Abstract
To evaluate the effect of population-based cervical cancer screening on the occurrence of cervical cancer in The Netherlands, we investigated the incidence and survival of cervical cancer registered by a cancer registry in the Greater Amsterdam area. The incidence rate of squamous cell carcinoma decreased significantly from 9.2/100 000 women in 1988 to 5.9/100 000 in 2000 (P<0.001). The incidence rate of adenocarcinomas remained stable. After adjustment for age, stage and lymph node involvement, the relative risk of death was 1.6 times higher for patients with adenocarcinomas than for patients with squamous cell carcinoma (95% CI 1.2–2.1). The decreased survival was related to histological type, as the effect remained significant after correction for confounding factors. Over time, the prognosis of women with squamous cell carcinoma improved significantly. No significant change was observed for women diagnosed with adenocarcinoma. These results suggest that the screening programme in The Netherlands as executed in the Greater Amsterdam area is associated with a decreased incidence and increased survival of patients with squamous cell carcinoma, but fails to detect (pre)malignant lesions of adenocarcinoma. Since more than 92% of adenocarcinomas and its precursors contain high-risk HPV, adding HPV testing to cytologic screening might improve the present screening programme in detecting adenocarcinoma and its precursor lesions.
Similar content being viewed by others
Main
Population-based cervical cancer screening has led to a decrease in the incidence of cervical cancer (Gustafsson et al, 1997; Vizcaino et al, 2000). However, recent data suggest that the decrease in incidence is caused by a decrease of squamous cell carcinoma, while the incidence of adenocarcinoma of the cervix shows no change or sometimes even an increase (Anttila et al, 1999; Bergstrom et al, 1999; Hemminki et al, 2001; Liu et al, 2001).
It has been suggested that the unchanged or even increased incidence of adenocarcinoma of the cervix is the result of systematic underscreening of cervical smears for (pre)malignant changes of adenocarcinoma of the cervix (Parkin et al, 1985; Mitchell et al, 1995; Stockton et al, 1997). Moreover, patients with adenocarcinomas of the cervix are considered to have a decreased survival compared to patients with squamous cell carcinomas (Hopkins and Morley, 1991; Lai et al, 1999; Nakanishi et al, 2000; Grisaru et al, 2001). It has been suggested that this decreased survival is associated with higher stages of disease with which patients with adenocarcinomas are detected.
Here, we report on the incidence and survival rates of cervical cancer cases registered by a cancer registry in a large geographically defined region of The Netherlands, the Greater Amsterdam area. Special attention was paid to trends in incidence and survival rates for cases of squamous cell carcinoma and adenocarcinoma.
Materials and methods
Data collection
The cancer registry of the Comprehensive Cancer Centre Amsterdam (CCCA, ‘Amsterdam Cancer Registry’) is a population-based cancer registry since 1988, and part of the nationwide Netherlands Cancer Registry as of 1989. It covers two out of 12 Dutch provinces: Noord-Holland and the major part of Flevoland. The population of the CCCA region increased from 2.50 million on 1 January, 1988 to 2.80 million on 1 January, 2001. All malignant tumours were registered in all 20 hospitals in the region, comprising two university hospitals and a specialised cancer hospital (where cancer patients are treated).
Clinical information and pathology data were extracted from the medical records. Apart from demographic data, data were collected on tumour site, morphological classification (according to the International Classification of Diseases for Oncology) and stage of the tumour. The fourth edition of the TNM-classification was used whenever applicable (Hermanek and Sobon, 1987). In 1988–1993, the FIGO stage was registered separately, and after 1993 the FIGO stage was derived from TNM stage. Data concerning participation in cervical cancer screening programmes were not available.
For this study, all cervical cancer cases diagnosed between 1 January, 1988 and 31 December, 2000 were selected from the cancer registry. The following tumours were excluded: noninvasive tumours and tumours diagnosed in patients living outside the CCCA region. Patients diagnosed in a hospital outside the region, but living in the CCCA region were included. Information on the vital status of all patients was collected in the hospitals and from general practitioners. However, the majority of the information on vital status was obtained from record linkage of computerised data on all deceased persons in the study period that were made available by 51 of the 74 municipalities in the CCCA region (covering more than 85% of the population). Inquiries about the vital status of patients living in the other 23 municipalities were made at the municipal population registers and at the Central Office for Genealogy of The Netherlands, The Hague. Less than 1% of the cases were lost to follow-up. In the survival analyses, cases diagnosed in 1998–2000 were excluded, because of the short period of follow-up. Tumours first diagnosed at autopsy, second (or third, etc.) tumours and noncarcinomas were also excluded from the survival analyses. Follow-up of the patients diagnosed in 1988–1997 was complete until at least 1 January, 1999.
Population data of The Netherlands were obtained from Statistics Netherlands (CBS, Voorburg/Heerlen, The Netherlands). Data from Statistics of Netherlands were also obtained with respect to the survival of the general Dutch population.
Statistical analysis
Incidence of cervical cancer was calculated per 100 000 person years. Direct standardisation was used for age adjustment with respect to the European standard population, and the European standardised rates (ESRs) were calculated. Trends in the incidence of the ESR were investigated by calculating the estimated annual percent change (EAPC) (Visser et al, 2001). For the analyses, cases were divided into squamous cell carcinoma, adenocarcinoma including adenosquamous carcinoma and other histological type (i.e., other and unspecified carcinomas, sarcomas and undefined tumours). Age was divided into 15-year categories. However, age categories of 15–29 and 30–44 years were analysed jointly in the survival analyses, based on the low number of cases (n=90) in the category of 15–29 years. Differences in distribution over stage and age categories were assessed with χ2 statistics.
Relative survival and 95% confidence intervals (CIs) were calculated as a measure of disease-specific survival (Hakulinen and Abeywickrama, 1985). The relative survival is the ratio between crude and expected survival and is close to disease-specific survival. We did not calculate disease-specific survival, because the cause of death was not available as linkage with the death registry in The Netherlands is not possible.
The Cox multivariate regression analysis for survival was performed to investigate survival. Associations were examined for all cases, and for cases of squamous cell carcinoma and adenocarcinoma separately. In the analyses, the FIGO classification was used to adjust for stage. Lymph node status is not considered in the FIGO classification for cervical carcinoma, and therefore it was introduced in the analyses as a separate variable. For cases diagnosed in 1988, TNM was not registered, so these cases were classified as ‘nodal involvement unknown’. Age, stage and nodal involvement were divided into categories and entered into the model as dummy variables. P-values of 0.05 or less were considered statistically significant. Using STATA 6.0 for Windows, hazard ratios (HRs) and 95% CIs were calculated.
Results
From 1988 up to 2000, 1925 patients were diagnosed with invasive cervical cancer (Table 1). The annual number of incident cases of cervical cancer decreased from 157 patients registered in 1988 to 135 patients in 2000. The ESR decreased from 11.8/100 000 women in 1988 to 8.2/100 000 women in 2000. The total ESR decreased by 2.7% annually (P=0.001). This decrease in incidence was mainly caused by a decrease in the incidence of squamous cell carcinoma cases, as the EAPC in ESR for squamous cell carcinomas was −3.2% (P<0.001). For adenocarcinomas, there was no statistically significant trend in the incidence (EAPC −1.1%, P=0.54). The incidence of other cervical malignancies decreased with 1.4% annually (P=0.74). During the study period, the contribution of adenocarcinomas to the total number of malignancies increased from 16% in 1988–1990 to 18% in 1998–2000.
The median age of patients with adenocarcinoma was 3 years below the median age of patients with squamous cell carcinoma, that is 44 years (range: 18–92) and 47 years (range: 19–98), respectively (P<0.05). Age-specific incidence was highest in age groups 35–39 and 70–84 years for squamous cell carcinoma patients, and the age-specific incidence was highest in the age group 35–49 years for adenocarcinoma patients (Figure 1).
Younger patients were more often diagnosed in early stages of cancer than older patients (Figure 2). Of women 15–29 years, 82% were diagnosed with FIGO stage I disease, while only 15% of patients 75 years and over were diagnosed with FIGO stage I disease. Only 2% of the patients in the age category 15–29 years were diagnosed in stage IV, while 14% of the oldest patients were diagnosed in this stage. Figure 3 shows that 55% of squamous cell carcinomas and 65% of patients with adenocarcinomas were diagnosed in FIGO stage I (P=0.003). However, adenocarcinomas were diagnosed less often in the microinvasive (i.e., Ia) stage of the disease than squamous cell carcinomas (15 and 22%, respectively) (P<0.0001). The percentage of cases diagnosed in FIGO stage IV did not differ statistically significantly between squamous cell carcinomas (7%) and adenocarcinomas (6%) (P=0.71). During the study period, there were no statistically significant changes in distribution over the stages.
During 1988–1997, there were 1441 patients with cervical carcinoma in the region of the CCCA, 480 of whom died (33.3%). The median follow-up time was 56 months (range: 0–165 months). The overall 5-year relative survival of cervical carcinoma was 71% (Table 2). Relative survival decreased from 85% for women <45 years to 41% for women of 75 years and over. Patients with FIGO stage I had a relative survival of 91% decreasing to 16% for tumours diagnosed in FIGO stage IV. Relative survival of squamous cell carcinomas was 72% (95% CI: 69–75%), and somewhat lower for adeno(squamous)carcinomas (66%, 95% CI: 59–72%).
Table 3 displays the results of the multivariate analysis of survival for all types of cervical cancer. Compared to FIGO stage I, all other stages had significantly increased HRs. Lymph node status is not considered in the FIGO classification for cervical carcinoma. For cases diagnosed in 1988, TNM was not registered and these cases were classified as ‘nodal involvement unknown’. However, nodal involvement appeared to be associated with an increased risk of death (HR 2.1, 95% CI 1.6–2.7). Tumour histology was investigated with squamous cell carcinoma cases as reference category. Univariately, the HR of adenocarcinomas was slightly increased (HR 1.1), while other/unspecified carcinomas were associated with a significant increase in risk. The increased risk for other/unspecified carcinomas disappeared with multivariate adjustment, indicating that the increase in risk was caused by confounding by age and stage. After adjustment, the HR for adenocarcinomas was significantly increased (HR 1.6, 95% CI 1.3–2.1). Over time, the prognosis of patients with cervical cancer improved, as the multivariate HRs were decreased for the periods 1991–1993 and 1994–1997 as compared to the reference period 1988–1990. Adjustment for stages 1a and 1b separately did not alter these findings substantially (data not shown).
Squamous cell carcinoma cases and adenocarcinoma cases were also analysed separately (Table 4). Both for squamous cell carcinomas and adenocarcinomas, survival decreased with increasing age, higher FIGO stage and positive lymph nodes at diagnosis (data not shown). The improvement in survival of women with cervical cancer during the period 1988–1997 was associated with cases of squamous cell carcinoma only. Survival of women with cervical adenocarcinoma did not improve during the study period (Table 4).
Discussion
Our results show that the incidence of cervical cancer has decreased significantly during the period 1988–2000, and that this decrease is caused by a decrease in the incidence of squamous cell carcinomas. In multivariate analyses, survival for patients diagnosed with adenocarcinoma of the cervix was significantly lower than survival for patients with squamous cell carcinoma. This indicates that women with adenocarcinoma of the uterine cervix have an intrinsically increased risk of death compared with women with squamous cell carcinoma independent of stage, age and nodal involvement.
We studied patients with cervical cancer who were all diagnosed within a geographically defined region in The Netherlands: the Greater Amsterdam area. As data were obtained by the Regional Cancer Registry, we were able to study an unbiased population of women with different histological types of cervical cancer for factors associated with survival. In this study, the histological verification rate was 99.8%. Nationally, the histological verification rate for cervical cancer is 99.7%, indicating a high accuracy rate of the Dutch Cancer Registries (Visser et al, 1997).
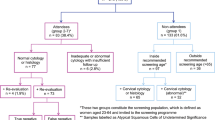
In this study, knowledge of participation in cervical cancer screening preceding the diagnosis of cancer may have been relevant. We did not have data on either individual Pap smear taking or participation in the nationwide screening programme in this group of women with cervical carcinoma. Cytological screening on an individual basis has been available for women in this region of The Netherlands since the 1970s. A nationwide screening programme aimed at specific age categories was initiated in 1988. Between 1988 and 1996, women aged 34–54 years were screened triannually, and from 1996 onwards, women aged 30–60 years are screened every 5 years. Overall, the coverage of cervical cancer screening activities over a period of 5 years is approximately 80% (van Ballegooijen and Hermens, 2000). However, regional participation in each screening round of the population-based programme is lower (60–70%). Even without data on screening participation, some findings do suggest the efficacy of screening in this region of The Netherlands. The incidence of cervical squamous cell carcinoma decreased significantly, while no statistically significant change in the incidence of adenocarcinoma was found. Previous studies have reported that cervical adenocarcinoma and its preinvasive stages are diagnosed less efficiently by Pap smear screening than squamous cell lesions (Mitchell et al, 1995; Stockton et al, 1997). In some countries, not only the absence of a decrease in incidence (Sigurdsson, 1993; Nieminen et al, 1995), but also increases in the incidence of cervical adenocarcinoma have been described in the presence of a screening programme (Bergstrom et al, 1999; Hemminki et al, 2001; Liu et al, 2001). One study even suggested an increase in incidence especially in younger women (Anttila et al, 1999), whereas older women were not affected by increases in the incidence rate of cervical cancer. Our data do not support this trend. Our findings suggest a positive effect of the screening programme as shown by the decrease in cervical carcinoma incidence. Increasing screening participation to obtain an even higher degree of coverage will most likely increase the efficacy of the screening programme in decreasing the incidence of cervical cancer.
In our analyses, patients with cervical adenocarcinoma had a worse prognosis than patients with squamous cell carcinoma after correction for confounders such as age, stage and nodal involvement. Previous studies either usually lacked sufficient numbers of patients with adenocarcinomas (Pilch et al, 2001), or were not population-based (Hopkins and Morley, 1991; Nakanishi et al, 2000), or did not make direct comparisons between patients with squamous cell carcinoma and adenocarcinoma (Benedet et al, 1998). Some studies attributed the decreased survival of women with adenocarcinoma to differences in histological type (Lai et al, 1999; Grisaru et al, 2001). In our study, patients with adenocarcinoma presented with more advanced stage I tumours than patients with squamous cell carcinomas. Still, patients with cervical adenocarcinoma were slightly younger at diagnosis than patients with squamous cell carcinoma, 48 and 50 years, respectively. As the association between adenocarcinomas and a worse prognosis increased after correction for confounding factors, this indicates that women with cervical adenocarcinoma have an inherently worse prognosis than women with squamous cell carcinoma. The main causal factor for the development of both squamous cell carcinoma and adenocarcinoma of the uterine cervix is infection with high-risk types of the human papillomavirus (hrHPV) (Walboomers et al, 1999; Bosch et al, 2002). There are substantial differences with respect to the exact type of hrHPV and the histological diagnosis. Adenocarcinomas are more often associated with HPV type 18 than squamous cell carcinomas (Bosch et al, 1995, 2002; Andersson et al, 2001; Clifford et al, 2003). Moreover, HPV 18 has been shown to be associated with a worse prognosis than other HPV types (Hildesheim et al, 1999; Schwartz et al, 2001), but this finding has been challenged (Pilch et al, 2001). An intrinsic difference between neoplasically converted squamous and cylindrical epithelium might also be the cause of the difference in prognosis, independent of HPV infection.
The survival of patients with squamous cell carcinoma increased during 1988–1997, while the survival of patients with adenocarcinomas did not change significantly. During the study period, there were no large changes in treatment of patients with cervical cancer in any stage of the disease. The nationwide screening programme was introduced in 1988. Theoretically, an improvement in the prognosis of patients with squamous cell carcinomas might have been caused by a major change in stage at diagnosis during the study period. We did not observe such a change in stage at diagnosis over time (data not shown). However, we cannot exclude an effect of subtle changes within broad stages, such as a shift from FIGO 1b to FIGO 1a. Screening, leading to an earlier detection of cervical cancer even without significant changes in broad FIGO stage distribution, may contribute to such an effect. We were not able to find a trend over time in histological lymph node positivity over all stages of disease, as lymph node sampling is dependent on stage at diagnosis. In this study, in 31% of women with adenocarcinoma and 43% of women with squamous cell carcinoma, lymph node status was not determined histologically. Stage migration due to improved staging procedures might also have contributed to the increased survival. Still, the statistically significant difference in survival was based on small numbers of adenocarcinoma cases compared to squamous cell carcinoma cases. Therefore, caution should be taken into account when interpreting trends in the survival of adenocarcinoma based on these data.
The overall 5-year survival rate was 71%. Compared to other countries in Europe, this is a high survival rate, with only the Nordic countries having comparable survival rates (Berrino et al, 1999). Other studies have also shown that within Europe, The Netherlands have a very low incidence, and a very high survival compared with other countries (Levi et al, 2000). It is reasonable to attribute these findings to the presence of a nationwide screening programme, as similar effects on incidence have been described in other countries with a screening programme (Gustafsson et al, 1997). Whether the effect on survival in the absence of changes in treatment can be exclusively attributed to the cervical cancer screening programme, remains a question of debate (Quinn et al, 1999; Sasieni and Adams, 1999).
Our study suggests that the present screening programme for cervical cancer is efficient in detecting (pre) malignant stages of squamous cell carcinoma, but fails to detect (pre) malignant stages of adenocarcinoma (Sasieni and Adams, 2001). Since more than 92% of the adenocarcinomas and its precursors contain hrHPV (Pirog et al, 2000; Pilch et al, 2001), adding hrHPV testing to conventional cytological screening might improve the present screening programme in detecting adenocarcinoma and its precursor lesions. This should be a focus of further research concerning the functioning of the screening programme for cervical cancer.
In conclusion, in the Greater Amsterdam area, the incidence of squamous cell carcinomas has decreased while there were no changes in the incidence of adenocarcinoma of the uterine cervix. Cases of adenocarcinoma of the uterine cervix are associated with a decreased survival rate compared to patients with squamous cell carcinoma. This decreased survival is related to tumour histology itself, since after correction for factors such as age, stage and lymph node status, the survival of adenocarcinoma patients is still lower compared with squamous cell carcinoma patients.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Andersson S, Rylander E, Larsson B, Strand A, Silfversvard C, Wilander E (2001) The role of human papillomavirus in cervical adenocarcinoma carcinogenesis. Eur J Cancer 37: 246–250
Anttila A, Pukkala E, Soderman B, Kallio M, Nieminen P, Hakama M (1999) Effect of organised screening on cervical cancer incidence and mortality in Finland, 1963–1995: recent increase in cervical cancer incidence. Int J Cancer 83: 59–65
Benedet J, Odicino F, Maisonneuve P, Severi G, Creasman W, Shepherd J, Sideri M, Pecorelli S (1998) Carcinoma of the cervix uteri. J Epidemiol Biostat 3: 5–34
Bergstrom R, Sparen P, Adami HO (1999) Trends in cancer of the cervix uteri in Sweden following cytological screening. Br J Cancer 81: 159–166
Berrino F, Capocaccia R, Esteve J, Gatta G, Hakulinen T, Micheli A, Sant M, Verdecchia A (1999) Survival of Cancer Patients in Europe: the EUROCARE-2 Study. IARC Scientific Publication [No. 151.]. Lyon: IARC
Bosch FX, Lorincz A, Munoz N, Meijer CJ, Shah KV (2002) The causal relation between human papillomavirus and cervical cancer. J Clin Pathol 55: 244–265
Bosch FX, Manos MM, Munoz N, Sherman M, Jansen AM, Peto J, Schiffman MH, Moreno V, Kurman R, Shah KV (1995) Prevalence of human papillomavirus in cervical cancer: a worldwide perspective. International biological study on cervical cancer (IBSCC) Study Group. J Natl Cancer Inst 87: 796–802
Clifford GM, Smith JS, Plummer M, Munoz N, Franceschi S (2003) Human papillomavirus types in invasive cervical cancer worldwide: a meta-analysis. Br J Cancer 88: 63–73
Grisaru D, Covens A, Chapman B, Shaw P, Colgan T, Murphy J, DePetrillo D, Lickrish G, Laframboise S, Rosen B (2001) Does histology influence prognosis in patients with early-stage cervical carcinoma? Cancer 92: 2999–3004
Gustafsson L, Ponten J, Zack M, Adami HO (1997) International incidence rates of invasive cervical cancer after introduction of cytological screening. Cancer Causes Control 8: 755–763
Hakulinen T, Abeywickrama KH (1985) A computer program package for relative survival analysis. Comput Programs Biomed 19: 197–207
Hemminki K, Li X, Mutanen P (2001) Age-incidence relationships and time trends in cervical cancer in Sweden. Eur J Epidemiol 17: 323–328
Hermanek P, Sobon LH (1987) TNM-Classification of Malignant Tumours. 4th revised edn. UICC International Union Against Cancer. Berlin: Springer Verlag
Hildesheim A, Hadjimichael O, Schwartz PE, Wheeler CM, Barnes W, Lowell DM, Willett J, Schiffman M (1999) Risk factors for rapid-onset cervical cancer. Am J Obstet Gynecol 180: 571–577
Hopkins MP, Morley GW (1991) A comparison of adenocarcinoma and squamous cell carcinoma of the cervix. Obstet Gynecol 77: 912–917
Lai CH, Hsueh S, Hong JH, Chang TC, Tseng CJ, Chou HH, Huang KG, Lin JD (1999) Are adenocarcinomas and adenosquamous carcinomas different from squamous carcinomas in stage IB and II cervical cancer patients undergoing primary radical surgery? Int J Gynecol Cancer 9: 28–36
Levi F, Lucchini F, Negri E, Franceschi S, la Vecchia C (2000) Cervical cancer mortality in young women in Europe: patterns and trends. Eur J Cancer 36: 2266–2271
Liu S, Semenciw R, Probert A, Mao Y (2001) Cervical cancer in Canada: changing patterns in incidence and mortality. Int J Gynecol Cancer 11: 24–31
Mitchell H, Medley G, Gordon I, Giles G (1995) Cervical cytology reported as negative and risk of adenocarcinoma of the cervix: no strong evidence of benefit. Br J Cancer 71: 894–897
Nakanishi T, Ishikawa H, Suzuki Y, Inoue T, Nakamura S, Kuzuya K (2000) A comparison of prognoses of pathologic stage Ib adenocarcinoma and squamous cell carcinoma of the uterine cervix. Gynecol Oncol 79: 289–293
Nieminen P, Kallio M, Hakama M (1995) The effect of mass screening on incidence and mortality of squamous and adenocarcinoma of cervix uteri. Obstet Gynecol 85: 1017–1021
Parkin DM, Nguyen-Dinh X, Day NE (1985) The impact of screening on the incidence of cervical cancer in England and Wales. Br J Obstet Gynaecol 92: 150–157
Pilch H, Gunzel S, Schaffer U, Tanner B, Brockerhoff P, Maeurer M, Hockel M, Hommel G, Knapstein PG (2001) The presence of HPV DNA in cervical cancer: correlation with clinico-pathologic parameters and prognostic significance: 10 years experience at the Department of Obstetrics and Gynecology of the Mainz University. Int J Gynecol Cancer 11: 39–48
Pirog EC, Kleter B, Olgac S, Bobkiewicz P, Lindeman J, Quint WG, Richart RM, Isacson C (2000) Prevalence of human papillomavirus DNA in different histological subtypes of cervical adenocarcinoma. Am J Pathol 157: 1055–1062
Quinn M, Babb P, Jones J, Allen E (1999) Effect of screening on incidence of and mortality from cancer of cervix in England: evaluation based on routinely collected statistics. BMJ 318: 904–908
Sasieni P, Adams J (1999) Effect of screening on cervical cancer mortality in England and Wales: analysis of trends with an age period cohort model. BMJ 318: 1244–1245
Sasieni P, Adams J (2001) Changing rates of adenocarcinoma and adenosquamous carcinoma of the cervix in England. Lancet 357: 1490–1493
Schwartz SM, Daling JR, Shera KA, Madeleine MM, McKnight B, Galloway DA, Porter PL, McDougall JK (2001) Human papillomavirus and prognosis of invasive cervical cancer: a population-based study. J Clin Oncol 19: 1906–1915
Sigurdsson K (1993) Effect of organized screening on the risk of cervical cancer. Evaluation of screening activity in Iceland, 1964–1991. Int J Cancer 54: 563–570
Stockton D, Cooper P, Lonsdale RN (1997) Changing incidence of invasive adenocarcinoma of the uterine cervix in East Anglia. J Med Screen 4: 40–43
van Ballegooijen M, Hermens R (2000) Cervical cancer screening in the Netherlands. Eur J Cancer 36: 2244–2246
Visser O, Coebergh JW, Otter R (1997) Gynaecological Tumours in the Netherlands 1989–1993. Utrecht: The Netherlands Cancer Registry
Visser O, Coebergh JW, Schouten LJ, van Dijck JAAM (2001) Incidence of cancer in the Netherlands 1997. Utrecht: Vereniging van Integrale Kankercentra
Vizcaino AP, Moreno V, Bosch FX, Munoz N, Barros-Dios XM, Borras J, Parkin DM (2000) International trends in incidence of cervical cancer: II. Squamous-cell carcinoma. Int J Cancer 86: 429–435
Walboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV, Snijders PJ, Peto J, Meijer CJ, Munoz N (1999) Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol 189: 12–19
Acknowledgements
We gratefully thank all registration clerks of the Amsterdam Cancer Registry for the collection of data. We thank FJ van Kemenade for helpful comments on this paper. This study was supported by Grant 2200.0089 from the Health Research & Development Council of The Netherlands (ZorgOnderzoek Nederland).
S Bulk, L Rozendaal, O Visser, RHM Verheijen and CJLM Meijer participated in the conception of the study. S Bulk wrote the report. O Visser was responsible for the data collection and statistical analyses. All investigators discussed findings and critically revised the paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Bulk, S., Visser, O., Rozendaal, L. et al. Incidence and survival rate of women with cervical cancer in the Greater Amsterdam area. Br J Cancer 89, 834–839 (2003). https://doi.org/10.1038/sj.bjc.6601157
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6601157
Keywords
This article is cited by
-
Management of Stage IIB Cervical Cancer: an Overview of the Current Evidence
Current Oncology Reports (2020)
-
Equity in human papilloma virus vaccination uptake?: sexual behaviour, knowledge and demographics in a cross-sectional study in (un)vaccinated girls in the Netherlands
BMC Public Health (2014)
-
Estimate of the global burden of cervical adenocarcinoma and potential impact of prophylactic human papillomavirus vaccination
BMC Cancer (2013)