Abstract
The independent and joint effects of within- and between-city contrasts in air pollution on mortality have been investigated rarely. To examine the differential effects of between- versus within-city contrasts in pollution exposure, we used both ambient measurements and land use regression models to assess associations with mortality and exposure to nitrogen dioxide (NO2) among ~735,600 adults in 10 of the largest Canadian cities. We estimated exposure contrasts partitioned into within- and between-city contrasts, and the sum of these as overall exposures, for every year from 1984 to 2006. Residential histories allowed us to follow subjects annually during the study period. We calculated hazard ratios (HRs) adjusted for many personal and contextual variables. In fully-adjusted, random-effects models, we found positive associations between overall NO2 exposures and mortality from non-accidental causes (HR per 5 p.p.b.: 1.05; 95% confidence interval (CI): 1.03–1.07), cardiovascular disease (HR per 5 p.p.b.: 1.04; 95% CI: 1.01–1.06), ischaemic heart disease (HR per 5 p.p.b.: 1.05; 95% CI: 1.02–1.08) and respiratory disease (HR per 5 p.p.b.: 1.04; 95% CI: 0.99–1.08), but not from cerebrovascular disease (HR per 5 p.p.b.: 1.01; 95% CI: 0.96–1.06). We found that most of these associations were determined by within-city contrasts, as opposed to by between-city contrasts in NO2. Our results suggest that variation in NO2 concentrations within a city may represent a more toxic mixture of pollution than variation between cities.
Similar content being viewed by others
INTRODUCTION
Previous cohort studies in the USA1, 2, 3, 4, 5, 6 and Europe7, 8, 9, 10, 11, 12 have shown positive associations between long-term exposure to ambient pollution or traffic exposure surrogates and mortality rates from non-accidental causes and cardiovascular diseases after adjusting for smoking and other risk factors. For example, in our previous study of the Canadian Census Health and Environment Cohort (CanCHEC),13 from which the present cohort is derived, we assigned estimates of fine particulate matter (particulate matter≤2.5 μm in diameter (PM2.5)) to 2.1 million non-immigrant adults and found hazard ratios (HRs) for mortality from non-accidental causes and cardiovascular disease of 1.10 (95% confidence intervals (CI): 1.05–1.15) and 1.15 (95% CI: 1.07–1.24), respectively, per 10-μg/m3 increase in PM2.5. Those exposures were derived from relatively coarse satellite-derived estimates (i.e., 10 × 10 km grid cells).
Within-city patterns of ambient pollution, nitrogen dioxide (NO2) in particular, are determined by traffic-related characteristics (e.g., street patterns and traffic counts), population densities, local land use patterns and physical geographical characteristics.14 Between-city contrasts in exposures on the other hand, are more influenced by climate, topography, presence of point-source emitters and overall city sizes.15 Estimates of exposure at finer spatial scales are expected to reduce exposure misclassification, resulting in more accurate estimates of association between air pollution and health outcomes. Most of the previous cohort studies of ambient air pollution and health focussed on either within-city or between-city and regional contrasts, but few have investigated these together. Studies on a Dutch cohort,7 however, considered estimates of exposure to regional concentrations of NO2 and black smoke, in addition to traffic intensity on nearby roads, and reported stronger associations with mortality and living near a major road than with background concentrations. Despite those findings, the general relationship between within- and between-city contrasts in exposure to ambient NO2 on mortality is still poorly understood.
Our objective here was to investigate associations between selected causes of mortality and exposure to NO2 from highly spatially resolved land use regression (LUR) models and from long-term fixed-site monitoring stations in a subset of the CanCHEC13, 16 residing in 10 of Canada’s largest cities. We sought to compare the strength of associations between mortality and NO2 concentrations among subjects using: (a) within-city contrasts of exposure (i.e., residential exposures); (b) between-city contrasts of exposure (i.e., city-wide mean exposures); and (c) the sum of these as overall exposures.
SUBJECTS AND METHODS
The Study Cohort
CanCHEC is a population-based cohort of subjects who were: ⩾25 years of age at baseline, a usual resident of Canada on the census reference day (4 June 1991), not a resident of an institution such as a prison, hospital or nursing home and among the 20% of Canadian households (about 3.6 million respondents) selected for enumeration with the mandatory long-form census questionnaire. The present study is limited to the 10 cities (not metropolitan areas) (Victoria, Vancouver, Edmonton, Winnipeg, Windsor, Sarnia, London, Hamilton, Toronto and Montreal) for which we had previously developed LUR surfaces for NO2. Subjects in CanCHEC were linked to the Canadian Mortality Database using deterministic and probabilistic linkage methods.16 We had date of death in days and underlying cause of death (coded to the International Classification of Diseases, 9th Revision (ICD-9 (ref. 17)) for deaths before 2000 and to ICD-10 (ref. 18) for those deaths registered from 2000 onward).
CanCHEC was amended to extend the years of mortality follow-up to 2006 and to link to annual place of residence (six-character postal code) from 1984 through 2006 using Historical Tax Summary Files.16 Residential histories were therefore unavailable in cases where a subject failed to file their annual income tax return. To assign estimates of exposure before the start of follow-up, we included only those subjects for whom we had residential histories in the study area during at least 4 years from 1984 to 1991 (i.e., ~98% of the subjects for whom we had exposure estimates at baseline).
In our study, we included the following covariates, which describe characteristics of subjects at baseline: immigrant status, visible minority status, marital status, employment status, highest level of education and quintiles of household income. Visible minorities are persons (other than aboriginal persons) who are non-Caucasian in race or non-white in colour.
Assignment of Exposure to Within-city Contrasts in NO2
We used LUR models that were developed separately for each of the 10 cities; the methods of sampling and modelling have been described previously.19, 20, 21, 22, 23, 24, 25, 26, 27 Briefly, we conducted sampling campaigns of ambient NO2 at between 39 and 133 locations per city using Ogawa passive diffusion samplers. Measurements were collected at different times between 2002 and 2010. We used these measurements in conjunction with data sets describing land use and traffic characteristics to develop city-specific models that described spatial patterns of NO2 across each city for the respective sampling periods. Although we used similar sampling approaches, equipment and data sets, the models for each city were created independently with the purpose of deriving the most locally appropriate exposure surface.
We assigned estimates of NO2 to the representative location of each subject’s residential six-character postal codes28 for every year from 1984 until the end of follow-up, under the condition that the subject had provided a residential address in one of the 10 study cities. That is, we accounted for subjects’ residential mobility within and between the 10 cities throughout follow-up. A subject’s exposure was coded as missing in years for which they provided either no residential postal code (which could indicate that they had left Canada or that they had simply failed to file their taxes that year) or a postal code located outside of the 10 cities (for which we had no exposure data). In Canadian urban areas, six-character residential postal codes most often correspond to a city block or a single apartment building. Next, we calculated the mean estimate of NO2 across the LUR model for each city and subtracted it from the residential exposures in the corresponding city, thus producing an exposure contrast describing the within-city component of exposure exclusively.
Assignment of Exposure to Between-city Contrasts in NO2 and Overall Exposures
To account for changes in the annual concentrations of NO2 over time, and because our LUR models were developed near, or after, the end of the follow-up period, we used historical observations of NO2 from Environment Canada’s National Air Pollution Surveillance network of fixed-site stations (http://www.ec.gc.ca/rnspa-naps) to estimate the between-city component of exposure. Environment Canada established the locations for these fixed-site stations across Canada with the purpose of monitoring and measuring background concentrations of criteria pollutants. The stations are specifically located away from major roads and from major point-source emitters. First, we calculated long-term city-wide trends in annual mean NO2 in each city for the period 1984 to 2006 using daily observations at available stations. The number of active stations in each city varied each year, ranging from only a single station in Sarnia in some years to 16 in Vancouver in some years. In each city, we then averaged the daily means across all active stations and calculated annual means. We then fit polynomial functions to these annual means, which allowed us to estimate smooth time trends describing the long-term temporal patterns in each city. This method did not consider changes in within-city spatial variability over time, but rather only the long-term trend in city-wide NO2, and it assumes that the trend is the same at all locations in the city. Therefore, every subject in a given city in a given year was assigned the same city-wide estimate of exposure.
Our method allowed us to assign to each subject an estimate of a within-city exposure contrast, a city-wide mean estimate of NO2 and then the sum of these as an estimate of overall NO2 exposure for each year from 1984 to the end of follow-up.
Finally, we calculated 7-year moving windows of exposure with a single-year lag (for each of within, between and overall exposures), beginning with estimates from 1984 (i.e., the earliest year available to us, and thus the largest window of exposure available to us). For example, each subject’s estimates of exposure at baseline were calculated as the mean of his or her annual exposures from 1984 to 1990 (i.e., the year previous to the year of follow-up). We implemented a 1-year lag because we assumed that any associations between mortality and NO2 are due to past exposures as opposed to those at the time of death and because the residential postal code provided on the final tax return (i.e., following a death) often differs from that on the death certificate, reflecting that of the next of kin or executor.29
Contextual Variables
We assigned contextual variables from the closest census year (i.e., either 1991, 1996, 2001 or 2006) to each subject annually using their postal code of residence linked to standard geographic identifiers. As such, contextual variables were reassigned each year, taking into account each subject’s residential location throughout the study area during the study period.
Contextual variables were calculated using Statistics Canada’s micro-level census data to describe: (1) demographic homogeneity, by the proportion of recent immigrants (i.e., within previous 5 years); (2) educational attainment, by the proportion of adults who had not completed high school and (3) economic status, by the proportion of individuals in the lowest income quintile in each census tract (CT) and in each city overall. Census tracts are defined to delineate neighbourhoods based on the physical characteristics of the landscape, administrative boundaries, and typically have populations of about 2,500–8,000 people with broadly similar socioeconomic profiles.30 To adjust for city-specific variations in these variables across the 10 cities, we subtracted the city mean from the values of each census tract. We thus defined two contextual measures for each of the three variables: the census division (CD) level and the census tract minus census division.
Local climate may influence the amount of time that subjects spend outdoors versus indoors, and may also modify associations between exposure and health outcomes.31, 32 Therefore, as an additional contextual covariate, we adjusted for city-specific annual mean temperature using data from first-order airport weather stations maintained by the Meteorological Service of Canada. That is, we assigned each year to each subject a time-varying estimate of the annual mean temperature corresponding to their city of residence.
Statistical Methods
We estimated HRs using standard Cox proportional hazards models and using random-effects models with city-level random effects, stratified by sex and by 5-year age groups from ages 25 to 89 years. We restricted our study to subjects <90 years of age due to potential inaccuracies in record-linkages among older subjects (e.g., the address reported on the annual income tax filings of older subjects may reflect those of next of kin or of institutional facilities). This age restriction was calculated as age during follow-up. That is, subjects >90 years of age were excluded at baseline, and other subjects were censored at the time of reaching that age, such that no models include any subjects aged ⩾90. Follow-up time was measured in days, and individuals were followed for mortality from 4 June 1991 to 31 December 2006. We developed models for mortality from ischaemic heart disease (ICD-9: codes 410–414; ICD-10: I20–I25), cerebrovascular disease (ICD-9: 430–434, 436–438; ICD-10: I60–I69), all cardiovascular diseases (ICD-9: 410–417, 420–438, 440–449; ICD-10: I20–I28, I30–I52, I60–I79), respiratory diseases (ICD-9: 460–519; ICD-10: J) and all non-accidental causes (ICD-9 codes<800; ICD-10 codes starting with letters A through R).
We ran two primary series of models: one in which we included the within- and between-city contrasts together, and one in which we included the overall exposures. The within-city HR estimates that we present are equivalent to fixed-effect pooled estimates of HRs estimated for each city separately. HRs were calculated per increment of 5 p.p.b. in NO2, which approximated the average inter-quartile range of the LUR NO2 concentrations. For both series of models, first we developed models including only NO2. Next, we added the personal-level covariates defined earlier. Then, we added the contextual covariates defined above.
Lastly, we used an empirical method33 to indirectly adjust for potential confounding by smoking behaviour and obesity. This method adjusts the observed HR for a series of risk factors not reported on the long-form census, while simultaneously controlling for the risk factors included in our survival model (e.g., education, income and contextual variables). The method requires estimates of the multivariate linear association between the variables in the survival model and the variables we indirectly adjust for. We obtained this association from an analysis of national health surveys34 for 2001, 2003 and 2005 for which we assigned our estimates of NO2 exposure to each subject completing the surveys. In particular, we were interested in indirectly adjusting for cigarette smoking habits (never, former or current cigarette smoker) and obesity as measured by body mass index (BMI). Details of our indirect adjustment are included in the Supplementary Information and Supplementary Table 1.
With results from the last model (i.e., fully-adjusted, random-effects model), we used Cochran’s Q-statistic35 to test heterogeneity in HRs for non-accidental mortality associated with overall exposures by age during follow-up (i.e., used follow-up of subjects only during specified age range).
RESULTS
There were ~736,000 subjects at baseline, 80,660 of whom died of non-accidental causes during follow-up (subject counts are rounded to meet Statistics Canada confidentiality requirements, proportions are based on unrounded counts; Table 1). There were more women than men (i.e., 52% versus 48%, respectively) and 35.8% were immigrants. Subjects in lower income categories had slightly higher exposures than those in higher income categories. At baseline (1991), subjects in Toronto and Hamilton had the highest mean overall exposures (i.e., 30.9 p.p.b. and 29.9 p.p.b., respectively) and those in Winnipeg and Victoria had the lowest (i.e., 18.3 p.p.b. and 20.5 p.p.b., respectively).
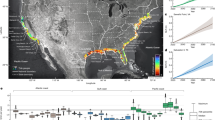
Table 2 provides summary information about the 10 cities and the 10 LUR models. Across the 10 original LURs, mean concentrations of NO2 ranged from 4.7 p.p.b. in London to 17.6 p.p.b. in Toronto, and the mean inter-quartile range was 4.3 p.p.b. We include as Supplementary Information and Supplementary Figure 1 an example of a typical LUR model, which depicts the spatial patterns of NO2 across Montreal. Temperatures in Edmonton and Winnipeg were notably colder than those in all other cities, and Victoria was characterised by the highest mean long-term temperature (Table 2). All 10 cities were characterised by generally decreasing concentrations over time (Supplementary Information and Supplementary Figure 2).
We compared models wherein exposure was modelled as a linear function to those in which it was modelled using splines with 2 and 3 degrees and found the best model fit (lowest Bayesian Information Criterion) in the linear model. All of our results are therefore based on a linear response function. Supplementary Information Table 2 shows the results of the standard Cox models for all five outcomes using each of the within-city, between-city and overall contrasts in NO2 according to covariate adjustments. The addition of personal and contextual covariates generally led to slightly decreased HRs associated with within-city contrasts, but had negligible effects on associations with the other two exposure estimates.
We present in Table 3 results from the fully-adjusted models with city-level random effects, indirectly adjusted for smoking and obesity. Generally, adjustment for smoking attenuated the associations between NO2 and mortality, adjustment for BMI strengthened the associations and adjustment for both together lead to little change in the original HRs. In our final models—with city-level random effects, adjusted for personal and contextual covariates and for smoking and obesity—we found positive associations with estimates of overall NO2 exposure and non-accidental mortality (HR: 1.05; 95% CI: 1.03–1.07), cardiovascular disease (HR: 1.04, 95% CI: 1.01–1.06), ischaemic heart disease (HR: 1.05, 95% CI: 1.02–1.08) and respiratory disease (HR: 1.04, 95% CI: 0.99–1.08), but no association for cerebrovascular disease (HR: 1.01, 95% CI: 0.96–1.06). In models with exposure partitioned into within-city and between-city components, we found no positive associations with the between-city contrasts, and similar associations with the within-city contrasts to those reported with the overall exposures. With these final models, we also performed statistical tests and compared P-values for differences between the coefficients for within-city and between-city contrasts. Here, we found that only the coefficients in models from deaths, non-accidental and respiratory diseases were significantly different at P<0.05 (results not shown).
We found significant effect modification by age for associations between overall NO2 exposures and non-accidental mortality (Table 4). Specifically, we found stronger associations among subjects aged <60 as compared with those aged 60–79 (i.e., HRs and 95% CIs: 1.14; 1.11–1.18 and 1.06; 1.04–1.08, respectively) and essentially no association among subjects aged 80–89.
DISCUSSION
In this population-based cohort study of ~735,590 subjects in 10 of the largest cities in Canada, while accounting for residential mobility through 16 years of follow-up, we found that exposure to outdoor NO2 was positively associated with mortality from several important causes of death. Moreover, we found that these associations were determined largely by residential, within-city contrasts in exposure as opposed to by contrasts in city-wide mean exposures between cities. Specifically, we found that a 5 p.p.b. increase in within-city contrasts in NO2 in our final models contributed to increases in mortality from non-accidental causes, cardiovascular, ischaemic heart and respiratory diseases of ~5% (95% CI: 4–7), 4% (95% CI: 2–7), 5% (95% CI: 2–9) and 8%,3, 4, 5, 6, 7, 8, 9, 10, 11, 12 respectively. In contrast, we found that between-city contrasts in exposure produced no clear, independent increase in risk of mortality.
A recent review36 of 14 studies that accounted for intra-urban spatial variation in NO2 reported a random-effects summary estimate for all-cause mortality of 5.5% (95% CI: 3.1–8.0%) per increment of 5.3 p.p.b., and noted significant heterogeneity of effect estimates across studies. In a cohort study of over 200,000 different subjects living in Hamilton, Toronto, Windsor and Ontario, Chen et al.37 assigned estimates of exposure to NO2 based on the same LUR models used here. In pooled models among subjects aged 35 to 85 years (adjusted for a slightly different set of covariates than used here), they reported increased risks of mortality per 5 p.p.b. of 8% (95% CI: 5–11%) from cardiovascular disease and of 9% (95% CI: 4–14%) from ischaemic heart disease—similar to, although somewhat stronger than, the associations found here. The associations that we found for cardiovascular mortality and NO2 were also similar to those reported in cohort studies in Rome,10 the Netherlands,7 and Norway38 (all in the range of 3–8% increased risk). We found weak to no association with mortality from cerebrovascular disease, which is similar to results reported elsewhere.9, 10, 11, 37
Very few studies have considered associations between mortality from respiratory diseases and long-term exposure to ambient air pollution (fewer still with NO2 specifically). There have been inconsistent findings among the existing studies, and there have been calls in the literature for more studies to evaluate associations between exposure and this outcome.36 A recent national English cohort study,12 found stronger associations with NO2 and respiratory mortality than with cardiovascular mortality. Here, with within-city contrasts in NO2, we also found stronger associations with respiratory mortality (HR: 1.08; 95% CI: 1.03–1.12) than with cardiovascular mortality (HR: 1.04; 95% CI: 1.02–1.07). We also found apparent protective effects for between-city contrasts and risk of respiratory mortality (HR: 0.89; 95% CI: 0.84–0.94). Our estimates for between- and within-city contrasts of NO2 and respiratory disease appear, however, to be less stable than those from the other causes of disease, which is likely due to the small number of respiratory deaths. We note that for all other causes, the HR associated with overall exposures is very close to that associated with the within-city contrasts and the HR for between-city contrasts is close to null. In the case of respiratory disease, we found that the HR for within-city contrasts is notably higher than that for overall exposures, and the HR for between-city contrasts is notably lower than null.
Alternatively, the fact that we found positive associations with local, within-city contrasts, but not with background, between-city contrasts somewhat corroborates the hypothesis that “respiratory mortality may be more related to primary traffic-related pollutants than with long-range transported particles” (the study by Hoek et al.,36 page 12). Anecdotally, with data from 2000–2002 Statistics Canada Vital Statistics, we found a negative correlation (r=−0.6) between long-term city-wide concentrations of NO2 and city-specific age-standardized mortality rates from respiratory disease across our 10 cities (results not shown). The two cities with the highest long-term concentrations of NO2 (namely, Toronto and Windsor) had by far the lowest mortality rates from respiratory disease. This apparent negative association between city-level NO2 and respiratory mortality likely contributes to the negative associations that we report here with our between-city contrasts in exposure.
City-wide mean NO2 (across all 10 cities, 1984 to 2006) was correlated with city-level percentage of immigrants and percentage of adults who had not completed high school (Pearson correlation coefficient (r)=0.60 and 0.38, respectively), but not with the percentage of the subjects in the lowest income quintile (r=−0.07). We also found generally larger coefficients for the city-level contextual covariates than for the census tract deviation from city-level covariates (Supplementary Information and Supplementary Table 3).
The fact that we found essentially no associations with mortality and between-city contrasts in exposure is not completely unexpected and could be attributed to several factors. In part, with only 10 cities, we may have had too little variability in exposures to detect between-city differences. In addition, our results may suggest that the between-city contrasts are more of a reflection of overall ambient exposures than of NO2 exposures specifically. It is also likely, therefore, that there are differences in factors that were unmeasured and unaccounted for in our models, including concentrations of other pollutants. The mixtures and degree of photochemical processing and hence the levels of toxicity of the ambient pollutant mix likely vary between cities. Our results suggest, therefore, that an exposure change of say 10 p.p.b. of NO2 across Montreal poses a different risk to health compared with a 10 p.p.b. change in NO2 across Toronto or Victoria. Unfortunately, we did not have access to exposure data at a high enough spatial resolution to allow us to control for within-city patterns of other pollutants (e.g., PM2.5 and SO2).
Furthermore, the city-wide mean estimates of NO2 measured at the fixed-site stations were likely insufficient for describing the full range of ambient concentrations within each city generally, and likely had differing ability to represent the exposure circumstances by city.39 Last, in some cities sub-groups of the population that may be more susceptible to the effects of exposure (e.g., socially and financially deprived individuals)40 may also be living in the areas of each city with the highest levels of pollution or vice versa. Our null findings here also somewhat echo those reported in two previous US cohort studies,41, 42 which reported that the health effects associated with within-city gradients in PM2.5 were larger than those found with between-city estimates.
There have been mixed reports on the evidence for effect modification by age in the association between air pollution and mortality. As noted earlier, we found no associations between NO2 and non-accidental mortality among subjects aged ⩾80. Among subjects in their large Italian cohort, Cesaroni et al.10 reported stronger associations between NO2 and mortality from non-accidental causes among subjects <60 years of age compared with among older groups. Conversely, Chen et al.37 found no evidence of effect modification by age in their study of NO2 and mortality in three Canadian cities. This is an issue that requires further study.
A key strength of this study is the large sample size and broadly representative nature of the cohort.16 We were able to include subjects from the three largest cities in Canada (i.e., Toronto, Montreal and Vancouver) and from cities in five different provinces (i.e., British Columbia, Alberta, Manitoba, Ontario and Quebec). Another strength of our study is that we were able to track each subject’s residential mobility for each year of follow-up, which allowed us to assign annual estimates of exposure as subjects relocated within the study area, thus reducing exposure misclassification bias. Approximately 80% of subjects (~600,000) moved at least once during follow-up, and would have contributed to additional exposure misclassification if we had assigned exposure only to their representative location at baseline. In our future work, we will explore the extent of the misclassification.
We also had the advantage of being able to include only subjects who had been residing in the study area for at least 4 of the 7 years prior to follow-up, thus ensuring better estimates of long-term exposure. Furthermore, the 7-year moving average of exposure allowed us to compare events against a consistent, relatively long-term period of exposure.
An additional strength of this study is that our exposure estimates were derived from highly spatially resolved LUR surfaces that were developed independently, using predictor variables and model structures specific to each city. This is the first multi-city cohort study of mortality in which individual-level estimates of exposure were assigned to each subject, and that allowed for comparison of within- and between-city effects.
A limitation of our analysis is that our sampling periods for NO2 in each city were at or beyond the end of the follow-up period. Our scaling approach allowed us to adjust our exposure estimates to reflect historical city-wide trends, but assumed that the spatial patterns within each city remained constant. Previous studies in Montreal,43 Vancouver,26 Rome44 and The Netherlands,45 however, reported that the general spatial patterns of NO2 within large cities tend to remain fairly stable over time—at least within a 5–10-year period. Recently, Gulliver et al.46 demonstrated that LUR models for NO2 across Great Britain could be back-extrapolated 18 years (from 2009 to 1991) and provide valid estimates of historic concentrations. There are no other extant studies, nor sufficient data, to evaluate long-term patterns in NO2 over greater periods for any city in Canada. In this context, it is important to note that our LUR models are restricted to the main city boundaries of each city, and do not cover the greater, suburban areas, where growth, expansion and urban change would have occurred most substantially in each city during the period of our follow-up. For example, our model for Montreal covers only the Island of Montreal, and does not include the communities of Laval or the South Shore, where substantial new development and expansion would have occurred during this period.
Although, we lacked reported information on smoking behaviour and obesity, which are important risk factors for cardiovascular mortality, we were able to adjust for those jointly and indirectly. The indirect adjustment produced only marginal changes to our results, which is consistent with other cohort studies that have also used this approach.13, 37, 47 We do not have extensive information on smoking or BMI spatial patterns in Canada prior to 2001 and thus cannot evaluate the temporal changes in this association over time. We acknowledge that this is a limitation in our data sets.
In summary, we found positive associations between long-term exposure to local concentrations of NO2 and selected causes of mortality among subjects living in 10 Canadian cities. We found weaker associations among older subjects. We found the strongest associations with mortality from ischaemic heart and respiratory diseases. Importantly, we found stronger associations with cause-specific mortality and within-city contrasts than with between-city contrasts in NO2, suggesting an important role for local traffic emissions on the health risks of long-term exposure to urban air pollution.
References
Dockery DW, Pope CA, 3rd, Xu X, Spengler JD, Ware JH, Fay ME et al. An association between air pollution and mortality in six U.S. cities. N Engl J Med 1993; 329: 1753–1759.
Krewski D, Jerrett M, Burnett RT, Ma R, Hughes E, Shi Y et al. Extended follow-up and spatial analysis of the American Cancer Society study linking particulate air pollution and mortality. Res Rep Health Eff Inst 2009; 140: 5–114.
Laden F, Schwartz J, Speizer FE, Dockery DW . Reduction in fine particulate air pollution and mortality: extended follow-up of the Harvard Six Cities study. Am J Respir Crit Care Med 2006; 173: 667–672.
Pope CA, 3rd, Burnett RT, Thun MJ, Calle EE, Krewski D, Ito K et al. Lung cancer, cardiopulmonary mortality, and long-term exposure to fine particulate air pollution. JAMA 2002; 287: 1132–1141.
Pope CA, 3rd, Thun MJ, Namboodiri MM, Dockery DW, Evans JS, Speizer FE et al. Particulate air pollution as a predictor of mortality in a prospective study of U.S. adults. Am J Respir Crit Care Med 1995; 151: 669–674.
Jerrett M, Burnett RT, Beckerman BS, Turner MC, Krewski D, Thurston G et al. Spatial analysis of air pollution and mortality in California. Am J Respir Crit Care Med 2013; 188: 593–599.
Beelen R, Hoek G, van den Brandt PA, Goldbohm RA, Fischer P, Schouten LJ et al. Long-term effects of traffic-related air pollution on mortality in a Dutch cohort (NLCS-AIR study). Environ Health Perspect 2008; 116: 196–202.
Hoek G, Brunekreef B, Goldbohm S, Fischer P, van den Brandt PA . Association between mortality and indicators of traffic-related air pollution in the Netherlands: a cohort study. Lancet 2002; 360: 1203–1209.
Nafstad P, Haheim LL, Wisloff T, Gram F, Oftedal B, Holme I et al. Urban air pollution and mortality in a cohort of Norwegian men. Environ Health Perspect 2004; 112: 610–615.
Cesaroni G, Badaloni C, Gariazzo C, Stafoggia M, Sozzi R, Davoli M et al. Long-term exposure to urban air pollution and mortality in a cohort of more than a million adults in Rome. Environ Health Perspect 2013; 121: 324–331.
Raaschou-Nielsen O, Andersen ZJ, Jensen SS, Ketzel M, Sorensen M, Hansen J et al. Traffic air pollution and mortality from cardiovascular disease and all causes: a Danish cohort study. Environ Health 2012; 11: 60.
Carey IM, Atkinson RW, Kent AJ, van Staa T, Cook DG, Anderson HR . Mortality associations with long-term exposure to outdoor air pollution in a national English cohort. Am J Respir Crit Care Med 2013; 187: 1226–1233.
Crouse DL, Peters PA, van Donkelaar A, Goldberg MS, Villeneuve PJ, Brion O et al. Risk of nonaccidental and cardiovascular mortality in relation to long-term exposure to low concentrations of fine particulate matter: a Canadian national-level cohort study. Environ Health Perspect 2012; 120: 708–714.
Hoek G, Beelen R, de Hoogh K, Vienneau D, Gulliver J, Fischer P et al. A review of land-use regression models to assess spatial variation of outdoor air pollution. Atmos Environ 2008; 42: 7561–7578.
Jacobson M Atmospheric Pollution: History, Science, and Regulation. Cambridge University Press: Cambridge, UK, 2002.
Peters PA, Tjepkema M, Wilkins R, Fines P, Crouse DL, Chan PC et al. Data resource profile: 1991 Canadian Census Cohort. Int J Epidemiol 2013; 42: 1319–1326.
WHO. Manual of the International Statistical Classification of Diseases, Injuries and Causes of Death, Geneva, 9th Revision, 1977.
WHO. International Statistical Classification of Diseases and Related Health Problems, Geneva, 10th Revision, 1992.
Allen RW, Amram O, Wheeler AJ, Brauer M . The transferability of NO and NO2 land use regression models between cities and pollutants. Atmos Environ 2011; 45: 369–378.
Atari DO, Luginaah I, Xu X, Fung K . Spatial variability of ambient nitrogen dioxide and sulfur dioxide in Sarnia, “Chemical Valley,” Ontario, Canada. J Toxicol Environ Health A 2008; 71: 1572–1581.
Crouse DL, Goldberg MS, Ross NA . A prediction-based approach to modelling temporal and spatial variability of traffic-related air pollution in Montreal, Canada. Atmos Environ 2009; 43: 5075–5084.
Jerrett M, Arain MA, Kanaroglou P, Beckerman B, Crouse DL, Gilbert NL et al. Modeling the intraurban variability of ambient traffic pollution in Toronto, Canada. J Toxicol Environ Health A 2007; 70: 200–212.
Oiamo TH, Luginaah I, Buzzelli M, Tang K, Xu X, Brook J et al. Assessing the spatial distribution of nitrogen dioxide in London, Ontario. J Air Waste Manag Assoc 2012; 62: 1335–1345.
Poplawski K, Gould T, Setton E, Allen R, Su J, Larson T et al. Intercity transferability of land use regression models for estimating ambient concentrations of nitrogen dioxide. J Expo Sci Environ Epidemiol 2009; 19: 107–117.
Sahsuvaroglu T, Arain A, Kanaroglou P, Finkelstein N, Newbold B, Jerrett M et al. A land use regression model for predicting ambient concentrations of nitrogen dioxide in Hamilton, Ontario, Canada. J Air Waste Manag Assoc 2006; 56: 1059–1069.
Wang R, Henderson S, Sbihi H, Allen R, Brauer M . Temporal Stability of Land Use Regression Models for Traffic-Related Air Pollution. Atmos Environ 2013; 64: 312–319.
Wheeler AJ, Smith-Doiron M, Xu X, Gilbert NL, Brook J . Intra-urban variability of air pollution in Windsor, Ontario—Measurement and modeling for human exposure assessment. Environ Res 2008; 106: 7–16.
Wilkins R, Peters P PCCF+ Version 5K User’s Guide: Automated Geocoding Based on the Statistics Canada Postal Code Conversion Files. Statistics Canada: Ottawa, ON, Canada, 2012. Catalogue 82F0086-XDB..
Canada Revenue AgencyPreparing Returns for Deceased Persons, Canada Revenue Agency, Ottawa, ON, Canada, 2012. Guide T4011(E) Rev. 12..
Ross NA, Tremblay SS, Graham K . Neighbourhood influences on health in Montreal, Canada. Soc Sci Med 2004; 59: 1485–1494.
Vanos JK, Cakmak S, Bristow C, Brion V, Tremblay N, Martin SL et al. Synoptic weather typing applied to air pollution mortality among the elderly in 10 Canadian cities. Environ Res 2013; 126: 66–75.
Vanos JK, Hebbern C, Cakmak S . Risk assessment for cardiovascular and respiratory mortality due to air pollution and synoptic meteorology in 10 Canadian cities. Environ Pollut 2014; 185: 322–332.
Shin HH, Cakmak S, Brion O, Villeneuve PJ, Turner MC, Goldberg MS et al. Indirect adjustment for multiple missing variables applicable to environmental epidemiology. Environ Res 2014; 134: 482–487.
Statistics Canada. Canadian Community Health Survey 2003: User Guide for the Public Use Microdata File. Statistics Canada: Ottawa, ON, Canada, 2005. Catalogue no. 82M0013GPE.
Axelson O . Aspects of confounding and effect modification in the assessment of occupational cancer risk. J Toxicol Environ Health 1980; 6: 1127–1131.
Hoek G, Krishnan RM, Beelen R, Peters A, Ostro B, Brunekreef B et al. Long-term air pollution exposure and cardio- respiratory mortality: a review. Environ Health 2013; 12: 43.
Chen H, Goldberg MS, Burnett RT, Jerrett M, Wheeler AJ, Villeneuve PJ . Long-term exposure to traffic-related air pollution and cardiovascular mortality. Epidemiology 2013; 24: 35–43.
Naess O, Nafstad P, Aamodt G, Claussen B, Rosland P . Relation between concentration of air pollution and cause-specific mortality: four-year exposures to nitrogen dioxide and particulate matter pollutants in 470 neighborhoods in Oslo, Norway. Am J Epidemiol 2007; 165: 435–443.
Levy I, Mihele C, Lu G, Narayan J, Brook JR . Evaluating multipollutant exposure and urban air quality: pollutant interrelationships, neighborhood variability, and nitrogen dioxide as a proxy pollutant. Environ Health Perspect 2013; 122: 65–72.
Crouse DL, Ross NA, Goldberg MS . Double burden of deprivation and high concentrations of ambient air pollution at the neighbourhood scale in Montreal, Canada. Soc Sci Med 2009; 69: 971–981.
Jerrett M, Burnett RT, Ma R, Pope CA, 3rd, Krewski D, Newbold KB et al. Spatial analysis of air pollution and mortality in Los Angeles. Epidemiology 2005; 16: 727–736.
Miller KA, Siscovick DS, Sheppard L, Shepherd K, Sullivan JH, Anderson GL et al. Long-term exposure to air pollution and incidence of cardiovascular events in women. N Engl j Med 2007; 356: 447–458.
Crouse DL, Goldberg MS, Ross NA, Chen H, Labreche F . Postmenopausal breast cancer is associated with exposure to traffic-related air pollution in Montreal, Canada: a case-control study. Environ Health Perspect 2010; 118: 1578–1583.
Cesaroni G, Porta D, Badaloni C, Stafoggia M, Eeftens M, Meliefste K et al. Nitrogen dioxide levels estimated from land use regression models several years apart and association with mortality in a large cohort study. Environ Health Perspect 2012; 11: 48.
Eeftens M, Beelen R, Fischer P, Brunekreef B, Meliefste K, Hoek G . Stability of measured and modelled spatial contrasts in NO(2) over time. Occup Environ Med 2011; 68: 765–770.
Gulliver J, de Hoogh K, Hansell A, Vienneau D . Development and back-extrapolation of NO2 land use regression models for historic exposure assessment in Great Britain. Environ Sci Technol 2013; 47: 7804–7811.
Villeneuve PJ, Jerrett M, Su J, Burnett RT, Chen H, Brook J et al. A cohort study of intra-urban variations in volatile organic compounds and mortality, Toronto, Canada. Environ Pollut 2013; 183: 30–39.
Acknowledgements
We thank Stan Judek of Health Canada for compiling the nitrogen dioxide data from the National Air Pollution Surveillance network.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interests.
Additional information
Supplementary Information accompanies the paper on the Journal of Exposure Science and Environmental Epidemiology website
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Crouse, D., Peters, P., Villeneuve, P. et al. Within- and between-city contrasts in nitrogen dioxide and mortality in 10 Canadian cities; a subset of the Canadian Census Health and Environment Cohort (CanCHEC). J Expo Sci Environ Epidemiol 25, 482–489 (2015). https://doi.org/10.1038/jes.2014.89
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jes.2014.89
Keywords
This article is cited by
-
Intra-urban variability of long-term exposure to PM2.5 and NO2 in five cities in Colombia
Environmental Science and Pollution Research (2023)
-
Global fine-scale changes in ambient NO2 during COVID-19 lockdowns
Nature (2022)
-
A comprehensive evaluation of the association between ambient air pollution and adverse health outcomes of major organ systems: a systematic review with a worldwide approach
Environmental Science and Pollution Research (2019)
-
The Canadian Urban Environmental Health Research Consortium – a protocol for building a national environmental exposure data platform for integrated analyses of urban form and health
BMC Public Health (2018)
-
Air Pollution and Cardiovascular Disease: a Focus on Vulnerable Populations Worldwide
Current Epidemiology Reports (2018)