Abstract
Classically, Parkinson's disease (PD) is linked to dopamine neuron death in the substantia nigra pars compacta. Intracytoplasmic protein inclusions named Lewy bodies, and corresponding Lewy neurites found in neuronal processes, are also key features of the degenerative process in the substantia nigra. The molecular mechanisms by which substantia nigra dopamine neurons die and whether the Lewy pathology is directly involved in the cell death pathway are open questions. More recently, it has become apparent that Lewy pathology gradually involves greater parts of the PD brain and is widespread in late stages. In this review, we first discuss the role of misfolded α-synuclein protein, which is the main constituent of Lewy bodies, in the pathogenesis of PD. We then describe recent evidence that α-synuclein might transfer between cells in PD brains. We discuss in detail the possible molecular mechanisms underlying the proposed propagation and the likely consequences for cells that take up α-synuclein. Finally, we focus on aspects of the pathogenic process that could be targeted with new pharmaceutical therapies or used to develop biomarkers for early PD detection.
Similar content being viewed by others
Main
Multiple hypotheses exist to help explain dopamine neuron cell death and Lewy body formation observed in Parkinson's disease (PD). Mutations of the main proteinaceous constituent of Lewy bodies, α-synuclein (α-syn), lead to dominant, familial disease forms.1, 2, 3, 4, 5 More recently, genome-wide association studies (GWASs) identified variants of the α-synuclein gene (SNCA) gene, encoding α-syn protein, that are coupled to increased PD susceptibility, thus clearly linking this protein to idiopathic PD.6, 7, 8 Furthermore, overexpressed and/or misfolded α-syn is pathogenic to cells while α-syn can be secreted from cells, enter other cells, and seed small intracellular aggregates, demonstrating a connection between α-syn and pathogenic mechanisms of PD.9, 10, 11, 12, 13, 14, 15, 16 In parallel, a much-discussed hypothesis by Braak and colleagues17 states that a pathogenic agent, introduced via ingestion and/or inhalation, may transfer from the entry site along known long, unmyelinated axons to basal brain areas and eventually to brain stem and cortical regions. Although α-syn is unlikely to be this initial pathogen, it might be the initial target of the unknown agent. If α-syn is misfolded because of the action of the unknown agent, it might contribute to the spreading of pathology by moving from one cell to another and triggering misfolding in the recipient cells. If so, it might explain the surprising presence of Lewy bodies in the young neural grafts of transplanted PD patients observed more than a decade after surgery.18, 19, 20, 21 In this review, we discuss possible mechanisms by which α-syn could spread between cells and have deadly consequences by describing the molecular evidence for α-syn cellular exit, transit to other cells, uptake by cells, intracellular aggregation, and responses to α-syn accumulation.
The Relationship Between α-Syn and PD
Genetic studies
The first connection between α-syn and PD arose when researchers discovered a mutation (encoding the mutant Ala53Thr protein) in the SNCA gene in a family with autosomal-dominant PD.1 In the years since, additional coding region mutations in and multiplications of SNCA that cause neurological disease have been identified.2, 3, 4, 5 These findings clearly illustrate a key relationship between alterations in α-syn expression or function and familial PD. In addition to coding region mutations, several SNCA promoter polymorphisms are associated with autosomal-dominant Parkinsonism.22 Perhaps even more interesting is the discovery by GWAS of several single-nucleotide polymorphisms (SNPs) in the SNCA gene strongly associated with PD risk.6, 7, 8 These recent findings strengthen the relationship between α-syn biology and mechanisms underlying PD pathology as, importantly, α-syn is now linked not only to the rare forms of familial PD but also to idiopathic PD.
Aggregation potential of α-syn
How can we connect overexpression of normal α-syn or expression of mutant α-syn with Lewy bodies? α-Syn is the main protein component of Lewy bodies,23 but, importantly, the α-syn found in Lewy bodies is misfolded and phosphorylated,24, 25 indicating that a pathogenic variety of α-syn accumulates in diseased or damaged cells. The native α-syn monomer is an unfolded, soluble protein, and in vitro studies have shown that monomeric, oligomeric, and fibrillar species of α-syn exist in equilibrium26, 27, 28 (Figure 1a). Upon oligomerization, α-syn remains soluble, but once the protein undergoes fibrillization, α-syn becomes insoluble and has the capacity to self-aggregate.26, 27, 28 Aggregation of α-syn proteins into β-sheet-rich amyloid assembles is a nucleation-dependent process, that is, addition of preformed fibrillar seeds accelerates the process29 (Figure 1b). Growing evidence suggests that oligomers are the cytotoxic species, although it is unclear if they alone underlie neurotoxicity.30 What is also uncertain is whether α-syn-containing Lewy bodies and neurites trigger neurodegeneration or whether they reveal appropriate cellular coping mechanisms that sequester proteins into less harmful aggregates in response to an underlying pathogenic process.31
α-Synuclein aggregation process. (a) In certain conditions, the natively unfolded α-syn monomers are able to self-aggregate in soluble oligomers and then to form typical amyloid fibrils with β-sheet structure. These different species of α-syn assemblies coexist in a highly dynamic equilibrium. (b) α-Syn fibrillization is a nucleation-dependent process. Addition of exogenous preformed fibrils (red) speeds up the conversion of monomers to fibrils. The color reproduction of this figure is available on the html full text version of the manuscript
Lewy bodies found in young neural grafts
In the 1980s–1990s, neural grafts derived from midbrain tissue obtained from aborted fetuses were transplanted into the striata of several people with PD worldwide.32 Curiously, in addition to the expected Lewy pathology observed in the host tissue, we and others found Lewy bodies containing misfolded α-syn in the 10–16-year-old grafted neurons.18, 19, 20, 21
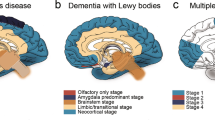
These intriguing findings led to renewed discussion of the seminal work of Braak et al.,33 which suggests that PD pathology spreads in specific stages according to a stereotypic pattern from one brain area to another. Briefly, based on extensive analysis of post-mortem samples from patients at different stages of PD progression, Braak and co-workers17 hypothesized that a pathogen can transfer in predictable steps from the gut and nasal epithelium to basal parts of the brain, and finally, via the midbrain to cortical areas. We, and others, suggested that a mechanism related to the one proposed by Braak might explain the presence of Lewy bodies in the neural grafts too; specifically, pathogen transfer from host cells to grafted cells might occur and induce formation of Lewy bodies in the young neurons.34, 35, 36, 37, 38, 39, 40, 41, 42, 43 The core of this review will focus on the idea that α-syn is the pathogenic agent that can transfer from one cell to another, thus propagating pathology from diseased neurons to others.
Molecular Mechanisms Involved in Intercellular Transfer of α-Syn Pathology
In order for a pathogenic agent to transfer from one cell to another and act to harm the recipient cell, several steps must take place. First, the pathogen must exit the host cell. Second, it must somehow transit from the first cell to the second. After arrival at the recipient cell, the pathogen must gain access to the cell, somehow crossing the cell membrane. Finally, once inside the recipient cell, the pathogen must cause cellular stress or otherwise incapacitate the recipient cell, for example, by acting as a template that promotes misfolding of endogenous protein. In this section, we will discuss the latest findings that indicate that α-syn is capable of performing all of the actions listed above; in fact, α-syn might be the pathogenic agent that spreads from one cell to another, throughout the nervous system, during the course of PD.
How does α-syn leave cells?
α-Syn can leave cells via various mechanisms including secretion and, more specifically, exocytosis (Figure 2a). Multiple forms of α-syn have been detected in cerebrospinal fluid, blood plasma,44, 45, 46 and more recently, in saliva,47 indicating a secretory process. Monomers and aggregated forms of α-syn are secreted from neuroblastoma cells overexpressing α-syn and from rat primary cortical neurons.10, 15 This secretion is inhibited by low temperature, suggesting an exocytotic process.10, 15 The intraluminal vesicular localization of α-syn further supports this role for exocytosis, although the classical endoplasmic reticulum/Golgi-dependent pathway is likely not involved.10, 15 Cellular stressors, such as serum deprivation, proteosomal or lysosomal inhibition, and hydrogen peroxide promote vesicular translocation of α-syn and subsequent release15 (Figure 2a). Finally, induction of misfolding also increases association of α-syn with both vesicles and secretion, whereas medium-derived α-syn shows more oxidative modifications than the cellular forms, suggesting that neurons preferentially release damaged and aggregation-prone α-syn proteins.15
Model of α-synuclein cell-to-cell transfer. Transfer of α-syn from a donor cell (blue) to a recipient cell (red) requires two consecutive steps: (a) Exit of α-syn from the donor cell. Exocytotic vesicles10, 15 and exosomes,14, 54 derived from multivesicular bodies, themselves derived from endosomes, have been reported to mediate α-syn release from cells. Oxidative stress and proteasomal and lysosomal inhibition increase both vesicular translocation and release of α-syn.15 Lysosomal impairment also promotes exosome-mediated secretion of α-syn.54 Dying neurons, which discharge their content into the environment, are another potential source of extracellular α-syn. The precise mechanism of α-syn exocytosis, the potential association of extracellular α-syn with other proteins, and the nature of released α-syn in terms of aggregation remain outstanding issues. (b) Entry of α-syn into the recipient cell. Passive diffusion through the plasma membrane,11, 68 endocytosis,9, 11, 12, 16 and exosome-mediated transfer of α-syn into a recipient cell14, 54 have been reported. Whether an unknown receptor or lipid rafts are involved in α-syn endocytotic uptake remains to be elucidated. Although α-syn that has transferred between cells passively or via exosomes is likely to have a direct access to the cytosol in the recipient cell, the mechanism by which α-syn might move from an endosome into the cytoplasm has not yet been clarified
Impairment of the autophagy-lysosome pathway is another feature of PD48 that might explain the extracellular release of α-syn.48 Autophagosomes, which normally degrade misfolded cytosolic proteins, could be overwhelmed by accumulation and/or presence of abnormal forms of α-syn proteins and thus might dispose of them by discharging their contents in the extracellular space.35 Interestingly, α-syn can be secreted from cells in association with exosomes14, 49 (Figure 2a), which may be affected by autophagosomes.50 Exosomes are small vesicles that can break off from the endocytic machinery of one cell, transverse the extracellular space, and then fuse with the outer membrane of another cell, thus transferring their contents to the new cell.51 Of relevance to other neurodegenerative disorders, they have been shown to transmit pathogenic prion proteins52, 53, 54 and β-amyloid (Aβ) aggregates.55 Recently, α-syn-containing exosomes secreted from neuroblastoma cells overexpressing α-syn were found to transfer α-syn to other cultured neuroblastoma cells. Lysosomal inhibition of donor cells increased both exosome-mediated release and transfer of α-syn49 (Figure 2a). Finally, uncontrolled exit of α-syn might occur when dying cells lyse and expel their contents into the extracellular space (Figure 2a). However, it is important to note that typical release of α-syn is likely a regulated, low-probability event.15
Propagation of α-syn to a new cell
Once α-syn leaves the first cell, it must somehow transit to the recipient cell. Direct cell-to-cell transfer could occur, especially if many proteins are in the extracellular space because of lysed cells. Alternately, if α-syn were enclosed in an exocytosed vesicle10, 15 or exosome,14, 49 as described above, the protein would be protected during its journey from extracellular enzymes. If unprotected, the risk for degradation is apparent as matrix metalloproteinase 3 has been shown to cleave both recombinant α-syn proteins56, 57 and neuroblastoma cell-secreted α-syn.56 Recently, it was suggested that the molecular chaperone heat shock protein 70 (Hsp70) is released from cells together with α-syn and might modulate levels of extracellular α-syn oligomers.13 Whether this association of Hsp70 with extracellular α-syn plays a role in α-syn transit from one cell to another remains to be investigated. Finally, cellular mechanisms known to contribute to intercellular transit of other proteins could be involved. For example, tunneling nanotubes (TNTs), which are thin extensions of surface membrane interconnecting cells over long distances, have been shown to convey the scrapie form of prion protein (PrPsc) not only between co-cultured infected and naive neuronal cells but also from bone marrow-derived dendritic cells to primary neurons.58 Therefore, it has been hypothesized that TNT-mediated neuroimmune interactions within lymphoid organs could account for the spread of PrPsc from intestine, the peripheral entry site into the body for PrPsc derived from ingested food, to the peripheral nervous system and then to the brain. Given that α-syn might be the pathogenic agent spreading from the gut or the nose to the brain according to Braak's hypothesis, it would be interesting to investigate whether TNTs could act as conduits for intercellular transport of α-syn.
Considering that Braak's hypothesis requires pathology to spread over long distances, axons could participate in transfer of misfolded α-syn between different brain regions. α-Syn moves antero- and retro-gradely along axons, mainly through the slow component of axonal transport59, 60 with kinesin and dynein, the motor proteins mediating antero- and retro-grade axoplasmic transport, respectively, providing bidirectional movement of α-syn along the axon.61 More recently, compartmentalized microfluidic culture systems were used to demonstrate α-syn release and uptake at axonal terminals and suggest a mechanism of trans-synaptic cell-to-cell transfer.13
Cellular entry of α-syn
How does extracellular α-syn enter a cell and gain access to the cytoplasm of the recipient cell? α-Syn is known to directly interact with lipids and membranes.62 Thus, extracellular α-syn protein can associate directly with the exterior of cells. The simplest option is then passive diffusion of α-syn through the membrane (Figure 2b), which has been suggested in cases where exogenous, monomeric α-syn is applied to the outside of cells and taken up by a process insensitive to low temperature, and to inhibition of endocytosis, and very likely limited to a small number of extracellular proteins with particular hydrophobic properties.11, 63 Alternatively, α-syn proteins that bind to either lipid or proteins in the outer cell membrane could conceivably enter cells in a nonspecific fashion during the perpetual renewal of membrane proteins. More specifically, in HeLa cells64 and yeast,65 α-syn can be associated with lipid rafts, where subsets of proteins and lipids concentrate, thereby creating signaling platforms at the cell surface. Interaction of α-syn with the ganglioside GM1, an essential component of the lipid rafts, has been proposed to mediate its recruitment to these structures.66 This lipid raft-mediated endocytosis has been proposed to mediate internalization of Aβ peptide by primary neurons67 and extracellular α-syn by microglial cells.68 Whether such a mechanism could also mediate α-syn uptake by neuronal cells remains to be investigated (Figure 2b).
Uptake of oligomeric and fibrillar α-syn is not necessarily analogous to that of monomeric α-syn. For high-order species of α-syn to enter cells, a more classical endocytic process has been proposed (Figure 2b). Uptake of oligomers and fibrils of α-syn is attenuated by both low temperature and inhibitors of dynamin.11, 16 Treatment of the cell surface with trypsin, resulting in removal of potential endocytosis receptor proteins, inhibits uptake of α-syn.9 Furthermore, α-syn colocalizes with GTPases Rab5a and Rab7 (Desplats et al.12), and dominant-negative Rab5a has been shown to reduce endocytosis of α-syn. In fact, the ability of cells to take up α-syn has perhaps evolved so they can reduce a potentially toxic extracellular load of α-syn by taking the protein up and degrading it.11 Of course, this uptake and destroy mechanism will work efficiently only if cells are healthy enough to degrade and clear pathogenic proteins, which is not always the case—as we discuss below.
Finally, it should be underlined that whereas passive diffusion through the plasma membrane and exosome-mediated delivery of α-syn into the recipient cell could lead to direct access of α-syn to the cytosol, endocytosis-imported α-syn would enter cells associated with vesicles, with the lumen, or in close apposition to the membrane. In order to interact with other intracellular proteins and/or exert its cytotoxic effect, α-syn likely must exit these compartments through an unknown mechanism that remains to be elucidated (Figure 2b).
Much recent work has focused on the detrimental effects of internalized α-syn on the recipient cell. We will briefly review the experimental proof that α-syn derived from the extracellular space can damage cells and then discuss possible underlying mechanisms.
Induction of aggregation inside the recipient cells
Several groups recently reported that α-syn taken up from the extracellular space induces the aggregation of other α-syn proteins expressed by the recipient cells within the cytoplasm of these cells.16, 69, 70, 71, 72, 73 Typically, investigators used recombinant α-syn proteins as the source of extracellular α-syn, either in oligomeric69, 70 or fibrillar conformation.71, 72, 73 In these cases, they observed the induced formation of intracellular inclusions containing both endogenous and exogenous α-syn proteins71, 72, 73 and mimicking some of the histological features of Lewy bodies. These inclusions were mainly perinuclear,71, 72 positive for ubiquitin, and labeled with thioflavine S,71, 72, 73 indicating the presence of β-sheet-rich structures. The filamentous structure of the material in the inclusions was confirmed by electron microscopy analysis,71, 72 which also revealed vesicles71 within the deposits. These Lewy body-like structures contained misfolded and phosphorylated α-syn,71, 72, 73 whose origin, endogenous71, 73 or exogenous,72 differs among the reports. Finally, the chaperones Hsp70 and Hsp90 have also been detected within these inclusions.71 Notably, reliance on unusual protocols of unclear physiological relevance seems to be necessary to observe these induced α-syn inclusions over short time periods (hours to days). For example, Danzer et al.69, 70 designed different protocols to produce varying kinds of α-syn oligomers, but only one led to formation of intracellular α-syn inclusions when added to the culture medium of neuroblastoma cells. The use of iron chloride in this protocol, as well as extensive shaking and ultracentrifugation steps, brings into question the physiological significance of such oligomers. Similarly, other investigators used cationic liposomes,71 calcium phosphate,73 or lipofectamine72 in order to achieve artificially significant entry of extracellular α-syn fibrils into cells. Because of the highly artificial methods used to promote entry of α-syn, the relevance of these in vitro results to physiological systems is unclear. In contrast, we recently found that, in the absence of facilitating agents, α-syn produced by cultured neuroblastoma cells could enter neighboring cells and interact with cytoplasmic α-syn within small aggregates in the recipient cell.16
By analogy with prion protein, a so-called ‘nucleation’ or ‘seeding’ activity of internalized α-syn is usually invoked to explain the induction of aggregation of cytoplasmic α-syn proteins in the recipient cell after uptake of extracellular α-syn. In other words, after passage from the extracellular to the intracellular compartment, exogenous misfolded α-syn protein could recruit natively unfolded α-syn proteins expressed by the recipient cell, act as a template, and induce their conversion into misfolded forms that will aggregate around a core of transmitted protein (Figure 3). However, is this seeding effect of intercellularly transferred α-syn the only possible explanation for the appearance of aggregates containing both exogenous and endogenous α-syn?
Two models for induction of endogenous α-synuclein aggregation after transfer of exogenous α-synuclein to the recipient cell. Step 1. Exogenous α-syn (in red), whose precise nature (monomer and/or more aggregated form) remains to be determined, is transferred to a recipient cell expressing endogenous α-syn (in blue). In this healthy cell, proteasomal and lysosomal machineries handle α-syn degradation. Steps 2A and 3A. In the first model (‘increase of intracellular α-syn concentration’), the entry of extracellular α-syn increases the intracellular concentration of α-syn. This could overload the degradation systems and lead to their impairment, which in turn would raise even more the intracellular concentration of α-syn and favor the formation of big α-syn aggregates (step 4). Steps 2B and 3B. Alternatively, in the second model (‘nucleation/seeding process’), the misfolded exogenous α-syn seed recruits the unfolded endogenous α-syn and induces its misfolding. In a last step, these endogenous misfolded forms of α-syn aggregate around the core of exogenous α-syn, leading to the formation of fibrils made up of both exo- and endo-genous α-syn (step 4)
The topology of the induced aggregates argues in favor of this nucleation mechanism. It has been reported that the core of induced inclusions consists of transferred α-syn surrounded by an additional layer of cytoplasmic α-syn present in the recipient cells.16, 71 Moreover, the unaltered ability of amino- or carboxy-terminal truncated forms of exogenous α-syn to ‘seed’ the aggregation of intercellularly expressed α-syn proteins71, 73 shows that the central portion of α-syn, containing the hydrophobic domain critical for α-syn fibrillization in vitro, is sufficient to induce aggregation in recipient cells. In addition, protein transfection of full-length and non-mutated α-syn fibrils into cells expressing α-syn proteins lacking this hydrophobic sequence71, 73 or bearing mutations known to abrogate fibril formation in vitro73 does not lead to the formation of intracellular α-syn inclusions. These results suggest that in vitro nucleation-dependent fibrillization of α-syn and formation of intracellular α-syn inclusions may be governed by the same mechanisms and thus support the seeding theory of induction of α-syn aggregation following intercellular transfer of misfolded α-syn.
To further interrogate this hypothesis, it would be interesting to investigate whether loading of recipient cells with above-mentioned mutated or truncated proteins, unable to induce formation of α-syn fibrils in vitro, would still lead to aggregation of endogenous wild-type α-syn in the recipient cell. The absence of seeding phenomenon in such conditions would argue in favor of the nucleation hypothesis, whereas an unaltered effect would suggest that an alternative mechanism could contribute to this induction of α-syn aggregation. Indeed, one could argue that induction of aggregation of cytoplasmic α-syn after entry of exogenous α-syn proteins into recipient cells simply results from an increase of concentration of intracellular α-syn (Figure 3). However, the amounts of α-syn that enter cells from the extracellular space appear to be relatively small, compared with the endogenous levels. On the other hand, it could be hypothesized that a modest elevation of intracellular α-syn level leads to overloading, if not dysfunction, of the normal degradation systems (Figure 3), which will in turn further raise the intracellular concentration of α-syn and favor aggregation. This hypothesis seems even more relevant if the imported form of α-syn is misfolded, as aggregated or abnormal forms of α-syn have been shown to impair the ubiquitin-proteasome system.74, 75, 76, 77 In accordance with this alternative mechanism, impairment of proteasome activity, coupled with formation of intracellular α-syn inclusions, was recently reported to occur in recipient cells following introduction of exogenous α-syn fibrils.72
Consequences of α-Syn Transfer for the Recipient Cell
Thus far, we have discussed possible mechanisms whereby α-syn might be released, transit between cells, undergo cellular uptake, and give rise to protein aggregation in recipient cells. An important question is what the functional sequelae of such an uptake of extracellular α-syn might be for these cells. In addition to the impairment of proteasome activity mentioned above,72 disruption of the cis-Golgi in cells transduced with recombinant α-syn fibrils has been reported.71 There are reports of cell death in the presence of extracellular α-syn; this cell death is counteracted by inhibition of endocytosis and therefore likely to be dependent upon α-syn uptake.9 Seed-dependent aggregation of α-syn has also been closely correlated to neurotoxicity. Thus, introduction of recombinant α-syn seeds leads to the death of neuroblastoma cells expressing wild-type α-syn proteins that readily aggregate, but not of cells that express a fibrillization-deficient mutant.72 Moreover, absence of nuclear fragmentation, caspase 3 activation, or terminal deoxynucleotidyl transferase dUTP nick end labeling (TUNEL) indicates nonapoptotic cell death.72 In contrast, uptake of cell-derived α-syn leads to apoptosis of the recipient primary cortical neurons, as shown by increased activation of caspase 3 (Desplats et al.12 and Danzer et al.13) and caspase 7 (Danzer et al.13). Interestingly, Emmanouilidou et al.14 also report the death of neuroblastoma cells and primary cortical neurons after treatment with cell-produced α-syn. However, this cell death occurs without detectable uptake of exogenous α-syn, suggesting a different, unknown toxic mechanism mediated by α-syn at the cell surface.14 Neurodegeneration induced by intercellular transfer of α-syn has also been proposed to occur in vivo. Mouse cortical neural stem cells transplanted in the brains of transgenic mice expressing human α-syn take up human α-syn from the host tissue and express activated caspase 3, whereas cells grafted into wild-type hosts do not exhibit this sign of apoptotic cell death.12
Intercellular Transfer of α-Syn in Animal Models
Very recent studies have shed light on the possibility that the in vitro mechanisms discussed above operate in a similar fashion in vivo. As mentioned briefly above, Desplats et al.12 addressed the host-to-graft transmission hypothesis by demonstrating transfer of α-syn from α-syn-overexpressing mouse brain to an intrahippocampal graft of cortical neural stem cells. In a recent report, analogous to the human grafting studies, we demonstrate that embryonic mouse dopaminergic neurons grafted in the striata of human α-syn-expressing mice take up host human α-syn16 (Figure 2). In addition, we have shown that rodent cortical neurons internalize stereotactically injected recombinant monomeric, oligomeric, and fibrillar α-syn, and furthermore, that the endocytosis inhibitor dynasore partially blocks this uptake in vivo.16 However, no in vivo study has so far presented evidence that transferred α-syn can trigger the formation of Lewy bodies. Ongoing experimental studies will likely clarify whether Lewy bodies can form as the result of cell-to-cell transfer of α-syn in vivo and will thereby shed light on how PD pathology spreads in the human brain.
Clues from Other Diseases
α-Syn as well as mutant huntingtin (Htt), superoxide dismutase-1 (SOD-1), and Tau proteins or Aβ peptide belong to a class of proteins whose abnormal aggregation plays a central role in neurodegenerative diseases called proteinopathies, which are, respectively, PD, Huntington's disease, amyotrophic lateral sclerosis (ALS), tauopathies, and Alzheimer's disease (AD). The observed intercellular transfer and seeding abilities of each of these proteins recall some of the features of PrPsc and thus leads to their classification as ‘prion-like’ proteins or ‘prionoids’.35, 36, 37, 38, 39, 40, 41, 42, 43 However, it is important to stress that epidemiological studies have not yet presented any evidence of infectivity for any of these proteinopathies, whereas infectious abilities characterize PrPsc. It is not unlikely that the propagation of β-sheet amyloid structures peculiar to each of these proteins shares some common features. Therefore, studies addressing the mechanisms involved in cell-to-cell transfer of one of the disease-related proteins might be relevant to the others.
Huntington's disease
Huntington's disease is an inherited neurodegenerative disorder caused by the mutation of the HD gene leading to expression of Htt protein with an extended polyglutamine (polyQ) tract. This expanded polyQ leads to the formation of cytoplasmic and intranuclear Htt inclusions in affected neurons. In a study addressing possible prion-like properties of mutant Htt, exogenous aggregates of polypeptides containing 44 glutamines (Q) were added to culture medium. They were taken up by cultured cells expressing Htt with a nonpathogenic polyQ tract (25Q), inducing the aggregation of the 25Q-Htt, which normally should not fibrillize.78 These results support the theory of a seeding process. The nucleation capacity of mutated Htt was recently further documented by a novel technique where the fluorescence signal within cultured cells was correlated to the extent of Htt exon 1 protein aggregation.79 This technique allowed live visualization of formation of large Htt exon 1 aggregates within cells, as well as recruitment of dimers and oligomers and cell-to-cell transfer of 103Q Htt exon 1 protein.79 Finally, the incapacity of other amyloid aggregates, such as the prion domain of the yeast Sup35 prion protein or Aβ, to nucleate wild-type Htt underscores the importance of sequence specificity for the nucleation of polyQ fibrils.78 Such specificity may likely also apply to intracellular nucleation-dependent seeding of α-syn, but it remains to be investigated.
Amyotrophic lateral sclerosis
ALS, a neurodegenerative disease specifically affecting motor neurons, leads to death within 3 to 5 years after diagnosis. Mutations in SOD-1 account for many of the inherited ALS cases, which represent only ∼10% of the total incidence. SOD-1 protein is one of the components of the non-amyloid cytoplasmic aggregates that form in affected motor neurons. Recently, not only in vitro-induced fibrils of recombinant SOD-1 proteins, but also spinal cord homogenates from a transgenic mouse model overexpressing mutant human SOD-1 have been shown to seed aggregation of wild-type and mutant SOD-1 proteins in a test tube.80 These results demonstrate the nucleation capacity of SOD-1 proteins derived from an in vivo model. More recently, in vitro-induced aggregates of mutant SOD-1 proteins produced in insect cells have been shown to be internalized by neuroblastoma cells, seed the aggregation of otherwise soluble mutant SOD-1 proteins expressed by these cells, and finally, to transfer from one cell to another independently of cell-to-cell contact.81 Whereas the exogenous seeds progressively disappear when the cells divide, the induced aggregation of endogenous mutant SOD-1 is a persistent and heritable phenotype.81 Interestingly, extracellular mutant SOD-1 aggregates use lipid raft-dependent macropinocytosis to enter cells,81 a process that could be worth examining as a α-syn cell-to-cell transfer mechanism.
Tauopathies
Tau is a microtubule-associated protein that aggregates in its hyperphosphorylated form to generate intraneuronal tangles during progression of neurodegenerative diseases named tauopathies, including AD. In similar cell culture paradigms as for α-syn, cellular uptake of exogenous mutant Tau coupled to seeding activity has been shown in vitro.82 Recent in vivo studies have provided further support for the notion that seeding activity of misfolded Tau is an important pathogenic event. Intracerebral injection of brain extracts from transgenic mice displaying abundant filamentous Tau inclusions into mice expressing wild-type human Tau induced Tau pathology around the site of injection. Importantly, in these mice that normally do not develop Tau depositions, neighboring brain regions also exhibited Tau inclusions.83 Interestingly, studies identified a polymorphism in the gene MAPT, encoding Tau protein, as a risk factor for idiopathic PD in the same GWAS that showed a strong association between PD susceptibility and SNPs in the SNCA gene.6, 7, 8 The possibility of a link between these genetic observations and the prion-like properties shared by these two proteins may be worth exploring. The observed synergy between the in vitro mixture of purified α-syn and Tau proteins in promoting cross-fibrillization84 could be a good starting point.
Alzheimer's disease
In vivo seeding experiments, comparable with the ones described above for Tau, were previously performed using Aβ, whose misfolded and aggregated forms contribute to extracellular amyloid plaques in AD. Misfolded Aβ proteins contained in brain extracts from AD patients or aged transgenic amyloid precursor protein (APP) mice seed the deposition of Aβ in young APP mice that normally would not display Aβ aggregates.85 Similarly, soluble recombinant Aβ oligomers, infused in the hippocampus of APP mice, contribute to growth of pre-existing plaques and seed formation of new plaques.86 This work is the first readily visualized evidence for a seeding effect of an amyloid protein in vivo, revealing a core of injected seed surrounded by endogenous material. The ability of Aβ and Tau to induce aggregation of endogenous proteins after intracerebral injections may suggest that α-syn could also display seeding capacity in vivo, even if this property has yet to be properly demonstrated. Finally, in contrast to oral, intravenous, intraocular, and intranasal inoculation of Aβ-containing brain extracts, which do not lead to any detectable cerebral amyloidosis,87 intraperitoneal injections of these extracts are able to induce Aβ deposition in the brains of young transgenic APP mice after a 7-month incubation period.88 These results suggest that transport of Aβ from periphery to brain can occur and might be a first step in questioning the presumed noninfectious features of AD. Whether such mechanisms are also relevant for α-syn and PD is worth examining.
Concluding Remarks
As delineated above, many possibilities exist for each step of the process by which pathogenic α-syn might transfer from one cell to another and cause deadly consequences to the recipient cell. The requirements for this process include exit of α-syn from the host cell, transit to the recipient cell, entry into this new cell, and triggering of a toxic cascade inside the recipient cell. If these mechanisms are specific to α-syn and PD, then there exist many points at which to interfere in the pathogenic process in attempts to develop much-needed therapies that retard PD development.
Several strategies are likely to be the subject of intensive research in the future. For example, immunotherapy targeting extracellular α-syn89 and leading to the removal by the immune system of the seeds in transit between cells may stop or at least delay the propagation of α-syn pathology in the brains of people with PD. However, a better knowledge of the precise nature of the seed is needed in order to design specific antibodies that spare the normal function of α-syn. Specific inhibitors of α-syn aggregation appear also promising, as they may interfere with seeding activity of transmitted α-syn. Particularly, short peptides targeting the binding region of α-syn responsible for self-aggregation have been reported to prevent α-syn oligomerization and fibrillization in a test tube90, 91 and could lead to development of peptide-based inhibitors of α-syn aggregation.
Overall, the connections between α-syn and PD are strong and the power in determining whether the specific steps we discussed above are accurate and relevant goes far beyond PD. If these mechanisms are conserved across many neurodegenerative diseases, multiple methods of investigation both currently in place and also under development now could eventually lead to novel therapies for very large groups of patients.
Abbreviations
- PD:
-
Parkinson's disease
- α-syn:
-
α-synuclein
- SNCA :
-
α-synuclein gene
- GWAS:
-
genome-wide association study
- SNP:
-
single-nucleotide polymorphism
- Hsp70:
-
heat shock protein 70
- TUNEL:
-
terminal deoxynucleotidyl transferase dUTP nick end labeling
- PrPsc:
-
scrapie form of prion protein
- TNT:
-
tunneling nanotube
- Htt :
-
Huntingtin gene
- Htt:
-
Huntingtin protein
- SOD-1:
-
superoxide dismutase 1
- ALS:
-
amyotrophic lateral sclerosis
- Aβ:
-
β-amyloid protein
- AD:
-
Alzheimer's disease
- PolyQ:
-
polyglutamine
- APP:
-
amyloid precursor protein
References
Polymeropoulos MH, Lavedan C, Leroy E, Ide SE, Dehejia A, Dutra A et al. Mutation in the alpha-synuclein gene identified in families with Parkinson's disease. Science 1997; 276: 2045–2047.
Krüger R, Kuhn W, Muller T, Woitalla D, Graeber M, Kosel S et al. Ala30Pro mutation in the gene encoding alpha-synuclein in Parkinson's disease. Nat Genet 1998; 18: 106–108.
Singleton AB, Farrer M, Johnson J, Singleton A, Hague S, Kachergus J et al. alpha-Synuclein locus triplication causes Parkinson's disease. Science 2003; 302: 841.
Zarranz JJ, Alegre J, Gomez-Esteban JC, Lezcano E, Ros R, Ampuero I et al. The new mutation, E46K, of alpha-synuclein causes Parkinson and Lewy body dementia. Ann Neurol 2004; 55: 164–173.
Chartier-Harlin MC, Kachergus J, Roumier C, Mouroux V, Douay X, Lincoln S et al. Alpha-synuclein locus duplication as a cause of familial Parkinson's disease. Lancet 2004; 364: 1167–1169.
Satake W, Nakabayashi Y, Mizuta I, Hirota Y, Ito C, Kubo M et al. Genome-wide association study identifies common variants at four loci as genetic risk factors for Parkinson's disease. Nat Genet 2009; 41: 1303–1307.
Simon-Sanchez J, Schulte C, Bras JM, Sharma M, Gibbs JR, Berg D et al. Genome-wide association study reveals genetic risk underlying Parkinson's disease. Nat Genet 2009; 41: 1308–1312.
Edwards TL, Scott WK, Almonte C, Burt A, Powell EH, Beecham GW et al. Genome-wide association study confirms SNPs in SNCA and the MAPT region as common risk factors for Parkinson disease. Ann Hum Genet 2010; 74: 97–109.
Sung JY, Kim J, Paik SR, Park JH, Ahn YS, Chung KC . Induction of neuronal cell death by Rab5A-dependent endocytosis of alpha-synuclein. J Biol Chem 2001; 276: 27441–27448.
Lee HJ, Patel S, Lee SJ . Intravesicular localization and exocytosis of alpha-synuclein and its aggregates. J Neurosci 2005; 25: 6016–6024.
Lee HJ, Suk JE, Bae EJ, Lee JH, Paik SR, Lee SJ . Assembly-dependent endocytosis and clearance of extracellular alpha-synuclein. Int J Biochem Cell Biol 2008; 40: 1835–1849.
Desplats P, Lee HJ, Bae EJ, Patrick C, Rockenstein E, Crews L et al. Inclusion formation and neuronal cell death through neuron-to-neuron transmission of alpha-synuclein. Proc Natl Acad Sci USA 2009; 106: 13010–13015.
Danzer KM, Ruf WP, Putcha P, Joyner D, Hashimoto T, Glabe C et al. Heat-shock protein 70 modulates toxic extracellular {alpha}-synuclein oligomers and rescues trans-synaptic toxicity. FASEB J 2010; 25: 326–336.
Emmanouilidou E, Melachroinou K, Roumeliotis T, Garbis SD, Ntzouni M, Margaritis LH et al. Cell-produced alpha-synuclein is secreted in a calcium-dependent manner by exosomes and impacts neuronal survival. J Neurosci 2010; 30: 6838–6851.
Jang A, Lee HJ, Suk JE, Jung JW, Kim KP, Lee SJ . Non-classical exocytosis of alpha-synuclein is sensitive to folding states and promoted under stress conditions. J Neurochem 2010; 113: 1263–1274.
Hansen C, Angot E, Bergström AL, Steiner JA, Pieri L, Paul G et al. Alpha-Synuclein propagates from mouse brain to grafted dopaminergic neurons and seeds aggregation in cultured human cells. J Clin Invest 2011; 121: 715–725.
Hawkes CH, Del Tredici K, Braak H . Parkinson's disease: a dual-hit hypothesis. Neuropathol Appl Neurobiol 2007; 33: 599–614.
Kordower JH, Chu Y, Hauser RA, Freeman TB, Olanow CW . Lewy body-like pathology in long-term embryonic nigral transplants in Parkinson's disease. Nat Med 2008; 14: 504–506.
Kordower JH, Chu Y, Hauser RA, Olanow CW, Freeman TB . Transplanted dopaminergic neurons develop PD pathologic changes: a second case report. Mov Disord 2008; 23: 2303–2306.
Li JY, Englund E, Holton JL, Soulet D, Hagell P, Lees AJ et al. Lewy bodies in grafted neurons in subjects with Parkinson's disease suggest host-to-graft disease propagation. Nat Med 2008; 14: 501–503.
Li JY, Englund E, Widner H, Rehncrona S, Bjorklund A, Lindvall O et al. Characterization of Lewy body pathology in 12- and 16-year-old intrastriatal mesencephalic grafts surviving in a patient with Parkinson's disease. Mov Disord 2010; 25: 1091–1096.
Mata IF, Shi M, Agarwal P, Chung KA, Edwards KL, Factor SA et al. SNCA variant associated with Parkinson disease and plasma alpha-synuclein level. Arch Neurol 2010; 67: 1350–1356.
Spillantini MG, Schmidt ML, Lee VM, Trojanowski JQ, Jakes R, Goedert M . Alpha-synuclein in Lewy bodies. Nature 1997; 388: 839–840.
Fujiwara H, Hasegawa M, Dohmae N, Kawashima A, Masliah E, Goldberg MS et al. alpha-Synuclein is phosphorylated in synucleinopathy lesions. Nat Cell Biol 2002; 4: 160–164.
Neumann M, Kahle PJ, Giasson BI, Ozmen L, Borroni E, Spooren W et al. Misfolded proteinase K-resistant hyperphosphorylated alpha-synuclein in aged transgenic mice with locomotor deterioration and in human alpha-synucleinopathies. J Clin Invest 2002; 110: 1429–1439.
Conway KA, Harper JD, Lansbury PT . Accelerated in vitro fibril formation by a mutant alpha-synuclein linked to early-onset Parkinson disease. Nat Med 1998; 4: 1318–1320.
Giasson BI, Uryu K, Trojanowski JQ, Lee VM . Mutant and wild type human alpha-synucleins assemble into elongated filaments with distinct morphologies in vitro. J Biol Chem 1999; 274: 7619–7622.
Hashimoto M, Hsu LJ, Sisk A, Xia Y, Takeda A, Sundsmo M et al. Human recombinant NACP/alpha-synuclein is aggregated and fibrillated in vitro: relevance for Lewy body disease. Brain Res 1998; 799: 301–306.
Wood SJ, Wypych J, Steavenson S, Louis JC, Citron M, Biere AL . alpha-synuclein fibrillogenesis is nucleation-dependent. Implications for the pathogenesis of Parkinson's disease. J Biol Chem 1999; 274: 19509–19512.
Uversky VN . Mysterious oligomerization of the amyloidogenic proteins. FEBS J 2010; 277: 2940–2953.
Olanow CW, Perl DP, DeMartino GN, McNaught KS . Lewy-body formation is an aggresome-related process: a hypothesis. Lancet Neurol 2004; 3: 496–503.
Brundin P, Barker RA, Parmar M . Neural grafting in Parkinson's disease: problems and possibilities. Prog Brain Res 2010; 184: 265–294.
Braak H, Del Tredici K, Bratzke H, Hamm-Clement J, Sandmann-Keil D, Rüb U . Staging of the intracerebral inclusion body pathology associated with idiopathic Parkinson's disease (preclinical and clinical stages). J Neurol 2002; 249 (Suppl 3): III/1–III/5.
Brundin P, Li JY, Holton JL, Lindvall O, Revesz T . Research in motion: the enigma of Parkinson's disease pathology spread. Nat Rev Neurosci 2008; 9: 741–745.
Aguzzi A . Cell biology: beyond the prion principle. Nature 2009; 459: 924–925.
Aguzzi A, Rajendran L . The transcellular spread of cytosolic amyloids, prions, and prionoids. Neuron 2009; 64: 783–790.
Angot E, Brundin P . Dissecting the potential molecular mechanisms underlying alpha-synuclein cell-to-cell transfer in Parkinson's disease. Parkinsonism Relat Disord 2009; 15 (Suppl 3): S143–S147.
Krammer C, Schatzl HM, Vorberg I . Prion-like propagation of cytosolic protein aggregates: insights from cell culture models. Prion 2009; 3: 206–212.
Olanow CW, Prusiner SB . Is Parkinson's disease a prion disorder? Proc Natl Acad Sci USA 2009; 106: 12571–12572.
Angot E, Steiner JA, Hansen C, Li JY, Brundin P . Are synucleinopathies prion-like disorders? Lancet Neurol 2010; 9: 1128–1138.
Brundin P, Melki R, Kopito R . Prion-like transmission of protein aggregates in neurodegenerative diseases. Nat Rev Mol Cell Biol 2010; 11: 301–307.
Frost B, Diamond MI . Prion-like mechanisms in neurodegenerative diseases. Nat Rev Neurosci 2010; 11: 155–159.
Lee SJ, Desplats P, Sigurdson C, Tsigelny I, Masliah E . Cell-to-cell transmission of non-prion protein aggregates. Nat Rev Neurol 2010; 6: 702–706.
El-Agnaf OM, Salem SA, Paleologou KE, Cooper LJ, Fullwood NJ, Gibson MJ et al. Alpha-synuclein implicated in Parkinson's disease is present in extracellular biological fluids, including human plasma. FASEB J 2003; 17: 1945–1947.
El-Agnaf OM, Salem SA, Paleologou KE, Curran MD, Gibson MJ, Court JA et al. Detection of oligomeric forms of alpha-synuclein protein in human plasma as a potential biomarker for Parkinson's disease. FASEB J 2006; 20: 419–425.
Tokuda T, Salem SA, Allsop D, Mizuno T, Nakagawa M, Qureshi MM et al. Decreased alpha-synuclein in cerebrospinal fluid of aged individuals and subjects with Parkinson's disease. Biochem Biophys Res Commun 2006; 349: 162–166.
Devic I, Hwang H, Edgar JS, Izutsu K, Presland R, Pan C et al. Salivary alpha-synuclein and DJ-1: potential biomarkers for Parkinson's disease. Brain 2011; e-pub ahead of print 24 February 2011.
Pan T, Kondo S, Le W, Jankovic J . The role of autophagy-lysosome pathway in neurodegeneration associated with Parkinson's disease. Brain 2008; 131: 1969–1978.
Alvarez-Erviti L, Seow Y, Schapira AH, Gardiner C, Sargent IL, Wood MJ et al. Lysosomal dysfunction increases exosome-mediated alpha-synuclein release and transmission. Neurobiol Dis 2011; 42: 360–367.
Fader CM, Sanchez D, Furlan M, Colombo MI . Induction of autophagy promotes fusion of multivesicular bodies with autophagic vacuoles in k562 cells. Traffic 2008; 9: 230–250.
Simons M, Raposo G . Exosomes--vesicular carriers for intercellular communication. Curr Opin Cell Biol 2009; 21: 575–581.
Fevrier B, Vilette D, Archer F, Loew D, Faigle W, Vidal M et al. Cells release prions in association with exosomes. Proc Natl Acad Sci USA 2004; 101: 9683–9688.
Fevrier B, Vilette D, Laude H, Raposo G . Exosomes: a bubble ride for prions? Traffic 2005; 6: 10–17.
Vella LJ, Sharples RA, Lawson VA, Masters CL, Cappai R, Hill AF . Packaging of prions into exosomes is associated with a novel pathway of PrP processing. J Pathol 2007; 211: 582–590.
Rajendran L, Honsho M, Zahn TR, Keller P, Geiger KD, Verkade P et al. Alzheimer's disease beta-amyloid peptides are released in association with exosomes. Proc Natl Acad Sci USA 2006; 103: 11172–11177.
Sung JY, Park SM, Lee CH, Um JW, Lee HJ, Kim J et al. Proteolytic cleavage of extracellular secreted {alpha}-synuclein via matrix metalloproteinases. J Biol Chem 2005; 280: 25216–25224.
Choi DH, Kim YJ, Kim YG, Joh TH, Beal MF, Kim YS . The role of matrix metalloproteinase 3-mediated alpha-synuclein cleavage in dopaminergic cell death. J Biol Chem 2011; 286: 14168–14177.
Gousset K, Schiff E, Langevin C, Marijanovic Z, Caputo A, Browman DT et al. Prions hijack tunnelling nanotubes for intercellular spread. Nat Cell Biol 2009; 11: 328–336.
Jensen PH, Nielsen MS, Jakes R, Dotti CG, Goedert M . Binding of alpha-synuclein to brain vesicles is abolished by familial Parkinson's disease mutation. J Biol Chem 1998; 273: 26292–26294.
Jensen PH, Li JY, Dahlstrom A, Dotti CG . Axonal transport of synucleins is mediated by all rate components. Eur J Neurosci 1999; 11: 3369–3376.
Utton MA, Noble WJ, Hill JE, Anderton BH, Hanger DP . Molecular motors implicated in the axonal transport of tau and alpha-synuclein. J Cell Sci 2005; 118: 4645–4654.
Auluck PK, Caraveo G, Lindquist S . alpha-Synuclein: membrane interactions and toxicity in Parkinson's disease. Annu Rev Cell Dev Biol 2010; 26: 211–233.
Ahn KJ, Paik SR, Chung KC, Kim J . Amino acid sequence motifs and mechanistic features of the membrane translocation of alpha-synuclein. J Neurochem 2006; 97: 265–279.
Fortin DL, Troyer MD, Nakamura K, Kubo S, Anthony MD, Edwards RH . Lipid rafts mediate the synaptic localization of alpha-synuclein. J Neurosci 2004; 24: 6715–6723.
Zabrocki P, Bastiaens I, Delay C, Bammens T, Ghillebert R, Pellens K et al. Phosphorylation, lipid raft interaction and traffic of alpha-synuclein in a yeast model for Parkinson. Biochim Biophys Acta 2008; 1783: 1767–1780.
Martinez Z, Zhu M, Han S, Fink AL . GM1 specifically interacts with alpha-synuclein and inhibits fibrillation. Biochemistry (Mosc) 2007; 46: 1868–1877.
Saavedra L, Mohamed A, Ma V, Kar S, de Chaves EP . Internalization of beta-amyloid peptide by primary neurons in the absence of apolipoprotein E. J Biol Chem 2007; 282: 35722–35732.
Park JY, Kim KS, Lee SB, Ryu JS, Chung KC, Choo YK et al. On the mechanism of internalization of alpha-synuclein into microglia: roles of ganglioside GM1 and lipid raft. J Neurochem 2009; 110: 400–411.
Danzer KM, Haasen D, Karow AR, Moussaud S, Habeck M, Giese A et al. Different species of alpha-synuclein oligomers induce calcium influx and seeding. J Neurosci 2007; 27: 9220–9232.
Danzer KM, Krebs SK, Wolff M, Birk G, Hengerer B . Seeding induced by alpha-synuclein oligomers provides evidence for spreading of alpha-synuclein pathology. J Neurochem 2009; 111: 192–203.
Luk KC, Song C, O’Brien P, Stieber A, Branch JR, Brunden KR et al. Exogenous alpha-synuclein fibrils seed the formation of Lewy body-like intracellular inclusions in cultured cells. Proc Natl Acad Sci USA 2009; 106: 20051–20056.
Nonaka T, Watanabe ST, Iwatsubo T, Hasegawa M . Seeded aggregation and toxicity of {alpha}-synuclein and tau: cellular models of neurodegenerative diseases. J Biol Chem 2010; 285: 34885–34898.
Waxman EA, Giasson BI . A novel, high-efficiency cellular model of fibrillar alpha-synuclein inclusions and the examination of mutations that inhibit amyloid formation. J Neurochem 2010; 113: 374–388.
Stefanis L, Larsen KE, Rideout HJ, Sulzer D, Greene LA . Expression of A53T mutant but not wild-type alpha-synuclein in PC12 cells induces alterations of the ubiquitin-dependent degradation system, loss of dopamine release, and autophagic cell death. J Neurosci 2001; 21: 9549–9560.
Snyder H, Mensah K, Theisler C, Lee J, Matouschek A, Wolozin B . Aggregated and monomeric alpha-synuclein bind to the S6′ proteasomal protein and inhibit proteasomal function. J Biol Chem 2003; 278: 11753–11759.
Lindersson E, Beedholm R, Hojrup P, Moos T, Gai W, Hendil KB et al. Proteasomal inhibition by alpha-synuclein filaments and oligomers. J Biol Chem 2004; 279: 12924–12934.
Emmanouilidou E, Stefanis L, Vekrellis K . Cell-produced alpha-synuclein oligomers are targeted to, and impair, the 26S proteasome. Neurobiol Aging 2010; 31: 953–968.
Ren PH, Lauckner JE, Kachirskaia I, Heuser JE, Melki R, Kopito RR . Cytoplasmic penetration and persistent infection of mammalian cells by polyglutamine aggregates. Nat Cell Biol 2009; 11: 219–225.
Herrera F, Tenreiro S, Miller-Fleming L, Outeiro TF . Visualization of cell-to-cell transmission of mutant huntingtin oligomers. PLoS Curr 2011; 3: RRN1210.
Chia R, Tattum MH, Jones S, Collinge J, Fisher EM, Jackson GS . Superoxide dismutase 1 and tgSOD1 mouse spinal cord seed fibrils, suggesting a propagative cell death mechanism in amyotrophic lateral sclerosis. PLoS One 2010; 5: e10627.
Münch C, O’Brien J, Bertolotti A . Prion-like propagation of mutant superoxide dismutase-1 misfolding in neuronal cells. Proc Natl Acad Sci USA 2011; 108: 3548–3553.
Frost B, Jacks RL, Diamond MI . Propagation of tau misfolding from the outside to the inside of a cell. J Biol Chem 2009; 284: 12845–12852.
Clavaguera F, Bolmont T, Crowther RA, Abramowski D, Frank S, Probst A et al. Transmission and spreading of tauopathy in transgenic mouse brain. Nat Cell Biol 2009; 11: 909–913.
Giasson BI, Forman MS, Higuchi M, Golbe LI, Graves CL, Kotzbauer PT et al. Initiation and synergistic fibrillization of tau and alpha-synuclein. Science 2003; 300: 636–640.
Meyer-Luehmann M, Coomaraswamy J, Bolmont T, Kaeser S, Schaefer C, Kilger E et al. Exogenous induction of cerebral beta-amyloidogenesis is governed by agent and host. Science 2006; 313: 1781–1784.
Gaspar RC, Villarreal SA, Bowles N, Hepler RW, Joyce JG, Shughrue PJ . Oligomers of beta-amyloid are sequestered into and seed new plaques in the brains of an AD mouse model. Exp Neurol 2010; 223: 394–400.
Eisele YS, Bolmont T, Heikenwalder M, Langer F, Jacobson LH, Yan ZX et al. Induction of cerebral beta-amyloidosis: intracerebral versus systemic Abeta inoculation. Proc Natl Acad Sci USA 2009; 106: 12926–12931.
Eisele YS, Obermuller U, Heilbronner G, Baumann F, Kaeser SA, Wolburg H et al. Peripherally applied Abeta-containing inoculates induce cerebral beta-amyloidosis. Science 2010; 330: 980–982.
Villoslada P, Moreno B, Melero I, Pablos JL, Martino G, Uccelli A et al. Immunotherapy for neurological diseases. Clin Immunol 2008; 128: 294–305.
El-Agnaf OM, Paleologou KE, Greer B, Abogrein AM, King JE, Salem SA et al. A strategy for designing inhibitors of alpha-synuclein aggregation and toxicity as a novel treatment for Parkinson's disease and related disorders. FASEB J 2004; 18: 1315–1317.
Madine J, Doig AJ, Middleton DA . Design of an N-methylated peptide inhibitor of alpha-synuclein aggregation guided by solid-state NMR. J Am Chem Soc 2008; 130: 7873–7881.
Acknowledgements
We acknowledge the financial support of our research. Our work is supported by the MJ Fox Foundation for Parkinson's Research, Swedish Brain Foundation, Swedish Parkinson Foundation, Söderbergs Foundation, the Swedish Research Council, Anna-Lisa Rosenberg Foundation, and a private donation from Mr Sven Astell. Additionally, JS is supported by the Human Frontier Science Program and EA is supported by the ERA-net Neuron program MIPROTRAN. These funding agencies did not play a role in the preparation of this review.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Edited by G Melino
Rights and permissions
About this article
Cite this article
Steiner, J., Angot, E. & Brundin, P. A deadly spread: cellular mechanisms of α-synuclein transfer. Cell Death Differ 18, 1425–1433 (2011). https://doi.org/10.1038/cdd.2011.53
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/cdd.2011.53
Keywords
This article is cited by
-
MIL-CELL: a tool for multi-scale simulation of yeast replication and prion transmission
European Biophysics Journal (2023)
-
The Relationships Among Metal Homeostasis, Mitochondria, and Locus Coeruleus in Psychiatric and Neurodegenerative Disorders: Potential Pathogenetic Mechanism and Therapeutic Implications
Cellular and Molecular Neurobiology (2023)
-
A breakdown in microglial metabolic reprogramming causes internalization dysfunction of α-synuclein in a mouse model of Parkinson’s disease
Journal of Neuroinflammation (2022)
-
Strong Predictive Algorithm of Pathogenesis-Based Biomarkers Improves Parkinson’s Disease Diagnosis
Molecular Neurobiology (2022)
-
Contribution of syndecans to cellular uptake and fibrillation of α-synuclein and tau
Scientific Reports (2019)