Abstract
Background:
The Mediterranean diet (MD) has been proposed as a means for cancer prevention, but little evidence has been accrued regarding its potential to prevent pancreatic cancer. We investigated the association between the adherence to the MD and pancreatic cancer risk within the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort.
Methods:
Over half a million participants from 10 European countries were followed up for over 11 years, after which 865 newly diagnosed exocrine pancreatic cancer cases were identified. Adherence to the MD was estimated through an adapted score without the alcohol component (arMED) to discount alcohol-related harmful effects. Cox proportional hazards regression models, stratified by age, sex and centre, and adjusted for energy intake, body mass index, smoking status, alcohol intake and diabetes status at recruitment, were used to estimate hazard ratios (HRs) associated with pancreatic cancer and their corresponding 95% confidence intervals (CIs).
Results:
Adherence to the arMED score was not associated with risk of pancreatic cancer (HR high vs low adherence=0.99; 95% CI: 0.77–1.26, and HR per increments of two units in adherence to arMED=1.00; 95% CI: 0.94–1.06). There was no convincing evidence for heterogeneity by smoking status, body mass index, diabetes or European region. There was also no evidence of significant associations in analyses involving microscopically confirmed cases, plausible reporters of energy intake or other definitions of the MD pattern.
Conclusions:
A high adherence to the MD is not associated with pancreatic cancer risk in the EPIC study.
Similar content being viewed by others
Main
Pancreatic cancer, of which pancreatic ductal adenocarcinoma is the most common type, is estimated to become the second leading cause of cancer-related death by 2030 in the United States (Rahib et al, 2014). A trend of increasing mortality rates for pancreatic cancer is also foreseen in Europe (Malvezzi et al, 2015; Ferlay et al, 2016). The past decade has witnessed little therapeutic progress for this disease and obstacles to primary prevention persist on grounds of insufficient knowledge of the causative factors. In fact, only few risk factors of pancreatic cancer are well established, namely smoking, non-O blood group, obesity, diabetes mellitus, heavy alcohol drinking and chronic pancreatitis (Maisonneuve and Lowenfels, 2015). The identification of additional risk factors is a challenge due to the complex and multi-factorial aetiology of pancreatic cancer. Dietary factors, which could be potentially modifiable, have not been consistently linked to pancreatic cancer (AICR/WCRF, 2012).
Results from numerous epidemiological studies support the hypothesis that the Mediterranean diet (MD) is associated with a reduced cancer risk (Couto et al, 2011; Benetou et al, 2008; Schwingshackl and Hoffmann, 2014), as for example concerns breast (Buckland et al, 2013), colorectal (Bamia et al, 2013) and gastric cancers (Buckland et al, 2010). The underlying mechanisms by which the MD may exert this cancer-preventive effect are based on the inhibition of inflammatory, mutagenic and proliferative pathways in the carcinogenic process, and have been attributed to the synergistic interplay of various nutritional components, for example, omega 6 and omega 3 fatty acids, fibre, antioxidants and polyphenols, provided by fruits, vegetables, legumes, olive oil and wine (Giacosa et al, 2013). There is, however, limited and inconsistent data on the association between a priori-defined scores of adherence to the MD and pancreatic cancer risk, with an Italian case–control study of nearly 700 pancreatic cancer cases reporting a significant inverse association (Bosetti et al, 2013a), and two prospective studies, one conducted in the United States (n=1057 cases) and another one in Sweden (n=92 cases), reporting conflicting results (Jiao et al, 2009; Tognon et al, 2012). The null results from the US study could be attributed to an overall lower adherence to the MD compared with European populations, whereas the sample size of the Swedish study undermines the reliability of a true inverse association between the MD and pancreatic cancer risk. Studies on a posteriori-defined MD patterns and their association with pancreatic cancer risk have also reported contradictory results (Michaud et al, 2005; Nkondjock et al, 2005; Inoue-Choi et al, 2011; Chan et al, 2013; Bosetti et al, 2013b). Therefore, it remains inconclusive whether an association between the MD and pancreatic cancer risk exists.
Despite the absence of a consistent pattern of association, a possible link between the MD and pancreatic cancer risk is supported by the fact that some dietary components of the MD have been associated individually with a reduced risk (e.g., fruits and vegetables) or increased risk (e.g., meat) of pancreatic cancer (Wu et al, 2016; Rohrmann et al, 2013). Further support for this association comes from the well-known MD and diabetes mellitus association. A high adherence to the MD as compared with a low adherence leads to a decreasing risk of diabetes mellitus (InterAct Consortium et al, 2011; Koloverou et al, 2014), which could subsequently reduce the risk of pancreatic cancer owing to the causal link between both diseases. Thus, the MD could have a potential role in reducing pancreatic cancer risk through diabetes as a mediating factor in this relationship, or by being a common preventive factor of both diabetes and pancreatic cancer.
Our aim was to prospectively investigate the association between adherence to an a priori-defined MD index and pancreatic cancer risk. To this end we used a large European study population, featuring a wide range of variability in adherence to the MD across a North–South gradient, which also included Mediterranean populations.
Materials and methods
Study population
European Prospective Investigation into Cancer and Nutrition is a multicenter prospective cohort study conducted in 23 centres in 10 European countries (Italy, France, Denmark, Germany, Greece, Spain, Norway, Sweden, UK and The Netherlands). Over half a million participants (30% men) were recruited in the 1990s from the general population, except in some centres where other target populations were approached: breast cancer screening participants in Florence (Italy) and Utrecht (The Netherlands), mostly blood donors in Italy and Spain, vegetarian and health-conscious volunteers in Oxford (UK), and female members of the health insurance scheme for state school employees in France. European Prospective Investigation into Cancer and Nutrition was approved by the Internal Review Board of the International Agency for Research on Cancer, as well as by local institutions of the participating centres. All participants provided written informed consent. Methods of recruitment have been described in detail elsewhere (Riboli and Kaaks, 1997; Riboli et al, 2002).
We excluded a total of 23 785 participants with prevalent cancer at baseline other than non-melanoma skin cancer, 4383 participants with missing or incomplete information on follow-up, 6253 participants with incomplete dietary or non-dietary data and 9600 participants with a ratio for energy intake vs energy expenditure in the top or bottom 1%. The final study sample comprised 477 309 participants (29.8% men).
Pancreatic cancer cases ascertainment
Record linkage with population-based cancer registries and national mortality registries was performed to identify incident cancer cases and to assess the vital status of the participants. Complete follow-up data were obtained between 2004 and 2008 depending on the EPIC centre. Active follow-up was carried out in Germany (up to 2008 for Potsdam and mid-2010 for Heidelberg), Greece (up to 2009) and France (up to 2006) by reviewing cancer, pathology and health insurance records of each participant, and also by directly contacting their next-of-kin. The mean duration of follow-up was 11.3 years.
Incident pancreatic cancer cases were defined as exocrine adenocarcinomas (International Classification of Diseases for Oncology, Third Edition (ICD-O-3), codes C25.0–C25.3, C25.7–C25.9). Endocrine tumours (n=40), secondary tumours (n=67) and tumours of uncertain, benign or metastatic behaviour (n=3) were all censored at the date of their diagnosis. We ended up with 865 pancreatic cancer cases, of which 608 cases (70.3%) were microscopically confirmed, based on histology of the primary tumour, histology of the metastasis, cytology or autopsy.
Assessment of diet and adherence to the MD
Participants were asked about their habitual diet over the previous year using country-specific validated dietary questionnaires (Riboli et al, 2002), namely: quantitative food frequency questionnaires in Germany, Greece, Northern Italy and the Netherlands, diet history questionnaires in Spain, France and Ragusa (Italy), and semi-quantitative food frequency questionnaires in Denmark, Naples (Italy), Norway, the UK (combined with a 7-day record) and Umeå (Sweden). In Malmö (Sweden), a quantitative food frequency questionnaire and a 7-day food record with menu book to estimate portion sizes were used. The EPIC nutrient database was used to estimate nutrient and total energy intake from the dietary questionnaires (Slimani et al, 2007).
The relative Mediterranean diet score (rMED), as previously applied in other EPIC studies (Buckland et al, 2010, 2013) and similar in concept to the original MD score (Trichopoulou et al, 2003), was used to estimate level of conformity to the MD. It is an 18-point scale that incorporates nine selected components of the MD. Each component was calculated as a function of energy density (g per 1000 kcal per day), using the nutrient density model (Willet el al, 1997), and then divided into country-specific tertiles of intakes (except for olive oil). For the six components presumed to fit the MD; fruits (including nuts and seeds), vegetables (excluding potatoes), legumes, fish (including seafood), olive oil and cereals (white and nonwhite), a score of 0–2 points was assigned to the first (0 points), second (1 point) and third (2 points) tertile of intake, respectively. The scoring scheme for olive oil consisted of assigning 0 points to non-consumers, 1 point for participants below the median of intake and 2 points for levels of intake equal or above this median. For the 2 components presumed not to fit MD, meat (including meat products) and dairy products, the scoring was reversed (first, second and third tertile: 2, 1 and 0 points, respectively). Because alcohol consumption has been potentially associated with pancreatic cancer (Maisonneuve and Lowenfels, 2015), the alcohol component (the ninth component) was removed from the score and the non-alcohol MD score (arMED) was used instead (Buckland et al, 2013). Thus, the range of the arMED score contained eight components and the point scale ranks from 0 to 16, whereby 0 represents the lowest adherence to the MD pattern and 16 the highest adherence. The arMED score was further classified into low (0–5 points), medium (6–9 points) or high (10–16 points) adherence levels based on the previously published cutoff points (Buckland et al, 2013).
Lifestyle data
Standardised questionnaires were used to collect lifestyle data at recruitment including self-reported diabetes status, history of smoking and alcohol consumption, physical activity and socio-economic status. Diagnosis of diabetes of about half of all self-reported cases was confirmed through linkage to diabetes mellitus registries, patient records or using other procedures (Nöthlings et al, 2011). Height and weight were measured in all EPIC centres except in Norway, France and in a subgroup of the Oxford cohort where these data were self-reported. Anthropometric measurements also included waist circumference, except in Norway, in Umeå and in Oxford where only self-reported data were collected (Riboli et al, 2002). Measurements were corrected for differences in clothing and self-reported data of the aforementioned centres were corrected using prediction equations based on a fraction of real measurements (Haftenberger et al, 2002).
Statistical analysis
Cox proportional hazards regression models were used to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) for adherence to the arMED score associated with pancreatic cancer risk. Regression models were stratified by age at recruitment in 1-year categories, sex and centre to control for between-centre differences in the dietary assessment methods used at recruitment and differences in follow-up procedures. Time at entry was age at recruitment, and time at exit was age at first pancreatic cancer diagnosis for cases and age at censoring for non-cases (death, loss to follow-up or end of the follow-up, whichever came first). The proportional hazard assumption was satisfied in all models as indicated by the plots of Schoenfeld residuals on functions of time (Schoenfeld, 1982).
Adherence to the arMED was modelled as a categorical variable by dividing the score into low, medium and high levels of adherence. The low adherence category was considered as the referent group. The trend of association across levels of adherence was evaluated by using a linear variable of the medians of the score in each stratum.
Adherence to the arMED was also modelled on a continuous scale to estimate risks associated per increments of two units in the adherence. Restricted cubic splines functions in models of three and four knots on the distribution of the arMED score, to evaluate the shape of the dose–response relationship between the arMED and pancreatic cancer risk (Heinzl and Kaider, 1997), suggested a linear relationship.
Covariates considered a priori as factors known or suspected to be associated with pancreatic cancer risk and the MD were tested for confounding by comparing models with and without each variable. Those variables that changed estimates by more than 10% were retained in the regression model. Physical activity and educational level did not comply with these criteria. Risk estimates for models with waist circumference or body mass index (BMI) did not substantially differ. The association of adherence to the arMED score with pancreatic cancer risk was examined in crude models (stratified by age, sex and centre), and in multivariate models (additionally adjusted for energy intake, BMI, smoking status, alcohol intake and diabetes status).
The modifying effect of sex, BMI (normal, overweight and obese, according to WHO criteria), waist circumference (normal/moderate and large, according to National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III), 2002), physical activity (active and non-active) to elucidate further the potential effect-measure modification of overweight and obesity, smoking status (never, former and current smoker), median age at recruitment (<60 and ⩾60 years) and alcohol consumption (abstainers, moderate drinkers and drinkers, equivalent to 0 g/day, ⩽12 g/day or >12 g/day alcohol use, respectively) was evaluated through stratified analyses and the likelihood ratio test statistic in regression models with and without multiplicative interaction terms between these variables and the arMED score. In addition, we considered the influence of smoking duration and intensity on the arMED and pancreatic cancer risk association in current and former smokers. Heterogeneity by country and region (Southern, Central and Northern Europe) was also assessed by introducing an interaction term between countries/regions and the arMED score in the model.
The possible mediating effect of diabetes mellitus on this association was further evaluated in two different scenarios using mediation analysis (Tingley et al, 2014): (i) a direct effect of the arMED score on pancreatic cancer risk; and (ii) an indirect effect with diabetes mellitus as an intermediate in the causal pathway. A logistic regression model of the arMED score on diabetes status at baseline, followed by a hazard model to the onset of pancreatic cancer including arMED and the same covariates as well as the mediator variable (diabetes status) were fitted to estimate the average direct and the average causal mediation effect of diabetes.
Sensitivity analyses were performed by the exclusion of cases diagnosed within the first 2 years of follow-up (88 cases) to evaluate the influence of early effects of subclinical disease on the associations as well as those occurred within the first 5 years of follow-up (258 cases) to account for another time point of disease progression. We also excluded (i.e., censored) non-microscopically confirmed cases (257 cases) to minimise possible misclassification of tumours. Analyses were further restricted to 523 confirmed cases belonging to the pancreatic ductal adenocarcinoma histological subtype. Hazard ratios of pancreatic cancer associated with adherence to the arMED score were compared with the score including alcohol as an additional component, that is, the original rMED score (Buckland et al, 2010). Alcohol was scored dichotomously assigning two for moderate consumption (sex-specific cutoff points: 5–25 g per day for women and 10–50 g per day for men) and 0 for intakes outside this range. Other sensitivity analyses included the comparison of HRs estimated using cohort-wide tertiles, the Mediterranean diet scale (MDS; Trichopoulou et al, 2003) and the Mediterranean dietary pattern MDP scores (Sánchez-Villegas et al, 2006). Analyses excluding misreporters of energy intake, as defined by Goldberg (under-repoters if ratio of energy intake:basal metabolic rate -EI:BMR <1.14 and over-reporters if EI:BMR >2.1), were also conducted (Goldberg et al, 1991). In addition, each dietary component of the MD score was subtracted one at a time from the arMED score to investigate whether the removed component changed the risk estimates with respect to the regression models of the complete arMED score.
Statistical software used for the data analysis were Stata 12.0 (College Station, TX, USA: Stata Corp LP, 2005) and R 3.2.1. Statistical significance was based on two-sided P values <0.05.
Results
The arMED score ranged between 4 and 11.3 points (mean score: 7.81±2.63). Mean overall adherence to the arMED score was higher in southern European countries than in northern European countries, except in the UK (possibly driven by the vegetarian and health-conscious participants of the Oxford subcohort) (Supplementary Table 1). According to the participants’ demographic and lifestyle characteristics, higher levels of adherence to the arMED score were more frequent among those who were younger, less educated, non-smokers, physically inactive or obese. Participants with self-reported diabetes mellitus at baseline also showed a higher adherence level to this dietary pattern probably as a result of adopting healthier dietary habits to manage their disease. Intakes of nutrient antioxidants, fibre, plant-based food and olive oil were higher in the high adherence group, while that of dairy products and meats was lowest (Table 1).
Table 2 shows HR estimates of adherence to the arMED score associated with pancreatic cancer risk, overall and by subgroups. Compared with a low level of adherence to the arMED score, a higher adherence was not associated with risk of pancreatic cancer, either in the minimally adjusted (HR=0.88; 95% CI: 0.69–1.12; p-trend=0.24), or multivariate-adjusted models (HR=0.99; 95% CI: 0.77–1.26; p-trend=0.95). HRs associated to increments of two units in the adherence to the arMED score did also not reach statistical significance (HR=1.00; 95% CI: 0.94–1.06).
No indication for effect modification by BMI, age, smoking status, sex, physical activity, alcohol status and abdominal obesity was apparent (P-value for interaction=0.43, 0.59, 0.56, 0.90, 0.46, 0.20 and 0.76, respectively). There was also no evidence for interaction by diabetes status (P-value=0.11). Hazard ratios for pancreatic cancer per two units increment in arMED in non-diabetics tended to be inversely associated with pancreatic cancer risk in crude models (HR=0.97; 95% CI: 0.94–1.00), but not after adjusting for smoking in the multivariate-adjusted model (HR=0.98; 95% CI: 0.91–1.04). No such inverse pattern of association was observed in the subset of diabetics, although a relatively small number of pancreatic cancer cases (n=55) were available for this analysis (data not shown). Results of the mediation analysis also did not support a mediating effect of diabetes on this association (average causal mediation effect P-value=0.90, average direct effect P-value=0.02).
Stratified analyses by country or European region did not reveal statistically significant heterogeneity between strata for the association between adherence to the arMED score with pancreatic cancer risk (P-value=0.62 and 0.11, respectively). A borderline inverse association in the southern European cohort was observed, yet without reaching statistical significance (HR per two unit increment in arMED=0.88; 95% CI: 0.76–1.03, P-value=0.07).
Results of the sensitivity analyses are shown in Table 3 and Supplementary Table 2. Hazard ratios remained virtually the same in analyses restricted to microscopically confirmed cases or to participants with a follow-up longer than 2 or 5 years. No differences in the associations were further observed for pancreatic ductal adenocarcinoma tumours. The distribution of participants by the arMED score either defined as country-specific or cohort-wide tertiles was similar (23.1%, 46.7%, 29.4% and 24.2%, 45.3%, 30.5%, respectively) and HR estimates did not appreciably change when cohort-wide tertiles of the arMED score were used as the exposure of interest variable. We did also not observe any variations in risk estimates when considering adherence to the rMED score, that is, the score including alcohol, instead. The same was true for the other MD scores (MDS and MDP), with or without the contribution of alcohol to the scores. Estimates of HRs in the study population of valid reporters of energy intake did also not reach the level of statistical significance (HR per two unit increments in arMED=0.95; 95% CI: 0.88–1.03). Furthermore, no differences in risk estimates were seen after removing each arMED component of the score (Table 3). In addition, none of these components was individually associated with pancreatic cancer risk in multivariate-adjusted models controlling for the remaining components (data not shown).
Discussion
Risk of pancreatic cancer was not associated with adherence to a non-alcohol defined MD score (arMED) in this large European prospective cohort study, nor was there any evidence of a significant association between the arMED score and pancreatic cancer risk in stratified analyses by diabetes, smoking, BMI or European region.
Few studies have examined the association between adherence to the MD and pancreatic cancer risk. The National Institutes of Health-AARP Diet and Health Study prospectively evaluated this association in a diabetes-free study population including 1057 pancreatic cancer cases (Jiao et al, 2009). In this study, adherence to the MD was considered as part of a healthy lifestyle score, which also included tobacco and alcohol consumption, BMI and physical activity. The MD score was derived from the MDS (Trichopoulou et al, 2003), but was further adapted by removing the alcohol component. The risk of pancreatic cancer was significantly lower in participants who scored highest compared with those in the group of lowest compliance with the lifestyle score (RR=0.42; 95% CI: 0.26–0.66). The independent effect of the MD score on pancreatic cancer risk was also evaluated in this study, but a non-statistically significant 8% (95% CI 0.81–1.05) reduced pancreatic cancer risk was seen when a high vs a low non-alcohol MD adherence was compared, indicating that a healthy dietary pattern, such as the MD, may not have the capacity on its own to reduce risk of pancreatic cancer. Interestingly, non-smoking (never or former smokers who quit smoking for 10 or more years) and normal weight (BMI <25 kg m2) were the only two features of the lifestyle score independently associated with a decreased pancreatic cancer risk. Non-smoking yielded the greatest risk reduction within the score (RR=non-smokers vs smokers=0.59; 95% CI: 0.51–0.67). Therefore, the pancreatic cancer risk-reducing effect of this lifestyle score could be entirely attributed to the smoking component. In support of this argument, a cross-comparison of smoking status and levels of adherence to the arMED score in our study revealed that non-smokers, defined likewise as never or long-term former smokers (⩾10 years), with a high adherence to the arMED score as compared with current smokers or early former smokers with a low adherence to the arMED score had a 42% (95% CI: 0.43–0.78) lower risk of pancreatic cancer.
Another prospective study addressing the association between adherence to the MD (defined as the MDS, with some modifications) and pancreatic cancer mortality reported a 28% reduction in mortality (though, statistically significant only in men: 95% CI: 0.68–0.99) for high vs low adherence to the MD score (Tognon et al, 2012). This study included only 92 pancreatic cancer cases, which were ascertained in Sweden among the 77 151 participants of the Västerbotten Intervention Program study. Residual confounding and selection bias (subjects with higher mortality risk were excluded) prevent direct comparison of their results with those obtained in our study. The only study reporting a significant association between the MD (the MDS) and pancreatic cancer is an Italian case–control study that included 688 cases and 2204 hospital-based controls. In this study, risk of pancreatic cancer decreased by 15% (95% CI: 0.80–0.91) per one unit increment in the adherence to the MD (Bosetti et al, 2013a, 2013b). This association was consistent across strata of age, BMI, alcohol and smoking status, and was stronger in non-diabetics (OR=0.84) as compared with diabetics (OR=0.99; P-value for interaction: 0.01). In our study, high vs low adherence to the arMED score also pointed to a stronger, though non-statistically significant, inverse association between the MD and pancreatic cancer risk in non-diabetics (HR=0.91; 95% CI: 0.70–1.19). We could not examine the association in diabetics because only 55 of them developed pancreatic cancer during follow-up, but we did not observe any evidence for effect modification by diabetes status. The other prospective studies did not assess how MD is associated with pancreatic cancer risk in diabetics as compared with non-diabetics. Although the number of diabetics with pancreatic cancer was limited in number in our study population, our results suggest that diabetes status does not mediate any possible association between the MD and pancreatic cancer risk.
Finally, a recently published meta-analysis on the adherence to the MD and cancer incidence and mortality concluded for pancreatic cancer that a high adherence to this dietary pattern leads to a statistically non-significant reduced risk (RR=0.64; 95% CI: 0.38–1.08) when compared with a low adherence (Schwingshackl and Hoffmann, 2014). However, this reported risk estimate was not derived from all available published studies on this association; only estimates of the Italian and Swedish studies were pooled.
All of these earlier studies exploring the association between the MD and pancreatic cancer risk are prone to misclassification of the outcome (data for histologically confirmed cases were not provided), and some of them did not account for implausible reporting of dietary intake on the basis of estimated energy requirements to rule out exposure misclassification. Selection bias, although less likely present in cohort studies, might be another issue. Also, MD patterns in American and Nordic populations might not adequately reflect the traditional MD pattern. In our study, the association was, indeed, to some extent stronger in southern European countries, though it still did not reach statistical significance. Thus, our results seem to indicate that adherence to the MD does not reduce pancreatic cancer risk.
Similarly, two prospective studies assessing a posteriori-defined MD-like dietary patterns reported no association with pancreatic cancer risk (Michaud et al, 2005; Inoue-Choi et al, 2011). Also, neither single dietary components of the MD nor the combination of them in the arMED score appeared to be linked to pancreatic cancer risk in our study. In addition, we rendered similar risk estimates after considering the traditional rMED score that includes the alcohol component (Buckland et al, 2010). Overall, evidence supporting a role of dietary factors commonly supplied by the MD (antioxidant-rich foods, such as fruits and vegetables, and limited intake of red meat) for the prevention of this disease is still sparse (Vrieling et al, 2009; AICR/WCRF, 2012; Koushik et al, 2012; Larsson and Wolk, 2012; Rohrmann et al, 2013).
Several limitations of this study should be considered. Our results rely on dietary data measured at a single time point, which would not reflect longitudinal changes in dietary intake. Residual confounding might be present as we were unable to control for all known risk factors of pancreatic cancer, such as family history of pancreatic cancer, or for other putative factors potentially associated with pancreatic cancer risk. Confounding by smoking might be also an issue, despite the fact that additionally controlling for smoking duration and intensity did not substantially affect our results. Diabetes mellitus status could have biased our results due to misclassification, but neither self-reported nor validated data on type 2 diabetes mellitus status at baseline made a substantial difference.
Strengths of our study are its prospective nature, as well as the large sample size and long follow-up, which enabled us to conduct stratified analysis by potential effect modifiers with sufficient statistical power. Also, we were able to minimise bias due to misclassification of the outcome after restricting the study population to microscopically confirmed cases, and could confirm absence of any influence of pre-diagnostic disease on the association. Moreover, our results remained unchanged at different follow-up time points. We excluded misreporters of energy intake to ensure that reporting bias did not influence our results. However, as in any other diet-cancer association study, dietary measurement error cannot be dismissed. Our results also rely on a MD score that has been widely used in diet-cancer risk-association studies, in which the utility of the MD for the primary prevention of various cancer sites was demonstrated (Buckland et al, 2010, 2013; Bamia et al, 2013). Moreover, our study addresses the MD-pancreatic cancer risk association, for the first time, in a large European population that includes countries from the Mediterranean regions, accounting for a wide range of adherence to the MD pattern.
In conclusion, results of our study, conducted within the prospective EPIC cohort, suggest that adherence to the MD is not associated with the development of pancreatic cancer.
Change history
14 March 2017
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
AICR/WCRF (2012) Continuous Update Project. Pancreatic Cancer http://www.wcrf.org/int/research-we-fund/continuous-update-project-findings-reports/pancreatic-cancer . (accessed 12 August 2015).
Bamia C, Lagiou P, Buckland G, Grioni S, Agnoli C, Taylor AJ, Dahm CC, Overvad K, Olsen A, Tjønneland A, Cottet V, Boutron-Ruault MC, Morois S, Grote V, Teucher B, Boeing H, Buijsse B, Trichopoulos D, Adarakis G, Tumino R, Naccarati A, Panico S, Palli D, Bueno-de-Mesquita HB, van Duijnhoven FJ, Peeters PH, Engeset D, Skeie G, Lund E, Sánchez MJ, Barricarte A, Huerta JM, Quirós JR, Dorronsoro M, Ljuslinder I, Palmqvist R, Drake I, Key TJ, Khaw KT, Wareham N, Romieu I, Fedirko V, Jenab M, Romaguera D, Norat T, Trichopoulou A (2013) Mediterranean diet and colorectal cancer risk: results from a European cohort. Eur J Epidemiol 28 (4): 317–328.
Benetou V, Trichopoulou A, Orfanos P, Naska A, Lagiou P, Boffetta P, Trichopoulos D Greek EPICcohort (2008) Conformity to traditional Mediterranean diet and cancer incidence: the Greek EPIC cohort. Br J Cancer 99 (1): 191–195.
Bosetti C, Bravi F, Turati F, Edefonti V, Polesel J, Decarli A, Negri E, Talamini R, Franceschi S, La Vecchia C, Zeegers MP (2013b) Nutrient-based dietary patterns and pancreatic cancer risk. Ann Epidemiol 23 (3): 124–128.
Bosetti C, Turati F, Dal Pont A, Ferraroni M, Polesel J, Negri E, Serraino D, Talamini R, La Vecchia C, Zeegers MP (2013a) The role of Mediterranean diet on the risk of pancreatic cancer. Br J Cancer 109 (5): 1360–1366.
Buckland G, Agudo A, Luján L, Jakszyn P, Bueno-de-Mesquita HB, Palli D, Boeing H, Carneiro F, Krogh V, Sacerdote C, Tumino R, Panico S, Nesi G, Manjer J, Regnér S, Johansson I, Stenling R, Sanchez MJ, Dorronsoro M, Barricarte A, Navarro C, Quirós JR, Allen NE, Key TJ, Bingham S, Kaaks R, Overvad K, Jensen M, Olsen A, Tjønneland A, Peeters PH, Numans ME, Ocké MC, Clavel-Chapelon F, Morois S, Boutron-Ruault MC, Trichopoulou A, Lagiou P, Trichopoulos D, Lund E, Couto E, Boffeta P, Jenab M, Riboli E, Romaguera D, Mouw T, González CA (2010) Adherence to a Mediterranean diet and risk of gastric adenocarcinoma within the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort study. Am J Clin Nutr 91 (2): 381–390.
Buckland G, Travier N, Cottet V, González CA, Luján-Barroso L, Agudo A, Trichopoulou A, Lagiou P, Trichopoulos D, Peeters PH, May A, Bueno-de-Mesquita HB, Bvan Duijnhoven FJ, Key TJ, Allen N, Khaw KT, Wareham N, Romieu I, McCormack V, Boutron-Ruault M, Clavel-Chapelon F, Panico S, Agnoli C, Palli D, Tumino R, Vineis P, Amiano P, Barricarte A, Rodríguez L, Sanchez MJ, Chirlaque MD, Kaaks R, Teucher B, Boeing H, Bergmann MM, Overvad K, Dahm CC, Tjønneland A, Olsen A, Manjer J, Wirfält E, Hallmans G, Johansson I, Lund E, Hjartåker A, Skeie G, Vergnaud AC, Norat T, Romaguera D, Riboli E (2013) Adherence to the mediterranean diet and risk of breast cancer in the European prospective investigation into cancer and nutrition cohort study. Int J Cancer 132 (12): 2918–2927.
Chan JM, Gong Z, Holly EA, Bracci PM (2013) Dietary patterns and risk of pancreatic cancer in a large population-based case-control study in the San Francisco Bay Area. Nutr Cancer 65 (1): 157–164.
Couto E, Boffetta P, Lagiou P, Ferrari P, Buckland G, Overvad K, Dahm CC, Tjønneland A, Olsen A, Clavel-Chapelon F, Boutron-Ruault MC, Cottet V, Trichopoulos D, Naska A, Benetou V, Kaaks R, Rohrmann S, Boeing H, von Ruesten A, Panico S, Pala V, Vineis P, Palli D, Tumino R, May A, Peeters PH, Bueno-de-Mesquita HB, Büchner FL, Lund E, Skeie G, Engeset D, Gonzalez CA, Navarro C, Rodríguez L, Sánchez MJ, Amiano P, Barricarte A, Hallmans G, Johansson I, Manjer J, Wirfärt E, Allen NE, Crowe F, Khaw KT, Wareham N, Moskal A, Slimani N, Jenab M, Romaguera D, Mouw T, Norat T, Riboli E, Trichopoulou A (2011) Mediterranean dietary pattern and cancer risk in the EPIC cohort. Br J Cancer 104 (9): 1493–1499.
Ferlay J, Partensky C, Bray F (2016) More deaths from pancreatic cancer than breast cancer in the EU by 2017. Acta Oncol 55: 1158–1160.
Giacosa A, Barale R, Bavaresco L, Gatenby P, Gerbi V, Janssens J, Johnston B, Kas K, La Vecchia C, Mainguet P, Morazzoni P, Negri E, Pelucchi C, Pezzotti M, Rondanelli M (2013) Cancer prevention in Europe: the Mediterranean diet as a protective choice. Eur J Cancer Prev 22 (1): 90–95.
Goldberg GR, Black AE, Jebb SA, Cole TJ, Murgatroyd PR, Coward WA, Prentice AM (1991) Critical evaluation of energy intake data using fundamental principles of energy physiology: 1. Derivation of cut-off limits to identify under-recording. Eur J Clin Nutr 45 (12): 569–581.
Haftenberger M, Lahmann PH, Panico S, Gonzalez CA, Seidell JC, Boeing H, Giurdanella MC, Krogh V, Bueno-de-Mesquita HB, Peeters PH, Skeie G, Hjartåker A, Rodriguez M, Quirós JR, Berglund G, Janlert U, Khaw KT, Spencer EA, Overvad K, Tjønneland A, Clavel-Chapelon F, Tehard B, Miller AB, Klipstein-Grobusch K, Benetou V, Kiriazi G, Riboli E, Slimani N (2002) Overweight, obesity and fat distribution in 50- to 64-year-old participants in the European Prospective Investigation into Cancer and Nutrition (EPIC). Public Health Nutr 5 (6B): 1147–1162.
Heinzl H, Kaider A (1997) Gaining more flexibility in cox proportional hazards regression models with cubic spline functions. Comput Methods Programs Biomed 54 (3): 201–208.
Inoue-Choi M, Flood A, Robien K, Anderson K (2011) Nutrients, food groups, dietary patterns, and risk of pancreatic cancer in postmenopausal women. Cancer Epidemiol Biomarkers Prev 20 (4): 711–714.
InterAct Consortium, Romaguera D, Guevara M, Norat T, Langenberg C, Forouhi NG, Sharp S, Slimani N, Schulze MB, Buijsse B, Buckland G, Molina-Montes E, Sánchez MJ, Moreno-Iribas MC, Bendinelli B, Grioni S, van der Schouw YT, Arriola L, Beulens JW, Boeing H, Clavel-Chapelon F, Cottet V, Crowe FL, de Lauzon-Guillan B, Franks PW, Gonzalez C, Hallmans G, Kaaks R, Key TJ, Khaw K, Nilsson P, Overvad K, Palla L, Palli D, Panico S, Quirós JR, Rolandsson O, Romieu I, Sacerdote C, Spijkerman AM, Teucher B, Tjonneland A, Tormo MJ, Tumino R, van der AD, Feskens EJ, Riboli E, Wareham NJ (2011) Mediterranean diet and type 2 diabetes risk in the European Prospective Investigation into Cancer and Nutrition (EPIC) study: the InterAct project. Diabetes Care 34 (9): 1913–1918.
Jiao L, Mitrou PN, Reedy J, Graubard BI, Hollenbeck AR, Schatzkin A, Stolzenberg-Solomon R (2009) A combined healthy lifestyle score and risk of pancreatic cancer in a large cohort study. Arch Intern Med 169 (8): 764–770.
Koloverou E, Giugliano D, Panagiotakos D (2014) The effect of Mediterranean diet on the development of type 2 diabetes mellitus: a meta-analysis of 10 prospective studies and 136 846 participants. Metabolism 63 (7): 903–911.
Koushik A, Spiegelman D, Albanes D, Anderson KE, Bernstein L, van den Brandt PA, Bergkvist L, English DR, Freudenheim JL, Fuchs CS, Genkinger JM, Giles GG, Goldbohm RA, Horn-Ross PL, Männistö S, McCullough ML, Millen AE, Miller AB, Robien K, Rohan TE, Schatzkin A, Shikany JM, Stolzenberg-Solomon RZ, Willett WC, Wolk A, Ziegler RG, Smith-Warner SA (2012) Intake of fruits and vegetables and risk of pancreatic cancer in a pooled analysis of 14 cohort studies. Am J Epidemiol 176 (5): 373–386.
Larsson SC, Wolk A (2012) Red and processed meat consumption and risk of pancreatic cancer: meta-analysis of prospective studies. Br J Cancer 106 (3): 603–607.
Maisonneuve P, Lowenfels AB (2015) Risk factors for pancreatic cancer: a summary review of meta-analytical studies. Int J Epidemiol 44 (1): 186–198.
Malvezzi M, Bertuccio P, Rosso T, Rota M, Levi F, La Vecchia C, Negri E (2015) European cancer mortality predictions for the year 2015: does lung cancer have the highest death rate in EU women? Ann Oncol 26 (4): 779–786.
Michaud DS, Skinner HG, Wu K, Hu F, Giovannucci E, Willett WC, Colditz GA, Fuchs CS (2005) Dietary patterns and pancreatic cancer risk in men and women. J Natl Cancer Inst 7: 518–524.
National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) (2002) Third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III) final report. Circulation 106: 3143–3421.
Nkondjock A, Krewski D, Johnson KC, Ghadirian P Canadian Cancer Registries Epidemiology Research Group (2005) Dietary patterns and risk of pancreatic cancer. Int J Cancer 114 (5): 817–823.
Nöthlings U, Boeing H, Maskarinec G, Sluik D, Teucher B, Kaaks R, Tjønneland A, Halkjaer J, Dethlefsen C, Overvad K, Amiano P, Toledo E, Bendinelli B, Grioni S, Tumino R, Sacerdote C, Mattiello A, Beulens JW, Iestra JA, Spijkerman AM, van der A DL, Nilsson P, Sonestedt E, Rolandsson O, Franks PW, Vergnaud AC, Romaguera D, Norat T, Kolonel LN (2011) Food intake of individuals with and without diabetes across different countries and ethnic groups. Eur J Clin Nutr 65 (5): 635–641.
Rahib L, Smith BD, Aizenberg R, Rosenzweig AB, Fleshman JM, Matrisian LM (2014) Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res 74 (11): 2913–2921.
Riboli E, Hunt KJ, Slimani N, Ferrari P, Norat T, Fahey M, Charrondière UR, Hémon B, Casagrande C, Vignat J, Overvad K, Tjønneland A, Clavel-Chapelon F, Thiébaut A, Wahrendorf J, Boeing H, Trichopoulos D, Trichopoulou A, Vineis P, Palli D, Bueno-De-Mesquita HB, Peeters PH, Lund E, Engeset D, González CA, Barricarte A, Berglund G, Hallmans G, Day NE, Key TJ, Kaaks R, Saracci R (2002) European Prospective Investigation into Cancer and Nutrition (EPIC): study populations and data collection. Public Health Nutr 5 (6B): 1113–1124.
Riboli E, Kaaks R (1997) The EPIC project: rationale and study design. European Prospective Investigation into Cancer and Nutrition. Int J Epidemiol 26 (Suppl 1): 6–14.
Rohrmann S, Linseisen J, Nöthlings U, Overvad K, Egeberg R, Tjønneland A, Boutron-Ruault MC, Clavel-Chapelon F, Cottet V, Pala V, Tumino R, Palli D, Panico S, Vineis P, Boeing H, Pischon T, Grote V, Teucher B, Khaw KT, Wareham NJ, Crowe FL, Goufa I, Orfanos P, Trichopoulou A, Jeurnink SM, Siersema PD, Peeters PH, Brustad M, Engeset D, Skeie G, Duell EJ, Amiano P, Barricarte A, Molina-Montes E, Rodríguez L, Tormo MJ, Sund M, Ye W, Lindkvist B, Johansen D, Ferrari P, Jenab M, Slimani N, Ward H, Riboli E, Norat T, Bueno-de-Mesquita HB (2013) Meat and fish consumption and risk of pancreatic cancer: results from the European Prospective Investigation into Cancer and Nutrition. Int J Cancer 132 (3): 617–624.
Schoenfeld D (1982) Partial residuals for the proportional hazards regression model. Biometrika 69: 239–241.
Schwingshackl L, Hoffmann G (2014) Adherence to Mediterranean diet and risk of cancer: a systematic review and meta-analysis of observational studies. Int J Cancer 135 (8): 1884–1897.
Slimani N, Deharveng G, Unwin I, Southgate DA, Vignat J, Skeie G, Salvini S, Parpinel M, Møller A, Ireland J, Becker W, Farran A, Westenbrink S, Vasilopoulou E, Unwin J, Borgejordet A, Rohrmann S, Church S, Gnagnarella P, Casagrande C, van Bakel M, Niravong M, Boutron-Ruault MC, Stripp C, Tjønneland A, Trichopoulou A, Georga K, Nilsson S, Mattisson I, Ray J, Boeing H, Ocké M, Peeters PH, Jakszyn P, Amiano P, Engeset D, Lund E, de Magistris MS, Sacerdote C, Welch A, Bingham S, Subar AF, Riboli E (2007) The EPIC nutrient database project (ENDB): a first attempt to standardize nutrient databases across the 10 European countries participating in the EPIC study. Eur J Clin Nutr 61: 1037–1056.
Sánchez-Villegas A, Bes-Rastrollo M, Martínez-González MA, Serra-Majem L (2006) Adherence to a Mediterranean dietary pattern and weight gain in a follow-up study: the SUN cohort. Int J Obes (Lond) 30 (2): 350–358.
Tingley D, Yamamoto T, Hirose K, Keele L, Imai K (2014) Mediation: R Package for Causal Mediation Analysis. R Package version 4.4.5.
Tognon G, Nilsson LM, Lissner L, Johansson I, Hallmans G, Lindahl B, Winkvist A (2012) The Mediterranean diet score and mortality are inversely associated in adults living in the subarctic region. J Nutr 142 (8): 1547–1553.
Trichopoulou A, Costacou T, Bamia C, Trichopoulos D (2003) Adherence to a Mediterranean diet and survival in a Greek population. N Engl J Med 348 (26): 2599–2608.
Vrieling A, Verhage BA, van Duijnhoven FJ, Jenab M, Overvad K, Tjønneland A, Olsen A, Clavel-Chapelon F, Boutron-Ruault MC, Kaaks R, Rohrmann S, Boeing H, Nöthlings U, Trichopoulou A, John T, Dimosthenes Z, Palli D, Sieri S, Mattiello A, Tumino R, Vineis P, van Gils CH, Peeters PH, Engeset D, Lund E, Rodríguez Suárez L, Jakszyn P, Larrañaga N, Sánchez MJ, Chirlaque MD, Ardanaz E, Manjer J, Lindkvist B, Hallmans G, Ye W, Bingham S, Khaw KT, Roddam A, Key T, Boffetta P, Duell EJ, Michaud DS, Riboli E, Bueno-de-Mesquita HB (2009) Fruit and vegetable consumption and pancreatic cancer risk in the European Prospective Investigation into Cancer and Nutrition. Int J Cancer 124 (8): 1926–1934.
Willett WC, Howe GR, Kushi LH (1997) Adjustment for total energy intake in epidemiologic studies. Am J Clin Nutr 65 (4 Suppl): 1220–1228.
Wu QJ, Wu L, Zheng LQ, Xu X, Ji C, Gong TT (2016) Consumption of fruit and vegetables reduces risk of pancreatic cancer: evidence from epidemiological studies. Eur J Cancer Prev 25 (3): 196–205.
Acknowledgements
EM is thankful to Dr Núria Malats of the Spanish National Cancer Research Center (CNIO) for her critical comments on this paper. The coordination of EPIC is financially supported by the European Commission (DG-SANCO) and the International Agency for Research on Cancer. The national cohorts are supported by Danish Cancer Society (Denmark); Ligue Contre le Cancer, Institut Gustave Roussy, Mutuelle Générale de l’Education Nationale, Institut National de la Santé et de la Recherche Médicale (INSERM) (France); German Cancer Aid, German Cancer Research Center (DKFZ), Federal Ministry of Education and Research (BMBF), Deutsche Krebshilfe, Deutsches Krebsforschungszentrum and Federal Ministry of Education and Research (Germany); The Hellenic Health Foundation (Greece); Associazione Italiana per la Ricerca sul Cancro-AIRC-Italy and National Research Council (Italy); Dutch Ministry of Public Health, Welfare and Sports (VWS), Netherlands Cancer Registry (NKR), LK Research Funds, Dutch Prevention Funds, Dutch ZON (Zorg Onderzoek Nederland), World Cancer Research Fund (WCRF), Statistics Netherlands (the Netherlands); ERC-2009-AdG 232997 and Nordforsk, Nordic Centre of Excellence programme on Food, Nutrition and Health (Norway); Health Research Fund (FIS), PI12/00002 co-funded by ERDF, PI13/00061 to Granada, PI13/01162 to Murcia, Regional Governments of Andalucía, Asturias, Basque Country, Murcia and Navarra, ISCIII RETIC (RD06/0020; Spain); WCR (15–0391); Swedish Cancer Society, Swedish Research Council and County Councils of Skåne and Västerbotten (Sweden); Cancer Research UK (14136 to EPIC-Norfolk; C570/A16491 and C8221/A19170 to EPIC-Oxford), Medical Research Council (1000143 to EPIC-Norfolk, MR/M012190/1 to EPIC-Oxford; UK).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License.
Supplementary Information accompanies this paper on British Journal of Cancer website
Supplementary information
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Molina-Montes, E., Sánchez, MJ., Buckland, G. et al. Mediterranean diet and risk of pancreatic cancer in the European Prospective Investigation into Cancer and Nutrition cohort. Br J Cancer 116, 811–820 (2017). https://doi.org/10.1038/bjc.2017.14
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2017.14
Keywords
This article is cited by
-
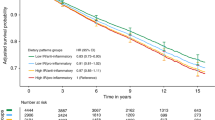
Inflammatory potential of diet and pancreatic cancer risk in the EPIC study
European Journal of Nutrition (2022)
-
An updated systematic review and meta-analysis on adherence to mediterranean diet and risk of cancer
European Journal of Nutrition (2021)
-
Healthy lifestyle and the risk of pancreatic cancer in the EPIC study
European Journal of Epidemiology (2020)