Abstract
Objective To investigate the effect of electro-chemically activated water on biofilm contamination in dental unit water lines.
Design Thirteen dental units fitted with independent water systems and used for 12 years with distilled water were divided into two groups, A and B. At the start, one week later, and again four weeks later, the bacterial counts in water from all units were determined. Also specimens of tubing were taken from the units at the beginning and at the end of the study for SEM investigation. In Group A distilled water was replaced with electrochemically activated water (a Russian invention), and used continuously for the duration of the study. In group B, distilled water was used as before, until confirmed to be contaminated. For ethical reasons group B was treated, one week into the study with conventional disinfectants.
Setting The project was carried out in a clinic of a department of periodontology of a faculty of dentistry during 1998.
Results Both groups showed a marked reduction in bacterial counts. Under SEM Group A showed a total elimination of the biofilm and Group B a partial removal.
Conclusions Distilled water was ineffective in controlling bacterial counts and biofilm. Electrochemically activated water was effective for this purpose.
Similar content being viewed by others
Main
It has long been known that the water which is delivered from dental units handpiece and syringe outlets is highly contaminated with micro-organisms.1,2,3,4 Initially it was thought that the main source of these micro-organisms were the bacterial populations in patients' mouths, aspirated back into waterlines, but more recently the true source has been identified as the biofilm present in all dental units.5,6,7,89,10,11,12,13 The origin of the bacteria in a biofilm is considered to be the planktonic bacteria in the water supply.14,15,16 The dental unit with its long, narrow bore appears to be an ideal environment for the formation of a biofilm. The water in the tubing remains stagnant 99% of the time and even when it moves, it does so at slow speed. Waterborne bacteria rapidly attach themselves to the surface of the tubing and express genes that code for synthesis and secretion of the extracellular, adhesive alginates that constitute the acellular content of the biofilm matrix.8 The bacteria proliferate and produce polysaccharide exopolymers which forms the framework and a bed for the bacteria to live and multiply in. The bacteria in a biofilm show higher levels of physiological activity17 and enhanced resistance to chemical antimicrobials.18,19 Although the major source of bacteria in the biofilms in dental units are harmless bacteria in the water source, several pathogens such as Pseudomonas, Mycobacterium and Legionella have been isolated from dental unit water lines (DUWL).15,20,21,22,23 Some of these pathogens are known to flourish in the aqueous environment and are a major cause of nosocomial infections, resulting not infrequently in death.24,25 Herein lies the danger of DUWL biofilm contamination. The mere presence of the bacteria in the DUWL, even in the very large numbers reported (more than 1 million organisms per millimeter), is not presently viewed as a major health threat to the general population. However some very real concern has been expressed by many about the threat that these opportunistic pathogens may pose to the ever increasing population of immunocompromised patients.5,25,26,27 Two cases of postoperative infections in cancer patients, caused by Pseudomonas aeruginosa apparently originating from dental unit water, have been reported.5
The implications of potential pathogens being iatrogenically transmitted to patients undergoing dental treatment are serious. For the patients there are the risks of disease and even death, and for the profession the added possibility of litigation and adverse publicity is very real.28 Dentists' health would also seem to be directly at risk.29,30,31 The American Dental Association (ADA) is concerned about these problems and adopted a statement on December 13, 1995, identifying it as one of the critical research areas in dentistry today.25 The ADA set a number of less than 200 colony forming units per millilitre as the goal to be reached by all members by the year 2000.
It would appear that the use of municipal water directly connected to dental units can now be considered sub-standard level of care. To overcome these problems the use of independent water systems and microfilters has been suggested.10,26,27,32 It was also advised that a strict maintenance regime, consisting of daily flushing and purging with sodium hypochlorite be followed. The use of special in-office DUWL monitoring technology has also been prescribed.33 The independent water system or sterile water system (SWS) consists of a container pressurised by compressed air, delivered from the standard dental compressor. A few of the disadvantages of this regimen are
Time and energy required for daily change of filters
Possibility of corrosive action of sodium hypochlorite
Possibility of contamination of sterile water by unclean compressed air
Cost of producing or buying sterile water.
A product (STEDS, Radical Waters, Midrand, South Africa) based on a Russian invention, electro-chemically activated water (ECA) was developed for use in dental unit water lines. The original Russian inventors of the product make many claims and hold almost 300 Russian patents for applications in fields varying from agriculture, cooling towers, swimming pools, dermatology, dressing and cleaning of wounds and disinfection of instruments.34,35 The products have been widely used in Russia for many years.
ECA is considered totally harmless to human tissue, yet highly microbicidal.34,35 The raw products are water and saline. These are fed into a special unit which then 'activates' the water. The inventors describe the 'activation' process as a change of the molecular state of the water from a stable to a metastable state. Two kinds of ECA are produced, anolyte and catholyte. The inventors described anolyte as having an oxidation-reduction potential (ORP) in the region of +1000 mV and catholyte an ORP of –800 mV. Current thinking centers around the concept that the ORP of both solutions fluctuates between these values at a rate too rapid to measure. It is known that some of the biocidal agents in the solutions are ClO2, HClO, Cl2, ClO–, H2O2, HO2–, H2O2, NaOH, O2, O3, 1O2, H, OH. The presence of the free radicals with their oxidising effects in the solutions are considered of great importance. Higher organisms possess antioxidant defence systems whereas micro-organisms generally do not. Certain human defence cells also kill microbes by producing some of these very same free radicals.36 Anolyte solution is thought to have the antimicrobial effect and catholyte a detergent or cleaning effect.
It is further established that ECA solutions return to a stable, inactive state, pure water in fact, within a period of 48 hours after production. Different kinds or species of ECA solutions can be produced by different units, each with its own application.34,35
The purpose of this study was to evaluate the effect of ECA on DUWL previously supplied with distilled water in SWS.
Materials and Methods
Thirteen dental units at the University of Pretoria's Department of Oral Medicine and Periodontology were selected for this study. Selection was based on the fact that these units had always, since installation twelve years previously, been fitted with SWS. Since installation up to the time of inception of the study, distilled water was used in the SWS.
Seven of the units were placed in Group A, to be treated with ECA, and the six other units constituted Group B, a control group, to be treated with distilled water as before.
The treatment of group A, consisted of the replacement of distilled water in the SWS by ECA. No installation of any filters or additional purging with any detergents or disinfectants was carried out.
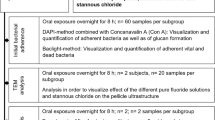
Immediately prior to the start of the experiment, samples of the water from all the units' three way syringes were collected in sterile vials for bacteriological culturing. Three samples of polyethylene tubing (internal diameter 1 mm) were also taken from each unit. One sample of each unit was immediately placed into a sterile vial filled with Ringers solution and the other two samples of tubing of each unit were immediately fixed in containers with glutaraldehyde solutions. The water taken from the three way syringes was serially diluted in sterile tap water. Aliquots (0.1 ml) were spread-plated onto R2A agarplates,37 and plates were incubated at 28°C for 96 hours. Similarly, specimens were taken from the tubing, transported in Ringers solution and cut in half, length-wise. One half was placed onto R2A agarplate, face down, and incubated at 28°C for 96 hours. The other half was fixed in gluteraldehyde, dried in a dustfree incubator, sputter coated with gold and viewed in a scanning electron microscope (SEM).
Immediately following the taking of the samples of tubing from the thirteen units, the units were repaired and the experimental phase commenced. A member of staff was designated to monitor all thirteen units continuously. All SWS in Group B were treated as before. The containers were merely topped up with distilled water as needed. The seven units in Group A were henceforth filled only with ECA. At the beginning of each working day, all containers in this group were emptied and filled with fresh anolyte solution. This anolyte solution was prepared on a daily basis, with a special STEDS unit, at a pH of 7.4. When these containers became empty through the course of the day, they were topped up with the supply of anolyte. At the end of the working day, all containers were emptied of anolyte solution and half filled with catholyte solution, pH 9.0, produced by the same STEDS unit. All these waterlines were then purged for 20 seconds allowing the catholyte to neutralize the anolyte and also, presumably, to carry out its cleaning effect. The anolyte is regarded as a strong oxidant and this may have some corrosive effect. The catholyte solution is considered to counter this effect.
One week after inception of the study, samples of water were again taken from all units' three way syringes and cultured as described above.
Five weeks after inception another series of water samples was taken and also two specimens of tubing were again taken from each unit, fixed in glutaraldehyde, and prepared and viewed in the SEM. Results were computed and analyzed using paired t-tests.
Results
At the start of the study the water samples taken from the three way syringes of all thirteen units produced counts of 3(breve)104–2(breve)105 colony forming units per millilitre (CFU/ml). The water (anolyte) from the three way syringes in Group A gave a count of <1 CFU/ml at one week after inception and Group B counts of 3(breve)104–2.5(breve)105CFU/ml. Group A were significantly less contaminated than Group B (p=0.000). This information gave rise to a serious ethical and moral dilemma which led to the demise of the control group (Group B) in certain respects. All thirteen units were in daily use with patients being treated with them. The continued use of these units represented an intolerable situation and the authorities decided to take immediate action to disinfect these units. The SWS were filled with a 0.5% sodium hypochlorite solution and the lines purged once daily for a week. Henceforth, only double distilled de-ionised water was used in these units (Group B). Group A was allowed to be used as described. Five weeks after inception of the experiment the water (anolyte) from all units in Group A again gave counts of <1 CFU/ml. Group B also gave counts of <1 CFU/ml. It was not attempted to carry out taxonomic identification of the micro-organisms present in the DUWL, because of the mammoth dimensions of an undertaking of this nature.
SEM studies of the samples taken at the start of the experiment clearly showed the presence of a well developed biofilm on all inner surfaces of tubing with several rods, cocci and spirochaetes present (fig. 1a – 1c). The biofilm in Group A was effectively destroyed and removed after five weeks of use of ECA (fig. 2a, 2b). The biofilm was still present, although in a 'cracked' or desquamated form, after five weeks in Group B (fig. 3a, 3b).
Discussion
The use of R2A agar plates and the incubation temperature of 28°C was based on the techniques described by others.37,38 They showed that many more bacteria can be cultured from water samples using this technique than using standard plate counts (SPC) and incubation at 37°C, and this is considered a more reliable method. Other investigators also made use of low nutrient media (dilute peptone) and reduced temperatures when studying biofilm contamination in DUWL.6,39 However a few also used enriched agar and 37°C (refs 7,40). It is thought that some opportunistic pathogens might be missed by the use of 37°C and enriched agar and therefore the use of these techniques should not be encouraged. This was highlighted in one study specifically directed at non-tuberculous mycobacteria using highly sophisticated techniques.22 They were able to show that dental treatment may be associated with heavy exposure to non-tuberculous mycobacteria. This is definitely not possible using SPC or the techniques employed by ourselves. In the same vein it can be argued that many other pathogens can be missed, because of the wide variety of micro organisms and techniques needed to identify them.
At the start of our study all DUWL proved to be heavily contaminated with micro-organisms. A well developed biofilm was also seen on the inner surfaces of all sections of tubing. The tubing containing water is an ideal habitat for a host of micro-organisms, to the extent of a thick biofilm forming. The water in the tubing only moves for a few hours every working day and is enriched with organics and contaminated during operation. This ensures the growth of bacteria in the system, especially at the surfaces, leading to the establishment of a stable source of innoculum for sterile water following replacement.
It is a fact that DUWL come into direct contact with patients' mouths every day and there is a real possibility of retrograde contamination of these lines from these rich sources, despite the presence of anti-retraction valves and devices.10 There has been no certain way in which these DUWL can be effectively sterilised, thereby preventing cross-contamination between patients. The fact that all thirteen dental units in this study, which had for years been used with distilled water in their SWS, proved to have well developed biofilms and to have unacceptably high levels of bacterial counts (3(breve)104–2(breve)105 CFU/ml), was quite alarming. The drastic reduction in contamination achieved by ECA on the other hand was cautiously considered as a breakthrough.
The presence of biofilm in dental units connected to municipal water supply is well documented.7,11,22,38 As mentioned above, the source of bacteria is thought to be the planktonic bacteria in the water supply, yet in our study these units had always, supposedly, been used with distilled water. In spite of this a biofilm had developed in all the units. Two explanations are offered for this phenomenon. The biofilm could be the result of retograde infection from oral cavities of patients through the lack of efficient anti-retraction valves in the equipment. Alternatively the possibility of unsupervised members of staff or students, through the years occasionally using tap water instead of distilled water, can not be ruled out. The use of tap water, with only a few hundred micro-organisms present in it, only once, is enough for the development of a biofilm. A biofilm consists of single bacterial cells embedded in a highly hydrated, predominately anionic matrix of bacterial expoloymers.15 This gel like matrix limits the access of anti-bacterial agents such as surfactants, biocides and antibiotics and is one of the reasons why biofilm bacteria do not respond in the same way as planktonic bacteria to the aforementioned agents.
Conventional disinfectants are ineffective against non-tuberculous mycobacteria (NTM) when used in DUWL.22 In that study the presence of NTM in DUWL of a series of 21 dental units, was found to exceed that of drinking water by a factor of 400. Five of these units were subjected daily to a routine of automatic disinfecion, using either a proprietary disinfectant or a process of anodic oxidation and the levels of contamination in these units were similar to that of the untreated units. The authors were of the opinion that dental treatment may be associated with heavy exposure to NTM.
Neutralization, removal or destruction of the matrix would render bacteria more vulnerable to the action of anti-bacterial agents. It is possible that the highly hydrated matrix's integrity could be injured by the action of free radicals such as the hydroxyl radicals, the strongest oxydising agent known to man, in the anolyte solution. The hydroxyl radicals would take hydroxen ions from the matrix, leading to a collapse of the matrix and exposure of the bacteria to the actions of more hydroxyl and other radicals. This could explain the dramatic drop in the numbers of bacteria and the removal of the biofilm in our study following the introduction of ECA.
From a purely technical point of view the demise of the control group, through the use of conventional disinfectants, was regrettable. There was, however, no other option. It was considered unethical to continue treating patients in units which were so heavily contaminated. The control group, group B, had served its initial purpose, having proven to be contaminated at one week, while group A, treated with ECA, gave a remarkable result of <1 CFU/ml at the same time. At the end of the study, both groups gave similar counts of <1 CFU/ml, proving the efficacy of both ECA and conventional disinfectants combined with sterile water in reducing the bacterial counts in DUWL. Bacterial counts of <1 CFU/ml are well below the 200 CFU/ml, set by the American Dental Association, for the year 2000. The problem with conventional disinfectants (sodium hypochlorite in this case) remains. It is highly corrosive and the taste and smell are unacceptable. Furthermore, a once daily, or worse once weekly flush with sodium hypochlorite does not provide round the clock protection as sterile water is easily contaminated in the SWS. This problem would seem to be overcome with ECA, because it can be used continually in DUWL.
ECA appeared to eliminate the biofilm more completely than did the conventional disinfectant. ECA produced smooth clean surfaces of tubing, whereas the biofilm in the control group, treated with sodium hypochlorite, still had the cracked, desquamating appearance. With time this biofilm may also disappear. The significance of these observations may be important for the control of biofilm in other areas (outside dentistry) as well.
The continuous supply of ECA as a coolant, directly onto burs, can be of value in the disinfection of cavities, as these are being prepared. Similarly the disinfection of root canals, as they are being prepared with rotary instruments, can be of considerable benefit. Another advantage may be the reduction in aerosol formed by the turbine handpiece.
The single greatest area of concern regarding ECA technology is the issue of safety to humans. There exists no published scientific evidence which can confirm or deny the safety of the product. However, circumstantial and anecdotal evidence intimates that the product may be safe, at least for use in DUWL.
Firstly, ECA is nothing but electrolyzed water, with a little salt added. Logic and common sense dictate that no noxious chemical compounds can be synthesized by such a device.
Secondly, it is reported from Russia that for many years, ECA has been used directly on open wounds and on purulent areas. It is used there to wash eyes and patients also drink large quantities of it.41,42 Obviously these reports need to be corroborated by scientific investigation.
Thirdly, it is salient to remember that dental patients are only exposed to very small volumes of water from DUWL. Most of the water is also immediately removed by the vacuum lines. The resultant exposure under normal circumstances is minimal.
Fourthly, there exists some concern about the dangers of free radicals in general. It is thought that continuous exposure to free radicals over many years might predispose to cancer, ageing and ischaemic heart diseases. The limited exposure of dental patients to the small quantities of free radicals in ECA and DUWL should pose no real health hazard, but until proven safe dental personnel should be advised to handle ECA with due care and caution, in the same ways as with röntgen rays, mercury and resins.
Fifthly, chemical compounds such as chlorhexidine gluconate,3 chlorhexidine acetate,40 sodium hypochlorite,4 povidone iodine (10%),26 and listerine,43 have been advocated for use in DUWL. These are all complex molecules with varying degrees of toxicity. ECA does not consist of a similar complex chemical compound. It is derived from pure water and saline and can only consist of different ions, radicals, atoms and molecules of hydrogen, oxygen, sodium and chloride. It is hard to imagine that substances in whatever form, derived from these atoms and molecules by the simple process of electrolysis, can be as toxic as sodium hypochlorite or chlorhexidine acetate or gluconate or povidone iodine.
Finally, a very similar system, the Moggod (Mixed oxidant gas generated on demand), which is also an electrolytic membrane cell which produces an oxidising gas by passing an electrical current through a saturated sodium chloride solution, has been recommended for use in potable water disinfection in small communities in developing countries.44,45 The authors of those studies, associated with the Imperial College of Science, Technology and Medicine, The Robens Institute of Health and Safety, University of Surrey and the Centre for Environmental Health and Engineering, University of Surrey expressed no concern whatsoever about the safety of the technology to humans. The important point is that this technology (Moggod) was invented for drinking water, whereas the Steds system, which uses the same raw products as the Moggod, is intended for use in DUWL. Thus the exposure of patients to the solutions produced by the Steds system would be minimal in comparison with that of people drinking water disinfected by the Moggod System.
Notwithstanding these arguments there exists an urgent need for the testing of ECA on experimental animals and on cell cultures before the widespread use of the product in DUWL can be recommended. Studies of this nature have been initiated and the results will be published as soon as they become available.
Conclusion
The use of distilled water in independent water systems offers no protection against bacterial contamination. Electro-chemically activated water effectively reduces bacterial counts and removes biofilm in dental unit water lines.
References
Scaiky I and Sultizeanu A . Importance of dental units in the mechanical transfer of oral bacteria. J Dent Res 1962; 41: 714–715.
Neff J H and Rosenthal S L . A possible means of inadvertant transmission of infection to dental patients. J Dent Res 1957; 36: 932–934.
Blake C . The incidence and control of infection in dental spray reservoirs. Br Dent J 1963; 115: 413–416.
Abel L C, Miller R L, Micik R E, Ryge G . Studies on dental aerobiology. Bacterial contamination of water delivered by dental units. J Dent Res 1971; 50: 1567–1569.
Martin M V . The significance of bacterial contamination of dental unit water systems. Br Dent J 1987; 163: 152–154.
Tall B D, Williams N S, George K S, Gray R T and Walch M . Bacterial succession within a biofilm in water supplies lines of dental air-water syringes. Can J Microbiol 1995; 41: 647–654.
Whitehouse R L S, Peters E, Lisotte J, Lilge C . The influence of biofilms on microbial contamination in dental unit water. J Dent 1991; 19: 290–295.
Williams J F, Molinari J A, Andrews N . Microbial contamination of dental unit waterlines: Origins and Characteristics. Compendium 1996; 17: 538–588.
Mayo J A, Oertling K M, Andrieu S C . Bacterial biofilm: a source of contamination in dental air–water syringes. Clin Prev Dent 1990; 12: 13–20.
Williams J F, Andrews N, Santiago J I . Microbial contamination of dental unit waterlines: Current preventive measures and emerging options. Compendium 1996; 17: 691–709.
Williams H N, Bear M L, Kelly J J . Contribution of biofilm to the contamination of the dental unit water supply. JADA 1995; 126: 1255–1260.
Williams H N, Johnson A, Kelley J J, Baer M L, King T S, Mitchell B, Hasler F . Bacterial contamination of the water supply in newly installed dental units. Quint Int 1995; 26: 331–337.
Kelstrup J, Funder-Neilsen T D, Theilade J . Microbial aggregate contamination of water lines in dental equipment and its control. Acta Path Microbiol Scand B 1977; 85: 177–183.
Costerton J W . Irvin R J, Cheng K J . The bacterial glycocalyx in nature and diseases. Ann Rev Microbiol 1981; 35: 299–324.
Costerton J W, Cheng K-J, Geesey G G, Ladd T I, Nickel J C, Dasgupta M, Marrie T J . Bacterial biofilms in nature and disease. Ann Rev Microb 1987; 41: 435–464.
Exner M, Tuschawitzki G J, Sharnagel J . Influence of biofilms by chemical disinfectants and mechanical cleaning. Zentralbl Bakteriol Microbiol Hyg 1987; 183: 549–563.
Manz W, Szewzyk U, Ericson P . In situ identification of bacteria in drinking water and adjoining biofilms by hybridization with 16s and 23s r RNA-directed fluorescent oligo-nucleotide probes. Appl Environ Microbiol 1993; 59: 2293–2298.
Costerton J W . The formation of biocide-resistant biofilms in industrial, natural and medical systems. Dev Ind Microbiology 1984; 25: 363–372.
Yu F P, McPeters G A . Physiological response of bacteria in biofilms to disinfection. Appl Environ Microbiol 1994; 60: 2462–2466.
Williams J F, Johnston A M, Johnson B, Huntington M K, MacKenzie C D Microbiological contamination of dental unit water lines: prevalence, intensity and microbial characteristics. JADA 1993; 124: 59–65.
Reinthaler F, Mascher F . Legionella pneumophilia in dental units. Zentralblatt fur Bakteriologie, Mikrobiologie und Hygiene; Series B 1986; 183: 86–88.
Schulze-Robecke R, Janning B, Fischeder R . Occurrence of mycobacteria in biofilm samples. Tubercle and Lung Disease 1992; 73: 141–144.
Von Graevenitz A . The role of opportunistic infections in human diseases. Ann Rev Microbiol 1977; 31: 441–471.
Institute of Medicine, Factors in Emergence. In: Lederberg J, Shope R E, Oaks S C, eds. Emerging infections: Microbiol threats to health in the USA. Washington DC National Academy Press 1992; 34–112.
Shearer B G . Biofilm and the dental office. JADA 1996; 27: 181–189.
Mills S, Bednarsh H . Dental Waterlines and biofilms. Dental teamwork 1996; May/June: 15–21.
Fayle S A, Pollard M A . Decontamination of dental unit water: a review of current recommendations. Br Dent J 1996; 181: 369–272.
Clappison R A . Priority one: Decontamination of Dental Unit Waterlines. Oral Health 1997; June: 11–15.
Reinthaler F F, Mascher F, Stunzner D . Serological examination for antibodies against Legionella species in dental personnel. J Dent Res 1988; 67: 942–943.
Fotos P, Westfall H N, Snyder I S, Miller R W, Mutchler B M . Prevalence of Legionella — specific IgG and IgM antibody in a dental clinic population. J Dent Res 1986; 64: 1382–1385.
Atlas R M, Williams J F, Huntington M K . Legionella contamination of dental-unit waters. Appl Envir Microb 1995; 61: 1208–1213.
Murdoch-Kinch C A, Andrews N L, Atwan S, Jude R, Gleason M J, Molinari J A . Comparison of Dental Water Quality Management Procedures. JADA 1997; 128: 1235–1243.
Karpay R I, Plamondon T J, Mills S E, Dove B . Validation of an in-office dental unit water monitoring technique. JADA 1998; 129: 207–211.
Leonov B I . Electrochemical activation of water and aqueous solutions: Past, present and future. In: Proceedings of the First International Symposium on Electrochemical activation 1997. Moscow; 11–27.
Bakhir VM . Electrochemical activation: Theory and practice. In: Proceedings of the First International Symposium on Electrochemical Activation 1997. Moscow; 38–45.
Block S S . Peroxygen compounds. In: Disinfection, Sterilization and Presentation, 4th Edition, Edited by S S Block (1991); 167–181.
Reasoner D J, Geldreich E E . A new medium for the enumeration and subculture of bacteria from potable water. Appl Envir Microb 1985; 49: 1–7.
Barbeau J, Tanguay R, Faucher E, Avezard C, Trunder L, Côté and Prévoust A P . Multiparametric Analysis of Waterline Contamination in Dental Units. Appl Environ Microbiol 1996; 62: 3954–3959.
Williams N H, Quinby H, Rombery E . Evaluation and use of a low nutrient medium and reduced incubation temperature to study bacterial contamination in the water supply of dental units. Can J Microbiol 1994; 40: 017–131.
Douglas C W I and van Noort R . Control of bacteria in dental water supplies. Br Dent J 1993; 174: 167.
Mashkoval O A, Vorontsova E M . Experience of anolyte and catholyte (electrochemically activated solutions). In: Proceedings of the First International Symposium on Electrochemical activation 1997. Moscow; 130–132.
Gitsevitch G N . Optimal drinking regime in an orthopedic hospital. In: Proceedings of the First International Symposium on Electrochemical Activation 1997. Moscow; 174–175.
Miller C H . Microbes in dental unit water. J Calif Dent Ass 1996; 24: 47–52.
Barrot L P, Lloyd B J, Graham V J D . Comparative evaluations of two novel disinfection methods for small-community water treatment in developing countries. J Water SRT-Aqua 1990; 39: 396–404.
Barrot L P, Graham V J D, Lloyd B J . Further evaluation of an on-site chlorine gas generator (Moggod) for small community water disinfection in developing countries. J Water SRT-Aqua 1994; 43: 145–153.
Author information
Authors and Affiliations
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Marais, J., Brözel, V. Electro-chemically activated water in dental unit water line. Br Dent J 187, 154–158 (1999). https://doi.org/10.1038/sj.bdj.4800228
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4800228