Abstract
Background:
Observational studies have associated adiposity with an increased risk of colorectal cancer (CRC). However, such studies do not establish a causal relationship. To minimise bias from confounding we performed a Mendelian randomisation (MR) analysis to examine the relationship between adiposity and CRC.
Methods:
We used SNPs associated with adult body mass index (BMI), waist-hip ratio (WHR), childhood obesity and birth weight as instrumental variables in a MR analysis of 9254 CRC cases and 18 386 controls.
Results:
In the MR analysis, the odds ratios (ORs) of CRC risk per unit increase in BMI, WHR and childhood obesity were 1.23 (95% CI: 1.02–1.49, P=0.033), 1.59 (95% CI: 1.08–2.34, P=0.019) and 1.07 (95% CI: 1.03–1.13, P=0.018), respectively. There was no evidence for association between birth weight and CRC (OR=1.22, 95% CI: 0.89–1.67, P=0.22). Combining these data with a concurrent MR-based analysis for BMI and WHR with CRC risk (totalling to 18 190 cases, 27 617 controls) provided increased support, ORs for BMI and WHR were 1.26 (95% CI: 1.10–1.44, P=7.7 × 10−4) and 1.40 (95% CI: 1.14–1.72, P=1.2 × 10−3), respectively.
Conclusions:
These data provide further evidence for a strong causal relationship between adiposity and the risk of developing CRC highlighting the urgent need for prevention and treatment of adiposity.
Similar content being viewed by others
Main
Colorectal cancer (CRC) is a major public health problem in economically developed countries (Forman et al, 2014). Migration and epidemiological studies have established that diet and other lifestyle factors have a major role in the aetiology of CRC (Haggar and Boushey, 2009). Among the lifestyle factors that have an impact on CRC risk, high body mass index (BMI) has generally been reported to be associated with an increased risk in observational studies (Bianchini et al, 2002; Bardou et al, 2013), with some evidence for a stronger influence being shown for men (Pan et al, 2004; Moghaddam et al, 2007). There is also evidence for an inverse relationship between adiposity at a young age and cancer development (Carpenter et al, 2003; Yang et al, 2014). The association between BMI and CRC in these observational studies does not, however, necessarily establish a causal relationship. Specifically, these studies cannot entirely exclude the possibility of the observed association being the consequence of confounding factors, such as socio-economic status, alcohol and other lifestyle factors (Moghaddam et al, 2007), whereas some studies have failed to exclude the possibility of reverse causation (Smith and Ebrahim, 2003).
An alternative to a traditional observational epidemiology study is the Mendelian randomisation (MR) approach. The strategy of MR uses genetic markers known to be associated with a potential risk factor in the assessment of its effect on another trait or disease (Lawlor et al, 2008). These markers, or instrumental variables (IV), rely on a number of assumptions, namely that the IVs are solely associated with the trait or disease, and the IVs are independent of confounders. This methodology permits the nature of the relation between the risk factor and the trait or disease to be assessed without the limitations present within observational studies, such as confounding factors, and importantly establish whether an association is causal. A further attribute of MR is the avoidance of the influence of factors whose effect may be time sensitive, for example weight loss being a consequence of CRC. Thus, an IV has the potential to more accurately assess lifetime exposure when compared with measurements of potential risk factors recorded in an observational study.
In the present study we examined, using MR, the impact of four metrics of adiposity on the risk of developing CRC. The adiposity traits we considered were adult BMI, adult waist-hip ratio (WHR), childhood obesity and birth weight.
Materials and methods
CRC GWAS data sets
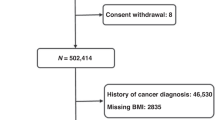
Our MR analysis was based on data from seven previously reported genome-wide association studies (GWAS) of CRC (Orlando et al, 2016). Briefly, these GWAS were all based on individuals with European ancestry and comprise: CCFR1 (1290 cases, 1055 controls), CCFR2 (796 cases, 2236 controls), COIN (2244 cases, 2162 controls), FINLAND (1172 cases, 8266 controls), UK1 (940 cases, 965 controls), Scotland1 (1012 cases, 1012 controls) and VQ58 (1800 cases, 2690 controls). Details of the genotyping, quality control and imputation of untyped single-nucleotide polymorphisms (SNPs) genotypes have been previously published. Summary statistics from the GWAS were used to calculate the ratio estimates for the adiposity-related SNPs.
Instrumental variables
For each of four adiposity traits (adult BMI, adult WHR, childhood obesity and birth weight), we used data from recent GWAS of individuals of European-decent for each trait. Specifically for adult BMI, we used data from the Genetic Investigation of Anthropometric Traits (GIANT) consortium, which was based on an analysis of up to 339 224 individuals (Locke et al, 2015). For the WHR, data were obtained from a meta-analysis comprising 61 studies, made up of up to 190 803 individuals (Heid et al, 2010). For childhood obesity, data was obtained from 2480 children with extreme obesity and 7370 controls (Wheeler et al, 2013). Birth weight data was obtained from up to 69 308 individuals from 43 studies (Horikoshi et al, 2013).
We used SNPs that were declared genome-wide significant (i.e., P⩽5.0 × 10−8) in these GWAS as IVs. From the 97 adult BMI-associated SNPs (kg m−2) as identified by Locke et al (2015), we confined the analysis to 76 SNPs that were found in European populations, and were separated by at least 500 kb. In addition, we used 14 SNPs for WHR as reported by Heid et al (2010); nine SNPs reported by Wheeler et al (2013), which were associated with childhood obesity (>3 s.d. from the mean of the BMI distribution); and the seven SNPs reported by Horikoshi et al (2013), which were associated with birth weight (kg) (Supplementary Table 1). None of these studies reported non-additive effects of the SNPs on the adiposity trait, hence per allele effects were considered additive. For each of the four adiposity traits we extracted the effect estimates and associated P-values of each SNP from the seven CRC GWAS.
Statistical analysis
We performed MR analysis to assess the association between each adiposity trait and CRC using summary statistics from the CRC GWAS, and the published effect size of the adiposity-related trait on CRC. As per Burgess et al (2015) the combined ratio estimate  of all SNPs associated with a particular adiposity trait on CRC risk was calculated under a fixed-effects model:
of all SNPs associated with a particular adiposity trait on CRC risk was calculated under a fixed-effects model:

Xk corresponds to the association between SNP k with the adiposity trait and Yk is the association between SNP k and CRC risk with standard error  . The standard error of the combined ratio estimate is approximately given by
. The standard error of the combined ratio estimate is approximately given by

We used MR-Egger and inverse weighted variance regression to examine for violation (e.g., from pleiotopy) of the standard IV assumptions in our analysis (Bowden et al, 2015). All analyses were performed using R software (R Development Core Team, Vienna, Austria) and we considered a P-value of <0.05 as significant.
Meta-analysis with published studies
An overlapping concurrent study has recently been published which has also reported an MR analysis to estimate the causal association between adiposity and CRC risk (Thrift et al, 2015). The study was based on the analysis of 10 226 CRC cases and 10 286 controls from 11 GWAS, including the CCFR1 study, reporting on the impact of adult BMI and WHR on CRC. The genetic risk score for these two adiposity traits in this study and in our analysis was based on the same set of SNPs. Hence, to enhance our power to establish a relationship between genetically defined adiposity and CRC risk, we performed a meta-analysis of our study and this published study pooling summary estimates of effect size under a fixed-effects model, avoiding duplication of the CCFR1 study.
Results
In six of the seven CRC GWAS there was a positive relationship between BMI-increasing alleles and CRC risk (Figure 1). From the pooled analysis we identified an odds ratio (OR) of 1.23 in risk of CRC per kg m−2 increase of BMI (95% confidence interval (CI): 1.02–1.49, P=0.033, test for heterogeneity between studies I2=0%, Phet=0.70).
MR results of adiposity traits on CRC risk from seven GWAS studies and the meta-analysis.
(A) Adult BMI; (B) adult WHR; (C) childhood obesity (CO); and (D) birth weight (BW). Boxes denote OR point estimates, with their areas proportional to the inverse variance weight of the estimate. Horizontal lines represent 95% CIs. The diamond represents the summary Ors, computed under a fixed-effects model, with 95% CI given by the width of the diamond. The unbroken vertical line is at the null value (OR=1.0).
Although the relationship between WHR and childhood obesity with CRC was less consistent between studies than for BMI in the pooled analysis, we also identified a correlation between both adiposity traits and CRC risk (Figure 1). For each unit increase in WHR we observed an OR of 1.59 in CRC risk (95% CI: 1.08–2.34, P=0.019 test for heterogeneity across studies I2=45%, Phet=0.09). For childhood obesity the OR for CRC was 1.07 (95% CI: 1.01–1.13, P=0.018, test for heterogeneity between studies I2=0%, Phet=0.61). In contrast to the relationship between BMI, WHR, and childhood obesity and CRC we observed no association with birth weight and risk (P=0.22, Figure 1).
Using both MR-Egger and IVW regression tests we did not detect violation of the standard IV assumptions in our MR analysis of BMI, WHR, childhood obesity or birth weight for CRC risk (Supplementary Figure 1, Supplementary Table 2).
The strongest reported SNP associations for BMI are provided by rs1558902 (FTO) and rs13021737 (TMEM18), which have a well-established impact on obesity (Frayling et al, 2007; Rohde et al, 2014). To examine if our findings of a correlation between BMI and CRC risk were primarily driven by these variants we performed a sensitivity analysis excluding these SNPs. The MR results remain statistically significant, albeit slightly less profound (OR=1.24, 95% CI: 1.01–1.51, P=0.035). The association between each of the adiposity-related SNP and CRC risk is shown in Supplementary Figure 1.
Given there is correlation between measures of adiposity (Serdula et al, 1993) we examined the specificity of each trait on CRC risk by repeating our analysis omitting SNPs if there were overlapping loci. With the exception of adult BMI and childhood obesity which share four associated loci FTO (rs1558902, rs1421085), MC4R (rs6567160, rs476828), TMEM18 (rs13021737, rs12463617) and NEGR1 (rs3101336) all of the adiposity-related SNPs are distinct. Omitting these overlapping SNPs from our MR analysis still provided evidence for a correlation between adult BMI and childhood obesity with CRC risk, albeit less significant than before (OR=1.23, 95% CI: 1.00–1.51, P=0.049 and OR=1.10, 95% CI: 1.02–1.20, P=0.019, respectively).
To explore if there were gender-specific associations for CRC for each of the four adiposity traits, we performed a stratified analysis of our data set. Although an increasing number of risk alleles for each trait was associated with an increased CRC in both men and women, only the relationship between adult WHR and CRC in men remained statistically significant (Supplementary Table 3; OR=2.13, 95% CI: 1.18–3.87, P=0.013).
In the meta-analysis combining these results with the data from Thrift et al (2015), adult BMI was associated with an OR of 1.26 for CRC risk (95% CI: 1.10–1.44, P=7.7 × 10−4) and adult WHR an OR of 1.40 for CRC risk (95% CI: 1.14–1.72, P=1.2 × 10−3; Table 1). Although the association between genetically influenced adult BMI was only significant in women (ORs in females and males were 1.43, 95% CI: 1.17–1.74, P=4.3 × 10−4 and 1.12, 95% CI: 0.92–1.38, P=0.26, respectively) and the WHR association was only significant for men (ORs in males and females were 1.63, 95% CI: 1.20–2.22, P=2.0 × 10−3 and 1.22, 95% CI: 0.91–1.63, P=0.18, respectively) these differences were not statistically different (P-values for difference were 0.09 and 0.18, respectively).
Discussion
In this study we have shown correlations between IVs for adult BMI, WHR and childhood obesity, and CRC risk. Even adjusting for multiple testing the correlations between IVs for adult BMI and WHR remained significant. The absence of data on childhood obesity in the study reported by Thrift et al (2015), precluded meta-analysis of this metric of adiposity. We did not identify a relationship between the IVs for birth weight and CRC. Although this is less likely to be a determinant of CRC risk per se, we acknowledge that our power to demonstrate a relationship was limited. Indeed, even the IVs for adult BMI we used explain ∼3% of the total phenotypic variation in BMI (Locke et al, 2015).
A possible explanation for a failure to demonstrate a significant correlation between genetic BMI and CRC risk could be that the distribution of body fat is a more important predictor of CRC risk in men rather than total body adiposity. Support for this postulate is that in men WHR has been reported to be superior in predicting CRC than BMI in observational studies. In our MR-based analysis we indeed found that WHR was associated with CRC in men but not in women. Given that the genetic risk score for WHR is derived from SNPs associated with WHR, which are adjusted for BMI, suggests that fat distribution may be important for CRC risk for men, whereas overall obesity is more important for CRC risk for women.
There is evidence that adiposity may have a more significant effect on the development of colon rather than rectal cancer. Given that the landscape of colonic and rectal cancers show differences relating IVs to molecular features is likely to be informative in terms of understanding disease aetiology (Yamauchi et al, 2012). Unfortunately the data sets on which our study has been based did not enable such analysis to be performed.
An important strength of our analysis is that by implementing an MR-based analysis we have avoided the potential biases in observational studies of factors such as recall bias and confounding. The combined ratio estimates of the impact of adiposity on CRC risk hold provided the marker is independent of factors that may confound the relationship between adiposity and CRC. The findings from our analysis are however reliant on a number of key assumptions. First, that the IVs are solely associated with CRC through its association with adiposity rather than pleiotropism, which would be seen by a departure from linearity of the relationship between SNPs and their effect size for adiposity and CRC. We did not observe such a relationship between CRC and adiposity risk SNPs. Second, the IV is independent of factors that confound observational associations. To date there is currently no evidence that the IVs we used are associated with factors that might confound adiposity CRC associations in conventional analyses. The generation of substantive IVs for highly complex traits is a major limitation of the MR-based strategy to investigate the aetiological basis of diseases like cancer.
Accepting these caveats our study findings can be viewed as quantifying the causal effect of adiposity on CRC risk. Moreover, they generally support previously published observational studies and provide further evidence for adiposity being a major risk factor for the development of CRC.
In the pooled analysis, genetically influenced BMI showed only a statistically significant association with CRC in women. This finding is discordant with observational studies which have generally found a stronger correlation in men. It is possible that some estimates from observational studies may have been biased toward the null if heavier women under-report their weight. Indeed it is noteworthy that this specific finding from the meta-analysis is primarily driven by data from Thrift et al (2015), hence independent replication is required.
The biological mechanism by which adiposity increases CRC risk remains to be established and several mechanisms have been variously suggested as explaining the correlation. These include increased insulin and insulin-like growth factor signalling, chronic inflammation and signalling via adipokines, such as leptin. Furthermore, it is plausible that increased adiposity may alter the intestinal microbiome, contributing to gastrointestinal carcinogenesis (Harriss et al, 2009; Kant and Hull, 2011; Aleman et al, 2014). Irrespective of the exact functional basis of the association between adiposity and CRC risk, demonstrating that it is causal makes obesity an important target for primary prevention of CRC in the population.
References
Aleman JO, Eusebi LH, Ricciardiello L, Patidar K, Sanyal AJ, Holt PR (2014) Mechanisms of obesity-induced gastrointestinal neoplasia. Gastroenterology 146 (2): 357–373.
Bardou M, Barkun AN, Martel M (2013) Obesity and colorectal cancer. Gut 62 (6): 933–947.
Bianchini F, Kaaks R, Vainio H (2002) Overweight, obesity, and cancer risk. Lancet Oncol 3 (9): 565–574.
Bowden J, Davey Smith G, Burgess S (2015) Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol 44 (2): 512–525.
Burgess S, Scott RA, Timpson NJ, Davey Smith G, Thompson SG Consortium E-I (2015) Using published data in Mendelian randomization: a blueprint for efficient identification of causal risk factors. Eur J Epidemiol 30 (7): 543–552.
Carpenter CL, Ross RK, Paganini-Hill A, Bernstein L (2003) Effect of family history, obesity and exercise on breast cancer risk among postmenopausal women. Int J Cancer 106 (1): 96–102.
Forman D, Bray F, Brewster DH, Gombe Mbalawa C, Kohler B, Piñeros M, Steliarova-Foucher E, Swaminathan R, Ferlay J (2014) Cancer incidence in five continents IARC Scientific publications X(164): 917.
Frayling TM, Timpson NJ, Weedon MN, Zeggini E, Freathy RM, Lindgren CM, Perry JR, Elliott KS, Lango H, Rayner NW, Shields B, Harries LW, Barrett JC, Ellard S, Groves CJ, Knight B, Patch AM, Ness AR, Ebrahim S, Lawlor DA, Ring SM, Ben-Shlomo Y, Jarvelin MR, Sovio U, Bennett AJ, Melzer D, Ferrucci L, Loos RJ, Barroso I, Wareham NJ, Karpe F, Owen KR, Cardon LR, Walker M, Hitman GA, Palmer CN, Doney AS, Morris AD, Smith GD, Hattersley AT, McCarthy MI (2007) A common variant in the FTO gene is associated with body mass index and predisposes to childhood and adult obesity. Science 316 (5826): 889–894.
Haggar FA, Boushey RP (2009) Colorectal cancer epidemiology: incidence, mortality, survival, and risk factors. Clin Colon Rectal Surg 22 (4): 191–197.
Harriss DJ, Atkinson G, George K, Cable NT, Reilly T, Haboubi N, Zwahlen M, Egger M, Renehan AG group CC (2009) Lifestyle factors and colorectal cancer risk (1): systematic review and meta-analysis of associations with body mass index. Colorectal Dis 11 (6): 547–563.
Heid IM, Jackson AU, Randall JC, Winkler TW, Qi L, Steinthorsdottir V, Thorleifsson G, Zillikens MC, Speliotes EK, Magi R, Workalemahu T, White CC, Bouatia-Naji N, Harris TB, Berndt SI, Ingelsson E, Willer CJ, Weedon MN, Luan J, Vedantam S, Esko T, Kilpelainen TO, Kutalik Z, Li S, Monda KL, Dixon AL, Holmes CC, Kaplan LM, Liang L, Min JL, Moffatt MF, Molony C, Nicholson G, Schadt EE, Zondervan KT, Feitosa MF, Ferreira T, Lango Allen H, Weyant RJ, Wheeler E, Wood AR, Magic, Estrada K, Goddard ME, Lettre G, Mangino M, Nyholt DR, Purcell S, Smith AV, Visscher PM, Yang J, McCarroll SA, Nemesh J, Voight BF, Absher D, Amin N, Aspelund T, Coin L, Glazer NL, Hayward C, Heard-Costa NL, Hottenga JJ, Johansson A, Johnson T, Kaakinen M, Kapur K, Ketkar S, Knowles JW, Kraft P, Kraja AT, Lamina C, Leitzmann MF, McKnight B, Morris AP, Ong KK, Perry JR, Peters MJ, Polasek O, Prokopenko I, Rayner NW, Ripatti S, Rivadeneira F, Robertson NR, Sanna S, Sovio U, Surakka I, Teumer A, van Wingerden S, Vitart V, Zhao JH, Cavalcanti-Proenca C, Chines PS, Fisher E, Kulzer JR, Lecoeur C, Narisu N, Sandholt C, Scott LJ, Silander K, Stark K, Tammesoo ML, Teslovich TM, Timpson NJ, Watanabe RM, Welch R, Chasman DI, Cooper MN, Jansson JO, Kettunen J, Lawrence RW, Pellikka N, Perola M, Vandenput L, Alavere H, Almgren P, Atwood LD, Bennett AJ, Biffar R, Bonnycastle LL, Bornstein SR, Buchanan TA, Campbell H, Day IN, Dei M, Dorr M, Elliott P, Erdos MR, Eriksson JG, Freimer NB, Fu M, Gaget S, Geus EJ, Gjesing AP, Grallert H, Grassler J, Groves CJ, Guiducci C, Hartikainen AL, Hassanali N, Havulinna AS, Herzig KH, Hicks AA, Hui J, Igl W, Jousilahti P, Jula A, Kajantie E, Kinnunen L, Kolcic I, Koskinen S, Kovacs P, Kroemer HK, Krzelj V, Kuusisto J, Kvaloy K, Laitinen J, Lantieri O, Lathrop GM, Lokki ML, Luben RN, Ludwig B, McArdle WL, McCarthy A, Morken MA, Nelis M, Neville MJ, Pare G, Parker AN, Peden JF, Pichler I, Pietilainen KH, Platou CG, Pouta A, Ridderstrale M, Samani NJ, Saramies J, Sinisalo J, Smit JH, Strawbridge RJ, Stringham HM, Swift AJ, Teder-Laving M, Thomson B, Usala G, van Meurs JB, van Ommen GJ, Vatin V, Volpato CB, Wallaschofski H, Walters GB, Widen E, Wild SH, Willemsen G, Witte DR, Zgaga L, Zitting P, Beilby JP, James AL, Kahonen M, Lehtimaki T, Nieminen MS, Ohlsson C, Palmer LJ, Raitakari O, Ridker PM, Stumvoll M, Tonjes A, Viikari J, Balkau B, Ben-Shlomo Y, Bergman RN, Boeing H, Smith GD, Ebrahim S, Froguel P, Hansen T, Hengstenberg C, Hveem K, Isomaa B, Jorgensen T, Karpe F, Khaw KT, Laakso M, Lawlor DA, Marre M, Meitinger T, Metspalu A, Midthjell K, Pedersen O, Salomaa V, Schwarz PE, Tuomi T, Tuomilehto J, Valle TT, Wareham NJ, Arnold AM, Beckmann JS, Bergmann S, Boerwinkle E, Boomsma DI, Caulfield MJ, Collins FS, Eiriksdottir G, Gudnason V, Gyllensten U, Hamsten A, Hattersley AT, Hofman A, Hu FB, Illig T, Iribarren C, Jarvelin MR, Kao WH, Kaprio J, Launer LJ, Munroe PB, Oostra B, Penninx BW, Pramstaller PP, Psaty BM, Quertermous T, Rissanen A, Rudan I, Shuldiner AR, Soranzo N, Spector TD, Syvanen AC, Uda M, Uitterlinden A, Volzke H, Vollenweider P, Wilson JF, Witteman JC, Wright AF, Abecasis GR, Boehnke M, Borecki IB, Deloukas P, Frayling TM, Groop LC, Haritunians T, Hunter DJ, Kaplan RC, North KE, O’Connell JR, Peltonen L, Schlessinger D, Strachan DP, Hirschhorn JN, Assimes TL, Wichmann HE, Thorsteinsdottir U, van Duijn CM, Stefansson K, Cupples LA, Loos RJ, Barroso I, McCarthy MI, Fox CS, Mohlke KL, Lindgren CM (2010) Meta-analysis identifies 13 new loci associated with waist-hip ratio and reveals sexual dimorphism in the genetic basis of fat distribution. Nat Genet 42 (11): 949–960.
Horikoshi M, Yaghootkar H, Mook-Kanamori DO, Sovio U, Taal HR, Hennig BJ, Bradfield JP, St Pourcain B, Evans DM, Charoen P, Kaakinen M, Cousminer DL, Lehtimaki T, Kreiner-Moller E, Warrington NM, Bustamante M, Feenstra B, Berry DJ, Thiering E, Pfab T, Barton SJ, Shields BM, Kerkhof M, van Leeuwen EM, Fulford AJ, Kutalik Z, Zhao JH, den Hoed M, Mahajan A, Lindi V, Goh LK, Hottenga JJ, Wu Y, Raitakari OT, Harder MN, Meirhaeghe A, Ntalla I, Salem RM, Jameson KA, Zhou K, Monies DM, Lagou V, Kirin M, Heikkinen J, Adair LS, Alkuraya FS, Al-Odaib A, Amouyel P, Andersson EA, Bennett AJ, Blakemore AI, Buxton JL, Dallongeville J, Das S, de Geus EJ, Estivill X, Flexeder C, Froguel P, Geller F, Godfrey KM, Gottrand F, Groves CJ, Hansen T, Hirschhorn JN, Hofman A, Hollegaard MV, Hougaard DM, Hypponen E, Inskip HM, Isaacs A, Jorgensen T, Kanaka-Gantenbein C, Kemp JP, Kiess W, Kilpelainen TO, Klopp N, Knight BA, Kuzawa CW, McMahon G, Newnham JP, Niinikoski H, Oostra BA, Pedersen L, Postma DS, Ring SM, Rivadeneira F, Robertson NR, Sebert S, Simell O, Slowinski T, Tiesler CM, Tonjes A, Vaag A, Viikari JS, Vink JM, Vissing NH, Wareham NJ, Willemsen G, Witte DR, Zhang H, Zhao J . Meta-Analyses of G, Insulin-related traits C, Wilson JF, Stumvoll M, Prentice AM, Meyer BF, Pearson ER, Boreham CA, Cooper C, Gillman MW, Dedoussis GV, Moreno LA, Pedersen O, Saarinen M, Mohlke KL, Boomsma DI, Saw SM, Lakka TA, Korner A, Loos RJ, Ong KK, Vollenweider P, van Duijn CM, Koppelman GH, Hattersley AT, Holloway JW, Hocher B, Heinrich J, Power C, Melbye M, Guxens M, Pennell CE, Bonnelykke K, Bisgaard H, Eriksson JG, Widen E, Hakonarson H, Uitterlinden AG, Pouta A, Lawlor DA, Smith GD, Frayling TM, McCarthy MI, Grant SF, Jaddoe VW, Jarvelin MR, Timpson NJ, Prokopenko I, Freathy RM Early Growth Genetics C (2013) New loci associated with birth weight identify genetic links between intrauterine growth and adult height and metabolism. Nat Genet 45 (1): 76–82.
Kant P, Hull MA (2011) Excess body weight and obesity—-the link with gastrointestinal and hepatobiliary cancer. Nat Rev Gastroenterol Hepatol 8 (4): 224–238.
Lawlor DA, Harbord RM, Sterne JA, Timpson N, Davey Smith G (2008) Mendelian randomization: using genes as instruments for making causal inferences in epidemiology. Stat Med 27 (8): 1133–1163.
Locke AE, Kahali B, Berndt SI, Justice AE, Pers TH, Day FR, Powell C, Vedantam S, Buchkovich ML, Yang J, Croteau-Chonka DC, Esko T, Fall T, Ferreira T, Gustafsson S, Kutalik Z, Luan J, Magi R, Randall JC, Winkler TW, Wood AR, Workalemahu T, Faul JD, Smith JA, Hua Zhao J, Zhao W, Chen J, Fehrmann R, Hedman AK, Karjalainen J, Schmidt EM, Absher D, Amin N, Anderson D, Beekman M, Bolton JL, Bragg-Gresham JL, Buyske S, Demirkan A, Deng G, Ehret GB, Feenstra B, Feitosa MF, Fischer K, Goel A, Gong J, Jackson AU, Kanoni S, Kleber ME, Kristiansson K, Lim U, Lotay V, Mangino M, Mateo Leach I, Medina-Gomez C, Medland SE, Nalls MA, Palmer CD, Pasko D, Pechlivanis S, Peters MJ, Prokopenko I, Shungin D, Stancakova A, Strawbridge RJ, Ju Sung Y, Tanaka T, Teumer A, Trompet S, van der Laan SW, van Setten J, Van Vliet-Ostaptchouk JV, Wang Z, Yengo L, Zhang W, Isaacs A, Albrecht E, Arnlov J, Arscott GM, Attwood AP, Bandinelli S, Barrett A, Bas IN, Bellis C, Bennett AJ, Berne C, Blagieva R, Bluher M, Bohringer S, Bonnycastle LL, Bottcher Y, Boyd HA, Bruinenberg M, Caspersen IH, Ida Chen YD, Clarke R, Daw EW, de Craen AJ, Delgado G, Dimitriou M, Doney AS, Eklund N, Estrada K, Eury E, Folkersen L, Fraser RM, Garcia ME, Geller F, Giedraitis V, Gigante B, Go AS, Golay A, Goodall AH, Gordon SD, Gorski M, Grabe HJ, Grallert H, Grammer TB, Grassler J, Gronberg H, Groves CJ, Gusto G, Haessler J, Hall P, Haller T, Hallmans G, Hartman CA, Hassinen M, Hayward C, Heard-Costa NL, Helmer Q, Hengstenberg C, Holmen O, Hottenga JJ, James AL, Jeff JM, Johansson A, Jolley J, Juliusdottir T, Kinnunen L, Koenig W, Koskenvuo M, Kratzer W, Laitinen J, Lamina C, Leander K, Lee NR, Lichtner P, Lind L, Lindstrom J, Sin Lo K, Lobbens S, Lorbeer R, Lu Y, Mach F, Magnusson PK, Mahajan A, McArdle WL, McLachlan S, Menni C, Merger S, Mihailov E, Milani L, Moayyeri A, Monda KL, Morken MA, Mulas A, Muller G, Muller-Nurasyid M, Musk AW, Nagaraja R, Nothen MM, Nolte IM, Pilz S, Rayner NW, Renstrom F, Rettig R, Ried JS, Ripke S, Robertson NR, Rose LM, Sanna S, Scharnagl H, Scholtens S, Schumacher FR, Scott WR, Seufferlein T, Shi J, Vernon Smith A, Smolonska J, Stanton AV, Steinthorsdottir V, Stirrups K, Stringham HM, Sundstrom J, Swertz MA, Swift AJ, Syvanen AC, Tan ST, Tayo BO, Thorand B, Thorleifsson G, Tyrer JP, Uh HW, Vandenput L, Verhulst FC, Vermeulen SH, Verweij N, Vonk JM, Waite LL, Warren HR, Waterworth D, Weedon MN, Wilkens LR, Willenborg C, Wilsgaard T, Wojczynski MK, Wong A, Wright AF, Zhang Q . LifeLines Cohort S, Brennan EP, Choi M, Dastani Z, Drong AW, Eriksson P, Franco-Cereceda A, Gadin JR, Gharavi AG, Goddard ME, Handsaker RE, Huang J, Karpe F, Kathiresan S, Keildson S, Kiryluk K, Kubo M, Lee JY, Liang L, Lifton RP, Ma B, McCarroll SA, McKnight AJ, Min JL, Moffatt MF, Montgomery GW, Murabito JM, Nicholson G, Nyholt DR, Okada Y, Perry JR, Dorajoo R, Reinmaa E, Salem RM, Sandholm N, Scott RA, Stolk L, Takahashi A, Tanaka T, Van’t Hooft FM, Vinkhuyzen AA, Westra HJ, Zheng W, Zondervan KT . Consortium AD, Group A-BW, Consortium CAD, Consortium CK, Glgc, Icbp, Investigators M, Mu TC, Consortium MI, Consortium P, ReproGen C, Consortium G, International Endogene C, Heath AC, Arveiler D, Bakker SJ, Beilby J, Bergman RN, Blangero J, Bovet P, Campbell H, Caulfield MJ, Cesana G, Chakravarti A, Chasman DI, Chines PS, Collins FS, Crawford DC, Cupples LA, Cusi D, Danesh J, de Faire U, den Ruijter HM, Dominiczak AF, Erbel R, Erdmann J, Eriksson JG, Farrall M, Felix SB, Ferrannini E, Ferrieres J, Ford I, Forouhi NG, Forrester T, Franco OH, Gansevoort RT, Gejman PV, Gieger C, Gottesman O, Gudnason V, Gyllensten U, Hall AS, Harris TB, Hattersley AT, Hicks AA, Hindorff LA, Hingorani AD, Hofman A, Homuth G, Hovingh GK, Humphries SE, Hunt SC, Hypponen E, Illig T, Jacobs KB, Jarvelin MR, Jockel KH, Johansen B, Jousilahti P, Jukema JW, Jula AM, Kaprio J, Kastelein JJ, Keinanen-Kiukaanniemi SM, Kiemeney LA, Knekt P, Kooner JS, Kooperberg C, Kovacs P, Kraja AT, Kumari M, Kuusisto J, Lakka TA, Langenberg C, Le Marchand L, Lehtimaki T, Lyssenko V, Mannisto S, Marette A, Matise TC, McKenzie CA, McKnight B, Moll FL, Morris AD, Morris AP, Murray JC, Nelis M, Ohlsson C, Oldehinkel AJ, Ong KK, Madden PA, Pasterkamp G, Peden JF, Peters A, Postma DS, Pramstaller PP, Price JF, Qi L, Raitakari OT, Rankinen T, Rao DC, Rice TK, Ridker PM, Rioux JD, Ritchie MD, Rudan I, Salomaa V, Samani NJ, Saramies J, Sarzynski MA, Schunkert H, Schwarz PE, Sever P, Shuldiner AR, Sinisalo J, Stolk RP, Strauch K, Tonjes A, Tregouet DA, Tremblay A, Tremoli E, Virtamo J, Vohl MC, Volker U, Waeber G, Willemsen G, Witteman JC, Zillikens MC, Adair LS, Amouyel P, Asselbergs FW, Assimes TL, Bochud M, Boehm BO, Boerwinkle E, Bornstein SR, Bottinger EP, Bouchard C, Cauchi S, Chambers JC, Chanock SJ, Cooper RS, de Bakker PI, Dedoussis G, Ferrucci L, Franks PW, Froguel P, Groop LC, Haiman CA, Hamsten A, Hui J, Hunter DJ, Hveem K, Kaplan RC, Kivimaki M, Kuh D, Laakso M, Liu Y, Martin NG, Marz W, Melbye M, Metspalu A, Moebus S, Munroe PB, Njolstad I, Oostra BA, Palmer CN, Pedersen NL, Perola M, Perusse L, Peters U, Power C, Quertermous T, Rauramaa R, Rivadeneira F, Saaristo TE, Saleheen D, Sattar N, Schadt EE, Schlessinger D, Slagboom PE, Snieder H, Spector TD, Thorsteinsdottir U, Stumvoll M, Tuomilehto J, Uitterlinden AG, Uusitupa M, van der Harst P, Walker M, Wallaschofski H, Wareham NJ, Watkins H, Weir DR, Wichmann HE, Wilson JF, Zanen P, Borecki IB, Deloukas P, Fox CS, Heid IM, O’Connell JR, Strachan DP, Stefansson K, van Duijn CM, Abecasis GR, Franke L, Frayling TM, McCarthy MI, Visscher PM, Scherag A, Willer CJ, Boehnke M, Mohlke KL, Lindgren CM, Beckmann JS, Barroso I, North KE, Ingelsson E, Hirschhorn JN, Loos RJ, Speliotes EK (2015) Genetic studies of body mass index yield new insights for obesity biology. Nature 518 (7538): 197–206.
Moghaddam AA, Woodward M, Huxley R (2007) Obesity and risk of colorectal cancer: a meta-analysis of 31 studies with 70,000 events. Cancer Epidemiol Biomarkers Prev 16 (12): 2533–2547.
Orlando G, Law PJ, Palin K, Tuupanen S, Gylfe A, Hänninen U, Cajuso T, Tanskanen T, Kondelin J, Kaasinen E, Sarin A-P, Kaprio J, Eriksson JG, Rissanen H, Knekt P, Pukkala E, Jousilahti P, Salomaa V, Ripatti S, Palotie A, Järvinen H, Renkonen-Sinisalo L, Lepistö A, Böhm J, Meklin J-P, Al-Tassan NA, Palles C, Martin L, Barclay E, Tenesa A, Farrington S, Timofeeva MN, Meyer BF, Wakil SM, Campbell H, Smith CG, Idziaszczyk S, Maughan TS, Kaplan R, Kerr R, Kerr D, Buchanan DD, Win AK, Hopper J, Jenkins M, Lindor NM, Newcomb PA, Gallinger S, Conti D, Schumacher F, Casey G, Taipale J, Cheadle JP, Dunlop MG, Tomlinson IP, Aaltonen LA, Houlston RS (2016) Variation at 2q35 (PNKD and TMBIM1) influences colorectal cancer risk and identifies a pleiotropic effect with inflammatory bowel disease. Hum Mol Genet.
Pan SY, Johnson KC, Ugnat AM, Wen SW, Mao Y Canadian Cancer Registries Epidemiology Research G (2004) Association of obesity and cancer risk in Canada. Am J Epidemiol 159 (3): 259–268.
Rohde K, Keller M, Klos M, Schleinitz D, Dietrich A, Schon MR, Gartner D, Lohmann T, Dressler M, Stumvoll M, Kovacs P, Bluher M, Bottcher Y (2014) Adipose tissue depot specific promoter methylation of TMEM18. J Mol Med 92 (8): 881–888.
Serdula MK, Ivery D, Coates RJ, Freedman DS, Williamson DF, Byers T (1993) Do obese children become obese adults? A review of the literature. Prevent Med 22 (2): 167–177.
Smith GD, Ebrahim S (2003) ‘Mendelian randomization’: can genetic epidemiology contribute to understanding environmental determinants of disease? Int J Epidemiol 32 (1): 1–22.
Thrift AP, Gong J, Peters U, Chang-Claude J, Rudolph A, Slattery ML, Chan AT, Locke AE, Kahali B, Justice AE, Pers TH, Gallinger S, Hayes RB, Baron JA, Caan BJ, Ogino S, Berndt SI, Chanock SJ, Casey G, Haile RW, Du M, Harrison TA, Thornquist M, Duggan DJ, Le Marchand L, Lindor NM, Seminara D, Song M, Wu K, Thibodeau SN, Cotterchio M, Win AK, Jenkins MA, Hopper JL, Ulrich CM, Potter JD, Newcomb PA, Hoffmeister M, Brenner H, White E, Hsu L, Campbell PT (2015) Mendelian randomization study of body mass index and colorectal cancer risk. Cancer Epidemiol Biomarkers Prev 24 (7): 1024–1031.
Wheeler E, Huang N, Bochukova EG, Keogh JM, Lindsay S, Garg S, Henning E, Blackburn H, Loos RJ, Wareham NJ, O’Rahilly S, Hurles ME, Barroso I, Farooqi IS (2013) Genome-wide SNP and CNV analysis identifies common and low-frequency variants associated with severe early-onset obesity. Nat Genet 45 (5): 513–517.
Yamauchi M, Lochhead P, Morikawa T, Huttenhower C, Chan AT, Giovannucci E, Fuchs C, Ogino S (2012) Colorectal cancer: a tale of two sides or a continuum? Gut 61 (6): 794–797.
Yang TO, Reeves GK, Green J, Beral V, Cairns BJ Million Women Study C, Million Women Study C (2014) Birth weight and adult cancer incidence: large prospective study and meta-analysis. Ann Oncol 25 (9): 1836–1843.
Acknowledgements
We are grateful to all individuals who participated in the various studies. This study made use of genotyping data from the 1958 Birth Cohort, kindly made available by the Wellcome Trust Case Control Consortium 2. A full list of the investigators who contributed to the generation of the data is available at http://www.wtccc.org.uk/. At the Institute of Cancer Research, this work was supported by Cancer Research UK (C1298/A8362–Bobby Moore Fund for Cancer Research UK). Additional support was provided by the National Cancer Research Network. DJ was supported by a summer student grant from the BBRSC. In Edinburgh, the work was supported by Programme Grant funding from Cancer Research UK (C348/A12076). In Oxford, additional funding was provided by the Oxford Comprehensive Biomedical Research Centre and the EU FP7 CHIBCHA grant. Core infrastructure support to the Wellcome Trust Centre for Human Genetics, Oxford was provided by grant (090532/Z/09/Z). We are grateful to many colleagues within UK Clinical Genetics Departments (for CORGI) and to many collaborators who participated in the VICTOR and QUASAR2 trials. We also thank colleagues from the UK National Cancer Research Network (for NSCCG). Support from the European Union (FP7/207-2013, grant 258236) and FP7 collaborative project SYSCOL and COST Action in the UK is also acknowledged (BM1206). The COIN and COIN-B trials were funded by Cancer Research UK and the Medical Research Council and were conducted with the support of the National Institute of Health Research Cancer Research Network. COIN and COIN-B translational studies were supported by the Bobby Moore Fund from Cancer Research UK, Tenovus, the Kidani Trust, Cancer Research Wales and the National Institute for Social Care and Health Research Cancer Genetics Biomedical Research Unit (2011–2014). NAA, BFM and SMW were funded and supported by KFSHRC. In Finland, this work was supported by grants from the Academy of Finland (Finnish Center of Excellence Program 2012–2017, 250345), the Jane and Aatos Erkko Foundation, the Finnish Cancer Society (to KP), the European Research Council (ERC; 268648), the Sigrid Juselius Foundation, SYSCOL, the Nordic Information for Action eScience Center (NIASC), the Nordic Center of Excellence financed by NordForsk (project 62721, to KP) and State Research Funding of Kuopio University Hospital (B1401). We acknowledge the computational resources provided by the ELIXIR node, hosted at the CSC–IT Center for Science, Finland, and funded by the Academy of Finland (grants 271642 and 263164), the Ministry of Education and Culture, Finland. VS was supported by the Finnish Academy (grant number 139635). Sample collection and genotyping in the Finnish Twin Cohort has been supported by the Wellcome Trust Sanger Institute, ENGAGE–European Network for Genetic and Genomic Epidemiology, FP7-HEALTH-F4-2007 (201413), the National Institute of Alcohol Abuse and Alcoholism (grants AA-12502 and AA-00145 to Richard J Rose, and K02AA018755 to Danielle M Dick) and the Academy of Finland (100499, 205585, 265240 and 263278 to Jaakko Kaprio (JK)). The work of the Colon Cancer Family Registry (CCFR) was supported by the National Cancer Institute (UM1 CA167551), National Institutes of Health and through cooperative agreements with the following CCFR centres: Australasian Colorectal Cancer Family Registry (U01 CA074778, U01/U24 CA097735), USC Consortium Colorectal Cancer Family Registry (U01/U24 CA074799), Mayo Clinic Cooperative Familial Registry for Colon Cancer Studies (U01/U24 CA074800), Ontario Familial Colorectal Cancer Registry (U01/U24 CA074783), Seattle Colorectal Cancer Family Registry (U01/U24 CA074794) and University of Hawaii Colorectal Cancer Family Registry (U01/U24 CA074806). The CCFR Illumina GWAS was supported by funding from the National Cancer Institute, National Institutes of Health (U01 CA122839 and R01 CA143237 to GC). Seattle CCFR research was also supported by the Cancer Surveillance System of the Fred Hutchinson Cancer Research Center–Control Nos. N01-CN-67009 (1996–2003), N01-PC-35142 (2003–2010) and the Surveillance, Epidemiology and End Results (SEER) Program of the National Cancer Institute (Contract No. HHSN2612013000121, 2010–2017) with additional support from the Fred Hutchinson Cancer Research Center. The collection of cancer incidence data for the State of Hawaii used in this study was supported by the Hawai‘i Department of Health as part of the statewide cancer reporting program mandated by Hawai‘i Revised Statutes; the National Cancer Institute’s Surveillance, Epidemiology and End Results Program (SEER) awarded to the University of Hawaii (Control Nos. N01-PC-67001 1996–2003, N01-PC-35137 2003–10, Contract Nos. HHSN26120100037C 2010–13, HHSN261201300009I 2010-). The collection of cancer incidence data used in this study was supported by the California Department of Public Health as part of the statewide cancer reporting program mandated by California Health and Safety Code Section 103885; the National Cancer Institute’s Surveillance, Epidemiology and End Results Program—contract HHSN261201000035C—awarded to the University of Southern California, and—contract HHSN261201000034C—awarded to the Public Health Institute; and the Centers for Disease Control and Prevention’s National Program of Cancer Registries, under agreement—U58DP003862-01—awarded to the California Department of Public Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
DISCLAIMER
The ideas and opinions expressed herein are those of the author(s) and endorsement by the State of Hawai‘i, Department of Health, the National Cancer Institute, SEER Program, the State of California, Department of Public Health the National Cancer Institute, and the Centers for Disease Control and Prevention or their Contractors and Subcontractors, is not intended nor should be inferred. The content of this manuscript does not necessarily reflect the views or policies of the National Cancer Institute or any of the collaborating centers in the CCFR, nor does mention of trade names, commercial products or organisations imply endorsement by the US Government or the CCFR.
Supplementary Information accompanies this paper on British Journal of Cancer website
Supplementary information
Rights and permissions
This work is licensed under the Creative Commons Attribution 4.0 International License. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Jarvis, D., Mitchell, J., Law, P. et al. Mendelian randomisation analysis strongly implicates adiposity with risk of developing colorectal cancer. Br J Cancer 115, 266–272 (2016). https://doi.org/10.1038/bjc.2016.188
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2016.188
Keywords
This article is cited by
-
Methodological approaches, challenges, and opportunities in the application of Mendelian randomisation to lifecourse epidemiology: A systematic literature review
European Journal of Epidemiology (2023)
-
Systematic review of Mendelian randomization studies on risk of cancer
BMC Medicine (2022)
-
The timing of adiposity and changes in the life course on the risk of cancer
Cancer and Metastasis Reviews (2022)
-
Genetic Obesity Variants and Risk of Conventional Adenomas and Serrated Polyps
Digestive Diseases and Sciences (2022)
-
Associations of six adiposity-related markers with incidence and mortality from 24 cancers—findings from the UK Biobank prospective cohort study
BMC Medicine (2021)