Abstract
Background:
Inodilators are routinely used in cardiovascular surgery with cardiopulmonary bypass (CPB). Information regarding safety and tolerability of the novel molecule, levosimendan (LEVO), in newborns is anecdotal; no pharmacokinetic data in this population are available.
Methods:
This was a phase I, randomized, and blinded study. Neonates undergoing surgical repair for congenital heart defects received stepwise dose increases of milrinone (MR; 0.5–1 μg/kg/min, n = 9) or LEVO (0.1–0.2 μg/kg/min, n = 11) as an i.v. continuous infusion, starting before CPB. Infants had continuous, time-locked, physiological, and near-infrared spectroscopy (NIRS) (cerebral and peripheral) recordings during the first 24 h, and at 48 and 96 h postsurgery. Serial biochemistry and pharmacokinetic studies were performed.
Results:
During the first 24 h postsurgery, patients showed time-related, group-independent increased cerebral tissue oxygenation and decreased diastolic blood pressure; in addition, group-dependent differences in heart rate and peripheral perfusion were found. Early postsurgery, MR-treated infants showed lower pH, higher glycemia, and higher inotrope score. The groups differed in cerebral NIRS-derived variables from 24 to 96 h. Study drug withdrawal at 96 h was more frequent with LEVO. LEVO intermediate metabolites were detected in plasma at day 14 after surgery.
Conclusion:
LEVO is well tolerated in critically ill neonates. LEVO may have advantages over MR in terms of the dosing regimen.
Similar content being viewed by others
Main
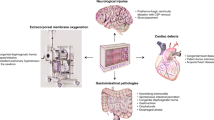
Surgical repair during the neonatal period is currently the standard approach for most cardiac malformations. Despite the milestones reached, newborns undergoing cardiovascular surgery have a high morbidity and neuropsychological sequelae that may diminish their quality of life (1). The vulnerability of the newborn to developing surgery-related low cardiac output syndrome could be one of the reasons for this unfavorable outcome. This condition, typically present 6–18 h after surgery, involves a combination of low myocardial contractility and the peripheral effects of ischemia–reperfusion on the endothelium and results in decreased heart rate, heightened pulmonary and systemic vascular resistance, and positive water balance (2,3,4). Therefore, in addition to catecholamines, the early use of inodilators (INDs) is proposed to reduce afterload and increase inotropism.
Milrinone (MR) is a selective phosphodiesterase III inhibitor that has inotropic and lusitropic effects on the myocardium. It also has a relaxing effect on the vascular muscle. MR improves mesenteric perfusion and attenuates myocardial oxydative stress following hypoxia–reoxygenation in piglets (5). Studies in pediatric populations appear to support the clinical usefulness of MR, which is similar to that observed in adults (6,7,8,9,10,11).
Levosimendan (LEVO) is a novel class IND developed for the treatment of heart failure (12,13,14,15,16,17). LEVO binds to troponin C, which, in turn, enhances the sensitivity of contractile proteins to calcium. LEVO has a positive lusitropic effect (12,13) and induces vascular relaxation in the smooth muscle of the peripheral and coronary vascular bed (14,15,16,17). The direct anti-inflammatory and antiapoptotic cardioprotective actions of LEVO have also been reported (12). LEVO can be used with conventional inotropic agents. One of the potential advantages of LEVO is related to its pharmacokinetic profile. The biotransformation of LEVO in the intestinal tract gives rise to intermediate metabolites (OR1855 and OR1896) with beneficial hemodynamic effects that last up to 7 d after discontinuing the drug in adults (16). However, experience with LEVO in pediatric patients is scarce (18,19,20,21,22,23), and the number of neonates in these studies is anecdotal (18,19,20,21,22,23). There are no data on LEVO pharmacokinetics in neonates.
The purpose of this study was to systematically test the efficacy and safety of MR and LEVO in newborns undergoing cardiovascular surgery with cardiopulmonary bypass (CPB). We introduce a key variant as compared with previous studies (7): the perioperative administration of the study drug, MR or LEVO. Given the uncertainty about LEVO pharmacokinetics in neonates, the study was designed as a pilot, phase I feasibility study.
Results
Study Population
Between November 2009 and November 2010, 20 neonates undergoing cardiovascular surgery with CPB who were in stable preoperative hemodynamic condition were enrolled, representing 69% of potential candidates for study. The remaining 9 infants (31%) were not included due to emergency surgery, IND contraindication, or refused consent. The clinical characteristics of the patients are described in Table 1 . IND11 carried a 22q11 deletion and IND15 had Goldenhar syndrome. The study period ran from the immediate preoperative (baseline) day to postoperative day 6. The predefined study time points were baseline, first 24 h (T1), 48 h (T2), 96 h (T3), and day 6 postsurgery.
The study groups did not differ with respect to gender, gestational age, postnatal age at surgery, risk adjustment using the congenital heart surgery method (24), duration of aortic cross-clamping, or CPB. However, their weights were significantly different at the time of surgery (3,278 (SD: 410) g LEVO; 2,875 (SD: 403) g MR; P < 0.02). On study entry, eight infants were receiving ventilatory support (four by nasal continuous positive air pressure and four by conventional mechanical ventilation) and were equally distributed between the groups. In addition, one MR patient was on dopamine (5 μg/kg/min) and urapidil (0.8 mg/kg/h) treatment. Baseline cardiac function according to the echocardiography is shown in Table 2 .
Study Procedures and Other Interventions
The mean time from the end of CPB to dose 2, the duration of dose 2, and the time to reach dose 3 from the initial IND infusion did not differ between the groups. Two infants in each group received the second study drug once the study was opened. However, at 96 h postsurgery, 91% of the infants on LEVO and 37.5% on MR had already been withdrawn from INDs (P = 0.041). No differences were found between groups with respect to the need for or duration of other vasodilators throughout the study period.
One infant (IND8) had only a partial follow-up in the study outcomes due to early death. Another infant (IND18) required extracorporeal membrane oxygenation for 62 h beginning soon after surgery. Two patients (IND2 and IND12) had permanent pacemakers inserted due to surgery-related third-degree atriventricular blocks. One infant (IND11), who showed atrioventricular asynchrony at 48 h postsurgery, was recaptured with a pacemaker. The groups did not differ with respect to ventilatory support, use of sedatives, or renal function (serum creatinine and urine output) during the 6-d postsurgery follow-up, or mortality. Six patients showed abnormal postatrioseptostomy or postsurgical cranial ultrasound findings with (IND2, IND11, and IND12) or without (IND9, IND15, and IND16) an amplitude-integrated electroencephalography correlation.
Evolution of Physiological Variables
A time-related treatment effect on heart rate was observed during T1, heart rate being higher in the MR than in the LEVO group ( Figure 1a ). In addition, a significant effect of time on diastolic blood pressure was found that was independent of the intervention type ( Figure 1b ).
Evolution of the continuous physiological and NIRS variables in the milrinone (black line) and levosimendan (gray line) study groups throughout the first 24 h postsurgery (expressed in min). Mixed linear models show (mean, SEM) (a) a time-related treatment effect on heart rate (beats per min) (P = 0.0213); (b) a time-related, group-independent effect on diastolic blood pressure (mm Hg) (P = 0.0098); (c) a time-dependent increase in the cerebral tissue oxygenation index (%; P = 0.0439); and (d) cerebral intravascular oxygenation (μmol/l; P = 0.0177); (e) a time-dependent decrease in cerebral fractional oxygen extraction (%; P = 0.0311); and (f) group-dependent differences in peripheral intravascular oxygenation (μmol/l; P = 0.0195). NIRS, near infrared spectroscopy.
No significant differences were observed in the rate–pressure index (heart rate × systolic blood pressure) (23), which showed decreasing trends with time in T1.
Group-dependent differences in the central-to-peripheral temperature gradient were significant during T1 (LEVO −0.42 (SD: 0.32) °C; MR 4.7 (SD: 0.24) °C; P = 0.021).
Finally, nonclinically relevant differences in arterial oxygen saturation (SaO2) were found between the groups during T1 (LEVO 93.4 (SD: 0.15); MR 93.1 (SD: 0.24); P < 0.0001) and at T2 (LEVO 92.8 (SD: 0.44); MR 92.7 (SD: 0.87); P = 0.038) time points.
Evolution of NIRS-Derived Variables
Time-dependent increases in the cerebral tissue oxygenation index (cTOI) ( Figure 1c ) and cerebral intravascular oxygenation ( Figure 1d ) and decreased cerebral fractional oxygen extraction ( Figure 1e ) were found in the first 24 h, which were independent of group allocation. At a peripheral level, infants receiving LEVO showed higher peripheral intravascular oxygenation ( Figure 1f ) than those receiving MR during T1, with no differences in peripheral fractional oxygen extraction. No other significant effects were evident in any of the NIRS-derived variables at the T2 and T3 monitoring periods.
The average mean values for absolute NIRS-derived variables at the T1, T2, and T3 monitoring periods were used for group comparisons across the study. The groups showed different profiles in both the cTOI (P = 0.0003) ( Figure 2a ) and cerebral fractional oxygen extraction (P = 0.002) ( Figure 2b ) patterns with time.
The lines represent the average mean value (left y-axis) of (a) the cerebral tissue oxygenation index (%) and (b) the fractional oxygen extraction (%) in the milrinone (dashed line) and levosimendan (gray line) study groups. Bars (right y-axis) show the number of patients still receiving INDs at the various time points (T1, first 24 h; T2, at 48 h; T3, at 96 h after surgery) in the milrinone (white bar) and levosimendan (gray bar) study groups. IND, inodilator.
Other Outcomes
Infants receiving MR showed a lower pH early on (although within the normal upper range) ( Figure 3a ) and higher blood glucose and inotrope scores ( Figure 3c,d ). Trends toward higher Pco2 and lactate serum levels ( Figure 3b ) were also found in these infants. No differences in mixed venous saturation or other biochemical parameters were found.
Evolution of (a) pH, (b) lactate (mmol/l), (c) glycemia (mg/dl), and (d) inotrope score (3) in the milrinone (dashed line) and levosimendan (gray line) study groups from baseline (BL) immediately presurgery, throughout the first 96 h after surgery. *P < 0.05; **P = 0.075.
Serial echocardiography did not reveal any differences between the groups ( Table 2 ). The tricuspid annular plane systolic excursion data showed normal baseline values (n = 7); however, the overall results of the studies conducted at T1 (n = 10), T2 (n = 9), and T3 (n = 9) were abnormal. On day 6 postsurgery, three of the nine infants assessed still showed abnormal tricuspid annular plane systolic excursion values. N-terminal probrain natriuretic peptide and troponine I serum levels from baseline to the end of the study did not differ between the groups ( Table 2 ).
Proinflammatory interleukin (IL)6 (P = 0.049) and IL8 (P = 0.004) increased and anti-inflammatory IL7 (P = 0.001) decreased with time, with no differences between the groups. The evolution of the pro- and anti-inflammatory variables was not associated with the duration of CPB or lactate serum levels at neonatal intensive care unit (NICU) admission.
The kinetic parameters and plasma concentrations of the study INDs are shown in Table 3 and Figure 4 , respectively. LEVO metabolite concentrations were within the limit of determination up to day 14 postsurgery ( Figure 4a ). Overall MR plasma concentrations were at or above the therapeutic range (300 ng/ml) (8) beyond 10 h of drug infusion ( Figure 4b ).
Indicators of plasma concentration. (a) Median (dots) and IQR (vertical whiskers) of levosimendan (gray circles, solid line) and metabolites OR1855 (white circles, solid line) and OR1896 (gray circles, dashed line) plasma concentrations in relation to time. (b) Median (gray circles, solid line) and IQR (vertical whiskers) of milrinone plasma concentration in relation to time. Milrinone elimination phase is marked by an arrow. The horizontal whiskers indicate the IQR time when blood samples were obtained, representing differences in milrinone withdrawal. IQR, interquartile range.
Discussion
The management of heart failure at the neonatal age is based on clinical guidelines derived from anecdotal experience in children and reports on adults.This study offers new data on the hemodynamic effects of a routinely used drug, MR, and a novel molecule, LEVO, currently being used compassionately for pediatric-age patients.
This is the first study to report pharmacokinetic data on MR and LEVO for the neonatal and other pediatric populations in which no loading dose was delivered for either drug. In addition, this study provides the first pharmacokinetic data on the metabolites OR1855 and OR1896 in neonates and children receiving LEVO. This information, derived from the systematized study of LEVO, is of particular interest given that the pharmacokinetic profile indicates that the drug generates a long-lasting active metabolite, which makes it highly attractive for clinical use.
Little pharmacokinetic data are available for the neonatal population undergoing specific surgical procedures. In children, weight-normalized MR elimination clearance can be expressed as a linear function of age (9). Information on neonates is scarce, and the application of procedures such as CPB or modified ultrafiltration can affect IND pharmacokinetics (10). With regard to LEVO, only one study has assessed the pharmacokinetics of the drug (given as a 12 μg/kg i.v. bolus) in children undergoing cardiac catheterization (18); neonates were not included in this series. Metabolite concentrations were under the limit of determination in all samples. Pharmacokinetic studies in adults showed stationary equilibrium at 4–8 h following continuous infusion (0.05–0.2 μg/kg/min) that remained constant thereafter for as long as the infusion was maintained (14). To avoid undesirable effects, particularly systemic hypotension, we administered the study drug without a loading dose. However, the infusion of IND in this study began earlier than in other trials (7,23). It is noteworthy that early in the postoperative course, MR-treated infants showed MR plasma concentrations within the therapeutic range (8). In the case of LEVO-treated infants, the median plasma concentrations of the parent drug and OR1896 were, 10 h after infusion of IND started, within the range that showed positive hemodynamic effects in adults with heart failure (14) and in healthy male volunteers (15), respectively. Therefore, the time of IND infusion initiation may be relevant to the efficacy of INDs in the prevention of low cardiac output syndrome, particularly in the case of LEVO, in which pre- and postconditioning properties suggest cardioprotective mechanisms in both animal and human studies (12).
INDs were well tolerated in our patients, given that only one infant failed to complete the study protocol due to death. The mean time to the corresponding step-increase in IND dose did not differ between the groups. Overall, the two groups were comparable with respect to the main neonatal clinical morbidities and mortality.
Neither MR nor LEVO appear to increase myocardial oxygen demand, according to the trends observed in the rate–pressure index in this study (23). During the first 24 h postsurgery, MR had a greater effect on heart rate (increase) than LEVO, which is in accordance with the data reported in a predominantly pediatric population (23). However, diastolic blood pressure showed a time-related, group-independent decreasing profile. Infants in the MR group showed significantly lower SaO2 and pH and trends toward higher Pco2, which possibly indicates differences in respiratory status. These infants also had higher lactate and glucose serum levels, and more need for other inotropes than infants on LEVO during the first hours postsurgery. However, both pH and lactate remained within an adequate range regardless of the intervention.
Cerebral NIRS-derived variables suggested a time-dependent improvement in blood flow (increased cerebral intravascular oxygenation) and oxygen availability (increased cTOI and decreased cerebral fractional oxygen extraction) in both groups in the first 24 h postsurgery. Beyond that time point, the groups differed with respect to cTOI and cerebral fractional oxygen extraction profiles in the first 96 h after surgery ( Figure 2 ), which coincided with significant differences in IND withdrawal. However, the differences found in cerebral perfusion and oxygen transport do not seem to be clinically relevant given that the critical regional oxygen saturation potential for brain injury has been established at ~45% (25).
At the peripheral level, infants on LEVO showed a significantly higher peripheral intravascular oxygenation than infants on MR. In addition, infants receiving LEVO showed a lower temperature gap. LEVO improves hemodynamic performance by dilation of coronary and resistance vessels. Phosphodiesterase III inhibition (a common pathway for both study INDs and one of the mechanisms proposed to explain this effect) does not seem to be the main determinant (12). The role of other LEVO-specific properties in peripheral vasodilation, such as the regulation of the opening of potassium channels or the desensitization to calcium by vascular smooth muscle cell contractile proteins remains to be defined. Whether these findings and the differences found in the temperature gap represent real differences in the effect on the peripheral perfusion of the study INDs needs to be addressed by appropriately designed studies.
The reduced number of data, related to the infants’ abnormal cardiac performance and confirmed by serial echocardiographic scans, precluded exploring any eventual relationship between echocardiography and N-terminal probrain natriuretic peptide or troponine I data.
The results of this study point toward a hemodynamic effect of LEVO that persists after the drug infusion ends. Although the percentage of infants receiving the second study drug was comparable during the open study, the successful withdrawal of the study INDs occurred significantly earlier in the LEVO-treated infants than in those treated with MR. The pharmacokinetic particularities of LEVO may explain its sustained effect. This notion is supported by the fact that MR plasma concentrations were at or above the target range (8) while the infusion drug persisted but had a rapid elimination phase once the infusion stopped ( Figure 4b ). As previously shown in healthy adult volunteers and patients with heart failure (14,15), the parent drug disappeared rapidly once the LEVO infusion was halted at 48 h ( Figure 4a ). The plasma concentration of the active metabolite OR1896 peaked at 36 h. As with adults (14), the active metabolite is detectable in plasma ~10 h after the initiation of the LEVO infusion, with the median OR1896 plasma concentration above 2 ng/ml. This result is in accordance with a report that showed the prolonged beneficial hemodynamic effects of LEVO on congestive heart failure after the infusion was stopped (14). The concentration of OR1896 remained stable in plasma up to day 8 and was still measurable up to 12 d after withdrawal of LEVO. Of note, the first derivative in LEVO’s metabolic pathway (OR1855), which serves as an intermediate metabolite in the conversion of LEVO to the N-acetylated conjugate active metabolite (OR1896) was formed slowly, and the plasma peak concentration was observed ~7 d after the start of the infusion. This fact may indicate an early biotransformation of the parent drug in the intestinal tract by reduction to OR1855 and a fast acetylation process causing higher concentrations of OR1896 than OR1855. The delayed deacetylation of OR1896 may explain the progressive accumulation of OR1855 (14,15). The acetylation capacity of an individual has a marked effect on the plasma levels and exposure to both metabolites. Individual differences in the acetylation activity related to the enzyme polymorphism would explain the wide interquartile range in OR1855 plasma concentrations found in this study.
A limitation of this study was that titration of the study INDs was not targeted against a clinical outcome; consequently, the titration may not have been optimized, which may have influenced the clinical responsiveness and side effects. However, the doses used encompass those used in previous reports (7) and our overall clinical experience with MR and LEVO (22). In addition, this is an exploratory, unpowered trial. Therefore, regardless of the difficulties related to this kind of study, which was performed in critically ill infants undergoing complex procedures in which a multidisciplinary team is involved, these results warrant the further study of MR as compared with LEVO in larger phase II and phase III confirmatory trials.
In summary, this pilot study describes the pharmacokinetic profile of MR and LEVO given in a continuous i.v. infusion without a loading dose in newborn infants undergoing CPB. The study provides reassuring data on the early intraoperative use of both INDs and points toward the persistent hemodynamic effects of LEVO after the conclusion of the drug infusion. These effects are partly related to the particularities of the biotransformation of LEVO into long-lasting active metabolites, which, in this study, were documented in plasma up to 12 d after drug withdrawal. This fact has practical benefits given that it reduces the time required for intravenous lines and NICU stays. Therefore, the results of this pilot trial offer relevant data that support the use of LEVO as a potential first-line IND for use in neonates; these results should be addressed in appropriate confirmatory trials.
Methods
This pilot, phase I randomized, blind clinical trial was conducted at the La Paz University Hospital in Madrid. The study protocol was approved by the Ethics Committee for Human Studies at the La Paz University Hospital of Madrid (Spain) and the Spanish Medicines Agency at the National Ministry of Health (European Union Drug Regulating Authorities Clinical Trials-EurodraCT 2009-01404-28). When admitting potential candidates, the medical suitability of patients was confirmed by the physician responsible for their clinical care. Parents were offered the opportunity to enroll their infants in the study through informed consent by members of the study team who were on the delegation log for consent (A.P., P.L.-O., and M.C.B.).
Intervention
Infants were randomized immediately before surgery to receive MR (milrinone lactate 1 mg/ml; Primacor, Sanofi-Aventis S.A., México City, Mexico) or LEVO (LEVO 2.5 mg/ml; Simdax, Orion Pharma, Espoo, Finland). Continuous intravenous infusion of the study drug through a separate central line was started intraoperatively and was increased stepwise: dose 1, starting immediately after the central lines were placed and maintained for the duration of the surgical procedure; dose 2, upon NICU admission, providing the infant was in stable hemodynamic condition; and dose 3, starting after 2 h of stability with dose 2, and maintained up to 48 h after the infusion of IND started. Accordingly, infants randomized to the MR group received 0.5, 0.75, and 1 μg/kg/min and those infants randomized to the LEVO group received 0.1, 0.15, and 0.2 μg/kg/min, for doses 1, 2, and 3, respectively.
The potentially undesirable side effects related to either IND studied were a >30% change in heart rate or a 35–40% decrease in systolic blood pressure as compared with baseline. If these conditions ocurred, the IND dose was interrupted for 30–60 min and resumed at half the previous infusion rate once the patient had recovered. The withdrawal criteria were (i) persistent arterial hypotension, with or without variations in heart rate, after discontinuation of IND infusion and (ii) systemic hypotension recurring on IND reintroduction.
Intravenous solutions of the study INDs were prepared in identical opaque syringes, and the concentration was adjusted to deliver the corresponding dose for each IND at the same infusion rate. Infusion tubes were covered by aluminium foil to avoid unmasking LEVO due to its yellow color. A study nurse who was not involved in the clinical care of the infants prepared the study medication and was the custodian of the allocation code.
The duration of treatment differed according to the IND based on a priori pharmacokinetic data (14,15,16). Per protocol, the infusion of LEVO was stopped 48 h after it was started. From 48 h onward, the MR infusion rate was tapered according to the crietria specified by the attending physician. Therefore, beyond 48 h this was an open study.
Other Interventions
The overall patient pre- and postoperative management followed the cardiovascular surgery treatment guidelines currently in place at the NICU. Hemodynamic stability was achieved first by adjusting the dose of other cardiovascular drugs in order to maintain the study drug infusion rate as stable as possible according to protocol. The aim was to maintain mean blood pressure above 40 mm Hg and reduce the afterload, for both the systemic and pulmonary circulation. A constellation of clinical, biochemical, and/or echocardiography-derived data guided the interventions, such as the need for volume expansion and the use of other cardiovascular drugs. Therefore, in addition to the study INDs, pressor-inotrope agents (dopamine and epinephrine), inotropes (dobutamine), and systemic (urapidil, sodium nitroprusside, and nitroglycerin) and pulmonary (nitric oxide) vasodilators were used when clinically indicated. As part of the routine management, all infants received three doses of methylprednisolone, 8 h apart, starting the night before surgery.
Primary Outcome Measures
Patients were monitored continuously for heart rate, breathing rate, central (axilla) and peripheral (foot) temperature, intravascular arterial blood pressure, and SaO2 (IntelliVue MP50, Phillips, Best, The Netherlands).
Changes in cerebral and peripheral perfusion–oxygenation were assessed using the NIRS instrument NIRO-300 (Hamamatsu Photonics, Fukuoka, Japan), equipped with two measuring units. The sensor from one of the measuring units was placed at the frontal–parietal level (cNIRS). The following cNIRS trend variables were obtained from the monitor: changes in oxyhemoglobin, deoxyhemoglobin, total hemoglobin, and cTOI. The cerebral intravascular oxygenation (equivalent to the difference between oxyhemoglobin and deoxyhemoglobin and used as a surrogate of cerebral blood flow changes) (26) and changes in total hemoglobin (used to estimate changes in cerebral blood volume) (27,28) were calculated offline. The cTOI was used as a continuous estimate of the cerebral venous oxygen saturation (29). The second measuring unit was used to assess changes in peripheral perfusion–oxygenation (pNIRS) by placing the optodes on a thigh. Changes in peripheral intravascular oxygenation and peripheral TOI were continuously derived (22). The emitter and receptor optodes were spaced 4 cm apart. The same path length factor of 4 (28) was used for the cerebral and peripheral circulation. The NIRS sampling time was 0.5 s.
At NICU admission, recordings of the physiological and NIRS-derived variables began immediately after surgery and continued throughout the first day (T1). The recordings were then restarted and maintained for at least 4 h at 48 and 96 h postsurgery (T2 and T3 study time points, respectively). A real-time, simultaneous, time-locked data acquisition system for NIRS and physiological variables was developed. After a period of stabilization, the baseline oxyhemoglobin, deoxyhemoglobin, and total hemoglobin were related to an arbitrary zero. Baseline TOI was defined as the value at the beginning of each study for both cTOI and peripheral TOI once the NIRS signal was considered stable. The fractional oxygen extraction, which represents the ratio of tissue oxygen consumption to tissue oxygen delivery (27), was calculated offline as (SaO2–TOI)/SaO2. We calculated the average values for all samples of the continuous NIRS and physiological variable recordings obtained during 5-min intervals, every 30 min (Matlab, MathWorks, Natick, MA), which were then used for analyses. SaO2 variation did not exceed 1% within the measurement time point.
Other Outcome Measures
Blood gases, acid–base status, co-oximetry, and lactate, glucose, and hemoglobin concentration readings were serially assessed at baseline (immediately before CPB) and every 6 h at T1 and once during NIRS monitoring at T2 andT3. Serum creatinine, N-terminal probrain natriuretic peptide, troponine I, and proinflammatory and anti-inflammatory factors (IL-β1, IL6, IL7, IL8, IL10, and tumor necrosis factor-α) were determined at baseline, at T2, and on day 6 postsurgery.
The steady-state IND plasma concentrations were measured immediately before CPB while on IND dose 1; 2 h after the start of the IND dose 2; and 24 and 48 h after the start of the infusion of IND in infants receiving IND dose 3. Beyond that period (open study), daily samples were obtained for LEVO up to day 7 postsurgery and at 10 and 14 d. In those infants randomized to MR, daily samples were obtained while the infants continued to receive the IND. Additional samples were taken once MR was stopped so as to study the elimination phase.
Blood samples were immediately centrifuged and plasma was stored at −20 ºC. LEVO and MR analyses were conducted using high-performance liquid chromatography and tandem mass spectrometry. The lower limits of quantification were set as follows: LEVO, 0.2 ng/ml; OR1855, 0.199 ng/ml; OR1896, 0.202 ng/ml; and MR, 2 ng/ml. The pharmacokinetic parameters of MR, LEVO, and metabolites were derived using noncompartmental methods (Phoenix WinNonlin 6.2.1, Pharsight Corporation, Cary, NC).
Serial echocardiography (Siemens Acuson X300, Siemens, Munich, Germany; 4–8 MHz probe) and cranial ultrasound (Toshiba Nemio XG, Tokyo, Japan; 5–12 MHz probe) studies were performed at baseline, T1, T2, T3, and on day 6 postsurgery. Parasternal, apical, subcostal, and suprasternal long and short axis views were used. A complete anatomical (surgical repair, residual lesions, or pericardial effusions) and functional (shortening/ejection fraction and preload status) evaluation was performed according to a standardized technique (30). Tricuspid annular plane systolic excursion was measured in a subset of patients to assess right-ventricular systolic function (31). Reported normative values in neonates are within 6.6 and 14.5 mm (31). The various cranial ultrasound diagnoses were classified according to a previously reported grading system (32). All infants had continuous amplitude-integrated electroencephalography monitoring (Olympic CFM 6000 (Olympic Medical, Port Angeles, WA) or Brainz (Natus Pediatrics, Mill Bay, BC, Canada)) while undergoing invasive procedures or during hemodynamic instability. The inotrope score was calculated according to Wernovsky et al. (3) for all the study time points.
Data Analysis
Data were analyzed using the statistical software SAS 9.1.3 (Cary, NC). Quantitative data are given as means (±SD) or median (interquartile range) and qualitative data as counts and percentages. The Mann–Whitney U test was used to compare quantitative variables for the study time points. The Pearson’s correlation coefficient was used to explore correlations between continuous variables. Mixed linear models were used to explore changes over time in physiological and NIRS-derived variables that were continuously recorded during T1, T2, and T3 to control for repeated unbalanced measures. An autoregressive or heterogeneous autoregressive variance–covariance matrix structure with components–variances was assumed in the mixed linear model. The mean values and SEM associated with the main effect of the group are reported. To analyze any changes (evolution) in these parameters over the three study times between the two groups, a two-way analysis of variance for two factors (time and group) was performed, with repeated measurements of one of these factors (time). The main effects and the interaction effects between the two factors were studied (a significant interaction effect would indicate a difference in the evolution profile). Post hoc comparisons were made using the Bonferroni method, adjusting for confounders, as appropriate. The qualitative clinical-evolution parameters between the two groups were compared using Fisher’s exact test. All statistical analyses were considered bilateral and values of P < 0.05 were considered significant.
This early-stage, exploratory study was not powered for any statistical objective. The randomization of patients was stratified by type of congenital heart defect and risk adjustment using the congenital heart surgery method (24). According to the a priori expected prevalence, the proportion of patients in each stratum was established as 20% in low-risk, 60% in moderate–low risk, and 20% in moderate–high risk. The Proc Plan of SAS 9.1.3 was used to generate the randomization list. The primary analysis of the results of this study was performed according to the intention-to-treat principle.
Statement of Financial Support
A.P. acknowledges the financial support of the Spanish Fondo de Investigación Sanitaria (Spanish Healthcare Research Fund), grant EC08/00206, and the SAMID network (RD08/0072/0018), as well as the Orion Pharma Spanish Division, for the pharmacokinetic studies.
Disclosure
The authors declared no conflict of interest.
References
Donofrio MT . Impact of congenital heart disease and surgical intervention on neurodevelopment. In: Kleinman CS, Seri I, eds. Hemodynamics and Cardiology: Neonatology Questions and Controversies. Philadelphia, PA: Saunders, 2008:275–96.
Burrows FA, Williams WG, Teoh KH, et al. Myocardial performance after repair of congenital cardiac defects in infants and children. Response to volume loading. J Thorac Cardiovasc Surg 1988;96:548–56.
Wernovsky G, Wypij D, Jonas RA, et al. Postoperative course and hemodynamic profile after the arterial switch operation in neonates and infants. A comparison of low-flow cardiopulmonary bypass and circulatory arrest. Circulation 1995;92:2226–35.
Asimakopoulos G, Taylor KM . Effects of cardiopulmonary bypass on leukocyte and endothelial adhesion molecules. Ann Thorac Surg 1998;66:2135–44.
Chang AC, Atz AM, Wernovsky G, Burke RP, Wessel DL . Milrinone: systemic and pulmonary hemodynamic effects in neonates after cardiac surgery. Crit Care Med 1995;23:1907–14.
Manouchehri N, Bigam DL, Churchill T, Joynt C, Vento M, Cheung PY . Milrinone is preferred to levosimendan for mesenteric perfusion in hypoxia-reoxygenated newborn piglets treated with dopamine. Pediatr Res 2012;71:241–6.
Hoffman TM, Wernovsky G, Atz AM, et al. Efficacy and safety of milrinone in preventing low cardiac output syndrome in infants and children after corrective surgery for congenital heart disease. Circulation 2003;107:996–1002.
Bailey JM, Miller BE, Lu W, Tosone SR, Kanter KR, Tam VK . The pharmacokinetics of milrinone in pediatric patients after cardiac surgery. Anesthesiology 1999;90:1012–8.
Bailey JM, Hoffman TM, Wessel DL, et al. A population pharmacokinetic analysis of milrinone in pediatric patients after cardiac surgery. J Pharmacokinet Pharmacodyn 2004;31:43–59.
Zuppa AF, Nicolson SC, Adamson PC, et al. Population pharmacokinetics of milrinone in neonates with hypoplastic left heart syndrome undergoing stage I reconstruction. Anesth Analg 2006;102:1062–9.
McNamara PJ, Laique F, Muang-In S, Whyte HE . Milrinone improves oxygenation in neonates with severe persistent pulmonary hypertension of the newborn. J Crit Care 2006;21:217–22.
Antoniades C, Antonopoulos AS, Tousoulis D, Bakogiannis C, Stefanadi E, Stefanadis C . Relationship between the pharmacokinetics of levosimendan and its effects on cardiovascular system. Curr Drug Metab 2009;10:95–103.
Haikala H, Nissinen E, Etemadzadeh E, Levijoki J, Lindén IB . Troponin C-mediated calcium sensitization induced by levosimendan does not impair relaxation. J Cardiovasc Pharmacol 1995;25:794–801.
Antila S, Sundberg S, Lehtonen LA . Clinical pharmacology of levosimendan. Clin Pharmacokinet 2007;46:535–52.
Puttonen J, Laine T, Ramela M, et al. Pharmacokinetics and excretion balance of OR-1896, a pharmacologically active metabolite of levosimendan, in healthy men. Eur J Pharm Sci 2007;32:271–7.
Kivikko M, Lehtonen L, Colucci WS . Sustained hemodynamic effects of intravenous levosimendan. Circulation 2003;107:81–6.
Follath F, Cleland JG, Just H, et al. Efficacy and safety of intravenous levosimendan compared with dobutamine in severe low-output heart failure (the LIDO study): a randomised double-blind trial. Lancet 2002;360:196–202.
Turanlahti M, Boldt T, Palkama T, Antila S, Lehtonen L, Pesonen E . Pharmacokinetics of levosimendan in pediatric patients evaluated for cardiac surgery. Pediatr Crit Care Med 2004;5:457–62.
Namachivayam P, Crossland DS, Butt WW, Shekerdemian LS . Early experience with Levosimendan in children with ventricular dysfunction. Pediatr Crit Care Med 2006;7:445–8.
Egan JR, Clarke AJ, Williams S, et al. Levosimendan for low cardiac output: a pediatric experience. J Intensive Care Med 2006;21:183–7.
Di Chiara L, Ricci Z, Garisto C, et al. Initial experience with levosimendan infusion for preoperative management of hypoplastic left heart syndrome. Pediatr Cardiol 2010;31:166–7.
Bravo MC, Bravo Mdel C, López P, et al. Acute effects of levosimendan on cerebral and systemic perfusion and oxygenation in newborns: an observational study. Neonatology 2011;99:217–23.
Momeni M, Rubay J, Matta A, et al. Levosimendan in congenital cardiac surgery: a randomized, double-blind clinical trial. J Cardiothorac Vasc Anesth 2011;25:419–24.
Jenkins KJ, Gauvreau K, Newburger JW, Spray TL, Moller JH, Iezzoni LI . Consensus-based method for risk adjustment for surgery for congenital heart disease. J Thorac Cardiovasc Surg 2002;123:110–8.
Dent CL, Spaeth JP, Jones BV, et al. Brain magnetic resonance imaging abnormalities after the Norwood procedure using regional cerebral perfusion. J Thorac Cardiovasc Surg 2005;130:1523–30.
Tsuji M, duPlessis A, Taylor G, Crocker R, Volpe JJ . Near infrared spectroscopy detects cerebral ischemia during hypotension in piglets. Pediatr Res 1998;44:591–5.
Pellicer A, Bravo Mdel C . Near-infrared spectroscopy: a methodology-focused review. Semin Fetal Neonatal Med 2011;16:42–9.
Wyatt JS, Cope M, Delpy DT, et al. Quantitation of cerebral blood volume in newborn human infants by near infrared spectroscopy. J Applied Physiol 1990;68:1086–91.
Nagdyman N, Fleck T, Schubert S, et al. Comparison between cerebral tissue oxygenation index measured by near-infrared spectroscopy and venous jugular bulb saturation in children. Intensive Care Med 2005;31:846–50.
Evans N . Functional echocardiography in the neonatal intensive care unit. In: Kleinman CS, Seri I, eds. Hemodynamics and Cardiology: Neonatology Questions and Controversies. Philadelphia, PA: Saunders, 2008:83–109.
Núñez-Gil IJ, Rubio MD, Cartón AJ, et al. Determination of normalized values of the tricuspid annular plane systolic excursion (TAPSE) in 405 Spanish children and adolescents. Rev Esp Cardiol 2011;64:674–80.
Pellicer A, Valverde E, Elorza MD, et al. Cardiovascular support for low birth weight infants and cerebral haemodynamics: a randomized, blinded, clinical trial. Pediatrics 2005;115:1501–12.
Acknowledgements
This study has been registered at EudraCT: 2009-010404-28 and Clinicaltrials.gov: NCT01576094. This study was presented in part at the European Society for Paediatric Research, 2011 annual meeting. The first author, who wrote the first draft, has not received an honorarium to produce the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pellicer, A., Riera, J., Lopez-Ortego, P. et al. Phase 1 study of two inodilators in neonates undergoing cardiovascular surgery. Pediatr Res 73, 95–103 (2013). https://doi.org/10.1038/pr.2012.154
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2012.154
This article is cited by
-
Population Pharmacokinetics of Levosimendan and its Metabolites in Critically Ill Neonates and Children Supported or Not by Extracorporeal Membrane Oxygenation
Clinical Pharmacokinetics (2023)
-
Reassessing the role of milrinone in the treatment of heart failure and pulmonary hypertension in neonates and children: a systematic review and meta-analysis
European Journal of Pediatrics (2023)
-
Near-infrared spectroscopy for perioperative assessment and neonatal interventions
Pediatric Research (2021)
-
Initial Observations of the Effects of Calcium Chloride Infusions in Pediatric Patients with Low Cardiac Output
Pediatric Cardiology (2016)
-
Management of Shock in Neonates
The Indian Journal of Pediatrics (2015)