Abstract
Objectives
Neck adipose tissue (NAT) volume increases with general adiposity, with fat accumulating in different neck tissue compartments. In patients with certain malignant/benign tumours, the accumulation of NAT, and certain NAT distributions, have been associated with cardiometabolic risk (CMR). However, it is unknown whether the same relationships exist in healthy people, and whether NAT accumulation and distribution are related to the inflammatory status.
Methods
In this cross-sectional study, 139 young healthy adults (68% women) underwent a computed tomography scan to quantify the volume of compartmental (i.e., subcutaneous, intermuscular and perivertebral) and total NAT at the height of vertebra C5. Anthropometric indicators were measured, and body composition determined using dual energy X-ray absorptiometry. Information on CMR factors (i.e., blood glycaemic and lipid markers, blood pressure and physical fitness) was also gathered, and a CMR score calculated. Several plasma cytokines and serum components of the innate immune system were measured to determine the inflammatory status.
Results
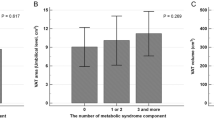
Compartmental and total NAT volumes were directly related to body mass index (BMI), and lean, fat, and visceral adipose tissue (VAT) masses (all, P ≤ 0.05). Larger compartmental (especially intermuscular) and total NAT volumes were directly associated with the CMR score, several CMR factors (i.e., glycaemic and lipid markers and blood pressure), and the C3, C4 and leptin concentrations. They were, however, inversely correlated with the CMR factors high density lipoprotein-cholesterol (HDL-C) and physical fitness, and with the adiponectin concentration (all P ≤ 0.05). Several of these associations remained statistically significant (P ≤ 0.05) after adjustment for BMI, body fat percentage or VAT mass. Overall, results did not change after applying false discovery rate correction.
Conclusions
NAT volume and its distribution among different tissue compartments is associated with the CMR and inflammatory profile of young healthy adults. Total NAT volume appears to be as valuable as VAT mass in terms of predicting CMR and inflammatory status.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Lafontan M. Historical perspectives in fat cell biology: the fat cell as a model for the investigation of hormonal and metabolic pathways. Am J Physiol Cell Physiol. 2012;302:C327–59. https://doi.org/10.1152/ajpcell.00168.2011.
Halade GV, Kain V. Obesity and cardiometabolic defects in heart failure pathology. Compr Physiol.2017;7:1463–77. https://doi.org/10.1002/cphy.c170011.
Alberti KG, Zimmet P, Shaw J. The metabolic syndrome-a new worldwide definition. Lancet. 2005;366:1059–62. https://doi.org/10.1016/s0140-6736(05)67402-8.
Cornier MA, Despres JP, Davis N, Grossniklaus DA, Klein S, Lamarche B, et al. Assessing adiposity: a scientific statement from the American Heart Association. Circulation. 2011;124:1996–2019. https://doi.org/10.1161/CIR.0b013e318233bc6a.
Amirabdollahian F, Haghighatdoost F. Anthropometric Indicators of Adiposity Related to Body Weight and Body Shape as Cardiometabolic Risk Predictors in British Young Adults: Superiority of Waist-to-Height Ratio. 2018;2018:8370304. https://doi.org/10.1155/2018/8370304.
Alzeidan R, Fayed A Performance of neck circumference to predict obesity and metabolic syndrome among adult Saudis: a cross-sectional study. 2019;6:13. https://doi.org/10.1186/s40608-019-0235-7.
Preis S, Massaro J, Hoffmann U, D’Agostino RB Sr, Levy D, Robins SJ, et al. Neck circumference as a novel measure of cardiometabolic risk: the Framingham Heart study. J Clin Endocrinol Metab. 2010;95:3701–10. https://doi.org/10.1210/jc.2009-1779.
Nielsen S, Guo Z, Johnson CM, Hensrud DD, Jensen MD. Splanchnic lipolysis in human obesity. J Clin Investig. 2004;113:1582–8. https://doi.org/10.1172/jci21047.
Guo Z, Hensrud DD, Johnson CM, Jensen MD. Regional postprandial fatty acid metabolism in different obesity phenotypes. Diabetes. 1999;48:1586–92. https://doi.org/10.2337/diabetes.48.8.1586.
Torriani M, Gill CM, Daley S, Oliveira AL, Azevedo DC, Bredella MA. Compartmental neck fat accumulation and its relation to cardiovascular risk and metabolic syndrome. Am J Clin NutR. 2014;100:1244–51. https://doi.org/10.3945/ajcn.114.088450.
Rosenquist K, Therkelsen K, Massaro J, Hoffmann U, Fox C. Development and reproducibility of a computed tomography-based measurement for upper body subcutaneous neck fat. J Am Heart Assoc. 2014;3:e000979. https://doi.org/10.1161/jaha.114.000979.
Pandzic JV, Grizelj D, Livun A, Boscic D, Ajduk M, Kusec R, et al. Neck adipose tissue - tying ties in metabolic disorders. Horm Mol Biol Clin Investig. 2018;33. https://doi.org/10.1515/hmbci-2017-0075.
Tal S, Litovchik I The association between neck adiposity and long-term outcome. 2019;14:e0215538. https://doi.org/10.1371/journal.pone.0215538.
Kodama S, Saito K, Tanaka S, Maki M, Yachi Y, Asumi M, et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. JAMA. 2009;301:2024–35. https://doi.org/10.1001/jama.2009.681.
Carobbio S, Pellegrinelli V, Vidal-Puig A. Adipose tissue function and expandability as determinants of lipotoxicity and the metabolic syndrome. Adv Exp Med Biol. 2017;960:161–96. https://doi.org/10.1007/978-3-319-48382-5_7.
Virtue S, Vidal-Puig A. Adipose tissue expandability, lipotoxicity and the Metabolic Syndrome-an allostatic perspective. Biochimica et biophysica acta. 2010;1801:338–49. https://doi.org/10.1016/j.bbalip.2009.12.006.
Saltiel AR, Olefsky JM. Inflammatory mechanisms linking obesity and metabolic disease. J Clin Investig. 2017;127:1–4. https://doi.org/10.1172/jci92035.
Sam S Differential effect of subcutaneous abdominal and visceral adipose tissue on cardiometabolic risk. Horm Mol Biol Clin Investig. 2018;33. https://doi.org/10.1515/hmbci-2018-0014.
Bruun JM, Lihn AS, Pedersen SB, Richelsen B. Monocyte chemoattractant protein-1 release is higher in visceral than subcutaneous human adipose tissue (AT): implication of macrophages resident in the AT. J Clin Endocrinol Metabol. 2005;90:2282–9. https://doi.org/10.1210/jc.2004-1696.
Kranendonk ME, van Herwaarden JA, Stupkova T, de Jager W, Vink A, Moll FL, et al. Inflammatory characteristics of distinct abdominal adipose tissue depots relate differently to metabolic risk factors for cardiovascular disease: distinct fat depots and vascular risk factors. Atherosclerosis. 2015;239:419–27. https://doi.org/10.1016/j.atherosclerosis.2015.01.035.
Pou KM, Massaro JM, Hoffmann U, Vasan RS, Maurovich-Horvat P, Larson MG, et al. Visceral and subcutaneous adipose tissue volumes are cross-sectionally related to markers of inflammation and oxidative stress: the Framingham Heart Study. Circulation. 2007;116:1234–41. https://doi.org/10.1161/circulationaha.107.710509.
Sanchez-Delgado G, Martinez-Tellez B, Olza J, Aguilera CM, Labayen I, Ortega FB, et al. Activating brown adipose tissue through exercise (ACTIBATE) in young adults: rationale, design and methodology. Contemp Clin Trials. 2015;45:416–25. https://doi.org/10.1016/j.cct.2015.11.004.
Martinez-Tellez B, Sanchez-Delgado G, Garcia-Rivero Y, Alcantara JMA, Martinez-Avila WD, Munoz-Hernandez MV, et al. A new personalized cooling protocol to activate brown adipose tissue in young adults. Front Physiol. 2017;8:863. https://doi.org/10.3389/fphys.2017.00863.
Chung H, Cobzas D, Birdsell L, Lieffers J, Baracos V Automated segmentation of muscle and adipose tissue on CT images for human body composition analysis. Paper presented at: Medical Imaging 2009: Visualization, Image-Guided Procedures, and Modeling 2009.
Stewart A, Marfell-Jones M, Olds T, Ridder dH. International Society for Advancement of Kinanthropometry. International standards for anthropometric assessment. Lower Hutt, New Zealand: International Society for the Advancement of Kinanthropometry. 2011:50–3.
Carbone S, Billingsley HE, Rodriguez-Miguelez P, Kirkman DL, Garten R, Franco RL, et al. Lean mass abnormalities in heart failure: the role of sarcopenia, sarcopenic obesity, and cachexia. Curr Probl Cardiol. 2019:100417. https://doi.org/10.1016/j.cpcardiol.2019.03.006.
Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502.
Matthews D, Hosker J, Rudenski A, Naylor B, Treacher D, Turner R. Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9.
Ruiz-Ruiz J, Mesa JL, Gutiérrez A, Castillo MJ. Hand size influences optimal grip span in women but not in men. J Hand Surg. 2002;27:897–901.
Balke B, Ware RW The present status of physical fitness in the Air Force. SCHOOL OF AVIATION MEDICINE RANDOLPH AFB TX;1959.
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–5. https://doi.org/10.1161/circulationaha.109.192644.
Arias Tellez MJ, Acosta FM, Garcia-Rivero Y, Pascual-Gamarra JM, Merchan-Ramirez E, Martinez-Tellez B, et al. Neck adipose tissue accumulation is related to a higher overall and central adiposity, cardiometabolic risk, and a pro-inflammatory profile in adults. figshare. Online resource. 2020. https://doi.org/10.6084/m9.figshare.12037233.v1.
Dmitrienko A, D’Agostino RB Sr, Huque MF. Key multiplicity issues in clinical drug development. Stat Med. 2013;32:1079–111. https://doi.org/10.1002/sim.5642.
Tate RL, Perdices M, Rosenkoetter U, Shadish W, Vohra S, Barlow DH, et al. The Single-Case Reporting Guideline In BEhavioural Interventions (SCRIBE) 2016 Statement. Phys Ther. 2016;96:e1–10. https://doi.org/10.2522/ptj.2016.96.7.e1.
Diedenhofen B, Musch J. cocor: a comprehensive solution for the statistical comparison of correlations. PLoS ONE. 2015;10:e0121945. https://doi.org/10.1371/journal.pone.0121945.
Williams CM. Lipid metabolism in women. Proc Nutr Soc. 2004;63:153–60.
Karpe F, Pinnick KE. Biology of upper-body and lower-body adipose tissue-link to whole-body phenotypes. Nat Rev Endocrinol. 2015;11:90–100. https://doi.org/10.1038/nrendo.2014.185.
Lee JJ, Pedley A, Therkelsen KE, Hoffmann U, Massaro JM, Levy D, et al. Upper body subcutaneous fat is associated with cardiometabolic risk factors. Am J Med. 2017;130:958–66.e951. https://doi.org/10.1016/j.amjmed.2017.01.044.
Malisova L, Rossmeislova L, Kovacova Z, Kracmerova J, Tencerova M, Langin D, et al. Expression of inflammation-related genes in gluteal and abdominal subcutaneous adipose tissue during weight-reducing dietary intervention in obese women. Physiol Res. 2014;63:73–82.
Pinnick KE, Nicholson G, Manolopoulos KN, McQuaid SE, Valet P, Frayn KN, et al. Distinct developmental profile of lower-body adipose tissue defines resistance against obesity-associated metabolic complications. Diabetes. 2014;63:3785–97. https://doi.org/10.2337/db14-0385.
Vallianou NG, Evangelopoulos AA, Bountziouka V, Vogiatzakis ED, Bonou MS, Barbetseas J, et al. Neck circumference is correlated with triglycerides and inversely related with HDL cholesterol beyond BMI and waist circumference. Diabetes/metabolism Res Rev. 2013;29:90–7. https://doi.org/10.1002/dmrr.2369.
Preis SR, Pencina MJ, D’Agostino RB Sr, Meigs JB, Vasan RS, Fox CS. Neck circumference and the development of cardiovascular disease risk factors in the Framingham Heart Study. Diabetes Care. 2013;36:e3. https://doi.org/10.2337/dc12-0738.
UD M, Raiko J, Saari T, Saunavaara V, Kudomi N, Solin O, et al. Human brown fat radiodensity indicates underlying tissue composition and systemic metabolic health. J Clin Endocrinol Metab. 2017;102:2258–67. https://doi.org/10.1210/jc.2016-2698.
Funding
This study was funded by the Spanish Ministry of Economy and Competitiveness via the Fondo de Investigación Sanitaria del Instituto de Salud Carlos III (PI13/01393) and PTA 12264-I, Retos de la Sociedad (DEP2016-79512-R) and European Regional Development Funds(ERDF), the Spanish Ministry of Education (FPU 13/03410), the Fundación Iberoamericana de Nutrición (FINUT), the Redes Temáticas de Investigación Cooperativa RETIC (Red SAMID RD16/0022), the AstraZeneca HealthCare Foundation, the University of Granada Plan Propio de Investigación 2016 – Excellence actions: Unit of Excellence on Exercise and Health (UCEES) – and Plan Propio de Investigación 2018: Programa Contratos-Puente, the Junta de Andalucía, Consejería de Conocimiento, Investigación y Universidades (ERDF, SOMM17/6107/UGR) - and the Fundación Carolina (C.2016-574961). This study is part of a PhD thesis conducted with the framework of the Biomedicine Doctoral Studies Programme of the University of Granada, Spain.
Author information
Authors and Affiliations
Contributions
MJAT, FAM, JMPG, BMT, JMLL, JRR designed the study; MJAT, FAM, YGR, JMPG, EMR, and BMT conducted the research; JMLL and JRR provided essential reagents and materials; MJAT, FAM, JMPG, and EMR analysed the data and performed the statistical analysis; MJAT and FAM wrote the manuscript; MJAT, FAM, YGR, JMPG, EMR, BMT, AMS, JAL, JMLL, and JRR reviewed the manuscript and provided scientific assistance; JRR had primary responsibility for the paper’s final content.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Arias-Tellez, M.J., Acosta, F.M., Garcia-Rivero, Y. et al. Neck adipose tissue accumulation is associated with higher overall and central adiposity, a higher cardiometabolic risk, and a pro-inflammatory profile in young adults. Int J Obes 45, 733–745 (2021). https://doi.org/10.1038/s41366-020-00701-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-020-00701-5
This article is cited by
-
Change of neck circumference in relation to visceral fat area: a Chinese community-based longitudinal cohort study
International Journal of Obesity (2022)
-
Circulating concentrations of free triiodothyronine are associated with central adiposity and cardiometabolic risk factors in young euthyroid adults
Journal of Physiology and Biochemistry (2022)