Abstract
Aim:
To investigate the effects of inhaler device technique education on improving inhaler technique in older people with asthma.
Methods:
In a randomised controlled trial, device technique education was provided to a sample of 123 adults aged >55 years who had a doctor diagnosis of asthma. The active education group received one-on-one technique coaching, including observation, verbal instruction and physical demonstration at baseline. The passive group received a device-specific instruction pamphlet only. Inhaler technique, including the critical steps for each device type, was assessed and scored according to Australian National Asthma Council (NAC) guidelines. Device technique was scored objectively at baseline and again at 3 and 12 months post education.
Results:
The majority of participants demonstrated poor technique at baseline. Only 11 (21%) of the active intervention group and 7 (16%) of the passive group demonstrated 100% correct technique. By 3 months 26 (48%) of the active group achieved adequate technique. Improvement in technique was observed in the active group at 3 months (P<0.001) and remained significant at 12 months (P<0.001). No statistically significant improvement was observed in the passive group.
Conclusion:
The provision of active device technique education improves device technique in older adults. Passive education alone fails to achieve any improvement in device technique.
Similar content being viewed by others
Introduction
In asthma self-management, ineffective inhalation technique and mishandling of devices is a common and widespread issue even among experienced adults.1,2 Good device technique is essential to maximise the benefits of asthma treatment3,4 and poor technique is associated with having poor asthma control, increased use of unscheduled health resources and poor adherence if therapeutic benefits are not experienced.1,4–6
Many types of inhalation devices are now available and current evidence indicates no difference in the clinical effectiveness of one device over another provided they are used properly.7 However, devices differ in the way they are used. The correct inspiration technique for a pressurised metered-dose inhaler requires a slow deep breath, while a dry powder device requires a faster initial breath. The correct technique is thus device-specific and treatment efficacy relies on the method being taught effectively for each specific inhaler.7–9 Device effectiveness is also dependent on patient-related factors such as manual dexterity and coordination. Drug choice, capacity to achieve targeted inspiratory flow and the skill to master a particular device also has a bearing on real-world efficacy.8–10
Asthma guidelines recommend regular monitoring of inhaler technique as part of good asthma management,11 and research has highlighted the need for inclusion of physical demonstration.12,13 Although device technique education has been shown to improve asthma outcomes, few educational interventions have focused on older adults or considered their specific needs.
Poor device technique is more often observed in older patients.1,14,15 Poor cognition, impaired vision and device handling are some reasons for this observation.15–18 Disease comorbidity is also common in older adults who may be taking multiple medications in addition to their asthma therapy.19 Use of multiple different devices has been shown to increase the risk of inadequate device technique in adults.20 Added to this, older patients’ perception of their inhaler technique has been shown to be a poor indicator of their actual ability.18
Although research has shown that older people can learn to improve their inhaler technique,21 only one previous study provided a device educational programme for older people, and this did not include those using dry powder inhalers, a control group or a tailored programme to address individual needs.22
The supposition of this study is that device technique can be improved and maintained in older people where education, including observation, verbal instruction and physical demonstration, and device-related knowledge are provided.
Materials and Methods
Study design
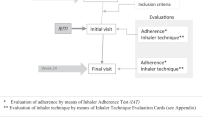
This paper presents a subanalysis of a single-blinded parallel randomised controlled trial measuring the effects of a tailored education intervention designed to address the concerns and unmet needs of older people with asthma.23 The aim of the current analysis was to investigate the effects of comprehensive device technique education versus passive information alone for older people with asthma.
Participants
Participants were recruited from the community across two trial sites in New South Wales and Victoria, Australia. Computer-generated stratified randomisation by age and site and preventer medication were used to allocate participants to either the comprehensive or the brochure-only arm of the intervention. All participants were aged >55 years and had a doctor diagnosis of asthma, a smoking history of <10 pack-years and were considered cognitively competent to understand instructions. Participants were blinded to their group allocation.
Ethics approval was obtained from the ethics committees of both sites.
Intervention
The comprehensive education intervention group received one-on-one technique coaching, which included critical observation of their device technique, verbal instruction regarding ways to improve their technique, physical demonstration of correct technique and encouragement. Education was provided at baseline. At 3- and 12-month visits, participants were asked to use their inhaler and technique was discretely observed. Additional technique coaching was provided where errors were observed. They were also provided with pictorial device information pamphlets. Patients in the active intervention group also received asthma education. This included knowledge about their particular inhalation devices, why good technique was important, and ways to improve the technique. Where patient-related factors affecting mastery over the device technique (such as difficulties associated with arthritis or inspiratory flow) were evident, other device options were also discussed and suggested to their practitioner. The passive information group participants received only the pictorial device information pamphlet and usual care by their practitioner. At the end of the study, the passive group received the interactive education.
The device information pamphlets were standard educational pamphlets supplied by Astra-Zeneca (North Ryde, NSW, Australia) and GlaxoSmithKline (Ermington, NSW, Australia) to healthcare practitioners. Turbuhaler device users received pamphlets provided by Astra-Zeneca, and pressurised metered-dose inhaler (pMDI) and Accuhaler device pamphlets were provided by GlaxoSmithKline.
Outcome measures
Device technique was reviewed in both groups, at baseline and at 3 and 12 months. In the active group, this was done prior to education. Device technique was assessed discretely according to current National Asthma Council (NAC) guidelines24 and critical inhaler technique steps were scored using the NAC checklist for each device.25 The checklists can be downloaded from the NAC website http://www.nationalasthma.org.au/publication/inhaler-technique-in-adults-with-asthma-or-copd. Lung function, asthma control and medication adherence were also measured as part of the wider intervention.23 Demographic information on participant characteristics was also collected.
Data analysis
Data were analysed using SPSS (Statistical Package for Social Sciences Version 19, Chicago, IL, 2010). Device checklist steps and scores were converted to percentages for comparison between devices. Associations between inhaler-related variables, correct technique and device errors were assessed using univariate and multivariate linear regression. Spearman’s correlation coefficient was used to examine nonparametric correlations. Comparisons between intervention and control groups were made using general linear models.
Results
Baseline characteristics
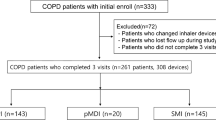
There were 123 participants in the study at baseline; 67 (54.5%) were using a dry power inhaler (DPI), 33 (26.8%) a pMDI preventer and 2 (1.6%) used a breath-activated AutohalerTM (Table 1). The remaining participants used no preventer (15%), a nebuliser (1.6%) or oral preventer alone (0.8%). No significant differences between the two groups were observed at baseline other than a greater number of participants in the active group who were using an Accuhaler (P<0.01).
The most common critical step errors observed for pMDI, Turbuhaler and Accuhaler devices at baseline are listed in Table 2. Across both groups, participants using an Accuhaler were more likely to employ the correct technique at baseline (t=2.79, P=0.006). Those using a pMDI (t=0.36, P=0.7), Turbuhaler device (t=−0.63, P=0.5) or those who owned a number of asthma devices (r=0.03, P=0.8) were no more likely to have a good technique using these devices.
At baseline 11 (21%) of the active group and 7 (16%) of the passive group were assessed as having the correct technique and there were no significant differences in device technique between the two groups (F=0.23, P=0.6).
Effects of the education intervention
Post education there was a statistically significant improvement in the proportion of participants with correct technique in the active group at 3-month follow-up (P<0.001), which was retained at the 12-month follow-up (P<0.001) (Table 3). In comparison, no significant change was evident in the passive group at 3 months (P=0.5) and 12 months (P=0.6) post intervention.
Between the baseline and 3-month follow-up visit, 7(6%) patients changed devices (4 from the active and 3 from the passive group) and a further 13 (11%) (10 from the active and 3 from the passive group) did so by the 12-month follow-up. The changes between devices were patient-specific, and no pattern was observed in the switching between devices across the two groups. Device changes had no effect over technique scores achieved at 3 months (P=0.6) or 12 months (P=0.8).
The proportion of patients achieving a maximal technique score in the active group at 3 months was 26 (48%) vs. 10 (20%) in the passive group and at 12 months 27 (52%) active participants retained maximal score versus 8 (26%) passive participants. The number of device errors made by those who did not achieve maximal score was initially higher in the active group (mean (s.d.) 2.7 (0.3) and 2.23 (0.2); active and passive group respectively). Post education intervention, the active group made fewer errors (Figure 1). At 3 months the active group made on average 1.21(1.4) errors and 0.91 (1.0) by 12 months whereas the passive group continued to produce similar errors with a mean of 2.05 (1.6) at 3- and 12-months.
Active participants using a pMDI device were encouraged to utilise a large volumatic spacer (LVS) with their pMDI device as a part of device education. Initially, 7 (43.8%) pMDI users in the active group and 7 (41.2%) in the passive group were using a spacer. By 3-month follow-up a greater proportion of both groups had started using an LVS (Figure 2); however, uptake was statistically higher in the active group compared with the passive group (3 months: P=0.001; 12 months: P<0.0001). Device technique was also better amongst those who used a spacer compared with pMDI alone. This was true in both active and control groups. At 12-month follow-up 9/15 (60%) active participants achieved maximal technique score using a spacer versus 1/3 (33%) who continued using a pMDI alone, while 4/11 (36%) control participants using a spacer achieved maximal score versus 1/9 (11%) with pMDI alone.
Discussion
Main findings
In older people asthma education is often neglected, and while acquisition and initial retention of acceptable technique is reduced in the elderly with a measurable cognitive deficit,27 this is not an excuse for neglect. This investigation has shown that device education, in particular, practical demonstration and coaching, can effectively improve the device technique of older people. It also asserts that written information, even in pictorial form, is not sufficient to achieve improved inhaler use in older adults with asthma.
Previous studies have found that older people have a significantly poorer device technique than younger adults.14 In this older cohort, inadequate technique was high at baseline, with 81% demonstrating at least one observed error. Correct device technique was, however, associated with the type of device used; specifically, the use of the Accuhaler was more likely to be correct, as measured by the checklist. In this study, a third of the participants used a pMDI preventer at baseline and the majority used a pMDI as their reliever device. Spacer uptake in the active group improved and was sustained as a result of device education. Thus, with device education good device technique was achieved amongst both DPI and pMDI users.
Interpretation of findings in relation to the previously published work
Within the period of one year, device technique was observed three times. Clear statistical improvement was observed in the active education group but was not observed in the passive education group. In the active group, good technique was sustained between 3- and 12-months suggesting that once the technique was improved it was retained for at least 9 months.
In younger and older populations it has been shown that pMDIs are more difficult to use, and that it is more difficult to maintain good technique compared with DPIs,28–30 and this has a bearing on asthma control. Dry powder devices generally require fewer technical skills to operate and in our study Accuhaler was used correctly at baseline by a larger proportion of participants than pMDI devices or Turbohaler DPIs. While DPIs may be easier to use, education is no less important.13 The majority of active and passive participants who were using DPIs failed to exhale before inhalation, had a tendency to breathe out over or into the device. Failure to exhale before inhalation is the most frequently reported error associated with DPI devices.28,31 Previous studies have demonstrated that exhaling over a DPI has the propensity to cause excess moisture to develop and decrease the delivery of future doses.32
With pMDI devices, better technique and thus better drug delivery of pMDIs can be obtained with a spacer2,33 and guidelines recommend their use in all age groups. Utilisation of these devices can, however, be a financial barrier to some patients. In this study, providing device education to pMDI users had an impact on spacer uptake. Spacers offer considerable advantages over pMDIs alone in the elderly34 and more recent evidence suggests better asthma control is achieved with a spacer or Autohaler.35 Our study adds to the evidence by demonstrating that adults using a pMDI can be taught to use a spacer and achieve better technique.
Strengths and limitations of this study
Few studies have specifically addressed the role of patient education in the older person. The strengths of this study are that it uses step-by-step guidelines to assess and teach optimal device technique.
As a limitation in this study, the effect of spacer uptake may be underestimated as all participants, including the passive group, underwent spirometry in which bronchodilator effect was measured. A disposable LVS was used for operator administration of the bronchodilator. No education was provided, yet a few control group participants commenced using a spacer with their pMDI, commenting that the use of a spacer during spirometry prompted them to start using or re-using a spacer. Frequent spirometry may also contribute to improving inhaler technique. However, spacer use was not sustained in the passive group, and the decline in spacer use in this group between 3- and 12-month follow-up suggests that the novelty wore off without education about the benefits of spacer use.
The study could have been influenced by observer bias in that, while the asthma educators were blinded to the initial randomised allocation, they were not blinded when evaluating individual device technique. However, an objective scoring system was used to standardise this assessment throughout. We did not assess participant cognition, and do not know whether the small proportion of the active group who were not able to attain correct technique were thus impaired.
Implications for future research, policy and practice
Providing patients with written information alone is inadequate in ensuring that device technique is performed. In older people with asthma, even with years of experience of living with the disease, inhaler education with demonstration and coaching is important, and can achieve good results. Several aspects of inhaler technique are skill-based and require training before they can be performed.14 Device preparation, inhalation method, actuation and breath holding are steps that require teaching and practical demonstration. In younger populations, practical demonstration has proven to be more effective in improving technique than written or verbal information.12
Older people with a long history of asthma may express confidence in their device use; however, evidence suggests their confidence is not well founded, and technique has been shown to deteriorate if it is not revisited.36 Dekhuijzen37 has recently proposed a patient-centred approach for prescribing inhaler devices in primary care. We would add that any approach needs to include and revisit device technique education, even in the later years, to achieve better outcomes.
New technologies such as telemedicine are changing the interface of the patient consultation. Provided observation and coaching can be delivered, the desired outcomes can be achieved. The internet is also becoming increasingly important as a tool for clinicians and patients, and video demonstrations of correct device technique are available from respiratory bodies and manufacturers. However, without someone with the knowledge to observe technique errors and provide feedback, internet videos, particularly for the older person, may be as inadequate as a two-dimensional brochure.
Device checklists, such as those used in this study,25 are readily available to assist clinicians and their patients. There may also be a place for family and friends to observe and provide feedback using the steps of the checklist, and this could be investigated in future studies. Addressing poor technique is important as this study has shown, but it may also help with issues of poor adherence, and we believe both issues need to be addressed in clinical practice.38 As discussed by Partridge,39 the responsibilities of the clinician need to extend beyond prescriptions to address meaningful self-management support and shared decision making. While the focus of this research has been on older people with asthma, similar issues in device technique have been observed in people with COPD and this learning can be similarly applied.40,41
Conclusions
Device technique can be improved and maintained in older people if inhaler education includes demonstration of technique and coaching is provided. It is through demonstration and device coaching that technique deficiencies can be exposed and the opportunity for correction or transition to an easier device can be made. Our results indicate that provision of passive written information alone, even in pictorial form, is not adequate as a form of inhaler education for older people with asthma.
References
Melani AS, Bonavia M, Cilenti V, Cinti C, Lodi M, Martucci P et al. Inhaler mishandling remains common in real life and is associated with reduced disease control. Respir Med 2011; 105: 930–938.
Melani AS, Zanchetta D, Barbato N, Sestini P, Cinti C, Aldo CP et al. Inhalation technique and variables associated with misuse of conventional metered-dose inhalers and newer dry powder inhalers in experienced adults. Ann Allergy Asthma Immunol 2004; 93: 439–446.
Haughney J, Price D, Barnes NC, Virchow JC, Roche N, Chrystyn H . Choosing inhaler devices for people with asthma: current knowledge and outstanding research needs. Respir Med 2010; 104: 1237–1245.
Cochrane MG, Bala MV, Downs KE, Mauskopf J, Ben-Joseph RH . Inhaled corticosteroids for asthma therapy: patient compliance, devices, and inhalation technique. Chest 2000; 117: 542–550.
Virchow JC, Crompton GK, Dal Negro R, Pedersen S, Magnan A, Seidenberg J et al. Importance of inhaler devices in the management of airway disease. Respir Med 2008; 102: 10–19.
Haughney J, Price D, Kaplan A, Chrystyn H, Horne R, May N et al. Achieving asthma control in practice: understanding the reasons for poor control. Respir Med 2008; 102: 1681–1693.
Brocklebank D, Ram F, Wright J, Barry P, Cates C, Davies L et al. Comparison of the effectiveness of inhaler devices in asthma and chronic obstructive airways disease: a systematic review of the literature. Health Technol Assess 2001; 5: 1–149.
Price D, Haughney J, Sims E, Ali M, von Ziegenweidt J, Hillyer E et al. Effectiveness of inhaler types for real-world asthma management: retrospective observational study using the GPRD. J Asthma Allergy 2011; 4: 37–47.
Broeders MEAC, Sanchis J, Levy ML, Crompton GK, Dekhuijzen PNR, Group AW . The ADMIT series–issues in inhalation therapy. 2. Improving technique and clinical effectiveness. Prim Care Respir J 2009; 18: 76–82.
Hardwell A, Barber V, Hargadon T, McKnight E, Holmes J, Levy ML . Technique training does not improve the ability of most patients to use pressurised metered-dose inhalers (pMDIs). Prim Care Respir J 2011; 20: 92–96.
Global Initiative for Asthma (GINA). Global Strategy for Asthma Management and Prevention (2010). Available from http://www.ginasthma.org.
Bosnic-Anticevich SZ, Sinha H, So S, Reddel HK . Metered-dose inhaler technique: the effect of two educational interventions delivered in community pharmacy over time. J Asthma 2010; 47: 251–256.
Basheti IA, Reddel HK, Armour CL, Bosnic-Anticevich SZ . Counseling about turbuhaler technique: needs assessment and effective strategies for community pharmacists. Respir Care 2005; 50: 617–623.
van Beerendonk I, Mesters I, Mudde AN, Tan TD . Assessment of the inhalation technique in outpatients with asthma or chronic obstructive pulmonary disease using a metered-dose inhaler or dry powder device. J Asthma 1998; 35: 273–279.
Chapman KR, Love L, Brubaker H . A comparison of breath-actuated and conventional metered-dose inhaler inhalation techniques in elderly subjects. Chest 1993; 104: 1332–1337.
Barua P, O’Mahony MS . Overcoming gaps in the management of asthma in older patients: new insights. Drugs Aging 2005; 22: 1029–1059.
Jones V, Fernandez C, Diggory P . A comparison of large volume spacer, breath-activated and dry powder inhalers in older people. Age Ageing 1999; 28: 481–484.
Ho SF, Omahony MS, Steward JA, Breay P, Burr ML . Inhaler technique in older people in the community. Age Ageing 2004; 33: 185–188.
Soriano JB, Visick GT, Muellerova H, Payvandi N, Hansell AL . Patterns of comorbidities in newly diagnosed COPD and asthma in primary care. Chest 2005; 128: 2099–2107.
McDonald VM, Gibson PG . Inhalation-device polypharmacy in asthma. Med J Aust 2005; 182: 250–251.
Armitage JM, Williams SJ . Inhaler technique in the elderly. Age Ageing 1988; 17: 275–278.
Abley C . Teaching elderly patients how to use inhalers. A study to evaluate an education programme on inhaler technique, for elderly patients. J Adv Nurs 1997; 25: 699–708.
Goeman DP, Jenkins C, Crane M, Paul E, Douglass J . Education intervention for older people with asthma: a randomised control trial. Patient Educ Couns 2013; 93: 586–595.
National Asthma Council Australia (ed.). Asthma Management Handbook. National Asthma Council Australia: South Melbourne, VIC, Australia, 2006.
National Asthma Council Australia. Inhaler Technique in Adults with Asthma or COPD. National Asthma Council Australia: Melbourne, VIC, Australia, 2008. http://www.nationalasthma.org.au/publication/inhaler-technique-in-adults-with-asthma-or-copd.
Brooks CM, Richards JM, Kohler CL, Soong SJ, Martin B, Windsor RA et al. Assessing adherence to asthma medication and inhaler regimens: a psychometric analysis of adult self-report scales. Med Care 1994; 32: 298–307.
Allen SC, Jain M, Ragab S, Malik N . Acquisition and short-term retention of inhaler techniques require intact executive function in elderly subjects. Age Ageing 2003; 32: 299–302.
Molimard M, Raherison C, Lignot S, Depont F, Abouelfath A, Moore N . Assessment of handling of inhaler devices in real life: an observational study in 3811 patients in primary care. J Aerosol Med 2003; 16: 249–254.
Ovchinikova L, Smith L, Bosnic-Anticevich S . Inhaler technique maintenance: gaining an understanding from the patient’s perspective. J Asthma 2011; 48: 616–624.
Hesselink AE, Penninx BW, Wijnhoven HA, Kriegsman DM, van Eijk JT . Determinants of an incorrect inhalation technique in patients with asthma or COPD. Scand J Prim Health Care 2001; 19: 255–260.
Lavorini F, Magnan A, Christophe Dubus J, Voshaar T, Corbetta L, Broeders M et al. Effect of incorrect use of dry powder inhalers on management of patients with asthma and COPD. Respir Med 2008; 102: 593–604.
Newman SP . Dry powder inhalers for optimal drug delivery. Expert Opin Biol Ther 2004; 4: 23–33.
Lavorini F, Fontana GA . Targeting drugs to the airways: The role of spacer devices. Expert Opin Drug Deliv 2009; 6: 91–102.
Connolly MJ . Inhaler technique of elderly patients: comparison of metered-dose inhalers and large volume spacer devices. Age Ageing 1995; 24: 190–192.
Levy M, Hardwell A, McKniht E, Holmes J . Asthma patients’ inability to use a pressurised metered-dose inhaler (pMDI) correctly correlates with poor asthma control as defined by the Global Initiative for Asthma (GINA) strategy: a retrospective analysis. Prim Care Respir J 2013; 22: 406–411.
Takemura M, Kobayashi M, Kimura K, Mitsui K, Masui H, Koyama M et al. Repeated instruction on inhalation technique improves adherence to the therapeutic regimen in asthma. J Asthma 2010; 47: 202–208.
Dekhuijzen PNR, Vincken W, Virchow JC, Roche N, Agusti A, Lavorini F et al. Prescription of inhalers in asthma and COPD: Towards a rational, rapid and effective approach. Respir Med 2013; 107: 1817–1821.
Pinnock H, Fletcher M, Holmes S, Keeley D, Leyshon J, Price D et al. Setting the standard for routine asthma consultations: a discussion of the aims, process and outcomes of reviewing people with asthma in primary care. Prim Care Respir J 2010; 19: 75–83.
Partridge MR . Self Management Education in Asthma and COPD: What does it involve and does it work? J Postgrad Med Inst 2012; 26: 07–12.
Lareau SC, Hodder R . Teaching inhaler use in chronic obstructive pulmonary disease patients. J Am Acad Nurse Pract 2012; 24: 113–120.
Yawn BP, Colice GL, Hodder R . Practical aspects of inhaler use in the management of chronic obstructive pulmonary disease in the primary care setting. Int J Chron Obstruct Pulmon Dis 2012; 7: 495–502.
Acknowledgements
This study was supported by the Co-operative Research Centre for Asthma and Airways.
Author information
Authors and Affiliations
Contributions
CRJ, JAD and DPG conceived the study. DPG and MAC undertook the data collection and provided the device education. MAC performed this analysis and prepared the manuscript. All authors have contributed to and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest. DPG is an Associate editor of npj Primary Care Respiratory Medicine, but was not involved in the editorial review of, nor the decision to publish, this article.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Crane, M., Jenkins, C., Goeman, D. et al. Inhaler device technique can be improved in older adults through tailored education: findings from a randomised controlled trial. npj Prim Care Resp Med 24, 14034 (2014). https://doi.org/10.1038/npjpcrm.2014.34
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/npjpcrm.2014.34
This article is cited by
-
Challenges in the Management of Asthma in Older Adults
Current Treatment Options in Allergy (2023)
-
Mobile device: a useful tool to teach inhaler devices to healthcare professionals
BMC Medical Education (2022)
-
Impact of repeated patient counseling using different pressurized metered-dose inhalers training devices on inhalation technique, lung function, and asthma control in adult asthmatics
Beni-Suef University Journal of Basic and Applied Sciences (2022)
-
Poor Inhaler Adherence and Techniques – How Can We Improve It?
Current Geriatrics Reports (2021)
-
The effects of repeated inhaler device handling education in COPD patients: a prospective cohort study
Scientific Reports (2020)