Abstract
Background:
Knowing a young woman with newly diagnosed breast cancer has a germline BRCA1 mutation informs her clinical management and that of her relatives. We sought an optimal strategy for identifying carriers using family history, breast cancer morphology and hormone receptor status data.
Methods:
We studied a population-based sample of 452 Australian women with invasive breast cancer diagnosed before age 40 years for whom we conducted extensive germline mutation testing (29 carried a BRCA1 mutation) and a systematic pathology review, and collected three-generational family history and tumour ER and PR status. Predictors of mutation status were identified using multiple logistic regression. Areas under receiver operator characteristic (ROC) curves were estimated using five-fold stratified cross-validation.
Results:
The probability of being a BRCA1 mutation carrier increased with number of selected histology features even after adjusting for family history and ER and PR status (P<0.0001). From the most parsimonious multivariate model, the odds ratio for being a carrier were: 9.7 (95% confidence interval: 2.6–47.0) for trabecular growth pattern (P=0.001); 7.8 (2.7–25.7) for mitotic index over 50 mitoses per 10 high-powered field (P=0.0003); and 2.7 (1.3–5.9) for each first-degree relative with breast cancer diagnosed before age 60 years (P=0.01).The area under the ROC curve was 0.87 (0.83–0.90).
Conclusion:
Pathology review, with attention to a few specific morphological features of invasive breast cancers, can identify almost all BRCA1 germline mutation carriers among women with early-onset breast cancer without taking into account family history.
Similar content being viewed by others
Main
About 5–10% of young women diagnosed with breast cancer carry germline mutations in BRCA1 (Newman et al, 1998; Southey et al, 1999; Malone et al, 2000; Ozcelik et al, 2003). Knowing a woman's BRCA1 mutation status soon after the time of diagnosis is important because it could inform her immediate treatment choices, particularly with regard to breast conservation therapy vs mastectomy (Pierce et al, 2010), and perhaps in the future, her use of targeted therapies, such as Poly (ADP-ribose) polymerase inhibitors (Goodwin et al, 2007; Fong et al, 2009). Her mutation status is also important for her female relatives because a substantial proportion of these women will carry the same mutation and so will therefore be at high risk of breast and ovarian cancer (Antoniou et al, 2003) and will have different preventive and screening options than the general population.
What is the best approach to identify the BRCA1 mutation carriers among young women with newly diagnosed breast cancer, in terms of timeliness, sensitivity, specificity? Family history is difficult to collect well, especially in a busy clinical setting, in the context of a young woman newly diagnosed with breast cancer. In addition, the woman might not know her family cancer history details and gathering the relevant data and ensuring its accuracy might involve other family members, a process that can be time consuming. Even when accurately reported, well collected and verified cancer family history is often uninformative, unless extreme, as it is neither sensitive nor specific to BRCA1 mutation status. The areas under the receiver operator characteristic (ROC) curves for algorithms based on family history alone, such as BRCAPRO and BOADICEA, are at most 0.7–0.8 (e.g., Antoniou et al, 2008b). The odds of being a carrier increases on average by only a few fold for each first-degree relative with breast cancer (Ozcelik et al, 2003; Apicella et al, 2007) and given that the mutation frequency in the general population is about 1 in 600 (Antoniou et al, 2008a), it can be seen that family history must be extreme before the probability of being a carrier exceeds a nominal and historic testing threshold of 10% (Burke et al, 1997), let alone the newer UK benchmark of 20% (National Institute for Clinical Excellence, 2004). Even for the women with apparently strong family histories being tested by cancer genetics services, the great majority (>70%) are found to be non-carriers (Parmigiani et al, 2007; Antoniou et al, 2008b). Further, large proportions of the women who have been tested have had low a priori probability of being a carrier. For example, in a high-risk setting in the United States >40% of those tested were below the 10% threshold based on BRCAPRO (Parmigiani et al, 2007), and similar figures have been observed in the United Kingdom (Antoniou et al, 2008b).
It has been known for some time that there are particular morphological and histopathological features evident on tumour review that are more common in cancers arising in BRCA1 mutation carriers (Lakhani et al, 1998). These features have been identified by studying carriers across a wide range of ages at diagnosis who were ascertained because of their strong family cancer history. Lack of ER and PR expression have also been reported to improve prediction of BRCA1 mutation status based on family history (Lakhani et al, 2002; James et al, 2006; Mavaddat et al, 2010). To date, no validated algorithm appears to have been developed based on all of these predictive features, let alone using a population-based series of early-onset breast cancers.
Our aim was to devise a practical strategy that could be applied at the time of diagnosis for identifying, with high sensitivity and specificity, those young women with early-onset breast cancer who have the highest probability of carrying a germline mutation in BRCA1. We used morphological and immunohistochemical data that could be routinely collected at diagnosis, as well as data on family history of breast cancer in first- and second-degree relatives.
Participants and Methods
Australian Breast Cancer Family Registry
The Australian Breast Cancer Family Registry (ABCFR) includes a population-based, case–control–family study of breast cancer, in which cases and controls (probands) and their relatives were administered the same questionnaires, carried out in Melbourne and Sydney, Australia (Hopper et al, 1994, 1999; McCredie et al, 1998). It is a component of the international Breast Cancer Family Registry (John et al, 2004; Neuhausen et al, 2008). The study was approved by the ethics committees of The University of Melbourne and The Cancer Councils of Victoria and New South Wales. All participants provided written informed consent for participation in the study.
Family history data
For each family, a pedigree was constructed by interviewing the proband and all participating relatives, covering all known first- and second-degree adult relatives of the proband, their vital statuses, cancer histories, dates of birth and, if appropriate, dates of death and/or diagnosis. Consequently, reports of cancer in relatives came from multiple sources within the family, so that the pedigree information for each person was based on a self-report or report(s) from first-degree relatives and rarely was only on a report from a second-degree relative. Attempts were made to verify cancer reports using cancer registries, death certificates and other medical records (Dite et al, 2003). For probands, a strong family history was defined as having two or more first- or second-degree relatives diagnosed with breast or ovarian cancer (including male breast cancer) on the same side of the pedigree.
Tumour retrieval, pathology review and morphology score
We attempted to retrieve archival blocks for the first primary invasive breast tumours of all 856 probands diagnosed before the age of 40 years. A total of 452 tumours (53%) were retrieved and included material from 16 surgical biopsies, 7 spot/needle localisations, 309 lumpectomy/quadrantectomies, 167 mastectomies and 442 axillary dissections. The mean age at diagnosis for these retrieved cases was 35 years, as it was for the 856 probands. Histological type was recorded for 442 (98%) of the reviewed cases, the majority of the tumours were infiltrating ductal carcinomas (NOS) (83%). Atypical medullary (5%), classical medullary (1%), pleomorphic lobular (4%), classical lobular (2%) and other very rare histological types (tubular, cribiform, mucinous, secretory, metaplastic and alveolar lobular, 4%) made up the remainder.
These were scored for morphology features by a pathologist blind to the mutation status as described by Armes et al (1998) and Longacre et al (2006). Briefly, the tumours were typed into primary pattern and secondary pattern using the World Health Organisation breast carcinoma classification with minor modifications as described by Page et al (1987). Tumour grade was scored using the modified system of Bloom and Richardson by assessing mitotic rate, tubular differentiation and nuclear pleomorphism (Page et al, 1987).
We then selected nine features that have been reported to be associated with BRCA1 germline mutation status (Eisinger et al, 1996; Breast Cancer Linkage Consortium, 1997; Jóhannsson et al, 1997; Armes et al, 1998; Lakhani et al, 1998):
-
1)
Very high mitotic index defined here (see justification below) as >50 mitoses per 10 high-powered fields (h.p.f.). The mitotic index of each tumour was scored as: number of mitoses per 10 h.p.f.
-
2)
High nuclear grade (score of 3 for nuclear pleomorphism according to Elston (1987), which is scored as: (1) bland, (2) intermediate or (3) malignant (high)).
-
3)
Little or no tubule formation (score of 3 for tubule formation (<10%)) according to Elston (1987), which is scored as: (1) >75%, (2) 10–75% and (3) <10%).
-
4)
Trabecular growth pattern. Primary and secondary growth patterns are scored as: (1) acinar (organoid), (2) lobular, (3) trabecular and (4) tubular. Primary trabecular growth pattern was scored according to Ridolfi criteria for medullary cancers requiring >75% of the tumour to have a trabecular growth pattern (Ridolfi et al, 1977).
-
5)
Pushing margin, defined here as a continuous front of cells observed in >50% of the tumour circumference and scored as: (1) yes and (2) no.
-
6)
Circumscribed growth pattern scored as: (1) yes and (2) no.
-
7)
Syncytial growth pattern >75% scored as: (1) yes or (2) no.
-
8)
Necrosis scored as: absent or present; and
-
9)
Moderate or intense lymphocytic infiltrate, scored as: (1) absent/minimal, (2) moderate or (3) intense.
We generated a morphology score for each tumour by adding up the number of the following features that were present; high mitotic index, high nuclear grade, little or no tubule formation, trabecular growth pattern, pushing margin, circumscribed growth pattern, syncytial growth pattern, necrosis and a moderate or intense lymphocytic infiltrate, so that the score ranged from 0 to 9.
ER and PR status had been collected by the ABCFR for 402 (89%) of the 452 reviewed breast cancer cases. This information was collected from the state cancer registries (58%), diagnostic pathology reports (29%) and from immunohistochemical staining of tumour tissues (13%; Armes et al, 1998) as described in McCredie et al (1998).
BRCA1 mutation screening
For 788 (92%) of the probands, and for all 455 of the reviewed cases, previous BRCA1 mutation screening included:
-
1)
Protein truncation testing covering exon 11 of BRCA1 (Hopper et al, 1999).
-
2)
Manual sequencing of the coding and flanking intronic regions of BRCA1 for: (i) a random sample of 91 probands (Southey et al, 1999, ii) 63 probands with a strong family history of breast and/or ovarian cancer, (iii) 6 probands whose mothers had two primary breast cancers and (iv) 9 probands who had at least two or first- or second-degree relatives (maternal and paternal) with breast or ovarian cancer.
-
3)
Large genomic alteration screening of BRCA1 using multiplex ligation-dependent probe amplification (MLPA) as previously described (Smith et al, 2007) for groups (ii), (iii) and (iv) in (2) above.
-
4)
Testing for the two Ashkenazi founder mutations in BRCA1, 185delAG and 5238insC for all (Leong et al, 2000; Dite et al, 2003; Apicella et al, 2007).
-
5)
Testing for the duplication of exon 13 in BRCA1 for 641 probands as described previously (Puget et al, 1999; Leong et al, 2000).
Definition of pathogenicity for BRCA1 sequence variants was consistent with the policy of the Breast Cancer Information Core database (http://research.nhgri.nih.gov/bic/) and Neuhausen et al (2008). The above testing identified 39 pathogenic mutation carriers. The breast cancers arising in 29 (74%) of these carriers were retrieved and reviewed.
Statistical analysis
Associations between features were assessed by dichotomising and calculating corresponding odds ratios (ORs). Associations between the outcome, mutation status and potential predictors were estimated using simple and multiple logistic regression. The best fitting model was defined to be the one with the lowest Bayesian information criterion (BIC) (Schwarz, 1978) using observations with no missing data for any variable (N=400). P-values were based on the likelihood ratio test unless otherwise indicated and all calculations were performed using R version 2.7.2 (R Development Core Team, 2010).
The performance of the best fitting model was assessed using the same data set on which the model was fitted using a five-fold stratified cross-validation approach, as recommended by Kohavi (1995).
The predicted probability that a woman carries a BRCA1 mutation according to the best fitting model was calculated in the standard way as f(xTβ) where f is the logistic function given by f(L)=exp(L)/(1+exp(L)), β is the column matrix of maximum likelihood estimates, and x is the relevant part of the woman's column matrix of covariates. Asymptotic likelihood theory implies that β is normally distributed and allows estimation of its variance–covariance matrix Σ so it follows that xTβ is normally distributed with variance σ2=xTΣx. A 95% confidence interval (CI) for the predicted carrier probability, f(xTβ), was obtained by applying f to the limits, xTβ±1.96σ, for the predicted log-odds.
Results
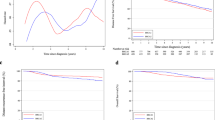
A total of 29 (6%) of the 452 probands whose tumours had undergone pathology review were found to be BRCA1 mutation carriers. The odds of being a carrier depended strongly on the morphology score, increasing on average by 80% (95% CI: 40–240%) with each additional feature after adjusting for family history and ER and PR status (P for trend <0.0001). Figure 1A shows that mutation carriers tended to have higher morphology scores than non-carriers; of the carriers, 27 (93%) had a morphology score of 5 or more compared with 25% of all probands. Figure 1B shows that, when restricted to probands with a strong family history, the distribution of the morphology score was bimodal. All 10 carriers with a strong family history also had a morphology score of 5 or more, and these carriers comprised 48% of all probands with a strong family history and a morphology score of 5 or more.
Table 1 shows that some characteristics of family history were associated with mutations status, but no family history feature alone was highly sensitive (maximum 41%) and all had low positive predictive values (<0.25%).
Table 1 also shows that, in contrast to family history features, most morphological features studied were individually predictive of BRCA1 mutation status, with four having smaller P-values than even the most significant family history feature. In general, the morphological features had high sensitivities (all but three>75%) and specificities (all but three⩾65%). Moderate or intense lymphocytic infiltrate, nuclear grade and little or no tubule formation had high sensitivities but low specificities while syncytial growth pattern, pushing margins and circumscribed growth pattern had high specificities but low sensitivities. The predictive features with crude OR>10 were: trabecular growth pattern, high mitotic index, and necrosis (sensitivity⩾79%, specificity⩾65%, positive predictive value 0.14–0.32).
Of the 452 tumours reviewed, 154 had mitotic indices between 0 and 9/10 h.p.f. and of these 1 (1%) was a BRCA1 mutation carrier, 115 had mitotic indices between 10 and 19/10 h.p.f and of these 1 (1%) was a BRCA1 mutation carrier, 111 had indices between 20 and 49/10 h.p.f. and of these 2 (2%) were BRCA1 mutation carriers and 72 had mitotic indices of 50 or more/10 h.p.f. (range 0–292/10 h.p.f.) and of these 25 (35%) were BRCA1 mutation carriers. A total of 74 tumours were scored to have primary trabecular growth pattern and 36 were scored to have a secondary trabecular growth pattern (all these 36 tumours were scored to have a primary acinar growth pattern).
ER and PR statuses were both individually predictive of mutation status, but while they had high sensitivities they did not have high specificities and alone their positive predictive values were each only 0.13. Being negative for both ER and PR was associated with an OR of 5.3 (95% CI: 2.3–13.0), sensitivity of 70%, specificity of 67% and positive and negative predictive values of 13 and 97%, respectively.
Figure 2 shows that the features within each of the three categories (family history, morphology and immunohistochemistry) were strongly associated with each other. The morphology features and ER and PR status were generally associated with each other but not with the family history features.
Levels of association between the features listed in Table 1. Each row and column corresponds to a feature (in the same order as in Table 1) and the shading represents different levels of odds ratios (ORs), as indicated in the figure. Odds ratios that were <1 were shaded the same as their reciprocals.
When models containing multiple features were considered, the best fitting model (as judged by BIC) included just three features. These features and their jointly estimated ORs (95% CI, Wald P-value) were: trabecular growth pattern, OR=9.7 (2.6–47.0; P=0.001); high mitotic index, OR=7.8 (2.7–25.7; P=0.0003); and number of first-degree relatives with breast cancer diagnosed before the age of 60 years, OR for each relative=2.7 (1.3–5.9; P=0.01). The area under the ROC curve for this model was 0.87 (95% CI: 0.83 to 0.90). The OR estimates for the two morphology features were negatively correlated with each other (r=−0.44) but neither was correlated with the OR estimate for family history (r=−0.04 and 0.09).
Table 2 shows cross-validation estimates of the areas under the ROC curves for models that included the most predictive features from one or more of the three categories of morphology, immunohistochemistry (comprising ER and PR receptor status) and family history. It is apparent from Table 2 that the morphology features have the greatest impact on the area under the ROC curve, and that models that include the morphology features are not improved by the addition of family history variables or ER and PR status.
Under the best fitting model, the probability that a woman diagnosed with breast cancer before age 40 years carries a BRCA1 mutation is exp(L)/[1+exp(L)] where the log-odds L is given by the formula L=−5.1544+2.0539 x+2.2750 y+0.9784 z and: x is 1 if the woman's tumour has high mitotic index and 0 otherwise; y is 1 if the woman's tumour has a trabecular growth pattern and 0 otherwise; and z is the number of the woman's first-degree relatives who have been diagnosed with breast cancer before the age of 60 years. A list of predicted probabilities for various values of x, y and z are given in Table 3.
The fit of the best model was not improved by more than could be attributed to chance by the addition of either ER and/or PR receptor status. After adjusting for the three variables in the best fitting model, the ORs (95% CI) associated with negative ER and PR receptor statuses were 1.8 (0.5–7.1) and 1.5 (0.6–4.4), respectively (both P=0.3).
Of the 58 probands whose tumours had both high mitotic index and trabecular growth pattern, 21 (36%) were BRCA1 mutation carriers. Of the 332 probands who had neither of these morphological features, only one (0.3%) was a carrier. Of the 123 who had one or both features, 28 were carriers, and this was associated with OR=98 (95% CI: 20–1750), sensitivity=97%, specificity=78% and positive predictive value=23%.
Of the 156 (34%) probands who had one or more of the three features high mitotic index, trabecular growth pattern and one or more first-degree relatives diagnosed with breast cancer before the age of 60 years, 28 (18%) were carriers. Of the 70 probands who had two or more of these three features, 24 (34%) were carriers.
Discussion
Our study has shown that, by considering just two tumour morphological features that could potentially be reported at the time of diagnostic pathology, and one aspect of family history of breast cancer, it is feasible to establish a simple way to identify those young women with breast cancer who are most likely to carry a BRCA1 germline mutation. Even if not supplemented by the information on family history, a trabecular growth pattern and a high mitotic index high were strong indicators of a woman's BRCA1 mutation status. Moreover, knowing ER and PR status did not improve the model predictions once the two morphology features and a family history variable were taken into account. In the context of breast cancers arising in young women, we found that any BRCA1 predictive value of these two measures appears to be subsumed by the two key morphological features. It would be of interest to know if this applied to breast cancers in women with later age at diagnosis.
For our population-based sample of women with early-onset breast cancer, if BRCA1 screening had been restricted to those with a strong family history then we would have screened 71 cases and found 10 carriers (14%). If instead we had screened those with a high mitotic index, we would still have screened 71 cases but found 23 carriers (32%), more than twice as many. If we also screened those with a trabecular growth pattern, we would have screened a further 53 cases and found another 5 carriers (10%). Therefore, screening those with high mitotic index and/or trabecular growth pattern would have found 28 BRCA1 mutation carriers in 124 women screened (24%) and missed only one carrier. Screening only one-quarter of early-onset cases based on just these two morphology features would have been sufficient to identify almost all carriers, without any reference to family history.
Table 2 shows the area under the ROC curve (AUC), an omnibus measure of a model's predictive power. Knowing family history in addition to the morphology features made no improvement in the AUC. The AUC based on family history alone was less than that based on ER and PR, and when used together was still less than the AUC based on the two key morphology features alone. In terms of predictive strength, the traditional indicators – measures of family history – were weaker than most of the morphological features. Our family history data are likely to be no less accurate and complete than family history data collected in a clinical setting.
This work has also identified a fascinating group of early-onset breast cancers that share the morphological features of early-onset breast cancers that carry identifiable BRCA1 mutations. These are the cancers, illustrated in Figure 1A, that have a morphology score of 5 or more but, despite extensive testing, are from women for whom we have not been able to identify germline BRCA1 mutations. We performed further BRCA1 mutation screening on DNA samples from the women whose tumours had mitotic indices over 50 per 10 h.p.f. and a trabecular growth pattern and who were not already known to carry a mutation in BRCA1 (n=37). (The mutation testing that had been performed on DNA from these women was varied because of the previous mutation testing strategy described above in the methods). A further two BRCA1 mutations, BRCA1 del1A-23 and BRCA1 delexon20, were identified by MLPA testing. The woman with the BRCA1 del1A-23 mutation had breast cancer diagnosed at the age of 33 years and a paternal grandmother with breast cancer diagnosed at age 71 years (verified). The women with the BRCA1 delexon20 mutation had a breast cancer diagnosed at the age of 31 at recruitment, and subsequently another at age 35 years, and had an unverified report of breast cancer in a paternal grandmother (age at diagnosis unknown).
Using tumours from multiple-case breast cancer families with on average later age at onset than in our series, Lakhani et al (1998 and 2002) carried out similar studies to ours to try to identify BRCA1 mutation carriers on the basis of pathology and immunohistochemistry. The ORs for prediction they found were somewhat lower than we observed for early-onset cases. This might be due to a potential change in morphological features associated with BRCA1 germline mutations in postmenopausal women that could be due to non-germline factors, such as oestrogens and methylation (both known to have a changing role with increasing age).
From our data and model fit, we have calculated the predicted probability of carrying a germline BRCA1 mutation based on the two morphology features and family history: see Table 3. It can be seen that 15% of our sample had predicted probabilities >10% (68 women in 7 categories). On the other hand, for the group of women who had none of the three predictive features, comprising 66% of our sample (299 women), the predicted probability was only 1%. This information could be clinically useful in helping decide where limited resources for counselling and mutation testing for BRCA1 carriers in women with early-onset breast cancer might best be directed.
Therefore, our data suggest that is possible to institute a pathology-based and more sensitive and specific method for prioritising women with early-onset breast cancer for BRCA1 mutation testing, similar to that which already applies to colorectal cancer and the DNA mismatch repair genes (Boland et al, 1998; Vasen et al, 1999; Southey et al, 2005; Lenz, 2005; Mead et al, 2007). We intend to undertake an independent study to further improve our algorithms, and we encourage others to try to validate and extend this approach, especially to later-onset disease. Pathology review, with attention to a few specific morphological features of invasive breast cancers, can identify almost all BRCA1 germline mutation carriers among women with early-onset breast cancer without taking into account family history.
Change history
29 March 2012
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Antoniou AC, Cunningham AP, Peto J, Evans DG, Lalloo F, Narod SA, Risch HA, Eyfjord JE, Hopper JL, Southey MC, Olsson H, Johannsson O, Borg A, Pasini B, Radice P, Manoukian S, Eccles DM, Tang N, Olah E, Anton-Culver H, Warner E, Lubinski J, Gronwald J, Gorski B, Tryggvadottir L, Syrjakoski K, Kallioniemi OP, Eerola H, Nevanlinna H, Pharoah PD, Easton DF (2008a) The BOADICEA model of genetic susceptibility to breast and ovarian cancers: updates and extensions. Br J Cancer 98 (8): 1457–1466
Antoniou AC, Hardy R, Walker L, Evans DG, Shenton A, Eeles R, Shanley S, Pichert G, Izatt L, Rose S, Douglas F, Eccles D, Morrison PJ, Scott J, Zimmern RL, Easton DF, Pharoah PD (2008b) Predicting the likelihood of carrying a BRCA1 or BRCA2 mutation: validation of BOADICEA, BRCAPRO, IBIS, Myriad and the Manchester scoring system using data from UK genetics clinics. J Med Genet 45 (7): 425–431
Antoniou A, Pharoah PD, Narod S, Risch HA, Eyfjord JE, Hopper JL, Loman N, Olsson H, Johannsson O, Borg A, Pasini B, Radice P, Manoukian S, Eccles DM, Tang N, Olah E, Anton-Culver H, Warner E, Lubinski J, Gronwald J, Gorski B, Tulinius H, Thorlacius S, Eerola H, Nevanlinna H, Syrjäkoski K, Kallioniemi OP, Thompson D, Evans C, Peto J, Lalloo F, Evans DG, Easton D (2003) Average risks of breast and ovarian cancer associated with BRCA1 or BRCA2 mutations detected in case series unselected for family history: a combined analysis of 22 studies. Am J Hum Genet 72 (5): 1117–1130
Apicella C, Dowty JG, Dite GS, Jenkins MA, Senie RT, Daly MB, Andrulis IL, John EM, Buys SS, Li FP, Glendon G, Chung W, Ozcelik H, Miron A, Kotar K, Southey MC, Foulkes WD, Hopper JL (2007) Validation study of the LAMBDA model for predicting the BRCA1 or BRCA2 mutation carrier status of North American Ashkenazi Jewish women. Clin Genet 72: 87–97
Armes JE, Egan AJ, Southey MC, Dite GS, McCredie MR, Giles GG, Hopper JL, Venter DJ (1998) The histologic phenotypes of breast carcinoma occurring before age 40 years in women with and without BRCA1 or BRCA2 germline mutations: a population-based study. Cancer 83 (11): 2335–2345
Boland CR, Thibodeau SN, Hamilton SR, Sidransky D, Eshleman JR, Burt RW, Meltzer SJ, Rodriguez-Bigas MA, Fodde R, Ranzani GN, Srivastava S (1998) A National Cancer Institute Workshop on Microsatellite Instability for cancer detection and familial predisposition: development of international criteria for the determination of microsatellite instability in colorectal cancer. Cancer Res 58 (22): 5248–5257
Breast Cancer Linkage Consortium (1997) Pathology of familial breast cancer: differences between breast cancer in carriers of BRCA1 or BRCA2 mutations and sporadic cases. Lancet 349 (9064): 1505–1510
Burke W, Daly M, Garber J, Botkin J, Kahn MJ, Lynch P, McTiernan A, Offit K, Perlman J, Petersen G, Thomson E, Varricchio C (1997) Recommendations for follow-up care of individuals with an inherited predisposition to cancer. II. BRCA1 and BRCA2. Cancer Genetics Studies Consortium. JAMA 277 (12): 997–1003
Dite GS, Jenkins MA, Southey MC, Hocking JS, Giles GG, McCredie MR, Venter DJ, Hopper JL (2003) Familial risks, early-onset breast cancer, and BRCA1 and BRCA2 germline mutations. J Natl Cancer Inst 95 (6): 448–457
Eisinger F, Stoppa-Lyonnet D, Longy M, Kerangueven F, Noguchi T, Bailly C, Vincent-Salomon A, Jacquemier J, Birnbaum D, Sobol H (1996) Germ line mutation at BRCA1 affects the histoprognostic grade in hereditary breast cancer. Cancer Res 56 (3): 471–474
Elston CW (1987) Grading of invasive carcinoma of the breast. In: Page DL, Anderson TJ (eds) Diagnostic Histopathology of the Breast, pp 300–311. Churchill Livingstone: Edinburgh
Fong PC, Boss DS, Yap TA, Tutt A, Wu P, Mergui-Roelvink M, Mortimer P, Swaisland H, Lau A, O’Connor MJ, Ashworth A, Carmichael J, Kaye SB, Schellens JH, de Bono JS (2009) Inhibition of poly(ADP-ribose) polymerase in tumours from BRCA mutation carriers. N Engl J Med 361 (2): 123–134
Goodwin PJ, Phillips KA, West DW (2007) Prognosis of breast cancer in carriers of BRCA1 and BRCA2 mutations. N Engl J Med 357 (15): 1555
Hopper JL, Giles GG, McCredie MR, Boyle P (1994) Background, rationale and protocol for a case-control-family study of breast cancer. Breast 3 (2): 79–86
Hopper JL, Southey MC, Dite GS, Jolley DJ, Giles GG, McCredie MR, Easton DF, Venter DJ (1999) Population-based estimate of the average age-specific cumulative risk of breast cancer for a defined set of protein truncating mutations in BRCA1 and BRCA2. Cancer Epidemiol Biomarkers Prev 8 (9): 741–747
James PA, Doherty R, Harris M, Mukesh BN, Milner A, Young MA, Scott C (2006) Optimal selection of individuals for BRCA mutation testing: a comparison of available methods. J Clin Oncol 24 (4): 707–715
Jóhannsson OT, Idvall I, Anderson C, Borg A, Barkardóttir RB, Egilsson V, Olsson H (1997) Tumour biological features of BRCA1-induced breast and ovarian cancer. Eur J Cancer 33 (3): 362–371
John EM, Hopper JL, Beck JC, Knight JA, Neuhausen SL, Senie RT, Ziogas A, Andrulis IL, Anton-Culver H, Boyd N, Buys SS, Daly MB, O’Malley FP, Santella RM, Southey MC, Venne VL, Venter DJ, West DW, Whittemore AS, Seminara D, Breast Cancer Family Registry. (2004) The breast cancer family registry: an infrastructure for cooperative multinational, interdisciplinary and translational studies of the genetic epidemiology of breast cancer. Breast Cancer Res 6 (4): R375–R389
Kohavi R (1995) A study of cross-validation and bootstrap for accuracy estimation and model selection. In Proceedings of the Fourteenth International Joint Conference on Artificial Intelligence. Morgan Kaufmann, San Francisco, pp 1137–1143
Lakhani SR, Jacquemier J, Sloane JP, Gusterson BA, Anderson TJ, van de Vijver MJ, Farid LM, Venter D, Antoniou A, Storfer-Isser A, Smyth E, Steel CM, Haites N, Scott RJ, Goldgar D, Neuhausen S, Daly PA, Ormiston W, McManus R, Scherneck S, Ponder BA, Ford D, Peto J, Stoppa-Lyonnet D, Bignon YJ, Struewing JP, Spurr NK, Bishop DT, Klijn JG, Devilee P, Cornelisse CJ, Lasset C, Lenoir G, Barkardottir RB, Egilsson V, Hamann U, Chang-Claude J, Sobol H, Weber B, Stratton MR, Easton DF (1998) Multifactorial analysis of differences between sporadic breast cancers and cancers involving BRCA1 and BRCA2 mutations. J Natl Cancer Inst 90 (15): 1138–1145
Lakhani SR, Van De Vijver MJ, Jacquemier J, Anderson TJ, Osin PP, McGuffog L, Easton DF (2002) The pathology of familial breast cancer: predictive value of immunohistochemical markers estrogen receptor, progesterone receptor, HER-2, and p53 in patients with mutations in BRCA1 and BRCA2. J Clin Oncol 20 (9): 2310–2318
Lenz HJ (2005) First Amsterdam, then Bethesda, now Melbourne? J Clin Oncol 23 (27): 6445–6449 Editorial
Leong T, Whitty J, Keilar M, Mifsud S, Ramsay J, Birrell G, Venter D, Southey M, McKay M (2000) Mutation analysis of BRCA1 and BRCA2 cancer predisposition genes in radiation hypersensitive cancer patients. Int J Radiat Oncol Biol Phys 48 (4): 959–965
Longacre TA, Ennis M, Quenneville LA, Bane AL, Bleiweiss IJ, Carter BA, Catelano E, Hendrickson MR, Hibshoosh H, Layfield LJ, Memeo L, Wu H, O’malley FP (2006) Interobserver agreement and reproducibility in classification of invasive breast carcinoma: an NCI breast cancer family registry study. Mod Pathol 19 (2): 195–207
Malone KE, Daling JR, Neal C, Suter NM, O’Brien C, Cushing-Haugen K, Jonasdottir TJ, Thompson JD, Ostrander EA (2000) Frequency of BRCA1/BRCA2 mutations in a population-based sample of young breast carcinoma cases. Cancer 88 (6): 1393–1402
Mavaddat N, Rebbeck TR, Rebbeck TR, Lakhani SR, Easton DF, Antoniou AC (2010) Incorporating tumour pathology information into breast cancer risk prediction algorithms. Breast Cancer Res 12 (3): R28
McCredie MR, Dite GS, Giles GG, Hopper JL (1998) Breast cancer in Australian women under the age of 40. Cancer Causes Control 9 (2): 189–198
Mead LJ, Jenkins MA, Young J, Royce SG, Smith L, St John DJ, Macrae F, Giles GG, Hopper JL, Southey MC (2007) Microsatellite instability markers for identifying early-onset colorectal cancers caused by germ-line mutations in DNA mismatch repair genes. Clin Cancer Res 13 (10): 2865–2869
National Institute for Clinical Excellence (2004) Clinical guideline 14. Familial breast cancer: the classification and care of women at risk of familial breast cancer in primary, secondary and tertiary care. Ref Type: Report
Neuhausen SL, Ozcelik H, Southey MC, John EM, Godwin AK, Chung W, Iriondo-Perez J, Miron A, Santella RM, Whittemore A, Andrulis IL, Buys SS, Daly MB, Hopper JL, Seminara D, Senie RT, Terry MB (2008) BRCA1 and BRCA2 mutation carriers in the Breast Cancer Family Registry: an open resource for collaborative research. Breast Cancer Res Treat 116 (2): 379–386
Newman B, Mu H, Butler LM, Millikan RC, Moorman PG, King MC (1998) Frequency of breast cancer attributable to BRCA1 in a population-based series of American women. JAMA 279 (12): 915–921
Ozcelik H, Knight JA, Glendon G, Yazici H, Carson N, Ainsworth PJ, Taylor SA, Feilotter H, Carter RF, Boyd NF, Andrulis IL (2003) Individual and family characteristics associated with protein truncating BRCA1 and BRCA2 mutations in an Ontario population based series from the Cooperative Family Registry for Breast Cancer Studies. J Med Genet 40 (8): e91
Page DL, Anderson TJ, Sakamoto G (1987) Infiltrating carcinoma: major histological types. In: Page DL, Anderson TJ (eds) Diagnostic Histopathology of the Breast, pp 193–235. Churchill Livingstone: Edinburgh
Parmigiani G, Chen S, Iversen Jr ES, Friebel TM, Finkelstein DM, Anton-Culver H, Ziogas A, Weber BL, Eisen A, Malone KE, Daling JR, Hsu L, Ostrander EA, Peterson LE, Schildkraut JM, Isaacs C, Corio C, Leondaridis L, Tomlinson G, Amos CI, Strong LC, Berry DA, Weitzel JN, Sand S, Dutson D, Kerber R, Peshkin BN, Euhus DM (2007) Validity of models for predicting BRCA1 and BRCA2 mutations. Ann Intern Med 147 (7): 441–450
Pierce LJ, Phillips KA, Griffith KA, Buys S, Gaffney DK, Moran MS, Haffty BG, Ben-David M, Kaufman B, Garber JE, Merajver SD, Balmaña J, Meirovitz A, Domchek SM (2010) Local therapy in BRCA1 and BRCA2 mutation carriers with operable breast cancer: comparison of breast conservation and mastectomy. Breast Cancer Res Treat 121 (2): 389–398
Puget N, Sinilnikova OM, Stoppa-Lyonnet D, Audoynaud C, Pagès S, Lynch HT, Goldgar D, Lenoir GM, Mazoyer S (1999) An Alu-mediated 6-kb duplication in the BRCA1 gene: a new founder mutation? Am J Hum Genet 64 (1): 300–302
R Development Core Team (2010). R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing: Vienna, Austria
Ridolfi RL, Rosen PP, Port A, Kinne D, Miké V (1977) Medullary carcinoma of the breast: a clinicopathologic study with 10 year follow-up. Cancer 40 (4): 1365–1385
Schwarz GE (1978) Estimating the dimension of a model. Ann Statist 6 (2): 461–464
Smith LD, Tesoriero AA, Ramus SJ, Dite G, Royce SG, Giles GG, McCredie MR, Hopper JL, Southey MC (2007) BRCA1 promoter deletions in young women with breast cancer and a strong family history: a population-based study. Eur J Cancer 43 (5): 823–827
Southey MC, Tesoriero AA, Andersen CR, Jennings KM, Brown SM, Dite GS, Jenkins MA, Osborne RH, Maskiell JA, Porter L, Giles GG, McCredie MR, Hopper JL, Venter DJ (1999) BRCA1 mutations and other sequence variants in a population-based sample of Australian women with breast cancer diagnosed before the age of 40. Br J Cancer 79 (1): 34–39
Southey MC, Jenkins MA, Mead L, Whitty J, Grubb G, St John DJB, Macrae F, Young J, Barker M, Walsh M, Royce SG, Jass J, Giles GG, Hopper JL (2005) Use of molecular tumor characteristics to prioritize mismatch repair gene testing in early-onset colorectal cancers. J Clin Oncol 23 (27): 6524–6532
Vasen HF, Watson P, Mecklin JP, Lynch HT (1999) New clinical criteria for hereditary nonpolyposis colorectal cancer (HNPCC, Lynch syndrome) proposed by the International Collaborative group on HNPCC. Gastroenterology 116 (6): 1453–1456
Acknowledgements
The Australian Breast Cancer Family Registry was supported by the National Health and Medical Research Council of Australia, the New South Wales Cancer Council, the Victorian Health Promotion Foundation (Australia) and the National Cancer Institute, National Institutes of Health under RFA-CA-06–503 and through cooperative agreements with members of the Breast Cancer Family Registry (CFR) and PIs. The University of Melbourne (U01 CA69638) contributed data to this study. The content of this paper does not necessarily reflect the views or the policies of the National Cancer Institute or any of the collaborating centres in the CFR, nor does mention of trade names, commercial products or organisations imply endorsement by the US Government or the CFR. We extend our thanks to the many women and their families who generously participated in the Australian Breast Cancer Family Registry and consented to us accessing their pathology material. We also thank the many study staff who made this work possible, the study Pathologists, Jane Armes, Deon Venter, Elena Provenzano, Sarbar Napaki and Beena Kumar, who worked to review and score the material presented in the study and Veronika Gazdik and Simon Royce for their expert technical support. JLH is a National Health and Medical Research Council Australia Fellow. MCS is a National Health and Medical Research Council Senior Research Fellow. JLH and MCS are both group leaders of the Victoria Breast Cancer Research Consortium. KAP is the Cancer Council Victoria Dr John Colebatch Clinical Research Fellow.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Southey, M., Ramus, S., Dowty, J. et al. Morphological predictors of BRCA1 germline mutations in young women with breast cancer. Br J Cancer 104, 903–909 (2011). https://doi.org/10.1038/bjc.2011.41
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2011.41
Keywords
This article is cited by
-
Loss of BRCA1 expression and morphological features associated with BRCA1 promoter methylation status in triple-negative breast cancer
Journal of Human Genetics (2021)
-
Heritable DNA methylation marks associated with susceptibility to breast cancer
Nature Communications (2018)
-
Performing and Declining PGD: Accounts of Jewish Israeli Women Who Carry a BRCA1/2 Mutation or Partners of Male Mutation Carriers
Journal of Genetic Counseling (2017)
-
Refined histopathological predictors of BRCA1 and BRCA2mutation status: a large-scale analysis of breast cancer characteristics from the BCAC, CIMBA, and ENIGMA consortia
Breast Cancer Research (2014)
-
Impact of recent parity on histopathological tumor features and breast cancer outcome in premenopausal Japanese women
Breast Cancer Research and Treatment (2013)