Abstract
Objective
The objective of this study was to describe the distribution of conjunctival ultraviolet autofluorescence (UVAF) in an adult population.
Methods
We conducted a cross-sectional, population-based study in the genetic isolate of Norfolk Island, South Pacific Ocean. In all, 641 people, aged 15 to 89 years, were recruited. UVAF and standard (control) photographs were taken of the nasal and temporal interpalpebral regions bilaterally. Differences between the groups for non-normally distributed continuous variables were assessed using the Wilcoxon–Mann–Whitney ranksum test. Trends across categories were assessed using Cuzick's non-parametric test for trend or Kendall's rank correlation τ.
Results
Conjunctival UVAF is a non-parametric trait with a positively skewed distribution. Median amount of conjunctival UVAF per person (sum of four measurements; right nasal/temporal and left nasal/temporal) was 28.2 mm2 (interquartile range 14.5–48.2). There was an inverse, linear relationship between UVAF and advancing age (P<0.001). Males had a higher sum of UVAF compared with females (34.4 mm2 vs23.2 mm2, P<0.0001). There were no statistically significant differences in area of UVAF between right and left eyes or between nasal and temporal regions.
Conclusion
We have provided the first quantifiable estimates of conjunctival UVAF in an adult population. Further data are required to provide information about the natural history of UVAF and to characterise other potential disease associations with UVAF. UVR protective strategies should be emphasised at an early age to prevent the long-term adverse effects on health associated with excess UVR.
Similar content being viewed by others
Introduction
Moderate ultraviolet radiation (UVR) exposure from the sun is an indispensable part of health, but excessive or inadequate amounts of UVR can be detrimental to well-being. Recently, a systematic review identified several diseases with sufficient evidence of a causal effect due to UVR: ophthalmic (acute photokeratitis and conjunctivitis, pterygium, cortical cataract, acute solar retinopathy, squamous cell carcinoma (SCC) of cornea and conjunctiva) and non-ophthalmic (sunburn, solar keratosis, basal cell carcinoma (BCC), cutaneous SCC, malignant melanoma, herpes labialis and medication reactions). In contrast, three diseases—rickets, osteomalacia, and osteoporosis—were associated with insufficient UVR exposure.1 Other possible disease ocular associations with UVR include cicatricial ectropion, climatic keratopathy, pinguecula, iris melanoma and macular degeneration.
A significant proportion of disease burden attributed to UVR is avoidable. Data on attributable risk from the World Health Organization Global Burden of Disease from Solar Ultraviolet Radiation study reveal that 50–90% of the disease burden of cutaneous melanoma is due to UVR exposure; 50–70% of the disease burden of SCC is due to UVR exposure; 50–90% of the disease burden of BCC is due to UVR exposure; 50–70% of the disease burden of SCC of the conjunctiva or cornea is due to UVR exposure.2 There were also 60 000 deaths attributed to excessive UVR exposure in the year 2000.2
The exposure of an individual to UVR (especially harmful UVB) is influenced by environmental factors, temporal factors and personal protective behaviours.3 The ozone layer acts as a physical barrier that limits the amount of UVR reaching the surface of the earth. It prevents virtually all short wavelengths (ie, those >290 nm, and including all of UVC) as well as 90% of UVB (wavelength 280–315 nm).4 The wavelength determines the percentage of UVR absorbed by the different components of the eye, with the overwhelming majority of shorter wavelengths being absorbed by the cornea and conjunctiva. There is a sharp rise in UVB transmission by the cornea at ∼308 nm and ∼60–80% of transmission of UVR to the cornea and aqueous occurs at wavelengths >300 nm.5 For this reason, we expect to see the greatest degree of damage attributed to UVB radiation in the most superficial segment of the eye and this area is where much of the absorption occurs, especially in the corneal epithelium and Bowman's membrane.6
Obtaining accurate estimates of individual ocular UVR exposure is difficult, but of paramount importance in accurately evaluating the relationship between UVR and ocular diseases, ocular traits and lifestyle factors. Biophysical, physiological and behavioural factors, as well as ground reflectance, are critical in determining ocular UV exposure and failure to account for these factors can lead to completely inaccurate assignments of lifetime exposure.7 Simple questionnaires collecting retrospective data about sunlight exposure and lifestyle habits are prone to significant recall bias. A sophisticated model for calculating the exposure of an individual to harmful UVB was developed and implemented in the Chesapeake Bay waterman study, and the Beaver Dam Eye Study. This model of exposure collected information regarding lifetime personal ocular exposure, UVR meteorological data (including laboratory and field measurements of harmful UVB exposure) and ocular protective factors.8 Other methods to gather information about ocular exposure to UVR have included placing UV-sensitive dye between the eyes of the participants,9 as well as measuring UVR through the placement of photodiode sensor arrays to the eye,10 and UV-blocking contact lenses.11
Despite our ability to collect useful data on UVR exposure of the skin, to date there has been no valid measurement that quantifies the amount of ocular UVR exposure. To obtain an objective measure of the amount of UVR reaching the eye, conjunctival ultraviolet autofluorescence (UVAF) has been developed. The biophysical principle of autofluorescence (AF) is the same as that used in dermatology with the Woods lamp detecting actinic damage to the skin.12 Using this technique, Coroneo and colleagues have described a phenomenon of UVAF of the conjunctiva associated with pterygium that correlated with ocular sun exposure.13, 14 This phenomenon appears to be a biomarker of early pinguecula/pterygium formation and can be used as an objective clinical marker of facial UV exposure.
Our rationale for conducting this study on Norfolk Island is multifaceted. Norfolk Island is a genetic isolate and has been targeted in previous genetic research into the aetiology of cardiovascular disease.15, 16, 17 Using a similar approach, we are hoping to use this initial framework to uncover novel information about ocular phenotypes. Collectively, the population has been very supportive of health-related research. Such isolated populations have already proved beneficial in increasing our understanding of the genetic determinants of simple and complex disease in ophthalmology.18 In addition, Norfolk Island is geographically isolated, has a very stable population with restricted migration, and has consistent sun/UV exposure and low levels of pollution.
The quantitative distribution of conjunctival UVAF in adults has not previously been assessed in a population study. Therefore, our aim was to determine the relationship between conjunctival UVAF, age and gender in an adult population-based study.
Materials and Methods
Study location and geography
Norfolk Island is located approximately 1600 km northeast of Sydney, Australia, in the Pacific Ocean at latitude 29° 02′ South—167° 56′ East. Climatic data on Norfolk Island are published through the Australian Bureau of Metereology.19 Mean daily sunshine ranges from 5.2 h per day in June to 7.9 h per day in November. Mean number of cloudy days ranges from 9 in August to 14 in both January and March. There is a mean of 2.8 days with clear skies in March, rising to 5.1 in August. Historically, February is the hottest month (mean 0900 temperature 16.0 °C; mean 1500 temperature 23.8 °C), and August is the coolest month (mean 16.0 °C at 0900; 17.1 °C at 1500).
Recruitment
The Norfolk Island Eye Study (NIES) was a population-based study performed on Norfolk Island in 2007 to 2008. Permanent residents of Norfolk Island, an external territory of Australia, aged ≥15 years were invited to participate in the NIES. There were no specific exclusion criteria for the conjunctival UVAF arm of NIES. 61.5% of the permanent population aged 15 years and over, and over 70% of residents aged ≥50 years were recruited for the NIES. Only 641 of the 781 people (82.1%) involved in the NIES had conjunctival UVAF photography performed.
Ethics
The Human Research and Ethics Committee at the Royal Victorian Eye and Ear Hospital in Melbourne approved the NIES. Informed consent was obtained before the ophthalmic examination and conjunctival UVAF photography. In addition, there was local community consultation with the hospital administration, local doctors, local optometrist and visiting ophthalmologists to check that all concerns were met regarding the possible long-term impact of the study.
Conjunctival UVAF
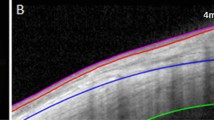
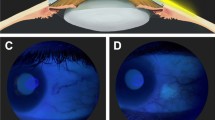
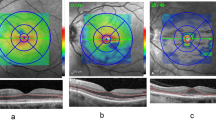
Conjunctival UVAF images were captured using the camera system developed by Coroneo and colleagues (Figure 1).13, 14 Photographs were taken using both reflected visible light (control) and UV-induced AF with the aid of two portable photographic systems. Each consisted of a height adjustable table equipped with subject head-rest, camera positioning assembly, digital single-lens reflex camera, macro lens and filtered electronic flash. An example of the setup of the camera apparatus used in the NIES is displayed (Figure 1). Each eye was photographed at 0.94 magnification, with separate views of the nasal and temporal regions of both eyes. Coloured low-voltage light emitting diodes were positioned on stands in the visual field of the subject at ∼35° to the camera–subject axis to aid fixation. The UV-induced fluorescence photography was based on standard principles, using a specially adapted electronic flash system fitted with UV-transmission filters (transmittance range 300–400 nm, peak 365 nm) as the excitation source. Subject fluorescence was recorded with a Nikon D100 (Nikon, Melville, NY, USA) digital camera and 105 mm f/2.8 Micro Nikon (Nikon) lens fitted with infrared and UV barrier filters. Thus, only fluorescence was recorded by the camera. Images were saved in RGB format at the D100 settings of JPEG fine (1 : 4 compression) and large resolution. Some unwanted red light allowed by the UV transmission filter was eliminated by removal of the red channel in Adobe PhotoShop (Adobe Systems Inc., San Jose, CA, USA), equivalent to the use of a cyan filter on the camera lens. Each photograph could be verified immediately after it was taken and recaptured, if necessary, to obtain an enhanced image. Examples of UVAF and control photographs of the same eye from the same person have been included (Figures 2 and 3).
Imaging software was then used to calculate the area of UVAF. Four photos were analysed per person (right nasal/left nasal/right temporal/left temporal). The settings required for the UVAF analysis were pixel length=3008 and logical length=2.4. The resultant area is expressed in mm2. The camera system detects a fairly uniform area of AF, and the area analysed corresponds to the summation of all of the areas. However, the area analysed is of varying intensity of AF, and it may be difficult to determine the specific area of the conjunctiva that needs to be determined. In most cases, only one discreet area of AF is found. However, in cases in which multiple areas of AF exist, each area is calculated separately and the total area is calculated for that eye.
One investigator (JCS) subsequently separately evaluated the UV photographs for the presence and pattern of fluorescence on the basis of the predefined fluorescence patterns. Intragrader reliability was assessed by intraclass correlation between 60 randomly selected images where repeat measurements were performed two months apart. Intra-grader correlation coefficients for each sector were excellent (nasal OD: 0.915, temporal OD: 0.824, nasal OS: 0.991 and temporal OS: 0.897).
Statistical analysis
Continuous variables were assessed for normality and summarised using mean (standard deviation) or median (interquartile range), as appropriate. Total UVAF was divided into quartiles. Differences between groups for non-normally distributed continuous variables were assessed using the Wilcoxon–Mann–Whitney rank sum test. Trends across categories were assessed using Cuzick's non-parametric test for trend or Kendall's rank correlation τ. Statistical significance was set at <0.05. All analyses were undertaken in Intercooled Stata 8.2 for Windows.20
Results
Distribution of conjunctival UVAF
Data were available for 641 people with 1282 eyes. Four measurements were recorded for each person, which resulted in nine different groups (Table 1). The trait was not normally distributed (P<0.001).
There was an inverse, linear relationship between UVAF and advancing age (P<0.001; Figure 4). Quantitative assessment of UVAF demonstrated a skewed distribution with over half of the population having a UVAF of <30.0 mm2 in both eyes (Figure 5).
There were 279 males (43.5%) in the sample. Males had a higher sum of UVAF (four measurements in two eyes) compared with females (34.4 mm2 vs 23.2 mm2, P<0.001; Table 2). This difference was observed in all nine measurements of UVAF. There was no statistically significant difference between median UVAF in right and left eyes. (P=0.359).
The age and gender associations with quartile UVAF were calculated. With increasing size of median UVAF, there was an increasing proportion of males (P<0.001), and decreasing age (P<0.001). Table 3 displays the UVAF readings in people according to several clinical diseases obtained from the questionnaire. There were no statistically significant differences in total UVAF in people with and without any of the diseases.
Absence of (or mild) conjunctival UVAF
There were 48 eyes (3.7%) that did not exhibit any AF; 21 right eyes (3.3%) had no AF; 16 right eyes between 0.1 and 0.9 mm; 200 eyes had between 1.0 and 9.9 mm2 of UVAF; and 27 left eyes (4.2%) did not show AF. There were 25 left eyes with UVAF between 0.1 and 0.9 mm2, and 195 left eyes between 1.0 and 9.9 mm2 of UVAF.
Temporal locations were more likely to have no UVAF than nasal locations (6.2 vs 3.4%, P=0.019). Of temporal locations, 40 eyes had no UVAF, 30 eyes between 0.1 and 0.9 mm2, and 190 eyes between 1.0 and 9.9 mm2 of UVAF. Of nasal locations, 22 eyes had no UVAF, 28 eyes between 0.1 and 0.9 mm2 and 188 eyes between 1.0 and 9.9 mm2 of UVAF. There were 13 people with no UVAF in either eye (2.0%). Furthermore, there were 107 people who had <1.0 mm2 total ocular UVAF.
Discussion
In a large population-based sample that underwent conjunctival UVAF photography, we found that conjunctival UVAF is a non-parametric trait that is associated with age and is higher in males. Our finding that conjunctival UVAF peaks in young adults, and then slowly declines with age is in contrast to results in children aged 15 years and younger.13
We propose that conjunctival UVAF is a biological dosimeter of acute ocular UV exposure, somewhat similar to a suntan. Given the higher degree of UVAF with earlier age it is likely that UVAF represents recent cumulative exposure to ocular UV radiation rather than lifetime cumulative exposure. Re-examining the same individuals over time, as well as examining previously unexamined individuals, will be required to assess for evidence of age, cohort or period effects that may affect the longitudinal changes in degree of UVAF.
We hypothesise that UVR-induced damage to the anterior eye in earlier years is sufficient to lead to UVR-related ocular diseases many years later. This is supported by Mackenzie et al,21 who found that sun exposure in early life is a strong risk factor for the development of pterygia. There is an age-related increasing prevalence of ocular disorders, such as pterygium22 and cataract,23 that have a strong association with UVR exposure. Higher UVAF may reflect poorer sun protective behaviours and/or a higher tendency (genetic or otherwise) to develop ocular UVAF.
It is also possible that in elucidating the natural history of UVAF we have found a situation analogous to that for solar keratoses. Around 26% of these lesions undergo spontaneous remission.24 If sun exposure is reduced over time, repair mechanisms, such as DNA repair, induction of apoptosis and immune surveillance mechanisms may come into play,25, 26 reversing some of the UV-induced damage. Further study of this trait in other populations, and assessment of protective behaviours in relation to UVAF, is required to further elucidate this relationship.
Male gender is associated with a higher degree of UVAF. This is not surprising given that males typically have a higher prevalence of many disorders strongly associated with UVR, including pterygium,27 climatic droplet keratopathy28 and SCC of the conjunctiva,29 and are generally more likely to spend working hours outdoors.
Norfolk Island has a tropical climate and a corresponding high prevalence of skin cancer (Dr Gary Mitchell, personal communication). Given its sub-tropical climate, Norfolk Island would probably represent a population at high risk, and therefore, determination of normative data in other populations of varying risk would be ideal. However, as there are no other population-based data on the quantification of UVAF we were unable to compare and contrast the degree of UVAF in this population to others. Moreover, even though only one person was involved in this grading of conjunctival UVAF photographs, the intra-observer agreement was high. Despite strong agreement, some degree of measurement error is likely.
Using similar methodology, Ooi et al13 reported that all of six pingueculae displayed UVAF. A further 16 children, all aged 9 years and above, showed fluorescence without signs of pingueculae. The presence of fluorescence (in at least one region) was 0% in 27 children aged 3 to 8 years, 6 of 23 (26%) for those ages 9–11 years and 17 of 21 (81%) for those ages 12 to 15 years. Using a confocal scanning laser ophthalmoscope, Utine et al30 measured AF in 40 eyes in 23 patients with pinguceulae. In all of the cases, the size of AF in the pinguecula was greater than the extent of the visible pinguecula on slit-lamp examination in 71.4% of the lesions. In addition, they found that a Vogt limbal girdle displayed hyperautofluorescence, but arcus senillis did not.30
AF of the fundus has been used in the imaging of several posterior segment diseases to detect changes in lipofuscin in the retinal pigment epithelium. Such disorders have included rare diseases such as central areolar choroidal dystrophy,31 Stargardt dystrophy and fundus flavimaculatus,32 Kjellin's syndrome,33 multifocal choroiditis and panuveitis,34 Best's vitelliform dystrophy35 and birdshot chorioretinopathy.36 In addition, fundus AF has been used to assess early age-related macular degeneration (AMD)37 and late AMD38 and is useful for monitoring progression in AMD.39 However, it is important to realise that AF imaging records every structure in the light path, and is not confined merely to the region of interest.40
Conjunctival UVAF allows early detection of, education about and prevention of future ocular and systemic sun damage. The current camera system used in this study is impractical for use in a non-research setting. If a portable camera system could be developed, it would have direct clinical use for documenting early actinic damage to the conjunctiva and public health use for population screening to demonstrate to young people the level of sun damage that they already have, thereby helping reinforce sun protective behaviours. Such a system would also enable lesions to be identified and may have an important role in epidemiological studies of ophthalmic and non-ophthalmic diseases related to UVR. We need to be able to determine the optimum amount of UV exposure that is a trade-off between the benefits and harms in order to implement health prevention strategies targeting adolescents and young adults. This technology is currently being tested in younger population in a cohort study of 2000 20-year-olds (Raine Eye Health Study), which should give us the answer in the next few years.
An interesting future direction of this research would be to investigate the tissue specific dose of AF, and time of dose, that is responsible for triggering some diseases. In addition, an understanding of the relationship between brightness of AF and the agreement between brightness and 2D area may provide further clues to the pathogenesis of several ophthalmic diseases. It is probable that the brightness of AF is highly variable, as there are almost certainly healing responses that would at least in part be genetically determined. Linked to this is the importance of elucidating the origin of the fluorescence. The 2D imaging is still essential, as it could be that the area of limbus affected may help to determine at what point the cornea is invaded. One possible source of fluorescence is altered stem cells41, 42 that have grown out from their niche, and if this is the case, then 2D imaging is certainly of significance.
The eye does not adapt to environmental challenges as well as the skin does. Some natural mechanisms do exist, which include the recessed position of the eye in the orbit, and squinting in response to strong levels of visible light. Limiting the amount of exposure to UVR through behavioural and lifestyle means is the mainstay for prevention of UVR-related diseases of the eye. The joint position statement from the Centre for Eye Research Australia/Cancer Council of Australia recommends:43 reducing UV radiation exposure as much as possible; wearing a broad-brimmed, bucket or legionnaire style hat and a havelock; wearing close fitting, wrap around style sunglasses that meet the Australian Standard; wearing glasses that transmit very little UVR, such as those labelled UV 400 or EPF (Eye Protection Factor) 9 or 10.
Conclusion
We have reported findings from a large population-based assessment of conjunctival UVAF following earlier work that suggests that conjunctival UVAF is an objective clinical marker of facial UV exposure. Our major findings are that conjunctival AF is higher in younger people and in males. Future studies using this novel assessment method of UVR exposure will investigate the relationship between conjunctival UVAF and ocular diseases, biometry and lifestyle factors. Additional data are required to assess the natural history of UVAF and its role in the cumulative measurement of facial UVR exposure.

References
Lucas RM, McMichael AJ, Armstrong BK, Smith WT . Estimating the global disease burden due to ultraviolet radiation exposure. Int J Epidemiol 2008; 37: 654–667.
Lucas R, McMichael T, Smith W, Armstrong B . Solar ultraviolet radiation: global burden of disease from solar ultraviolet radiation. Environmental Burden of Disease Series. No. 13. WHO: Geneva, 2006.
Oliva MS, Taylor H . Ultraviolet radiation and the eye. Int Ophthalmol Clin 2005; 45: 1–17.
Johnson GJ . The environment and the eye. Eye (Lond) 2004; 18: 1235–1250.
Boettner EA, Wolter JR . Transmission of the ocular media invest. Ophthalmology 1962; 1: 776–783.
Kolozsvari L, Nogradi A, Hopp B, Bor Z . UV absorbance of the human cornea in the 240- to 400-nm range. Invest Ophthalmol Vis Sci 2002; 43: 2165–2168.
Sliney DH . Epidemiological studies of sunlight and cataract: the critical factor of ultraviolet exposure geometry. Ophthalmic Epidemiol 1994; 1: 107–119.
Rosenthal FS, West SK, Munoz B, Emmett EA, Strickland PT, Taylor HR . Ocular and facial skin exposure to ultraviolet radiation in sunlight: a personal exposure model with application to a worker population. Health Phys 1991; 61: 77–86.
Rosenthal FS, Phoon C, Bakalian AE, Taylor HR . The ocular dose of ultraviolet radiation to outdoor workers. Invest Ophthalmol Vis Sci 1988; 29: 649–656.
Walsh JE, Bergmanson JP, Wallace D, Saldana G, Dempsey H, McEvoy H et al. Quantification of the ultraviolet radiation (UVR) field in the human eye in vivo using novel instrumentation and the potential benefits of UVR blocking hydrogel contact lens. Br J Ophthalmol 2001; 85: 1080–1085.
Kwok LS, Kuznetsov VA, Ho A, Coroneo MT . Prevention of the adverse photic effects of peripheral light-focusing using UV-blocking contact lenses. Invest Ophthalmol Vis Sci 2003; 44: 1501–1507.
Asawanonda P, Taylor CR . Wood's light in dermatology. Int J Dermatol 1999; 38: 801–807.
Ooi JL, Sharma NS, Papalkar D, Sharma S, Oakey M, Dawes P et al. Ultraviolet fluorescence photography to detect early sun damage in the eyes of school-aged children. Am J Ophthalmol 2006; 141: 294–298.
Ooi JL, Sharma NS, Sharma S, Papalkar D, Oakey M, Dawes P et al. Ultraviolet fluorescence photography: patterns in established pterygia. Am J Ophthalmol 2007; 143: 97–101.
Bellis C, Cox HC, Dyer TD, Charlesworth JC, Begley KN, Quinlan S et al. Linkage mapping of CVD risk traits in the isolated Norfolk Island population. Hum Genet 2008; 124: 543–552.
Bellis C, Cox HC, Ovcaric M, Begley KN, Lea RA, Quinlan S et al. Linkage disequilibrium analysis in the genetically isolated Norfolk Island population. Heredity 2008; 100: 366–373.
Bellis C, Hughes RM, Begley KN, Quinlan S, Lea RA, Heath SC et al. Phenotypical characterisation of the isolated norfolk island population focusing on epidemiological indicators of cardiovascular disease. Hum Hered 2005; 60: 211–219.
Sherwin JC, Hewitt AW, Ruddle JB, Mackey DA . Genetic isolates in ophthalmic diseases. Ophthalmic Genet 2008; 29: 149–161.
Climate statistics for Australian locations: Norfolk Island. (Accessed at http://www.bom.gov.au/climate/averages/tables/cw_200288_All.shtml.).
Statacorp. Intercooled Stata 8.2 for Windows, 8.2 edn. US StataCorp LP: College Station, TX, 2004.
Mackenzie FD, Hirst LW, Battistutta D, Green A . Risk analysis in the development of pterygia. Ophthalmology 1992; 99: 1056–1061.
Saw SM, Tan D . Pterygium: prevalence, demography and risk factors. Ophthalmic Epidemiol 1999; 6: 219–228.
Hyman L . Epidemiology of eye disease in the elderly. Eye (Lond) 1987; 1 (Part 2): 330–341.
Marks R, Foley P, Goodman G, Hage BH, Selwood TS . Spontaneous remission of solar keratoses: the case for conservative management. Br J Dermatol 1986; 115: 649–655.
Brash DE, Ponten J . Skin precancer. Cancer surveys 1998; 32: 69–113.
Heck DE, Gerecke DR, Vetrano AM, Laskin JD . Solar ultraviolet radiation as a trigger of cell signal transduction. Toxicol Appl Pharmacol 2004; 195: 288–297.
West S, Munoz B . Prevalence of pterygium in Latinos: proyecto VER. Br J Ophthalmol 2009; 93: 1287–1290.
Urrets-Zavalia JA, Knoll EG, Maccio JP, Urrets-Zavalia EA, Saad JA, Serra HM . Climatic droplet keratopathy in the Argentine Patagonia. Am J Ophthalmol 2006; 141: 744–746.
Lee GA, Hirst LW . Ocular surface squamous neoplasia. Surv Ophthalmol 1995; 39: 429–450.
Utine CA, Tatlipinar S, Altunsoy M, Oral D, Basar D, Alimgil LM . Autofluorescence imaging of pingueculae. Br J Ophthalmol 2009; 93: 396–399.
Boon CJ, Klevering BJ, Cremers FP, Zonneveld-Vrieling MN, Theelen T, Den Hollander AI et al. Central areolar choroidal dystrophy. Ophthalmology 2009; 116: 771–782, 782 e1.
Dolar-Szczasny J, Mackiewicz J, Biziorek B, Zagorski Z . Fundus autofluorescence imaging in patients with Stargardt dystrophy and fundus flavimaculatus. Klin Oczna 2007; 109: 176–178.
Frisch IB, Haag P, Steffen H, Weber BH, Holz FG . Kjellin's syndrome: fundus autofluorescence, angiographic, and electrophysiologic findings. Ophthalmology 2002; 109: 1484–1491.
Haen SP, Spaide RF . Fundus autofluorescence in multifocal choroiditis and panuveitis. Am J Ophthalmol 2008; 145: 847–853.
Jarc-Vidmar M, Kraut A, Hawlina M . Fundus autofluorescence imaging in Best's vitelliform dystrophy. Klin Monbl Augenheilkd 2003; 220: 861–867.
Koizumi H, Pozzoni MC, Spaide RF . Fundus autofluorescence in birdshot chorioretinopathy. Ophthalmology 2008; 115: e15–e20.
Bearelly S, Cousins SW . Fundus autofluorescence imaging in age-related macular degeneration and geographic atrophy. Adv Exp Med Biol 2010; 664: 395–402.
McBain VA, Townend J, Lois N . Fundus autofluorescence in exudative age-related macular degeneration. Br J Ophthalmol 2007; 91: 491–496.
Einbock W, Moessner A, Schnurrbusch UE, Holz FG, Wolf S . Changes in fundus autofluorescence in patients with age-related maculopathy. correlation to visual function: a prospective study. Graefes Arch Clin Exp Ophthalmol 2005; 243: 300–305.
Spaide RF . Potential causes of altered autofluorescence in diabetic persons. Arch Ophthalmol 2009; 127: 942–943; author reply 3–4.
Wun BP, Tao Q, Lyle S . Autofluorescence in the stem cell region of the hair follicle bulge. J Invest Dermatol 2005; 124: 860–862.
Teng SW, Tan HY, Peng JL, Lin HH, Kim KH, Lo W et al. Multiphoton autofluorescence and second-harmonic generation imaging of the ex vivo porcine eye. Invest Ophthalmol Vis Sci 2006; 47: 1216–1224.
Eye protection joint position statement: CERA/Cancer Council. (Accessed at http://www.cancer.org.au/File/PolicyPublications/Position_statements/PS-Eyeprotection-August2006.pdf.).
Acknowledgements
We thank the Norfolk Islanders for welcoming us into their community and for their participation and assistance in this study. We also wish to thank Sophie Rogers and Cong Sun for assistance with the statistical analysis. Financial support was provided by the RVEEH research committee and the Peggy and Leslie Cranbourne Foundation. CERA receives Operational Infrastructure Support from the Victorian Government. DAM is a recipient of the Pfizer Australia Senior Research Fellowship.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Sherwin, J., Hewitt, A., Kearns, L. et al. Distribution of conjunctival ultraviolet autoflourescence in a population-based study: the Norfolk Island Eye Study. Eye 25, 893–900 (2011). https://doi.org/10.1038/eye.2011.83
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2011.83