Abstract
Background:
Obesity is associated with decreased iron status, possibly due to a rise in hepcidin, an inflammatory protein known to reduce iron absorption. In animals, we have shown that maternal iron deficiency is minimised in the foetus by increased expression of placental transferrin receptor (pTFR1), resulting in increased iron transfer at the expense of maternal iron stores.
Objective:
This study examines the effect of obesity during pregnancy on maternal and neonatal iron status in human cohorts and whether the placenta can compensate for decreased maternal iron stores by increasing pTFR1 expression.
Subjects/Methods:
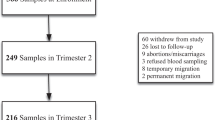
A total of 240 women were included in this study. One hundred and fifty-eight placentas (Normal: 90; Overweight: 37; Obese: 31) were collected at delivery. Maternal iron status was measured by determining serum transferrin receptor (sTFR) and ferritin levels at 24 and 34 weeks and at delivery. Hepcidin in maternal and cord blood was measured by ELISA and pTFR1 in placentas by western blotting and real-time RT-PCR.
Results:
Low iron stores were more common in obese women. Hepcidin levels (ng ml−1) at the end of the pregnancy were higher in obese than normal women (26.03±12.95 vs 18.00±10.77, P<0.05). Maternal hepcidin levels were correlated with maternal iron status (sTFR r=0.2 P=0.025), but not with neonatal values. mRNA and protein levels of pTFR1 were both inversely related to maternal iron status. For mRNA and all women, sTFR r=0.2 P=0.044. Ferritin mRNA levels correlated only in overweight women r=−0.5 P=0.039 with hepcidin (r=0.1 P=0.349), irrespective of maternal body mass index (BMI).
Conclusions:
The data support the hypothesis that obese pregnant women have a greater risk of iron deficiency and that hepcidin may be a regulatory factor. Further, we show that the placenta responds to decreased maternal iron status by increasing pTFR1 expression.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Aranceta J, Pérez Rodrigo C, Serra Majem L, Vioque J, Tur Marí JA, Mataix Verdú J et alEstudio DORICA: dislipemia, obesidad y riesgo cardiovascular. In: Aranceta J, Foz M, Gil B, Jover E, Mantilla T, Millán J (eds). Obesidad y riesgo cardiovascular Estudio DORICA. Madrid: Panamericana, 2004. pp 125–156.
Wallace JM, Horgan GW, Bhattacharya S . Placental weight and efficiency in relation to maternal body mass index and the risk of pregnancy complications in women delivering singleton babies. Placenta 2012; 33: 611–618.
Nohr EA, Bech BH, Davies MJ, Frydenberg M, Henriksen TB, Olsen J . Prepregnancy obesity and fetal death: a study within the Danish National Birth Cohort. Obstet Gynecol 2005; 106: 250–259.
Higgins L, Greenwood SL, Wareing M, Sibley CP, Mills TA . Obesity and the placenta: A consideration of nutrient exchange mechanisms in relation to aberrant fetal growth. Placenta 2011; 32: 1–7.
Bhutta ZA, Haider BA . Maternal micronutrient deficiencies in developing countries. Lancet 2008; 371: 186–187.
Baker RD, Greer FR . Diagnosis and prevention of iron deficiency and iron-deficiency anemia in infants and young children (0-3 years of age). Pediatrics 2010; 126: 1040–1050.
Kelly AM, MacDonald DJ, McDougall AN . Observations on maternal and fetal ferritin concentrations at term. Br J Obstet Gynaecol 1978; 85: 338–343.
WHO The prevalence of anemia in women: A tabulation of available information 2nd ed. Switzerland World Health Organization: Geneva, 1992.
ACOG. American College of Obstetricians and Gynecologists. Practice Bulletin No. 95: anemia in pregnancy. Obstet Gynecol 2008; 112: 201–207.
Gambling L, Charania Z, Hannah L, Antipatis C, Lea RG, McArdle HJ . Effect of iron deficiency on placental cytokine expression and fetal growth in the pregnant rat. Biol Reprod 2002; 66: 516–523.
Georgieff MK . Nutrition and the developing brain: nutrient priorities and measurement. Am J Clin Nutr 2007; 85: 614S–620S.
Gambling L, Lang C, McArdle HJ . Fetal regulation of iron transport during pregnancy. Am J Clin Nutr 2011; 94: 1903S–1907S.
Bekri S, Gual P, Anty R, Luciani N, Dahman M, Ramesh B et al. Increased adipose tissue expression of hepcidin in severe obesity is independent from diabetes and NASH. Gastroenterology 2006; 131: 788–796.
Yanoff LB, Menzie CM, Denkinger B, Sebring NG, McHugh T, Remaley AT et al. Inflammation and iron deficiency in the hypoferremia of obesity. Int J Obes (Lond) 2007; 31: 1412–1419.
Rehu M, Punnonen K, Ostland V, Heinonen S, Westerman M, Pulkki K et al. Maternal serum hepcidin is low at term and independent of cord blood iron status. Eur J Haematol 2010; 85: 345–352.
van Santen S, Kroot JJ, Zijderveld G, Wiegerinck ET, Spaanderman ME, Swinkels DW . The iron regulatory hormone hepcidin is decreased in pregnancy: a prospective longitudinal study. Clin Chem Lab Med 2012; 14: 1–7.
Gambling L, Czopek A, Andersen HS, Holtrop G, Srai SK, Krejpcio Z et al. Fetal iron status regulates maternal iron metabolism during pregnancy in the rat. Am J Physiol Regul Integr Comp Physiol 2009; 296: R1063–R1070.
Li YQ, Yan H, Bai B . Change in iron transporter expression in human term placenta with different maternal iron status. Eur J Obstet Gynecol Reprod Biol 2008; 140: 48–54.
Young MF, Pressman E, Foehr ML, McNanley T, Cooper E, Guillet R et al. Impact of maternal and neonatal iron status on placental transferrin receptor expression in pregnant adolescents. Placenta 2010; 31: 1010–1014.
Phillips AK, Roy SC, Lundberg R, Guilbert TW, Auger AP, Blohowiak SE et al. Neonatal iron status is impaired by maternal obesity and excessive weight gain during pregnancy. J Perinatol 2014; 34: 513–518.
Dao MC, Sen S, Iyer C, Klebenov D, Meydani SN . Obesity during pregnancy and fetal iron status: is Hepcidin the link[quest]. J Perinatol 2012; 33: 177–181.
Santacruz A, Collado MC, Garcia-Valdes L, Segura MT, Martin-Lagos JA, Anjos T et al. Gut microbiota composition is associated with body weight, weight gain and biochemical parameters in pregnant women. Br J Nutr 2010; 104: 83–92.
Punnonen K, Irjala K, Rajamaki A . Serum transferrin receptor and its ratio to serum ferritin in the diagnosis of iron deficiency. Blood 1997; 89: 1052–1057.
Walsh T, O'Broin SD, Cooley S, Donnelly J, Kennedy J, Harrison RF et al. Laboratory assessment of iron status in pregnancy. Clin Chem Lab Med 2011; 49: 1225–1230.
Mei Z, Cogswell ME, Looker AC, Pfeiffer CM, Cusick SE, Lacher DA et al. Assessment of iron status in US pregnant women from the National Health and Nutrition Examination Survey (NHANES), 1999-2006. Am J Clin Nutr 2011; 93: 1312–1320.
Cook JD, Flowers CH, Skikne BS . The quantitative assessment of body iron. Blood 2003; 101: 3359–3364.
Skikne BS, Flowers CH, Cook JD . Serum transferrin receptor: a quantitative measure of tissue iron deficiency. Blood 1990; 75: 1870–1876.
Duffy EM, Bonham MP, Wallace JM, Chang CK, Robson PJ, Myers GJ et al. Iron status in pregnant women in the Republic of Seychelles. Public Health Nutr 2010; 13: 331–337.
Iannotti LL, ÓBrien KO, Chang S-C, Mancini J, Schulman-Nathanson M, Liu S et al. Iron deficiency anemia and depleted body iron reserves are prevalent among pregnant African-American adolescents. J Nutr 2005; 135: 2572–2577.
CDC. Recommendations to prevent and control iron deficiency in the United States. Centers for Disease Control and Prevention. MMWR Recomm Rep 1998; 47: 1–29.
Gambling L, Danzeisen R, Gair S, Lea RG, Charania Z, Solanky N et al. Effect of iron deficiency on placental transfer of iron and expression of iron transport proteins in vivo and in vitro. Biochem J 2001; 356: 883–889.
Bradford MM . A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem 1976; 72: 248–254.
Bustin SA, Benes V, Garson JA, Hellemans J, Huggett J, Kubista M et al. The MIQE guidelines: minimum information for publication of quantitative real-time PCR experiments. Clin Chem 2009; 55: 611–622.
Lewis RM, Demmelmair H, Gaillard R, Godfrey KM, Hauguel-de Mouzon S, Huppertz B et al. The placental exposome: placental determinants of fetal adiposity and postnatal body composition. Ann Nutr Metab 2013; 63: 208–215.
Catalano PM . Increasing maternal obesity and weight gain during pregnancy: the obstetric problems of plentitude. Obstet Gynecol 2007; 110: 743–744.
Aranceta J, Perez-Rodrigo C, Serra-Majem L, Ribas L, Quiles-Izquierdo J, Vioque J et al. Influence of sociodemographic factors in the prevalence of obesity in Spain. The SEEDO'97 Study. Eur J Clin Nutr 2001; 55: 430–435.
Laurier D, Guiguet M, Chau NP, Wells JA, Valleron AJ . Prevalence of obesity: a comparative survey in France, the United Kingdom and the United States. Int J Obes Relat Metab Disord 1992; 16: 565–572.
Yu Z, Han S, Zhu J, Sun X, Ji C, Guo X . Pre-pregnancy body mass index in relation to infant birth weight and offspring overweight/obesity: a systematic review and meta-analysis. PLoS One 2013; 8: e61627.
Menzie CM, Yanoff LB, Denkinger BI, McHugh T, Sebring NG, Calis KA et al. Obesity-related hypoferremia is not explained by differences in reported intake of heme and nonheme iron or intake of dietary factors that can affect iron absorption. J Am Diet Assoc 2008; 108: 145–148.
Ausk KJ, Ioannou GN . Is obesity associated with anemia of chronic disease? A population-based study. Obesity (Silver Spring) 2008; 16: 2356–2361.
Tussing-Humphreys LM, Nemeth E, Fantuzzi G, Freels S, Guzman G, Holterman AX et al. Elevated systemic hepcidin and iron depletion in obese premenopausal females. Obesity (Silver Spring) 2010; 18: 1449–1456.
Ferguson BJ, Skikne BS, Simpson KM, Baynes RD, Cook JD . Serum transferrin receptor distinguishes the anemia of chronic disease from iron deficiency anemia. J Lab Clin Med 1992; 119: 385–390.
Carriaga MT, Skikne BS, Finley B, Cutler B, Cook JD . Serum transferrin receptor for the detection of iron deficiency in pregnancy. Am J Clin Nutr 1991; 54: 1077–1081.
Beguin Y . Soluble transferrin receptor for the evaluation of erythropoiesis and iron status. Clin Chim Acta 2003; 329: 9–22.
Akesson A, Bjellerup P, Berglund M, Bremme K, Vahter M . Serum transferrin receptor: a specific marker of iron deficiency in pregnancy. Am J Clin Nutr 1998; 68: 1241–1246.
Choi JW, Im MW, Pai SH . Serum transferrin receptor concentrations during normal pregnancy. Clin Chem 2000; 46: 725–727.
de Azevedo Paiva A, Rondo PH, Guerra-Shinohara EM, Silva CS . The influence of iron, vitamin B(12), and folate levels on soluble transferrin receptor concentration in pregnant women. Clin Chim Acta 2003; 334: 197–203.
Chelchowska M, Swiatek E, Ambroszkiewicz J, Gajewska J, Laskowska-Klita T, Leibschang J . [Concentrations of pro-hepcidin in serum of pregnant women and in umbilical cord blood]. Ginekol Pol 2008; 79: 754–757.
Ervasti M, Sankilampi U, Luukkonen S, Heinonen S, Punnonen K . Maternal pro-hepcidin at term correlates with cord blood pro-hepcidin at birth. Eur J Obstet Gynecol Reprod Biol 2009; 147: 161–165.
O'Brien KO, Zavaleta N, Abrams SA, Caulfield LE . Maternal iron status influences iron transfer to the fetus during the third trimester of pregnancy. Am J Clin Nutr 2003; 77: 924–930.
Young MF, Griffin I, Pressman E, McIntyre AW, Cooper E, McNanley T et al. Maternal hepcidin is associated with placental transfer of iron derived from dietary heme and nonheme sources. J Nutr 2012; 142: 33–39.
Lok CN, Ponka P . Identification of a hypoxia response element in the transferrin receptor gene. J Biol Chem 1999; 274: 24147–24152.
Tacchini L, Bianchi L, Bernelli-Zazzera A, Cairo G . Transferrin receptor induction by hypoxia. HIF-1-mediated transcriptional activation and cell-specific post-transcriptional regulation. J Biol Chem 1999; 274: 24142–24146.
Khatun R, Wu Y, Kanenishi K, Ueno M, Tanaka S, Hata T et al. Immunohistochemical study of transferrin receptor expression in the placenta of pre-eclamptic pregnancy. Placenta 2003; 24: 870–876.
Mando C, Tabano S, Colapietro P, Pileri P, Colleoni F, Avagliano L et al. Transferrin receptor gene and protein expression and localization in human IUGR and normal term placentas. Placenta 2010; 32: 44–50.
Zamudio S, Baumann MU, Illsley NP . Effects of chronic hypoxia in vivo on the expression of human placental glucose transporters. Placenta 2006; 27: 49–55.
Acknowledgements
We thank the families participating in the study, and clinicians and personnel from the hospital who provided invaluable assistance and support. This work was supported by Spanish Government Innovation, Science and Company Ministry (Excellence project P06-CTS-02341 (PREOBE) and Scottish Government (Rural and Environmental Scientific and Analytical Services (RESAS). Dr Luz Garcia Valdes gratefully acknowledges support from the Alfonso Martin Escudero Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on International Journal of Obesity website
Rights and permissions
About this article
Cite this article
Garcia-Valdes, L., Campoy, C., Hayes, H. et al. The impact of maternal obesity on iron status, placental transferrin receptor expression and hepcidin expression in human pregnancy. Int J Obes 39, 571–578 (2015). https://doi.org/10.1038/ijo.2015.3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2015.3
This article is cited by
-
Iron Profile in Term Small for Gestational Age Infants at 10 Weeks of Age and Correlation With Maternal Iron Profile: A Prospective Cohort Study
Indian Pediatrics (2023)
-
Iron transport across the human placenta is regulated by hepcidin
Pediatric Research (2022)
-
Association of maternal BMI during early pregnancy with infant anemia: a large Chinese birth cohort
Nutrition & Metabolism (2020)
-
Modification of the effects of prenatal manganese exposure on child neurodevelopment by maternal anemia and iron deficiency
Pediatric Research (2020)
-
Impact of maternal, antenatal and birth-associated factors on iron stores at birth: data from a prospective maternal–infant birth cohort
European Journal of Clinical Nutrition (2017)