Abstract
Background
Whether short sleep duration or high sleep variability may predict less weight loss and reduction in measures of adiposity in response to lifestyle interventions is unknown. The aim of this study was to compare the 12-month changes in weight and adiposity measures between those participants with short or adequate sleep duration and those with low or high sleep variability (intra-subject standard deviation of the sleep duration) in PREvención con DIeta MEDiterránea (PREDIMED)-Plus, a primary prevention trial based on lifestyle intervention programs.
Methods
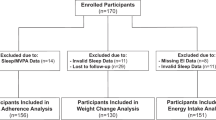
Prospective analysis of 1986 community-dwelling subjects (mean age 65 years, 47% females) with overweight/obesity and metabolic syndrome from the PREDIMED-Plus trial was conducted. Accelerometry-derived sleep duration and sleep variability and changes in average weight, body mass index (BMI), and waist circumference (WC) attained after 12-month interventions were analyzed.
Results
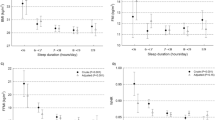
The adjusted difference in 12-month changes in weight and BMI in participants in the third tertile of sleep variability was 0.5 kg (95% CI 0.1 to 0.9; p = 0.021) and 0.2 kg/m2 (0.04 to 0.4; p = 0.015), respectively, as compared with participants in the first tertile. The adjusted difference in 12-month changes from baseline in WC was −0.8 cm (−1.5 to −0.01; p = 0.048) in participants sleeping <6 h, compared with those sleeping between 7 and 9 h.
Conclusions
Our findings suggest that the less variability in sleep duration or an adequate sleep duration the greater the success of the lifestyle interventions in adiposity.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Ogilvie RP, Patel SR. The epidemiology of sleep and obesity. Sleep Health. 2017;3:383–8.
Chaput JP, Després JP, Bouchard C, Tremblay A. Association of sleep duration with type 2 diabetes and impaired glucose tolerance. Diabetologia. 2007;50:2298–304.
Sperry SD, Scully ID, Gramzow RH, Jorgensen RS. Sleep duration and waist circumference in adults: a meta-analysis. Sleep. 2015;38:1269–76.
Xiao Q, Gu F, Caporaso N, Matthews CE. Relationship between sleep characteristics and measures of body size and composition in a nationally-representative sample. BMC Obes. 2016;3:48.
Rosique-Esteban N, Papandreou C, Romaguera D, Warnberg J, Corella D, Martínez-González MÁ, et al. Cross-sectional associations of objectively-measured sleep characteristics with obesity and type 2 diabetes in the PREDIMED-Plus trial. Sleep. 2018. https://doi.org/10.1093/sleep/zsy190.
Lopez-Garcia E, Faubel R, Leon-Muñoz L, Zuluaga MC, Banegas JR, Rodriguez-Artalejo F. Sleep duration, general and abdominal obesity, and weight change among the older adult population of Spain. Am J Clin Nutr. 2008;6:310–6.
Chaput JP, Després JP, Bouchard C, Tremblay A. The association between sleep duration and weight gain in adults: a 6-year prospective study from the Quebec Family Study. Sleep. 2008;31:517–23.
Appelhans BM, Janssen I, Cursio JF, Matthews KA, Hall M, Gold EB, et al. Sleep duration and weight change in midlife women: the SWAN sleep study. Obesity. 2013;21:77–84.
Chaput JP, Després JP, Bouchard C, Tremblay A. Longer sleep duration associates with lower adiposity gain in adult short sleepers. Int J Obes (Lond). 2012;36:752–6.
Garaulet M, Sánchez-Moreno C, Smith CE, Lee YC, Nicolás F, Ordovás JM. Ghrelin, sleep reduction and evening preference: relationships to CLOCK 3111 T/C SNP and weight loss. PLoS ONE. 2011;6:e17435.
Nedeltcheva AV, Kilkus JM, Imperial J, Schoeller DA, Penev PD. Insufficient sleep undermines dietary efforts to reduce adiposity. Ann Intern Med. 2010;153:435–41.
Hamet P, Tremblay J. Genetics of the sleep-wake cycle and its disorders. Metabolism. 2006;55(10Suppl 2):7–12.
Roenneberg T, Allebrandt KV, Merrow M, Vetter C. Social jetlag and obesity. Curr Biol. 2012;22:939–43.
Burgess HJ, Park M, Wyatt JK, Rizvydeen M, Fogg LF. Sleep and circadian variability in people with delayed sleep-wake phase disorder versus healthy controls. Sleep Med. 2017;34:33–9.
Ogilvie RP, Redline S, Bertoni AG, Chen X, Ouyang P, Szklo M, et al. Actigraphy measured sleep indices and adiposity: the multi-ethnic study of atherosclerosis (MESA). Sleep. 2016;39:1701–8.
He F, Bixler EO, Liao J, Berg A, Imamura Kawasawa Y, Fernandez-Mendoza J, et al. Habitual sleep variability, mediated by nutrition intake, is associated with abdominal obesity in adolescents. Sleep Med. 2015;16:1489–94.
Kobayashi D, Takahashi O, Shimbo T, Okubo T, Arioka H, Fukui T. High sleep duration variability is an independent risk factor for weight gain. Sleep Breath. 2013;17:167–72.
Knutson KL, Wu D, Patel SR, Loredo JS, Redline S, Cai J, et al. Association between sleep timing, obesity, diabetes: the Hispanic Community Health Study/Study of Latinos (HCHS/SOL) Cohort Study. Sleep. 2017. https://doi.org/10.1093/sleep/zsx014.
Taylor BJ, Matthews KA, Hasler BP, Roecklein KA, Kline CE, Buysse DJ, et al. Bedtime variability and metabolic health in midlife women: the SWAN sleep study. Sleep. 2016;39:457–65.
Wirth MD, Hébert JR, Hand GA, Youngstedt SD, Hurley TG, Shook RP, et al. Association between actigraphic sleep metrics and body composition. Ann Epidemiol. 2015;25:773–8.
Garaulet M, Corbalán MD, Madrid JA, Morales E, Baraza JC, Lee YC, et al. CLOCK gene is implicated in weight reduction in obese patients participating in a dietary programme based on the Mediterranean diet. Int J Obes (Lond). 2010;34:516–23.
Salas-Salvadó J, Díaz-López A, Ruiz-Canela M, Basora J, Fitó M, Corella D, et al. Effect of a lifestyle intervention program with energy-restricted Mediterranean diet and exercise on weight loss and cardiovascular risk factors: one-year results of the PREDIMED-Plus trial. Diabetes Care. 2018. https://doi.org/10.2337/dc18-0836.
Martínez-González MA, Buil-Cosiales P, Corella D, Bulló M, Fitó M, Vioque J, et al. Cohort profile: design and methods of the PREDIMED-Plus randomized trial. Int J Epidemiol. 2018. https://doi.org/10.1093/ije/dyy225.
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–5.
van Hees VT, Fang Z, Langford J, Assah F, Mohammad A, da Silva IC, et al. Autocalibration of accelerometer data for free-living physical activity assessment using local gravity and temperature: an evaluation on four continents. J Appl Physiol (1985). 2014;117:738–44.
van Hees VT, Sabia S, Anderson KN, Denton SJ, Oliver J, Catt M, et al. A novel, open access method to assess sleep duration using a wrist-worn accelerometer. PLoS ONE. 2015;10:e0142533.
Menai M, van Hees VT, Elbaz A, Kivimaki M, Singh-Manoux A, Sabia S. Accelerometer assessed moderate-to-vigorous physical activity and successful ageing: results from the Whitehall II study. Sci Rep. 2017;8:45772.
World Health Organization. Global recommendations on physical activity for health. 2010. http://www.who.int/dietphysicalactivity/factsheet_olderadults/en/. Accessed 3 Apr 2018.
Grandner MA, Patel NP, Gehrman PR, Perlis ML, Pack AI. Problems associated with short sleep: bridging the gap between laboratory and epidemiological studies. Sleep Med Rev. 2010;14:239–47.
Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, et al. National Sleep Foundation’s updated sleep duration recommendations: final report. Sleep Health. 2015;1:233–43.
Patel SR, Hayes AL, Blackwell T, Evans DS, Ancoli-Israel S, Wing YK, et al. The association between sleep patterns and obesity in older adults. Int J Obes (Lond). 2014;38:1159–64.
Broussard JL, Van Cauter E. Disturbances of sleep and circadian rhythms: novel risk factors for obesity. Curr Opin Endocrinol Diabetes Obes. 2016;23:353–9.
Oishi K, Shirai H, Ishida N. CLOCK is involved in the circadian transactivation of peroxisome-proliferator-activated receptor alpha (PPARalpha) in mice. Biochem J. 2005;386(Pt 3):575–81.
Turek FW, Joshu C, Kohsaka A, Lin E, Ivanova G, McDearmon E, et al. Obesity and metabolic syndrome in circadian Clock mutant mice. Science. 2005;308:1043–5.
Froy O. Metabolism and circadian rhythms-implications for obesity. Endocr Rev. 2010;31:1–24.
McHill AW, Melanson EL, Higgins J, Connick E, Moehlman TM, Stothard ER, et al. Impact of circadian misalignment on energy metabolism during simulated nightshift work. Proc Natl Acad Sci USA. 2014;111:17302–17.
Messina G, De Luca V, Viggiano A. Autonomic nervous system in the control of energy balance and body weight: personal contributions. Neurol Res Int. 2013;2013:639280.
Zitting KM, Vujovic N, Yuan RK, Isherwood CM, Medina JE, Wang W, et al. Human resting energy expenditure varies with circadian phase. Curr Biol. 2018;28:3685–90.
Mattson MP, Allison DB, Fontana L, Harvie M, Longo VD, Malaisse WJ, et al. Meal frequency and timing in health and disease. Proc Natl Acad Sci USA. 2014;111:16647–53.
Garaulet M, Gómez-Abellán P, Alburquerque-Béjar JJ, Lee YC, Ordovás JM, Scheer FA. Timing of food intake predicts weight loss effectiveness. Int J Obes (Lond). 2013;37:604–11.
Jakubowicz D, Barnea M, Wainstein J, Froy O. High caloric intake at breakfast vs. dinner differentially influences weight loss of overweight and obese women. Obesity (Silver Spring). 2013;21:2504–12.
Arble DM, Bass J, Laposky AD, Vitaterna MH, Turek FW. Circadian timing of food intake contributes to weight gain. Obesity (Silver Spring). 2009;17:2100–2.
Hairston KG, Bryer-Ash M, Norris JM, Haffner S, Bowden DW, Wagenknecht LE. Sleep duration and five-year abdominal fat accumulation in a minority cohort: the IRAS family study. Sleep. 2010;33:289–95.
Ardern CI, Katzmarzyk PT, Janssen I, Ross R. Discrimination of health risk by combined body mass index and waist circumference. Obes Res. 2003;11:135–42.
Janssen I, Katzmarzyk PT, Ross R. Waist circumference and not body mass index explains obesity-related health risk. Am J Clin Nutr. 2004;79:379–84.
Leproult R, Copinschi G, Buxton O, Van Cauter E. Sleep loss results in an elevation of cortisol levels the next evening. Sleep. 1997;20:865–70.
Donoho CJ, Weigensberg MJ, Emken BA, Hsu JW, Spruijt-Metz D. Stress and abdominal fat: preliminary evidence of moderation by the cortisol awakening response in Hispanic peripubertal girls. Obesity (Silver Spring). 2011;19:946–52.
Dashti HS, Zuurbier LA, de Jonge E, Voortman T, Jacques PF, Lamon-Fava S, et al. Actigraphic sleep fragmentation, efficiency and duration associate with dietary intake in the Rotterdam Study. J Sleep Res. 2016;25:404–11.
Acknowledgements
The authors especially thank the PREDIMED-Plus participants for their enthusiastic collaboration, the PREDIMED-Plus personnel for their outstanding support, and the personnel of all associated primary care centers for their exceptional effort. Centros de Investigación Biomédica en Red: Obesidad y Nutrición (CIBEROBN), Centros de Investigación Biomédica en Red: Epidemiología y Salud Pública (CIBERESP) and Centros de Investigación Biomédica en Red: Diabetes y Enfermedades Metabólicas asociadas (CIBERDEM) are initiatives of Instituto de Salud Carlos III (ISCIII), Madrid, Spain. Food companies, Hojiblanca and Patrimonio Comunal Olivarero, donated extra-virgin olive oil and Almond Board of California, American Pistachio Growers, and Paramount Farms donated nuts.
Funding
The PREDIMED-Plus trial was supported by the official funding agency for biomedical research of the Spanish government, ISCIII through the Fondo de Investigación para la Salud (FIS), which is co-funded by the European Regional Development Fund (three coordinated FIS projects led by JS-S and JV, including the following projects: PI13/00673, PI13/00492, PI13/00272, PI13/01123, PI13/00462, PI13/00233, PI13/02184, PI13/00728, PI13/01090, PI13/01056, PI14/01722, PI14/00636, PI14/00618, PI14/00696, PI14/01206, PI14/01919, PI14/00853, PI14/01374, PI16/00473, PI16/00662, PI16/01873, PI16/01094, PI16/00501, PI16/00533, PI16/00381, PI16/00366, PI16/01522, PI16/01120, PI17/00764, PI17/01183, PI17/00855, PI17/01347, PI17/00525, PI17/01827, PI17/00532, PI17/00215, PI17/01441, PI17/00508, PI17/01732, PI17/00926), the Especial Action Project entitled: Implementación y evaluación de una intervención intensiva sobre la actividad física Cohorte PREDIMED-PLUS grant to Jordi Salas-Salvadó, the European Research Council (Advanced Research Grant 2013–2018; 340918) grant to MÁM-G, the Recercaixa grant to JS-S (2013ACUP00194), the grant from the Consejería de Salud de la Junta de Andalucía (PI0458/2013; PS0358/2016), the PROMETEO/2017/017 grant from the Generalitat Valenciana, the SEMERGEN grant and FEDER funds (CB06/03), OC is granted by the JR17/00022, ISCIII. CP is supported by a postdoctoral fellowship granted by the Autonomous Government of Catalonia (PERIS 2016–2020 Incorporació de Científics i Tecnòlegs, SLT002/0016/00428). None of the funding sources took part in the design, collection, analysis or interpretation of the data, or in the decision to submit the manuscript for publication. The corresponding authors had full access to all the data in the study and had final responsibility to submit for publication.
Author contributions
CP, MB, and JS-S: designed the research. CP, MB, AD-L, MAM-G, DC, MF, JV, DR, JAM, JL-M, RE, AB-C, FA, JAT, FJT, LS-M, VM, JL, CV, XP, JV, LD, MD-R, ER, IA, JB-L, AG-A, NB, HS, ET, AA-G, and JS-S: conducted the research. CP, MB, and JS-S: analyzed the data. CP wrote the article. CP and JS-S are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. All authors revised the manuscript for important intellectual content and read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
JS-S reports serving on the board of and receiving grant support through his institution from International Nut and Dried Fruit Council; receiving consulting personal fees from Danone, Font Vella Lanjaron, Nuts for Life, and Eroski; and receiving grant support through his institution from Nut and Dried Fruit Foundation and Eroski. ER reports grants, non-financial support, and other fees from California Walnut Commission and Alexion; personal fees and non-financial support from Merck, Sharp & Dohme; personal fees, non-financial support, and other fees from Aegerion and Ferrer International; grants and personal fees from Sanofi Aventis; grants from Amgen and Pfizer and; personal fees from Akcea, outside of the submitted work. XP reports serving on the board of and receiving consulting personal fees from Sanofi Aventis, Amgen, and Abbott laboratories; receiving lecture personal fees from Esteve, Lacer, and Rubio laboratories. MD-R reports receiving grants from the Diputación Provincial de Jaén and the Caja Rural de Jaén. LD reports grants from Fundación Cerveza y Salud. The other authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Papandreou, C., Bulló, M., Díaz-López, A. et al. High sleep variability predicts a blunted weight loss response and short sleep duration a reduced decrease in waist circumference in the PREDIMED-Plus Trial. Int J Obes 44, 330–339 (2020). https://doi.org/10.1038/s41366-019-0401-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-019-0401-5
This article is cited by
-
Role of Sleep and Sleep Disorders in Cardiometabolic Risk: a Review and Update
Current Sleep Medicine Reports (2024)
-
Effect of sleep on weight loss and adherence to diet and physical activity recommendations during an 18-month behavioral weight loss intervention
International Journal of Obesity (2022)
-
Sleep characteristics modify the associations of physical activity during pregnancy and gestational weight gain
Archives of Gynecology and Obstetrics (2022)
-
The association between sleep health and weight change during a 12-month behavioral weight loss intervention
International Journal of Obesity (2021)
-
Type 1 Diabetes, Sleep, and Hypoglycemia
Current Diabetes Reports (2021)