Abstract
Purpose
The aim of this study was to investigate the causes of mortality in individuals with open-angle glaucoma (OAG).
Methods
All-cause mortality data from the Registry of Births, Deaths and Marriages for the Australian state of Tasmania, for all people who were at least 40 years of age at the time of death, were classified using International Classification of Diseases-10 guidelines. This information was cross-referenced to identify participants in the Glaucoma Inheritance Study in Tasmania (GIST) who had died. Contingency tables were used for crude analysis and then models were constructed, adjusting for age at death as well as gender.
Results
Between 1996 and 2005, a total of 33 879 deaths were recorded. Data were unavailable for 4868 (14.4%) people. The mean age at death for the study sample was 78.4±11.5 (range 41–109) years. Of those cases known to have OAG by their participation in GIST (n=2409), full mortality data were available for 741 (92.0%). Following adjustment for the age at death and male gender, the odds ratio for death due to ischaemic heart disease in people with OAG compared to the general population not known to have OAG was significant (OR=1.30, 95% CI: 1.08–1.56; P=0.006). Crude analysis revealed that there were significantly fewer people with OAG who died due to metastatic cancer (P<0.001); however, this did not remain significant following adjustment for age and gender.
Conclusion
The pathoaetiological relationship between OAG and ischaemic heart disease is unclear and requires further investigation. Increased awareness of the association between cardiovascular disease and OAG is warranted.
Similar content being viewed by others
Introduction
Antagonistic pleiotropy, whereby the molecular pathoaetiology for an age-related disease may confer an overall survival benefit before the reproductive age, is one of the peculiar aspects of diseases that typically manifest relatively late in life, such as primary open-angle glaucoma (OAG).1 Unfortunately, such relationships are generally difficult to study. The investigation of all-cause mortality data can provide insight into the phenotypic pleiotropy or significant associations between a systemic disease and another condition.
Glaucoma is the most common cause for irreversible blindness worldwide,2 with approximately 2–3% of people in our community having OAG.3, 4 Previous work has suggested an association between cardiac disease and OAG.5, 6, 7 Analysis of data from the United States National Health Interview Survey revealed an increased risk of mortality due to cardiovascular disease in participants with glaucoma.6 This study also identified a modest association between glaucoma in people without reported visual impairment and cancer.6 However, a limitation of this cross-sectional study was that glaucoma status was determined by self-report.6 Data from the Blue Mountains Eye Study in Australia have suggested that patients with glaucoma younger than 75 years of age have a greater risk of cardiovascular mortality, particularly following exposure to topical timolol.7 However, the conclusion from this work has been criticized because of the relatively small sample size following age stratification.8
In this study we investigated the cause for mortality in a large sample of individuals with OAG. We specifically sought to investigate the association between cardiovascular disease and glaucoma using data from a relatively homogenous, Caucasian population. In our large cohort comprising mortality information from over 27 000 people, of whom 741 were known to have OAG, we identified a modest, yet statistically significant association between death due to ischaemic heart disease and OAG.
Materials and methods
Specific approval for this study was obtained from the ethics committee of the Southern Tasmania Health and Medical Human Research. Written informed consent was obtained from each person clinically examined as part of this study. Raw data were obtained from the Tasmanian Registry of Birth, Deaths and Marriages, for the years December 1996 to December 2005. This database contained re-identifiable demographic details as well as all available data on the cause of death as listed on the medical death certificate for each person registered as deceased in the Australian island state of Tasmania. For the past decade, Tasmania has had a relatively stable population of approximately 500 000 who are predominantly of Anglo-Celtic ancestry.9 All-cause mortality data for individuals who were at least 40 years of age at the time of death were classified using the International Classification of Diseases (ICD)-10 guidelines by one trained grader (PS). This grader was masked to glaucoma status. The ICD-10 coded data were then re-identified and merged with the Glaucoma Inheritance Study in Tasmania (GIST) database.
The GIST has been described in depth previously.10, 11, 12 In brief, separate audits of all patients with glaucoma attending all ophthalmic practices in Tasmania, between 1994 and 1996, were performed. Subsequently, surveys inviting patients to participate in the study were directly mailed to over 3800 Tasmanian patients who had been investigated or treated for glaucoma. Additional surveys were distributed to all optometric and general practitioner clinics. Over 500 OAG index cases were found to have died or relocated from Tasmania before 1996. Initially a total of 2062 participants were examined, with definite OAG being diagnosed in 1700 (82.4%) of these participants.12 Since this original enrolment, an additional 709 people have been reviewed by GIST and diagnosed with OAG.
Study clinicians undertook independent assessments according to a standard examination protocol. One examiner obtained written informed consent, a medical history, measured refraction and then the subject's best-corrected Snellen visual acuities. A detailed questionnaire, covering knowledge of family history; demographic data; and medical history of systemic disorders such as hypertension, diabetes, migraine, corticosteroid use and systemic vascular disease, was administered. Questions related to past ocular disease and treatment, as well as ocular symptoms, were also included. Responses were cross-checked with patients' medications lists and medical summaries. Humphrey automated perimetry (Humphrey Inc., San Leandro, CA, USA) using a 24-2 array, a size III target and full-threshold test system, was performed. Results were reviewed for reliability using fixation losses, false-positive errors, false-negative errors and short-term fluctuations. Visual fields were graded as abnormal if three contiguous regions on pattern standard deviation had a probability of normality of <5%, or if the Glaucoma Hemifield Test was abnormal. Seated intraocular pressure (IOP) was measured using a calibrated Goldmann applanation tonometer (Haag-Streit AG, Bern, Switzerland), and gonioscopy was performed.
All optic discs were scored independently by at least two ophthalmologists who were masked to the patients' supplementary clinical findings. Simultaneous stereo-photographs of the optic discs were taken with a Nidek 3-Dx camera (Nidek, Gamagori, Japan). The vertical and horizontal cup-disc ratio as judged on contour as well as the size of the scleral canal were recorded. The presence of neuroretinal rim thinning, pallor and focal defects; nerve fibre layer defects; Drance-type nerve fibre layer haemorrhages; bayonetting of emerging nerve head vasculature and peripapillary changes to retinal pigment epithelium and choroidal vasculature were also noted. If there was a discrepancy, consensus between the graders was reached through open discussion.
For the purpose of this study, a diagnosis of OAG by a treating ophthalmologist was deemed to be appropriate for inclusion into the GIST database. Confirmation of disease status was performed when examined by the GIST team, where patients with OAG were required to have, in at least one eye, optic disc cupping (cup-disc ratio ⩾0.7); or a 0.2 inter-eye disparity in cup-disc ratio or focal rim notching, with corresponding visual field loss. Subjects were required to have an open iridocorneal angle on gonioscopic examination.
To assess the internal validity in ICD-10 classification, the assigned mortality code was graded twice for 6000 people. An identical all-cause mortality code was assigned on both occasions for 5944 (99.1%) people. Contingency tables of OAG disease status and each specific coded cause of death were used for crude analysis. Subsequent models adjusted for age at death as well as gender. Binary logistic regression analysis was performed using SPSS version 14.0.0 (SPSS Inc., Chicago, IL, USA). The odds ratio was computed as eβ, where β is the regression coefficient of the covariate and the 95% confidence interval was calculated as eβ±1.96 × SEβ, where SEβ is the standard error of the regression coefficient. Nonparametric continuous variables were compared using the Mann–Whitney U-test. Data are presented as the mean±SD.
Statement of ethics
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during this research.
Results
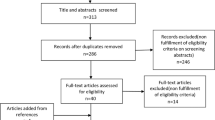
During the defined 9-year study period, a total of 33 879 deaths were recorded. Data were unavailable for 4868 (14.4 %) people (ie those who had incomplete documentation or underwent coronial investigation) and 1725 (5.1%) were younger at the time of death than the designated age (40 years) for inclusion into this study. Hence, information from 27 286 people (80.5% of the full Tasmanian Registry) was reviewed. The mean age at death for the study sample was 78.4±11.5 (range 41–109) years, and this cohort comprised 13 919 (51.0%) women.
A total of 805 patients with OAG were identified by cross tabulation with the GIST database. Full mortality information was available for 741 (92.0%) people known to have OAG, of whom 375 (50.6%) were women (Table 1). The mean age at death for patients with OAG included in this study was 83.8±7.8 years. The 61 patients for whom mortality data were not available were significantly younger at the age of death and enrolment in the GIST compared to those with complete mortality data (Table 1). In the final study population, there was no significant gender difference between people known to have OAG and those not known to have OAG (P=0.82; χ2=0.05). However, people known to have OAG were found to have died at a significantly older age (P<0.0001; z=−13.25).
Pooled analysis of mortality due to all forms of circulatory diseases revealed a significant association with OAG (Table 2). Following adjustment for the age at death and male gender, the odds ratio for death due to ischaemic heart disease in people with OAG was significant (OR=1.30, 95% CI: 1.08–1.56; P=0.006). This association increased when analysis was restricted to people who were less than 80 years of age at their time of death. This finding was not reflected in the pooled analysis of mortality due to all forms of circulatory disease. Although there was a trend towards an association between ischaemic heart disease mortality and OAG in people who were at least 80 years at their time of death, this was not statistically significant. Analysis of other sub-types of circulatory disease mortality revealed no other significant association with OAG. Crude analysis revealed that there were significantly fewer people with OAG who died due to metastatic cancer compared with those not known to have OAG (P<0.0001). However, this association did not remain significant following adjustment for age and gender (Table 2). No association between mortality cause and signs of OAG disease severity, such as cup-disc ratio, age at glaucoma diagnosis or maximum-recorded IOP, was identified (data not shown).
Conclusion
In this study we found that OAG was associated with an increased likelihood of death due to ischaemic heart disease. This effect was strongest when analysis was restricted to data from people who died before the age of 80 years. In this age group, the odds ratio for death due to ischaemic heart disease in patients with OAG was 1.72 (95% CI: 1.13–2.61). This supports previous work, which has identified an association between cardiovascular mortality and glaucoma.5, 6, 7 In a study investigating the cause of mortality in a diabetic population from Wisconsin in the United States, ischaemic heart disease was found to be associated with a history of glaucoma.5 This finding was subsequently supported in two population-based studies where participants were not selected for diabetes status.6, 7
The pathoaetiological relationship between OAG and ischaemic heart disease is unclear. However, it has been postulated that an association could possibly arise as an adverse complication of OAG treatment or due to a common overlapping pathogenic pathway.13 Acetazolamide treatment for OAG is known to be associated with an increased risk of mortality,14 and the systemic effects of other IOP-modulating medications are well established.13 Lee et al7 identified a significant relationship between topical β-blocker use and cardiovascular mortality. Use of acetazolamide and topical β-blocker therapy has decreased in recent years as newer treatments for glaucoma have become available. Unfortunately in our study, longitudinal data pertaining to OAG treatment were not available.
Altered haemodynamics at the optic nerve head is known to be associated with retinal ganglion cell apoptosis,15 and a vascular pathogenic origin for the glaucomas has long been debated.16 It is certainly plausible that some people with glaucoma may have altered haemodynamics of vessels both at the optic nerve head and the heart.17, 18 Interestingly the Myocilin gene, which has been unequivocally implicated in glaucoma and is not known to serve any physiological function, has been found to be highly expressed in the heart.19, 20
Using a clinic-based population, Tattersall et al21 found that despite better IOP control, patients with OAG with a poor life expectancy lost more functional vision than severity-matched patients. In our study no association between disease severity and mortality cause was identified. Additionally, we did not replicate the association between cancer mortality and OAG that was suggested by Lee et al.6 Following adjustment for age at death and gender, there was no significant difference in cancer mortality rates in patients with OAG and the general population.
This retrospective study has a number of important limitations. Given that data from medical notification certificates, as submitted to the regional registry for Births, Deaths and Marriages were used, substantial bias could have been introduced due to incorrect or misinformed documentation being provided by the primary care physician. Nonetheless, data integrity on the ICD-10 coding for this study was optimized by the use of one trained grader. Misclassification bias could have also been introduced due to the fact that approximately half of all people with OAG in our community are undiagnosed.3, 4 It is foreseeable that up to 800 people who died during the study period may have had undiagnosed OAG. Given that the GIST study was not longitudinal, with many people being examined at only one point in time, and that OAG is a progressive disease, such that many examined people may have developed signs of OAG after our initial recruitment, we felt that the use of the full population data was most appropriate. The use of historic or ‘un-phenotyped controls’ is becoming more widespread in association studies.22
Should the identified association with ischaemic heart disease and OAG be genuine and not related to treatment, we would expect that the conferred risk ratio would be strengthened by the inclusion of all actual cases of OAG from the study population. Nonetheless, such misclassification bias could lead to spurious false-positive associations. The social and economic status of people in this study is also an important factor that could not be addressed in this study. Such a bias would affect the number of people seeking ophthalmic review and potentially confound the mortality rate in patients with primary OAG.
Overall, our study supports the findings of others and suggests that a review for signs of cardiovascular disease may be warranted in people diagnosed with OAG. In time, as further work investigates the underlying molecular mechanisms of OAG, the precise pathoaetiological link between ischaemic heart disease and glaucoma should be uncovered.
References
Capri M, Salvioli S, Sevini F, Valensin S, Celani L, Monti D et al. The genetics of human longevity. Ann NY Acad Sci 2006; 1067: 252–263.
Resnikoff S, Pascolini D, Etya'ale D, Kocur I, Pararajasegaram R, Pokharel GP et al. Global data on visual impairment in the year 2002. Bull World Health Organ 2004; 82 (11): 844–851.
Mitchell P, Smith W, Attebo K, Healey PR . Prevalence of open-angle glaucoma in Australia. The Blue Mountains Eye Study. Ophthalmology 1996; 103 (10): 1661–1669.
Wensor MD, McCarty CA, Stanislavsky YL, Livingston PM, Taylor HR . The prevalence of glaucoma in the Melbourne Visual Impairment Project. Ophthalmology 1998; 105 (4): 733–739.
Klein R, Klein BE, Moss SE, Cruickshanks KJ . Association of ocular disease and mortality in a diabetic population. Arch Ophthalmol 1999; 117 (11): 1487–1495.
Lee DJ, Gomez-Marin O, Lam BL, Zheng DD . Glaucoma and survival: the National Health Interview Survey 1986–1994. Ophthalmology 2003; 110 (8): 1476–1483.
Lee AJ, Wang JJ, Kifley A, Mitchell P . Open-angle glaucoma and cardiovascular mortality: the Blue Mountains Eye Study. Ophthalmology 2006; 113 (7): 1069–1076.
Sharkawi E, Franks W . Glaucoma and mortality. Ophthalmology 2008; 115 (1): 213–214.
Australian Bureau of Statistics. Census of population and housing: selected social and housing characteristics for statistical local areas. 2001. Available from: http://www.abs.gov.au. 2001. 1-6-2007.
Coote MA, McCartney PJ, Wilkinson RM, Mackey DA . The ‘GIST’ score: ranking glaucoma for genetic studies. Glaucoma Inheritance Study of Tasmania. Ophthalmic Genet 1996; 17 (4): 199–208.
Wu J, Hewitt AW, Green CM, Ring MA, McCartney PJ, Craig JE et al. Disease severity of familial glaucoma compared with sporadic glaucoma. Arch Ophthalmol 2006; 124 (7): 950–954.
Green CM, Kearns LS, Wu J, Barbour JM, Wilkinson RM, Ring MA et al. How significant is a family history of glaucoma? Experience from the Glaucoma Inheritance Study in Tasmania. Clin Experiment Ophthalmol 2007; 35 (9): 793–799.
Leske MC . Glaucoma and mortality: a connection? Ophthalmology 2003; 110 (8): 1473–1475.
Egge K, Zahl PH . Survival of glaucoma patients. Acta Ophthalmol Scand 1999; 77 (4): 397–401.
Hayreh SS . Blood supply of the optic nerve head and its role in optic atrophy, glaucoma, and oedema of the optic disc. Br J Ophthalmol 1969; 53 (11): 721–748.
Flammer J, Orgul S, Costa VP, Orzalesi N, Krieglstein GK, Serra LM et al. The impact of ocular blood flow in glaucoma. Prog Retin Eye Res 2002; 21 (4): 359–393.
Broadway DC, Drance SM . Glaucoma and vasospasm. Br J Ophthalmol 1998; 82 (8): 862–870.
Weinreb RN . Why study the ocular microcirculation in glaucoma? J Glaucoma 1992; 1: 145–147.
Fingert JH, Stone EM, Sheffield VC, Alward WL . Myocilin glaucoma. Surv Ophthalmol 2002; 47 (6): 547–561.
Hewitt AW, Mackey DA, Craig JE . Myocilin allele-specific glaucoma phenotype database. Hum Mutat 2008; 29 (2): 207–211.
Tattersall CL, Vernon SA, Negi A . Is poor life expectancy a predictive factor in the progression of primary open angle glaucoma? Eye 2005; 19: 387–391.
Wellcome Trust Case Control Consortium. Genome-wide association study of 14 000 cases of seven common diseases and 3000 shared controls. Nature 2007; 447: 661–678.
Acknowledgements
This research was supported by the Ophthalmic Research Institute of Australia, Glaucoma Australia, the Royal Hobart Hospital Research Foundation, the Clifford Craig Research Trust. AWH was supported by an NHMRC Medical Postgraduate Scholarship. JEC was supported in part by an NHMRC Practitioner Fellowship, and DAM is the recipient of a Pfizer Australia research fellowship.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests: No authors of this paper have any competing interests related to this research.
Rights and permissions
About this article
Cite this article
Hewitt, A., Sanfilippo, P., Ring, M. et al. Mortality in primary open-angle glaucoma: ‘two cupped discs and a funeral’. Eye 24, 59–63 (2010). https://doi.org/10.1038/eye.2009.37
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2009.37