlation of the NT50 values with S1-binding-IgG levels (Spearman’s ρ = 0.71; 95% CI 0.63–0.77, p < 0.001) as examined on day 28 post-1st dose, while there was a moderate positive correlation of the NT50 values with S1-binding-IgM levels (Spearman’s ρ = 0.43; 95% CI 0.31–0.53, p < 0.001), suggesting that the neutralizing activity largely resides in IgG fraction of the sera of vaccinated participants around on day 28 post-1st dose (Fig. 1B, C). However, when examined on day 60 post-1st dose, the correlations of NT50 levels with both IgG and IgM levels became moderate or low (Spearman’s ρ = 0.56 [p < 0.001] and 0.32 [p < 0.001], respectively) (Supplementary Fig. 1).
Correlations of neutralizing titers with ages and S1-binding-IgG and -IgM levels. (A) Correlation between neutralizing titers (NT50s) on day 28 post-1st dose and the ages of the participants (on day 28 post-1st dose). The age range of the study participants was 21–72 (average 41.8 y.o.). A correlation is negligible between NT50 values and ages (Spearman’s ρ = − 0.22: 95% CI − 0.34 to − 0.09, p = 0.001). The geometric mean NT50 of the values from all participants (n = 225) was 375.2 (range 25.6–2680), greater by a factor of 2.3 than the geometric mean NT50 from 65 COVID-19-convalescent patients (geometric mean = 163.0; range 20.0–1470) shown as references on the far right (human COVID-19-convalescent serum: HCS). (B) A high correlation is identified (Spearman’s ρ = 0.71; 95% CI 0.63–0.77, p < 0.001) between NT50 values and S1-binding-IgG levels in samples obtained on day 28 post-1st dose. (C) Moderate correlation is seen between neutralizing titers and S1-binding-IgM levels (Spearman’s ρ = 0.43; 95% CI 0.31–0.53, p < 0.001). One participant, who had been infected with SARS-CoV-2 with PCR-positivity documented, is indicated as a solid-red solitary circle. This participant was excluded from all analyses at later timepoints.
The occurrence of adverse effects has no association with the BNT162b2-elicited neutralizing activity levels
Commonly observed adverse events reported following BNT162b2 vaccination include injection-site pain, systemic fever, headache, and fatigue11. In the present study, the events were observed largely more often following the 2nd dose (Supplementary Fig. 2) as previously reported by Polack et al.11. Pains in the inject-site were reported by 67.6 and 61.6% of the participants and systemic fever (≥ 37.1℃) was reported by 3.6 and 46.4% of the participants following the 1st and 2nd doses, respectively. Fever was measured when each participant felt feverish at any time points over weeks following the 1st and 2nd vaccinations. Since the severity of pains can be more easily quantified than other adverse effects such as headache and fatigue, the possible correlate of the NT50 values with the severity of pains rated with the short form McGill pain questionnaire23 was first examined. No correlation was seen between the NT50 values and the pain grades assessed following the 2nd dose (Spearman’s ρ = 0.14; 95% CI 0.00–0.26, p = 0.043). The correlation was also negligible between the NT50 values and the incidence of systemic fever (Spearman’s ρ = 0.26; 95% CI 0.13–0.38, p < 0.001) (Fig. 2A, B).
Correlations of neutralizing titers with injection-site pain scores and systemic fever grades. (A) No correlation was seen between NT50 values and injection-site pain (Spearman’s ρ = 0.14; 95% CI 0.00–0.26, p = 0.043). The injection-site pain following the 2nd BNT162b2 dose was scored by using the short-form McGill Pain Questionnaire23. (B) Correlation was negligible between NT50 values and systemic fever grades (Spearman’s ρ = 0.26; 95% CI 0.13–0.38, p < 0.001). A solid-red circle indicates a person with previous SARS-CoV-2 infection documented.
The average half-life of neutralizing activity in the vaccinees is approximately 67.8 days and the average time-length for their sera to lose the detectable activity is 198.3 days
Considering that recent multiple clinical studies strongly suggest that the presence of high-level neutralizing antibodies is generally sufficient to confer protection against SARS-CoV-2 infection and that the protection against COVID-19 development is largely explained by robust SARS-CoV-2-neutralizing antibody response9,10,11. If so, the once-established neutralizing antibody levels will decrease in time. We thus examined at what rate the levels of NT50 and S1-bindng-IgG and -IgM levels change by determining those levels from the data on day 28 (n = 220), day 60 (n = 211), and day 90 (n = 210) post-1st dose (Fig. 3A–C). The reduction of all NT50, IgG, and IgM levels from day 28 through day 90 post-1st dose was found to occur virtually linearly. By calculation, the predicted average half-life of all the NT50 values turned out to be 67.8 days and those of S1-binding-IgG and IgM levels were 53.5 days and 43.6 days, respectively (Fig. 3A–C). The half-life of the NT50 values and that of S1-binding-IgG were reasonably comparable, corroborating that the neutralizing activity largely resides in the S1-binding IgG fraction. As seen, chronologically linear nature of the reduction was identified between day 28 and 90 for both neutralization and antibody titers. However, the rate of decline was found to be more modest and slower between the data on day 90 and day 150 post-1st dose (especially in antibody titers) (Fig. 3A–C). We also asked whether the chronological decay rate of neutralization titers and S1-binding-IgG and -IgM differs among three age subgroups: (1) 20–39 yo, (2) 40–59 yo, and (3) 60 s and beyond. No significant difference was identified among the three age subgroups in the levels of neutralizing titers, IgG, or IgM levels (p = 0.60, 0.16, and 0.11, respectively: Supplementary Fig. 3A–C). The present data suggest that vaccinated individuals with good neutralization response would lose BNT162b2’s protection in 6–7 months without regard to age subgroups unless such people achieve robust immune boost response upon the future exposure to SARS-CoV-2. Otherwise, they should be protected by another booster vaccine dose or by other protective means.
Kinetics of neutralizing activity and S1-binding-IgG and -IgM levels. Time-course analyses of neutralizing activity for 90 days were conducted. The 1st vaccine was administered on day 0, and the 2nd vaccine on day 21. Blood samples from vaccinated individuals were obtained on days 7, 28, 60, 90 and 150 post 1st dose as illustrated in Table 1. (A) Neutralizing activity is shown as NT50 (50% neutralizing titer). The NT50 value of 20 is the detection limit and values determined to be less than 20 were treated as 20. (B, C) Kinetics of S1-binding-IgG and -IgM levels are shown. The average values of each data point are shown in black solid circles, which are connected with solid black lines. One participant, who had been infected with SARS-CoV-2 with PCR-positivity documented, is indicated as a solid-red solitary circle in (B) and (C). This participant was excluded from all analyses at later timepoints.
Neutralization titers, S1-binding-IgG levels, and pain scores in the injection site were greater in women than in men
We then asked whether there were differences between genders in neutralization activity levels, S1-bindng-IgG and -IgM levels, injection-site pain scores, and systemic fever grades. Statistically significant differences were identified in the levels of neutralization determined on 60 and 90 days post-1st dose (p = 0.002 and 0.002, respectively), S1-binding-IgG levels determined on 28, 60, and 90 days (p < 0.001, p = 0.001, and p = < 0.001, respectively) post-1st-dose, and S1-binding-IgM levels on 60 and 90 days post-1st dose (p = 0.025 and 0.044, respectively) (Supplementary Fig. 4A–C). The injection-site pain score was greater in women (p < 0.001) (Supplementary Fig. 4D). However, there was no difference in systemic fever grades between genders (Supplementary Fig. 4E).
Some sera retain potent activity against various VOCs, but others showed substantially less potent or undetectable activity
We finally asked whether the neutralizing antibodies elicited by BNT162b2 vaccination blocked the infectivity and replication of various variants of concerns (VOCs). To this end, we employed sera samples from 6 elite responders (NT50 values > 1,500: the top 4% of all participants’ NT50 values as determined on 28 days post-1st dose) and sera samples from twelve randomly-selected moderate responders (NT50 values = 200 ~ 1,500) and tested them for their inhibition of the infectivity and cytopathic effect of each variant in the VeroE6TMPRSS2 cell-based assay24. As shown in Fig. 4, sera from the elite responders (n = 6) showed potent inhibition against SARS-CoV-205-2 N (Wuhan strain, PANGO lineage B), while they showed less activity against SARS-CoV-2QHN001 and SARS-CoV-2QK002 (alpha), SARS-CoV-25356 (kappa), SARS-CoV-21734 (delta), and SARS-CoV-2TY8-612 (beta). Sera from moderate responders (n = 12) exerted less activity against the Wuhan strain than those from the elite responders. Some sera from the moderate responders also showed substantially low potency to all the VOCs tested. Notably, three sera from the moderate responders showed only marginal activity against SARS-CoV-2TY8-612 (beta). Two of those three samples had no detectable inhibitory activity against SARS-CoV-2TY8-612 (Fig. 4).
Blockade of the infectivity and replication of SARS-CoV-2 variants by vaccinees’ sera on day 28 post-1st dose. The activity of vaccinees’ sera to block the infectivity and replication of 5 SARS-CoV-2 variants (alpha variants: SARS-CoV-2QHN001 and SARS-CoV-2QK002; a beta strain: SARS-CoV-2TY8-612; a delta strain: SARS-CoV-21734; and a kappa strain: SARS-CoV-25356) was evaluated. A Wuhan strain SARS-CoV-205-2 N41 was employed as a reference SARS-CoV-2. Six sera were from elite responders (NT50 > 1,500) and 12 sera were from randomly-selected moderate responders (NT50 = 200 ~ 1,500). The NT50 titers of each sera against 6 SARS-CoV-2 strains are shown in red circles (for 6 elite responders) and in black circles (for 12 moderate responders). D043 is a sera from a COVID-19-convalescent patient43 and served as an internal control in the assays. P values for the difference between the averages of elite and moderate responders in each variant: < 0.001 (05-2 N), 0.006 (QHN001), 0.004 (QK002), 0.035 (5356), 0.119 (1734), and 0.371(TY8).
Discussion
In this prospective observational study, 225 healthy individuals [physicians (n = 36), nurses (n = 125), and other healthcare professionals (n = 64)], who received two doses of 30 µg BNT162b2 (Pfizer–BioNTech) vaccine in February 2021, were enrolled, and the correlates of neutralization activity represented by 50% neutralization titers (NT50) determined by employing the target living VeroE6TMPRSS2 cells and live SARS-CoV-2 with ages, adverse effects (AEs) that occur often such as injection-site pain and systemic fever were examined. The kinetics of NT50 values and S1-binding antibody levels were also examined. There was a significant rise in the NT50 values as determined on day 28 post-1st dose (a week after post 2nd dose) compared to those on day 7 post-1st dose. Correlation was negligible between NT50 values and ages or systemic fever grades. In this regard, most adverse effects that occur within 1–3 days following vaccine doses are thought to be caused by the release of certain pyrogenic and inflammatory cytokines (e.g., interleukin-1, interleukin-6, and tumor-necrosis factor) from antigen-presenting cells (APCs) such as macrophages and dendritic cells when they ingest and process the exogenous antigens (i.e., SARS-CoV-2 spike antigens) and transmit the antigenic information to relevant immune cells. Such early-phase defense events include response to antigenic determinants irrelevant to neutralizing activity but those eliciting S1-binding antibodies. The release of the pyrogenic and inflammatory cytokines mostly subsides within days following the vaccine dose. The released cytokines activate the antigen-specific-antibody-producing B-cells, which respond to the processed antigenic determinants presented by the APCs and start to produce antigen-specific antibodies such as neutralizing antibodies as well as non-neutralizing but S1-binding antibodies. Such antigen-specifically-activated and antibody-producing B-cells continue to produce antibodies. In the case of BNT162b2 vaccination, it appears that it takes 10–12 days from the 1st vaccine dose for the vaccinated individuals to achieve the amounts of neutralizing antibodies that are enough to block the infection of substantial numbers of the virally-targeted cells and to inhibit further spread of the infection10,11. It is thought that the release of pyrogenic and inflammatory cytokines and the build-up of the protective antibody levels are different events, occurring chronologically ~ 10–12 days apart. These two different events appear to have resulted in the absence of significant correlates between NT50 levels and AEs examined in the present study.
In the present study, the NT50 values had a substantial correlation with S1-binding-IgG levels but had only moderate correlation with S1-binding IgM levels, suggesting that the major neutralizing activity resides within the S1-binding IgG fraction. Interestingly, the approximate half-life of NT50 values (69.7 days) and that of S1-binding-IgG levels (54.7 days) were reasonably close to each other, corroborating the assumption of the presence of the major fraction of neutralizing antibodies within IgG fraction. In human body, IgG has concentration-dependent half-life of approximately 21 days and IgM around 5–6 days25. By contrast, the half-lifes of NT50, S1-bindng-IgG, and -IgM levels determined in the present study were much longer with 39.0–54.7 days. This discrepancy is perhaps attributed to the persistence of continuously-antibody-producing B cells over weeks or months in the body of the participants following the vaccination26,27, thereby the half-lifes of neutralizing activity and S1-binding-IgG and -IgM levels have been extended as compared to the physiological half-lifes of IgG and IgM. In terms of the persistence for the efficacy of vaccine, Doria-Rose et al. reported that anti-SARS-CoV-2 antibodies persist through 6 months after the second dose of mRNA-1273 administration28. However, the study was of a relatively small scale (n = 33), and more definite data are needed for the understanding the nature of vaccine efficacy. In addition, Tartof et al. have also demonstrated that an examination of individuals receiving BNT-162b vaccine showed a decrease of protection, but the protection remained consistent up to 6 months29. Planas et al. have also showed that the sera from individuals had reduced at 16 weeks after receiving ChAdOx1 nCoV-19/AZD1222 vaccine, but such individuals with the reduced neutralizing activity had been well-protected from infection30. In our present study, we demonstrated that both neutralization and antibody titers decrease virtually linearly at the initial phase (up to ~ 3 months post-1st dose) but that reduction rate becomes rather slower when examined in ~ 5 months post-1st dose (Fig. 3A–C), which is in line with the data shown by others29,30. In addition, we examined N-IgG antibody levels (indicator for viral infection) in all participants at each time point (on Days 7, 28, 60, 90, and 150 post-1st dose) and found that none of the participants were positive for N-IgG throughout the test period. Moreover, none of the participants reported that they had no symptom suggesting new infection by SARS-CoV-2. Since the number of the participants is limited to 210 by day 150 post-1st dose, it is not clear as to whether the absence of infected participants over 150 days post-1st dose is due to the protective effect of the reduced neutralization and antibody levels.
In the present limited study enrolling only 225 participants, it is not possible to precisely associate the immune response seen with clinical outcomes such as development of severe COVID-19 and death. In this regard, Walsh et al. examined the immunogenicity of the Pfizer’s BNT162b2 vaccine and Polack et al. examined the outcomes in 21,728 vaccinated individuals and 21,720 placebo-receiving individuals8,11. In the two reports together, the BNT162b2 vaccine very effectively elicited good immune response; however, 5% of the participants in the study performed by Polack et al. contracted SARS-CoV-2 infection. In our present study, ~ 5% of the participants apparently failed to build reasonable neutralizing antibody levels (< × 110, on day 28; Fig. 3A). These probable low-responders might be susceptible to SARS-CoV-2 infection, might contract SARS-CoV-2 infection, and might develop severe COVID-19 and end up in death. However, as of this writing, reportedly none of the participants have contracted the virus or had COVID-19 symptom.
For the immunity against SARS-CoV-2, it is highly likely that the mucosal immunity also contributes the body’s defence against COVID-19. We have not examined the level of antibodies (especially IgA class) in mucosa after vaccinations in the present study, but that should be elucidated in future. It is also likely that the role and strength of mucosal immunity, antibody-dependent cellular cytotoxicity (ADCC), antibody-dependent cellular phagocytosis (ADCP), and such in the control of SARS-CoV-2 depends on the class of vaccines (mRNA-based vaccines, vector-based vaccines, or subunit vaccines) administered. The role of cellular immunity (mainly driven by cytotoxic T-cells and NK cells) after vaccination has also been reported upon anti-COVID-19 vaccination31. However, detailed dynamics of the potency and persistence of cellular immunity against SARS-CoV-2 still remain to be elucidated.
There is a growing body of evidence that COVID-19 results in more severe symptoms and greater mortality among men than among women32,33. A cohort study of 17 million adults in England has revealed a strong association between male sex and the risk of death from COVID-19 (hazard ratio 1.59, 95% confidence interval 1.53–1.65)34. In the present data set, significantly greater levels (p < 0.001) of NT50 (Days 60 and 90 post-1st dose), S1-binding-IgG (Days 28, 60 and 90), and -IgM (Days 60 and 90) were documented in women than in men when examined on 28, 60, and 90 days post-1st dose, while there was no difference in either of NT50, S1-binding-IgG or -IgM levels on day 7 post-1st dose (Supplementary Fig. 4A–C). These results apparently relate to the findings by others reporting that women, in general, have more robust ability to control infectious pathogens (i.e., SARS-CoV-2) than men34,35. Indeed, there is increasing evidence indicating strong correlation between SARS-CoV-2-neuralizing antibody titers and clinical efficacy, suggesting that a neutralizing antibody response provides the primary contribution to protection against COVID-1936 and that the presence of high levels of neutralizing antibody is largely sufficient for protection against SARS-CoV-2 infection and clinical onset upon exposure to the virus37,38. In fact, Imai et al. have reported that the administration of convalescent plasma from previously-SARS-CoV-2-infected hamsters completely protected newly SARS-CoV-2-exposed hamsters from contracting viral pneumonitis39. Thus, the greater neutralizing activity in women than in men observed in the present study can contribute at least in part to the gender differences in COVID-19 disease outcomes.
We also examined how the BNT162b2-elicited neutralizing antibodies blocked the infectivity and cytopathic effect of five different variants of concerns in the cell-based assays using various infectious variants (one Wuhan strain, two alpha strains, one strain each of beta, delta and kappa strains). Six selected sera from elite responders showed quite potent activity to the alpha, kappa, and delta variants, while they exerted relatively moderate activity against the beta strain (Fig. 4). On the other hand, one of the randomly-selected 12 sera from moderate responders showed a marginal activity (NT50 value of 40) and two of them failed to show detectable activity (NT50 values < 20) against the beta strain (Fig. 4). These data suggest that BNT162b2-receiving vaccinees who develop high magnitudes of neutralizing antibody should probably be well protected against the infection by most variants; however, those who develop only low levels of neutralizing antibody may be vulnerable to the infection by certain variants such as beta strains. If so, to such low-responders to BNT162b2 even after the 2nd dose, an additional 3rd dose may be needed. If the 3rd dose of the same vaccine fails to elicit good levels of neutralizing antibodies, new types of vaccines with different platform have to be stratified.
Methods
Participants and sera specimens
Sera were collected from 225 vaccinated (BNT-162b, 30 μg/dose) health care workers at JCHO Kumamoto General Hospital (Kumamoto, Japan). All the 225 participants were of Japanese citizen. Sera samples were analyzed at the National Center for Global Health and Medicine (NCGM) in Tokyo. The Ethics Committees from the Kumamoto General Hospital and NCGM approved this study (Kumamoto General Hospital No. 180, and NCGM-G-004176–00, respectively). Each participant provided a written informed consent, and this study abided by the Declaration of Helsinki principles. The vaccination (on days 0 and 21) and sera collection (from day 7 through day 90 post-1st dose) were conducted as shown in Table 1.
Cells and viruses
VeroE6TMPRSS2 cells24 were obtained from Japanese Collection of Research Bioresources (JCRB) Cell Bank (Osaka, Japan). VeroE6TMPRSS2 cells were maintained in DMEM supplemented with 10% FCS, 100 µg/ml of penicillin, 100 µg/ml of streptomycin, and 1 mg/mL of G418. SARS-CoV-2 NCGM-05-2 N strain (SARS-CoV-205-2 N) was isolated from nasopharyngeal swabs of a patient with COVID-19, who was admitted to the NCGM hospital40,41. Five clinically isolated SARS-CoV-2 mutant strains were used in the current study: two B.1.1.7 (alpha) strains [hCoV-19/Japan/QHN001/2020 (SARS-CoV-2QHN001, GISAID Accession ID; EPI_ISL_804007) and hCoV-19/Japan/QK002/2020 (SARS-CoV-2QK002, GISAID Accession ID; EPI_ISL_768526)] and a B.1.351 (beta) strain [hCoV-19/Japan/TY8-612-P0/2021 (SARS-CoV-2TY8-612)] were obtained from National Institute of Infectious Diseases, Tokyo, Japan. A B.1.617.1 (kappa) strain [TKYTK5356_2021 (SARS-CoV-25356, DDBJ Accession ID; LC633761)] and a B.1.617.2 (delta) strain [hCoV-19/Japan/TKYK01734/2021 (SARS-CoV-21734, GISAID Accession ID; EPI_ISL_2080609)] were provided from Tokyo Metropolitan Institute of public Health, Tokyo, Japan. Each variant was confirmed to contain each VOC-specific amino acid substitutions before the assays conducted in the present study (vide infra).
Neutralization assay
The neutralizing activity of sera on days 7, 28, 60, 90, and 150 from vaccinated individuals was determined by quantifying the sera-mediated suppression of the cytopathic effect (CPE) of each SARS-CoV-2 strain in VeroE6TMPRSS2 cells as previously described with minor modifications40. In brief, each sera was fourfold serially diluted in culture medium. The diluted sera were incubated with 100 50% tissue culture infectious dose (TCID50) of viruses at 37 °C for 20 min (final sera dilution range of 1:20–1:4000), after which the sera-virus mixtures were inoculated to VeroE6TMPRSS2 cells (1.0 × 104/well) in 96-well plates. For SARS-CoV-2 strains used in this assay are as follows: a wild-type strain, SARS-CoV-205-2 N (PANGO lineage B)40,41, two alpha variants (SARS-CoV-2QHN001 and SARS-CoV-2QK002), a beta variant SARS-CoV-2TY8-612, a delta variant SARS-CoV-21734, and a kappa variant SARS-CoV-25356. After culturing the cells for 3 days, the levels of CPE observed in SARS-CoV-2-exposed cells were determined using the WST-8 assay employing Cell Counting Kit-8 (Dojindo, Kumamoto, Japan). The sera dilution that gave 50% inhibition of CPE was defined as the 50% neutralization titer (NT50). Each sera was tested in duplicate.
Measurement of anti-SARS-CoV-2 antibody titers
Measurement of 3 anti-SARS-CoV-2 antibody levels (anti-S1-IgG, anti-S1-IgM, and anti-N-IgG) in sera of each participant obtained on days 7, 28, 60, 90, and 150 from 1st dose was performed using the chemiluminescence enzyme immunoassay (CLEIA) platform (HISCL) manufactured by Sysmex Co. (Kobe, Japan) as previously reported22.
Statistical analyses
Out of the 225 participants, one participant, who had been infected by SARS-CoV-2 with PCR positivity documented was primarily excluded. Demographic characteristics of the participants are described in Table 1. Correlates of neutralizing activity levels with S1-binding-IgG and -IgM levels, ages, pain scores in the injection-site, and systemic fever up to 40℃ were examined by Spearman rank correlation coefficient. Also, neutralizing activity levels, S1-binding-IgG, and -IgM, pain scores, systemic fever were compared between genders using the Wilcoxon rank sum test. As for the normal body temperature of the participants, 36.89 degree was used, which has been reported to be a normal body temperature in Japanese42. Percentage of the adverse events reported in writing following the 1st and 2nd dose administration were determined and assessed in regard to gender. The differences in neutralization activity between each measurement time point were tested by the Wilcoxon rank sum test, and were assessed among categorized age subgroups. Similarly, difference of S1-binding-IgG and -IgM levels among time points were tested. We considered the computed correlation coefficient low if the value was below 0.4, moderate if the value was between 0.4 and 0.7 and high if the value was above 0.7 according to Guilford’s Rule of Thumb. The threshold for statistical significance was p < 0.05. All the analyses were conducted with the use of R, version 4.1.0 (R Foundation for Statistical Computing).
References
World Health Organization. Coronavirus disease (COVID-19) outbreak situation. https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---29-june-2021 (2021).
Wu, F. et al. A new coronavirus associated with human respiratory disease in China. Nature 579, 265–269 (2020).
Zhou, P. et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 579, 270–273 (2020).
Mitsuya, H. & Kokudo, N. Sustaining containment of COVID-19: Global sharing for pandemic response. Glob. Health Med. 2, 53–55 (2020).
Dal-Re, R. et al. Ongoing and future COVID-19 vaccine clinical trials: Challenges and opportunities. Lancet Infect. Dis. 21, e342–e347 (2021).
Cohen, J. Effective vaccine offers shot of hope for pandemic. Science 370, 748–749 (2020).
Richman, D. D. COVID-19 vaccines: Implementation, limitations and opportunities. Glob. Health Med. 3, 1–5 (2021).
Walsh, E. E. et al. Safety and immunogenicity of two RNA-based Covid-19 vaccine candidates. N. Engl. J. Med. 383, 2439–2450 (2020).
Pfizer. News/Pfizer and BioNTech conclude phase 3 study of COVID-19 vaccine candidate, meeting all primary efficacy endpoints. https://www.pfizer.com/news/press-release/press-release-detail/pfizer-and-biontech-conclude-phase-3-study-covid-19-vaccine (2021).
Baden, L. R. et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N. Engl. J. Med. 384, 403–416 (2021).
Polack, F. P. et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N. Engl. J. Med. 383, 2603–2615 (2020).
Voysey, M. et al. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: An interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet 397, 99–111 (2021).
Johnson & Johnson. Johnson & Johnson COVID-19 vaccine authorized by U.S. FDA for emergency use—First single-shot vaccine in fight against global pandemic. https://www.jnj.com/johnson-johnson-covid-19-vaccine-authorized-by-u-s-fda-for-emergency-usefirst-single-shot-vaccine-in-fight-against-global-pandemic (2021).
Sadoff, J. et al. Safety and efficacy of single-dose Ad26.COV2.S vaccine against Covid-19. N. Engl. J. Med. 384, 2187–2201 (2021).
Korber, B. et al. Tracking changes in SARS-CoV-2 spike: Evidence that D614G increases infectivity of the COVID-19 virus. Cell 182, 812–827 (2020).
Xie, X. et al. Neutralization of SARS-CoV-2 spike 69/70 deletion, E484K and N501Y variants by BNT162b2 vaccine-elicited sera. Nat. Med. 27, 620–621 (2021).
Cele, S. et al. Escape of SARS-CoV-2 501Y.V2 from neutralization by convalescent plasma. Nature 593, 142–146 (2021).
Heath, P. T. et al. Safety and efficacy of NVX-CoV2373 Covid-19 vaccine. N. Engl. J. Med. 385, 1172–1183 (2021).
Novavax. Novavax COVID-19 vaccine demonstrates 89.3% efficacy in UK phase 3 Trial. https://www.globenewswire.com/news-release/2021/01/28/2166253/0/en/Novavax-COVID-19-Vaccine-Demonstrates-89-3-Efficacy-in-UK-Phase-3-Trial.html (2021).
Shinde, V. et al. Efficacy of NVX-CoV2373 Covid-19 vaccine against the B.1.351 variant. N. Engl. J. Med. 384, 1899–1909 (2021).
Wall, E. C. et al. Neutralising antibody activity against SARS-CoV-2 VOCs B.1.617.2 and B.1.351 by BNT162b2 vaccination. Lancet 397, 2331–2333 (2021).
Noda, K. et al. A novel highly quantitative and reproducible assay for the detection of anti-SARS-CoV-2 IgG and IgM antibodies. Sci. Rep. 11, 5198 (2021).
Melzack, R. The short-form McGill Pain Questionnaire. Pain 30, 191–197 (1987).
Matsuyama, S. et al. Enhanced isolation of SARS-CoV-2 by TMPRSS2-expressing cells. Proc. Natl. Acad. Sci. U S A 117, 7001–7003 (2020).
Waldmann, T. A. & Strober, W. Metabolism of immunoglobulins. Prog Allergy 13, 1–110 (1969).
Turner, J. S. et al. SARS-CoV-2 mRNA vaccines induce persistent human germinal centre responses. Nature 596, 109–113 (2021).
Stephens, D. S. & McElrath, M. J. COVID-19 and the path to immunity. JAMA 324, 1279–1281 (2020).
Doria-Rose, N. et al. Antibody persistence through 6 months after the second dose of mRNA-1273 vaccine for Covid-19. N. Engl. J. Med. 384, 2259–2261 (2021).
Tartof, S. Y. et al. Effectiveness of mRNA BNT162b2 COVID-19 vaccine up to 6 months in a large integrated health system in the USA: A retrospective cohort study. Lancet 398, 1407–1416 (2021).
Planas, D. et al. Reduced sensitivity of SARS-CoV-2 variant Delta to antibody neutralization. Nature 596, 276–280 (2021).
Oberhardt, V. et al. Rapid and stable mobilization of CD8(+) T cells by SARS-CoV-2 mRNA vaccine. Nature 597, 268–273 (2021).
Chen, N. et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 395, 507–513 (2020).
Yang, X. et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir. Med. 8, 475–481 (2020).
Williamson, E. J. et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature 584, 430–436 (2020).
Collazos, J., Asensi, V. & Carton, J. A. Sex differences in the clinical, immunological and virological parameters of HIV-infected patients treated with HAART. AIDS 21, 835–843 (2007).
Voysey, M. et al. Single-dose administration and the influence of the timing of the booster dose on immunogenicity and efficacy of ChAdOx1 nCoV-19 (AZD1222) vaccine: A pooled analysis of four randomised trials. Lancet 397, 881–891 (2021).
Khoury, D., et al. What level of neutralising antibody protects from COVID-19? medRxiv (2021).
Earle, K. A., et al. Evidence for antibody as a protective correlate for COVID-19 vaccines. medRxiv (2021).
Imai, M. et al. Syrian hamsters as a small animal model for SARS-CoV-2 infection and countermeasure development. Proc. Natl. Acad. Sci. U S A 117, 16587–16595 (2020).
Maeda, K. et al. Neutralization of SARS-CoV-2 with IgG from COVID-19-convalescent plasma. Sci. Rep. 11, 5563 (2021).
Hattori, S. I. et al. GRL-0920, an indole chloropyridinyl ester, completely blocks SARS-CoV-2 infection. MBio https://doi.org/10.1128/mBio.01833-20 (2020).
Wada, Y. For health care by taking the body temperature. Jpn. Soc. Mech. Eng. 112, 484–485 (2009).
Takamatsu, Y., et al. Highly-neutralizing COVID-19-convalescent-plasmas potently block SARS-CoV-2 replication and pneumonia in Syrian hamsters. bioRxiv (2021).
Acknowledgements
The authors thank Drs. Kenji Sadamasu, Mami Nagashima, Hiroyuki Asakura, and Mr. Isao Yoshida for providing two SARS-CoV-2 variants, Drs. Nobuyo Higashi-Kuwata, Shinichiro Hattori, Kouki Matsuda, Ms. Mariko Kato and Ms. Sachiko Otsu for helping some experiments, and Dr. Norihiro Kokudo for critical discussion for the manuscript. This research was supported in part by a grant from the Japan Agency for Medical Research and Development to Maeda (Grant Number JP20fk0108260, JP20fk0108502) and to Mitsuya (Grant Number 20fk0108502), and in part by a grant for MHLW Research on Emerging and Re-emerging Infectious Diseases and Immunization Program to Maeda (Grant Number JPMH20HA1006) from Ministry of Health, Labor and Welfare, and in part by a grant for COVID-19 to Mitsuya (Grant Number 19A3001) and Maeda (Grant Number 20A2003D) from the Intramural Research Program of National Center for Global Health and Medicine, and in part by the Intramural Research Program of the Center for Cancer Research, National Cancer Institute, National Institutes of Health (Mitsuya).
Author information
Authors and Affiliations
Contributions
K.M. and H.M. had access to all data in this study and took and hold all responsibility for the integrity of the data and the accuracy of the data analysis. K.M. and H.M.: Concept and design. K.M., M.A., K.T., T.M., K.N., Y.T., H.G., K.Y., S.O., T.S., and T.Y.: Acquisition, analysis, or interpretation of data. Y.U., Y.S., A.F., and H.M.: Statistical analysis. A.F., Y.I., H.N., M.K., S.M., A.M., W.S., and S.S.: Administrative, technical, or material support. K.M. and H.M.: Original draft writing. All authors: Reading and writing manuscript.
Corresponding authors
Ethics declarations
Competing interests
Matsushima, Noda, Sato, and Yoshida are employees of Sysmex Corporation. Other authors declare that there is no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Maeda, K., Amano, M., Uemura, Y. et al. Correlates of neutralizing/SARS-CoV-2-S1-binding antibody response with adverse effects and immune kinetics in BNT162b2-vaccinated individuals. Sci Rep 11, 22848 (2021). https://doi.org/10.1038/s41598-021-01930-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-01930-y
This article is cited by
-
Omicron BA.1 neutralizing antibody response following Delta breakthrough infection compared with booster vaccination of BNT162b2
BMC Infectious Diseases (2023)
-
Neutralization against Omicron sublineages (BA.2/BA.5/BQ.1.1/XBB/XBB.1.5) in bivalent BNT162b2-vaccinated HCWs with or without risk factors, or following BT infection with Omicron
Scientific Reports (2023)
-
Neutralization activity of IgG antibody in COVID‑19‑convalescent plasma against SARS-CoV-2 variants
Scientific Reports (2023)
-
SARS-CoV-2 specific T cell and humoral immune responses upon vaccination with BNT162b2: a 9 months longitudinal study
Scientific Reports (2022)
-
Neutralization activity of sera/IgG preparations from fully BNT162b2 vaccinated individuals against SARS-CoV-2 Alpha, Beta, Gamma, Delta, and Kappa variants
Scientific Reports (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.