Abstract
Background:
Adjuvant therapy increases disease-free survival in endometrial cancer (EC), but has no impact on overall survival and negatively influences the quality of life. We investigated the discriminatory power of classical and immunological predictors of recurrence in a cohort of EC patients and confirmed the findings in an independent validation cohort.
Methods:
We reanalysed the data from 355 EC patients and tested our findings in an independent validation cohort of 72 patients with EC. Predictors were selected and Harrell’s C-index for concordance was used to determine discriminatory power for disease-free survival in the total group and stratified for histological subtype.
Results:
Predictors for recurrence were FIGO stage, lymphovascular space invasion and numbers of cytotoxic and memory T-cells. For high risk cancer, cytotoxic or memory T-cells predicted recurrence as well as a combination of FIGO stage and lymphovascular space invasion (C-index 0.67 and 0.71 vs 0.70). Recurrence was best predicted when FIGO stage, lymphovascular space invasion and numbers of cytotoxic cells were used in combination (C-index 0.82). Findings were confirmed in the validation cohort.
Conclusions:
In high-risk EC, clinicopathological or immunological variables can predict regional or distant recurrence with equal accuracy, but the use of these variables in combination is more powerful.
Similar content being viewed by others
Main
Endometrial cancer (EC) is the most common gynaecological cancer in the western world, with yearly over 8500 new cases in the UK alone (Cancer Research UK, 2014). A distinction can be made between low- and high-risk EC based on histological parameters (Bokhman, 1983; Hecht and Mutter, 2006; Evans et al, 2011). Low-risk EC comprises grade 1–2 endometrioid neoplasms and is most common. High-risk EC includes non-endometrioid and high-grade endometrioid neoplasms. Although high-risk EC accounts for just 10% of new cases, it is responsible for more than 40% of deaths from EC (Amant et al, 2005; Evans et al, 2011; Boll et al, 2012). Molecular studies describe distinct molecular pathways involved in pathogenesis and suggest that low and high-risk EC are manifestations of two different diseases (Lax, 2007; Samarnthai et al, 2010; Matias-Guiu and Prat, 2013).
There is a clear need to better predict recurrence and disease-free survival (DFS) in order to optimise patient-tailored treatment, especially in high-risk EC. The mainstay of treatment is hysterectomy and bilateral salpingo-oophorectomy (Amant et al, 2005; Wright et al, 2012) with or without pelvic and para-aortic lymphadenectomy. Adjuvant radiotherapy is advised depending on age, depth of myometrial invasion, tumour grade and the presence of lymphovascular space involvement (LVSI) (Creutzberg et al, 2000; ASTEC study group et al, 2009; Nout et al, 2010; Kong et al, 2012; Salvesen et al, 2012; Wright et al, 2012). This reduces locoregional recurrence from 15 to 5% but has no impact on overall survival and is associated with considerable toxicity in a substantial proportion of patients. For patients with advanced and/or high-grade disease, chemotherapy reduces recurrence outside the pelvis by 5%, but has no effect on survival (Johnson et al, 2011).
Many studies show a relationship between tumour-infiltrating lymphocytes (TILs) and cancer behaviour (Kondratiev et al, 2004; Chang et al, 2005; Galon et al, 2006; de Jong et al, 2009; Leffers et al, 2009; Gooden et al, 2011; Schreiber et al, 2011; Vesely et al, 2011). In a cohort of 90 EC patients, Kondratiev et al (2004) described that low numbers of cytotoxic T cells (CTLs) was related to poor prognosis (hazard ratio (HR) 2.79). A favourable effect of high numbers of CTLs on progression-free and overall survival in EC patients was confirmed by staining for CD8-positive cells with a HR for survival of 0.48 (95% confidence interval 0.26–0.89) (de Jong et al, 2009). de Jong et al (2009) also described a strong relation with recurrence for the ratio between CD8-positive cytotoxic T cells and FoxP3-positive regulatory T cells with a HR of 0.44 (95% confidence interval 0.23–0.84). The downregulated expression of classical major histocompatibility complex class I by EC cells also correlates with the risk of recurrence (Bijen et al, 2010).
In colorectal cancer, an immune score based on TILs has been shown to better predict recurrence compared with standard TNM classification (Galon et al, 2006; Pages et al, 2009; Bindea et al, 2011; Fridman et al, 2011; Mlecnik et al, 2011). The use of TILs as a predictor of colorectal cancer, together with an already established relation of TIL with disease course, has prompted us to investigate these immunological variables and their value in predicting EC recurrence. We examined this possibility by re-analysing existing data and validated our findings in an independent cohort of high-risk EC patients.
Patients and methods
Patients
For this study, a new analysis was performed on data pooled from two previous studies (de Jong et al, 2009; Bijen et al, 2010). This initial study cohort comprised a consecutive series of 355 EC patients treated at a single institution in the Netherlands between 1984 and 2004 (de Jong et al, 2009; Bijen et al, 2010). Patients with a previous malignancy or radiotherapy prior to surgery were excluded. Patients received standard care, undergoing hysterectomy followed by adjuvant radiotherapy as stipulated by local and international guidelines. (Creutzberg et al, 2000; ASTEC study group et al, 2009; Nout et al, 2010; Kong et al, 2012; Oncoline, 2014). Sections were reviewed by an experienced Gynaecologic Pathologist (HH) and classified according to the WHO criteria. Low-risk EC was defined as grade 1–2 endometrioid cancer. High-risk EC was defined as grade 3 or undifferentiated endometrioid cancer or non-endometrioid cancer. Owing to the retrospective character of this study, staging according to FIGO 1988 classification was used. Follow-up visits were performed for a period of 5 years, in accordance with local practice. During each follow-up visit, clinical history was updated and a physical examination was performed. Data were accrued until September 2011 and entered into a password-protected database. Patient identity was protected by study specific patient numbers. According to Dutch legislation, no further approval by an Institutional Review Board approval was necessary.
Our validation cohort comprised an international series of 106 high-risk patients selected for grade 3 with deep invasion, advanced stage or serous or clear cell EC. These patients were included from 1985 to 2013 and underwent treatment in Manchester (UK), London (UK), Villejuif (FR), Leiden (NL) and Groningen (NL), and were selected as a pilot series in the international TransPORTEC collaboration (Stelloo et al, 2015). To avoid overlapping cases across the two study cohorts, patients from the Groningen centre were excluded, leaving 72 cases for the validation cohort. Clinical follow-up was accrued on all patients in the validation cohort until September 2014.
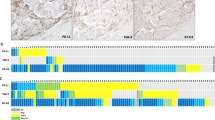
Immunohistochemistry
Details of the staining procedure and the antibodies used in the initial study cohort were described previously (de Jong et al, 2009, Bijen et al, 2010). In brief, tissue microarrays were constructed by transferring three core biopsies of 0.6 mm diameter from representative areas of tumour centre to a pre-defined location in a recipient paraffin block. Sections of 4 μm were cut from these blocks and stained using the antibodies summarised in Supplementary Table 1. CD8 was used as a marker for cytotoxic T cells, CD45R0 as a marker for memory T cells and FoxP3 as a marker for regulatory T cells. Major histocompatibility complex class 1 expression was stained using antibodies for a wide range of major histocompatibility complex class 1 heavy chains. Antigen–antibody reactions for FoxP3 was visualised with NovaRED (Vector Laboratories, Burlingame, CA, USA) and with 3,3′-diaminobenzidine in all other cases. Tumours were evaluated if more than 20% of at least two cores consisted of tumour material. Slides were scored by two independent observers, blinded for patient characteristics and outcome. Discrepancies were resolved by consensus. Tumour-infiltrating cells per core were counted and findings were dichotomised using the median as a cut-off. We choose to use the median because an optimal threshold is unknown. In studies on prediction of recurrence in colorectal cancer, the median was also used as a cut-off (Galon et al, 2006; Pages et al, 2009; Bindea et al, 2011; Fridman et al, 2011; Mlecnik et al, 2011). As for the ratio of cytotoxic/regulatory T-cells, there is also no consensus on an optimal threshold. In a previous study, the median value for the ratio showed a strong relation with survival and we therefore maintained the median as a cut-off (de Jong et al, 2009). In line with previous publications, CD45RO+ cells were classified as either present or not present. For scoring of HLA expression a semiquantative scale as described in literature was used to categorise expression into normal, partial loss or loss of expression (Rolland et al, 2007; Bijen et al, 2010). Tissue microarrays have been used in previous histological studies on EC. Fons et al (2007) showed a high concordance for protein expression with full slide sections. Concordance for immunological markers was also evaluated for the previous to the study by de Jong et al (2009).
For the validation cohort, tissue microarrays were constructed in a similar manner. Sections used for staining CD8 were pre-treated with Ultra CC1 for 52 min at 95 °C. Staining for CD45R0 and CD8 was performed automatically with Ventana BenchMark ULTRA IHC/ISH Staining Module according to the manufacturer’s instructions (Ventana Medical Systems Inc., Roche Group, Tucson, AZ, USA). Scoring was again carried out by two independent observers, blinded for patient characteristics. Discrepancies were resolved by consensus. Examples of staining for CTLs are shown in Figure 1.
Statistical analysis
Disease-free survival (DFS) was defined as time until regional or distant recurrence. Local recurrence was not considered an event because radiotherapy reduces the local recurrence rate and the indication for radiotherapy is based upon clinicopathological parameters. Disease-specific survival (DSS) was defined as time until death of disease. Although DFS was the main objective in this analysis, we also performed an analysis on DSS for comparison. Because not all cores were suitable for scoring, missing values for immunological variables varied between 14.4 and 19.2%. Therefore, missing values for all immunological variables were imputed based on correlation structure. Myometrial invasion, FIGO stage, LVSI, nodal status, tumour grade, histological type, age and immunological variables were used as predictors (five imputations). To assess the impact of the imputations on the results, the analysis was also carried out on the complete cases.
To analyse relations between clinicopathological and immunological variables, Chi-square tests or Fishers’ exact tests were used. For survival analysis, log rank test and Cox regression analysis were performed. To identify predictors for DFS, variables were selected if these had a previously reported relationship with disease course. The following variables were considered: age, FIGO stage, LVSI, myometrial invasion, grade, histological type, HLA-class 1 expression, presence of CD45R0+ cells, high/low numbers of CD8+ cells and high/low ratio CD8+/Foxp3+ cells. Survival analysis was performed and HRs with a 95% confidence interval were estimated. Predictors for further analysis were selected from the candidate predictors through backward elimination. To this end, a multivariate Cox regression analysis for DFS was performed using all candidate predictors. The least significant variable was left out in the subsequent Cox regression analysis, and the analysis was repeated until only significant variables remained (P<0.05). Backward selection was performed to build a model including only clinicopathological variables, as well as a model including only immunological variables, as well as a model combining both groups of variables. These analyses were performed with SPSS (v20, IBM statistics, Chicago, IL, USA).
To assess the discriminatory power of the three models, Harrell’s concordance index (C-index) (Harrell et al, 1996) was calculated for each model, using STATA (v 11, Statacorp LP, College Station, TX, USA). This was calculated for the entire cohort and separately for low/high-risk EC as well as for endometrioid/non-endometrioid and low(1–2)/high(3)-grade subgroups. A C-index close to 0.5 indicates low predictive power and a C-index closer to 1.0 indicates increasing discriminatory power. In the final step, the three models were applied to the validation cohort and again the C-index was calculated.
Results
Baseline characteristics, stratified for low/high-risk EC, are shown in Table 1. The distribution of variables in the imputed dataset was not different from the original cohort dataset. The relative efficiency of imputation for both cohorts varied between 0.97 and 1.00, indicating that more imputations would not contribute to a more reliable analysis. Median follow-up time was 6.0 years for the initial study cohort and 2.2 years for the validation cohort. Median age at diagnosis was 64 and 65, respectively, for low/high-risk EC and 69 in the validation cohort. Patients from the initial study cohort with high-risk EC presented more frequently with unfavourable clinicopathological findings: advanced FIGO stage (chi2=53.0; df=3; P=0.000), deep myometrial invasion (chi2=22.2; df=1; P=0.000), LVSI (chi2=42.3; df=1; P=0.000) and positive lymph nodes (chi2=4.9; df=1; P=0.027), compared with those with low-risk EC. Patients with high-risk EC were also more likely to receive adjuvant radiotherapy (chi2=19.6; df=1; P=0.000). Significantly, more patients received adjuvant chemotherapy in the validation cohort compared with high-risk patients in the study cohort. Immunological findings in the initial study cohort show that a ratio of cytotoxic/regulatory T-cells above the median was seen more often in low-risk EC compared with high-risk EC (55.8% vs 38.5%, respectively (chi2=10.0; df=1; P=0.002). Memory T-cells were present in 62.3% of low-risk and 54.1% of high-risk EC (chi2=3.7; df=1; P=0.056). There was no significant difference in HLA class 1 expression or number of CTLs between low- and high-risk EC. Immunological findings were similar in the validation cohort. Survival is shown in Table 2. In the initial study cohort, disease recurred in 32% of patients with high-risk EC and in 21% of low-risk EC (chi2=5.4; df=1; P=0.020). The location of recurrence showed a similar pattern in both low- and high-risk EC. Almost all patients with recurrence of high risk died during follow-up. Overall, 44% of patients with high-risk EC died of disease during follow-up vs 25% of patients with low-risk EC (chi2=16.9; df=1; P=0.000). For the validation cohort, clinicopathological and immunological findings as well as survival was not significantly different from the high-risk subgroup from the initial study cohort.
Backward selection of clinicopathological variables resulted in FIGO stage and LVSI as independent predictors for DFS. In backward selection of immunological variables, only high/low numbers of CTLs remained significant. Analysis of both clinicopathological and immunological variables resulted in the presence of memory cells, FIGO stage and LVSI as predictors for DFS. The HR and discriminatory power for DFS of the selected variables for the entire cohort are shown in Table 3. Disease-free survival is best predicted by FIGO and LVSI combined (C-index 0.81). Addition of either immunological variable (CTLs or memory cells) to this combination did not improve the discriminatory power (C-index 0.83). The discriminatory power of either CTLs or memory T-cells alone as a predictor of recurrence or death was low in the total cohort (C-index of 0.60 and 0.61, respectively).
Results after stratification for low/high-risk EC are shown in Table 4. In low risk, FIGO and LVSI were the best predictors for DFS and addition of either CTLs or memory T cells did not improve the discriminatory power. However, in high-risk EC, DFS is best predicted by FIGO and LVSI combined with CTLs (Table 4, C-index 0.79). A combination of clinicopathological variables with the presence of memory T cells also performs well (C-index 0.76). Separately, the discriminatory power of either immunological variable was similar to that of FIGO and LVSI combined (C-index of 0.71 vs 0.70).
C-index for the subgroups low- vs high-grade EC and endometrioid vs non-endometrioid EC was similar to the combination of these subgroups in low- vs high-risk EC. In both high-grade and non-endometrioid EC, DFS was best predicted by a combination of FIGO and LVSI with CTLs (C-index 0.80 vs 0.85, respectively).
For comparison, DSS was also analysed and showed a similar pattern (data not shown). In high-risk EC, clinicopathological variables performed similarly to either CTLs or memory T cells (C-index 0.63 vs 0.64–0.68). The combination of FIGO, LVSI and CTLs had the highest predictive accuracy for survival (C-index 0.72). Both presence of memory T cells and low numbers of CTLs contribute to the prediction of DSS (data not shown).
Table 5 shows HRs and the C-index for the validation cohort. The discriminatory power of CTLs below/above the median in the validation cohort equalled that of advanced FIGO stage and LVSI combined (C-index 0.71). The combination increased the discriminatory power (C-index 0.79) confirming the results of the initial study cohort. Furthermore, findings in the subgroup analysis of low- vs high-grade EC (C-index 0.84) and endometrioid vs non-endometrioid EC (C-index 0.80) was similar to low- vs high-risk EC (data not shown).
Figure 2 represents DFS in the validation cohort and confirms the finding in previous studies that a high number of CTLs is related to a favourable disease course. Figure 3 is a boxplot illustrating the distribution of CTLs for patients from the validation cohort, with and without an event in DFS. There was one recurrence out of 19 patients with a CTL count above 50.
Without imputation, and using only cases with all variables complete, the datasets contained 257 and 54 cases for the study and validation cohort, respectively. Results were similar to that of the imputed dataset. Cytotoxic T cells performed well as a predictor for regional and distant recurrence in the high-risk study cohort and the validation cohort (C-index 0.71 and 0.74, respectively). Combination with FIGO stage and LVSI again increased the predictive power with a C-index of 0.80 in the high-risk study cohort and 0.83 in the validation cohort.
Discussion
Immunological parameters may be useful to select patients with high-risk EC for adjuvant therapy. Low numbers of CTLs is equivalent to FIGO stage and LVSI combined for predicting regional and distant recurrence or death from disease in type 2 EC. A model that combines all three parameters has the highest predictive power in high-risk EC.
Currently, the selection of patients for adjuvant treatment depends on age, depth of myometrial invasion and histological subtype (Creutzberg et al, 2000; ASTEC study group et al, 2009; Nout et al, 2010; Kong et al, 2012). Our data support the role of FIGO stage and LVSI in decision-making. Age was not selected in backward selection and we therefore cannot confirm the role of age in decision-making. Cytotoxic T cells could contribute to decision-making in order to reduce the number of patients receiving adjuvant treatment while at the adjuvant radiotherapy with its associated toxicity, whilst at the same time keeping the risk of recurrence as low as possible. Furthermore, a model that accurately predicts distant recurrence could indicate which patient should additionally receive adjuvant chemotherapy, rather than radiotherapy alone.
In theory, a high discriminatory power of CTLs and memory T cells could be explained by the involvement of immune system in the development and progression of cancer. The immune system can eliminate tumours by killing of cancer cells (Schreiber et al, 2011; Vesely et al, 2011). However, in doing so, a selection of tumour cells will survive by escaping immune surveillance. The presence of memory and especially CTLs may reflect a functional immune response capable of eradication of tumour cells. This immune response consists of a chain of events from antigen presentation and recognition to tumour infiltration and destruction of cancer cells. Tumour infiltration by CTLs and memory T cells indicates that previous steps in the immune response were successful.
Predicting recurrence using immunological variables is a relatively new concept. In colorectal cancer, an immunological prediction model has shown promising results (Galon et al, 2006; Pages et al, 2009; Bindea et al, 2011; Fridman et al, 2011; Mlecnik et al, 2011). A score derived from number of intratumoural cytotoxic and memory T cells had a concordance index of 0.65 for DFS and 0.66 for DSS in colorectal cancer, which was higher than that of TNM classification. To our knowledge, we are the first to explore the possibility of an immune prediction score for recurrence in EC. Similarly to what has been shown in colorectal cancer, CTLs and, to a lesser extent, memory T cells are the best predictors for recurrence in our study. We used the median number of cytotoxic cells per core as the cut-off for distinguishing low and high CTL density, as was previously described by Galon et al (2006) in colorectal cancer (Pages et al, 2009; Bindea et al, 2011; Fridman et al, 2011; Mlecnik et al, 2011). However, this cut-off is arbitrary and may not be the optimal threshold for predicting disease recurrence. With a higher cut-off point, discriminatory power for no recurrence will increase. The boxplot (Figure 3) shows that there were only a few recurrences for patients with a high CTL count. In fact, there was only one recurrence in the 21 cases with a count above 50. Of these 21 patients, 18 had an indication for adjuvant radiotherapy. These data do exemplify that patients with a high number of CTLs may be better off without adjuvant radiotherapy. Future studies are needed to determine the optimal threshold.
We specifically evaluated TIL and HLA-class 1 expression as possible predictors in EC. Other immunological variables such as PD1 were not evaluated but may also contribute in patient selection. We performed immunofluorescent staining for PD1 in sections of EC as part of another study but were unable to confirm a relation to survival. Nonetheless, it might be useful to examine a possible contribution of other immunological variables in patient selection.
Radiotherapy reduces local recurrence and is advised for patients with a high-risk profile based on clinicopathological variables, and this could be a confounding factor in our study. As patients in our cohorts were treated accordingly, fewer local recurrences were seen, as expected, in those patients who received radiotherapy. We therefore excluded local recurrence when defining DFS. We are aware that this may cause a selection bias if local recurrence is related to distant recurrence. Future work should include similar cohorts of patients treated in randomised trials of radiotherapy and/or adjuvant chemotherapy.
Here, we describe an innovative statistical approach to establish which immunological predictors can select patients for adjuvant treatment. A multivariate Cox regression analysis was used to select relevant predictors from a pool of candidate predictors. This analysis also provides the relative risk of recurrence in HRs, but gives no information on how well a variable or combination of variables can discriminate between recurrence or no recurrence. The discriminatory power of selected clinicopathological and immunological variables was assessed by calculating a C-index, where a C-index close to 1 is indicative of a strong discrimination between recurrence and no recurrence, and the resultant C-index can also be used to determine the quality of a model.
There are several issues to address in the statistical approach. For example, missing data can be problematic in developing a model and several methods have been described to deal with missing values (Royston et al, 2009). In this study, we choose to impute for missing values because of limitations caused by alternative approaches. The high relative efficiency in our imputation (0.97–1.00) suggests a high concordance between the five imputations. Alternatively, missing values could be ignored or deleted. However, this would result in the loss of significance and possibly to incorrect estimates of discriminatory power. Also, in our approach, the best predictors were selected by first including all variables and then selecting the best model using backward selection. The advantage of this approach is that the information of the correlation structure between the variables is used in the selection of variables. Another possibility would have been to select the most significant variables from univariate analysis and take these forward into the multivariate analysis. However, selecting variables by significance testing allows for a selection bias and over fitting of a model. Furthermore, including all variables may result in an impractical model (Royston et al, 2009).
We used as our initial study cohort a large, consecutive case series previously described and subsequently updated to include up to 6 years of follow-up (de Jong et al, 2009; Bijen et al, 2010). Two studies have already described a relationship between immunological variables and disease course. Over fitting may occur when these variables are subsequently tested for prediction of recurrence. Results were therefore tested in an independent, international validation cohort of patients collected in the TransPORTEC collaboration with high-risk EC. Clinicopathological findings in this cohort were similar to the study cohort except for a lower number of patients receiving adjuvant chemotherapy in the latter. Possibly, this reflects an international difference in pattern of care between institutions. The validation cohort confirms the findings from our initial study cohort and agrees with previously published studies in EC (Kondratiev et al, 2004; Chang et al, 2005; de Jong et al, 2009; Gooden et al, 2011). Presence of memory T cells and high numbers of CTLs in the tumour relates to DFS and DSS. The discriminatory power of high/low numbers of CTLs was similar in both the study and validation cohorts.
In conclusion, here, we describe for the first time a prospective statistical approach to select immunological variables as predictors of recurrence in EC. In high-risk EC, recurrence was best predicted by a combination of FIGO stage and LVSI in addition to cytotoxic or memory T-cell numbers. The discriminatory power of both cytotoxic and memory T cells should be confirmed in a larger cohort, preferably from a randomised controlled trial of high-risk EC.
Change history
01 September 2015
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Amant F, Cadron I, Fuso L, Berteloot P, de Jonge E, Jacomen G, Van Robaeys J, Neven P, Moerman P, Vergote I (2005) Endometrial carcinosarcomas have a different prognosis and pattern of spread compared to high-risk epithelial endometrial cancer. Gynecol Oncol 98 (2): 274–280.
ASTEC study group,, Blake P, Swart AM, Orton J, Kitchener H, Whelan T, Lukka H, Eisenhauer E, Bacon M, Tu D, Parmar MK, Amos C, Murray C, Qian W (2009) Adjuvant external beam radiotherapy in the treatment of endometrial cancer (MRC ASTEC and NCIC CTG EN.5 randomised trials): pooled trial results, systematic review, and meta-analysis. Lancet 373 (9658): 137–146.
Bijen CB, Bantema-Joppe EJ, de Jong RA, Leffers N, Mourits MJ, Eggink HF, van der Zee AG, Hollema H, de Bock GH, Nijman HW (2010) The prognostic role of classical and nonclassical MHC class I expression in endometrial cancer. Int J Cancer 126 (6): 1417–1427.
Bindea G, Mlecnik B, Fridman WH, Galon J (2011) The prognostic impact of anti-cancer immune response: a novel classification of cancer patients. Semin Immunopathol 33 (4): 335–340.
Bokhman JV (1983) Two pathogenetic types of endometrial carcinoma. Gynecol Oncol 15 (1): 10–17.
Boll D, Verhoeven R, van der Aa MA, Pauwels P, Karim-Kos HE, Coebergh JW, van Doorn HC (2012) Incidence and survival trends of uncommon corpus uteri malignancies in the Netherlands, 1989-2008. Int J Gynecol Cancer 22 (4): 599–606.
Cancer Research UK (2014) Cancer Research UK. Available at: http://www.cancerresearchuk.org/cancer-info/cancerstats/types/uterus/ Accessed 15 September 2014.
Chang WC, Huang SC, Torng PL, Chang DY, Hsu WC, Chiou SH, Chow SN, Sheu BC (2005) Expression of inhibitory natural killer receptors on tumor-infiltrating CD8+ T lymphocyte lineage in human endometrial carcinoma. Int J Gynecol Cancer 15 (6): 1073–1080.
Creutzberg CL, van Putten WL, Koper PC, Lybeert ML, Jobsen JJ, Warlam-Rodenhuis CC, De Winter KA, Lutgens LC, van den Bergh AC, van de Steen-Banasik E, Beerman H, van Lent M (2000) Surgery and postoperative radiotherapy versus surgery alone for patients with stage-1 endometrial carcinoma: multicentre randomised trial. PORTEC Study Group. Post Operative Radiation Therapy in Endometrial Carcinoma. Lancet 355 (9213): 1404–1411.
de Jong RA, Leffers N, Boezen HM, ten Hoor KA, van der Zee AG, Hollema H, Nijman HW (2009) Presence of tumor-infiltrating lymphocytes is an independent prognostic factor in type I and II endometrial cancer. Gynecol Oncol 114 (1): 105–110.
Evans T, Sany O, Pearmain P, Ganesan R, Blann A, Sundar S (2011) Differential trends in the rising incidence of endometrial cancer by type: data from a UK population-based registry from 1994 to 2006. Br J Cancer 104 (9): 1505–1510.
Fons G, Hasibuan SM, van der Velden J, ten Kate FJ (2007) Validation of tissue microarray technology in endometrioid cancer of the endometrium. J Clin Pathol 60 (5): 500–503.
Fridman WH, Galon J, Pages F, Tartour E, Sautes-Fridman C, Kroemer G (2011) Prognostic and predictive impact of intra- and peritumoral immune infiltrates. Cancer Res 71 (17): 5601–5605.
Galon J, Costes A, Sanchez-Cabo F, Kirilovsky A, Mlecnik B, Lagorce-Pages C, Tosolini M, Camus M, Berger A, Wind P, Zinzindohoue F, Bruneval P, Cugnenc PH, Trajanoski Z, Fridman WH, Pages F (2006) Type, density, and location of immune cells within human colorectal tumors predict clinical outcome. Science 313 (5795): 1960–1964.
Gooden MJ, de Bock GH, Leffers N, Daemen T, Nijman HW (2011) The prognostic influence of tumour-infiltrating lymphocytes in cancer: a systematic review with meta-analysis. Br J Cancer 105 (1): 93–103.
Harrell FE Jr, Lee KL, Mark DB (1996) Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med 15 (4): 361–387.
Hecht JL, Mutter GL (2006) Molecular and pathologic aspects of endometrial carcinogenesis. J Clin Oncol 24 (29): 4783–4791.
Johnson N, Bryant A, Miles T, Hogberg T, Cornes P (2011) Adjuvant chemotherapy for endometrial cancer after hysterectomy. Cochrane Database Syst Rev 10 (10): CD003175.
Kondratiev S, Sabo E, Yakirevich E, Lavie O, Resnick MB (2004) Intratumoral CD8+ T lymphocytes as a prognostic factor of survival in endometrial carcinoma. Clin Cancer Res 10 (13): 4450–4456.
Kong A, Johnson N, Kitchener HC, Lawrie TA (2012) Adjuvant radiotherapy for stage I endometrial cancer. Cochrane Database Syst Rev 4: CD003916.
Lax SF (2007) Molecular genetic changes in epithelial, stromal and mixed neoplasms of the endometrium. Pathology 39 (1): 46–54.
Leffers N, Gooden MJ, de Jong RA, Hoogeboom BN, ten Hoor KA, Hollema H, Boezen HM, van der Zee AG, Daemen T, Nijman HW (2009) Prognostic significance of tumor-infiltrating T-lymphocytes in primary and metastatic lesions of advanced stage ovarian cancer. Cancer Immunol Immunother 58 (3): 449–459.
Matias-Guiu X, Prat J (2013) Molecular pathology of endometrial carcinoma. Histopathology 62 (1): 111–123.
Mlecnik B, Tosolini M, Kirilovsky A, Berger A, Bindea G, Meatchi T, Bruneval P, Trajanoski Z, Fridman WH, Pages F, Galon J (2011) Histopathologic-based prognostic factors of colorectal cancers are associated with the state of the local immune reaction. J Clin Oncol 29 (6): 610–618.
Nout RA, Smit VT, Putter H, Jurgenliemk-Schulz IM, Jobsen JJ, Lutgens LC, van der Steen-Banasik EM, Mens JW, Slot A, Kroese MC, van Bunningen BN, Ansink AC, van Putten WL, Creutzberg CL PORTEC Study Group (2010) Vaginal brachytherapy versus pelvic external beam radiotherapy for patients with endometrial cancer of high-intermediate risk (PORTEC-2): an open-label, non-inferiority, randomised trial. Lancet 375 (9717): 816–823.
Oncoline guidelines, cancer clinical practice guidelines, the Netherlands. (2014) Available at: http://www.oncoline.nl/endometriumcarcinoom Accessed 15 October 2014.
Pages F, Kirilovsky A, Mlecnik B, Asslaber M, Tosolini M, Bindea G, Lagorce C, Wind P, Marliot F, Bruneval P, Zatloukal K, Trajanoski Z, Berger A, Fridman WH, Galon J (2009) In situ cytotoxic and memory T cells predict outcome in patients with early-stage colorectal cancer. J Clin Oncol 27 (35): 5944–5951.
Rolland P, Deen S, Scott I, Durrant L, Spendlove I (2007) Human leukocyte antigen class I antigen expression is an independent prognostic factor in ovarian cancer. Clin Cancer Res 13 (12): 3591–3596.
Royston P, Moons KG, Altman DG, Vergouwe Y (2009) Prognosis and prognostic research: Developing a prognostic model. BMJ 338: b604.
Salvesen HB, Haldorsen IS, Trovik J (2012) Markers for individualised therapy in endometrial carcinoma. Lancet Oncol 13 (8): e353–e361.
Samarnthai N, Hall K, Yeh IT (2010) Molecular profiling of endometrial malignancies. Obstet Gynecol Int 2010: 162363.
Schreiber RD, Old LJ, Smyth MJ (2011) Cancer immunoediting: integrating immunity's roles in cancer suppression and promotion. Science 331: 1565–1570.
Stelloo E, Bosse T, Nout RA, MacKay HJ, Church DN, Nijman HW, Leary A, Edmondson RJ, Powell ME, Crosbie EJ, Kitchener HC, Mileshkin L, Pollock PM, Smit VT, Creutzberg CL (2015) ‘Refining prognosis and identifying targetable pathways for high-risk endometrial cancer; a TransPORTEC initiative. Mod Pathol 28: 836–844.
Vesely MD, Kershaw MH, Schreiber RD, Smyth MJ (2011) Natural innate and adaptive immunity to cancer. Annu Rev Immunol 29: 235–271.
Wright JD, Barrena Medel NI, Sehouli J, Fujiwara K, Herzog TJ (2012) Contemporary management of endometrial cancer. Lancet 379 (9823): 1352–1360.
Acknowledgements
Research Support: We acknowledge the contribution Claudia Bijen and Renske de Jong to the previous studies of our initial study cohort. We acknowledge all members of the TransPORTEC consortium (www.msbi.nl/transportec) in their contribution to the validation cohort.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License.
Supplementary Information accompanies this paper on British Journal of Cancer website
Supplementary information
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Versluis, M., de Jong, R., Plat, A. et al. Prediction model for regional or distant recurrence in endometrial cancer based on classical pathological and immunological parameters. Br J Cancer 113, 786–793 (2015). https://doi.org/10.1038/bjc.2015.268
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2015.268
Keywords
This article is cited by
-
Prognostic implications of tumor-infiltrating T cells in early-stage endometrial cancer
Modern Pathology (2022)
-
Circulating tumor DNA as a prognostic marker in high-risk endometrial cancer
Journal of Translational Medicine (2021)
-
Pten and Dicer1 loss in the mouse uterus causes poorly differentiated endometrial adenocarcinoma
Oncogene (2020)
-
Endometrioid endometrial cancer “recurring” as high-grade serous adenocarcinoma in the inguinal lymph nodes in a patient with germline MLH1 mutated Lynch syndrome: consequence or coincidence?
Hereditary Cancer in Clinical Practice (2019)