Abstract
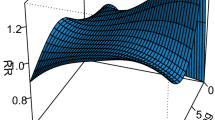
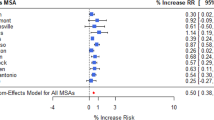
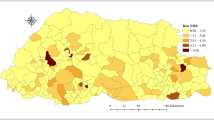
Pneumonia accounts for 1.5% of all overnight hospital admission in Australia. We investigated the nonlinear and delay effect of weather (temperature and rainfall) on pneumonia. This study was based on a large cohort of inpatients that were hospitalized due to pneumonia between 2006 and 2016. Cases were identified using the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, Australian Modification (ICD10-AM) codes J10.0*–J18.0*. A time-varying distributed lag nonlinear model was used to estimate the burden of the disease attributable to varying weather-lag pneumonia relationships and identify vulnerable groups. The relative risk (presented as logRR) associated with temperature was immediate and highest in late winter at the lowest temperature of 16 °C (logRR = 1.13, 95% confidence intervals (CI): 0.59, 1.66). The cumulative effect over the lag range 0–8 weeks revealed two peaks for low (12 mm, logRR = 0.73, 95% CI: 0.32, 1.13) and moderately high rainfall (51 mm) with logRR of 1.15 (95% CI: 0.10, 2.20). A substantial number, 22.50% (95% empirical CI: 1.83, 34.68), of pneumonia cases were attributable to temperature (mostly due to moderate low temperatures). Females and indigenous (Aboriginal and Torres Strait Islander) patients were particularly vulnerable to the impact of temperature-related pneumonia. In this study, we highlighted the delayed effects and magnitude of burden of pneumonia that is associated with low temperature and rainfall. The findings in this study can inform a better understanding of the health implications and burden associated with pneumonia to support discussion-making in healthcare and establish a strategy for prevention and control of the disease among vulnerable groups.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Troeger C, Forouzanfar M, Rao PC, Khalil I, Brown A, Swartz S, et al. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of lower respiratory tract infections in 195 countries: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Infect Dis. 2017;17:1133–61.
Australian Institute of Health and Welfare. Australian Burden of Disease Study: impact and causes of illness and death in Australia 2011. Australian Burden of Disease Study series no. 3. BOD4. Canberra: AIHW; 2016.
Australian Institute of Health and Welfare. Admitted patient care 2016–17: Australian hospital statistics. Health services series no. 84. Cat no. HSE 201. Canberra: AIHW; 2018.
Chan P, Chew F, Tan T, Chua K, Hooi P. Seasonal variation in respiratory syncytial virus chest infection in the tropics. Pediatr Pulmonol. 2002;34:47–51.
Paynter S, Weinstein P, Ware RS, Lucero MG, Tallo V, Nohynek H, et al. Sunshine, rainfall, humidity and child pneumonia in the tropics: time-series analyses. Epidemiol Infect. 2013;141:1328–36.
Enwere G, Cheung YB, Zaman SM, Akano A, Oluwalana C, Brown O, et al. Epidemiology and clinical features of pneumonia according to radiographic findings in Gambian children. Trop Med Int health. 2007;12:1377–85.
Green RS, Basu R, Malig B, Broadwin R, Kim JJ, Ostro B. The effect of temperature on hospital admissions in nine California counties. Int J Public health. 2010;55:113–21.
Song G, Chen G, Jiang L, Zhang Y, Zhao N, Chen B, et al. Diurnal temperature range as a novel risk factor for COPD death. Respirology. 2008;13:1066–9.
Xu Z, Hu W, Tong S. Temperature variability and childhood pneumonia: an ecological study. Environ Health. 2014;13:51.
Xu Z, Hu W, Tong S. The geographical co-distribution and socio-ecological drivers of childhood pneumonia and diarrhoea in Queensland, Australia. Epidemiol Infect. 2015;143:1096–104.
Xu Z, Liu Y, Ma Z, Li S, Hu W, Tong S. Impact of temperature on childhood pneumonia estimated from satellite remote sensing. Environ Res. 2014;132:334–41.
Onozuka D, Hashizume M, Hagihara A. Impact of weather factors on Mycoplasma pneumoniae pneumonia. Thorax. 2009;64:507–11.
Kim PE, Musher DM, Glezen WP, Barradas MCR, Nahm WK, Wright CE. Association of invasive pneumococcal disease with season, atmospheric conditions, air pollution, and the isolation of respiratory viruses. Clin Infect Dis. 1996;22:100–6.
Chen Z, Ji W, Wang Y, Yan Y, Zhu H, Shao X, et al. Epidemiology and associations with climatic conditions of Mycoplasma pneumoniae and Chlamydophila pneumoniae infections among Chinese children hospitalized with acute respiratory infections. Ital J Pediatr. 2013;39:34.
Qiu H, Sun S, Tang R, Chan K-P, Tian L. Pneumonia hospitalization risk in the elderly attributable to cold and hot temperatures in Hong Kong, China. Am J Epidemiol. 2016;184:570–8.
Murdoch KM, Mitra B, Lambert S, Erbas B. What is the seasonal distribution of community acquired pneumonia over time? A systematic review. Australas Emerg Nurs J. 2014;17:30–42.
Gasparrini A. Distributed lag linear and non-linear models in R: the package dlnm. J Stat Softw. 2011;43:1–20.
Gasparrini A. Modeling exposure–lag–response associations with distributed lag non‐linear models. Stat Med. 2014;33:881–99.
Gasparrini A, Armstrong B, Kenward MG. Distributed lag non‐linear models. Stat Med. 2010;29:2224–34.
Gasparrini A, Guo Y, Hashizume M, Lavigne E, Tobias A, Zanobetti A, et al. Changes in susceptibility to heat during the summer: a multicountry analysis. Am J Epidemiol. 2016;183:1027–36.
Gasparrini A, Leone M. Attributable risk from distributed lag models. BMC Med Res Methodol. 2014;14:55–55.
R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2017.
Tian D-D, Jiang R, Chen X-J, Ye Q. Meteorological factors on the incidence of MP and RSV pneumonia in children. PLoS One. 2017;12:e0173409.
Zhang Z, Hong Y, Liu N. Association of ambient Particulate matter 2.5 with intensive care unit admission due to pneumonia: a distributed lag non-linear model. Sci Rep. 2017;7:8679.
Cilloniz C, Ewig S, Gabarrus A, Ferrer M, Puig de la Bella Casa J, Mensa J, et al. Seasonality of pathogens causing community‐acquired pneumonia. Respirology. 2017;22:778–85.
Adegboye O, Adegboye M. Spatially correlated time series and ecological niche analysis of cutaneous leishmaniasis in Afghanistan. Int J Environ Res Public Health. 2017;14:309.
Lytras T, Pantavou K, Mouratidou E, Tsiodras S. Mortality attributable to seasonal influenza in Greece, 2013 to 2017: variation by type/subtype and age, and a possible harvesting effect. Eurosurveillance. 2019; 24:1800118.
Adegboye MA, Olumoh J, Saffary T, Elfaki F, Adegboye OA. Effects of time-lagged meteorological variables on attributable risk of leishmaniasis in central region of Afghanistan. Sci Total Environ. 2019;685:533–41.
Adegboye O, Al-Saghir M, Leung D. Joint spatial time-series epidemiological analysis of malaria and cutaneous leishmaniasis infection. Epidemiol Infect. 2017;145:685–700.
Gasparrini A, Scheipl F, Armstrong B, Kenward M. A penalized framework for distributed lag non‐linear models. Biometrics. 2017;73:938–48.
Watson M, Gilmour R, Menzies R, Ferson M, McIntyre P, New South Wales Pneumococcal Network. The association of respiratory viruses, temperature, and other climatic parameters with the incidence of invasive pneumococcal disease in Sydney, Australia. Clin Infect Dis. 2006;42:211–5.
Onozuka D, Hashizume M, Hagihara A. Impact of weather factors on Mycoplasma pneumoniae pneumonia. Thorax. 2009;64:507–11.
Graudenz GS, Landgraf RG, Jancar S, Tribess A, Fonseca SG, Faé KC, et al. The role of allergic rhinitis in nasal responses to sudden temperature changes. J Allergy Clin Immunol. 2006;118:1126–32.
Sun S, Laden F, Hart JE, Qiu H, Wang Y, Wong CM, et al. Seasonal temperature variability and emergency hospital admissions for respiratory diseases: a population-based cohort study. Thorax. 2018;73:951–8.
Fares A. Factors influencing the seasonal patterns of infectious diseases. Int J Prev Med. 2013;4:128.
Mamani M, Muceli N, Basir HRG, Vasheghani M, Poorolajal J. Association between serum concentration of 25-hydroxyvitamin D and community-acquired pneumonia: a case-control study. Int J Gen Med. 2017;10:423.
McNally JD, Leis K, Matheson LA, Karuananyake C, Sankaran K, Rosenberg AM. Vitamin D deficiency in young children with severe acute lower respiratory infection. Pediatr Pulmonol. 2009;44:981–8.
Eccles R. An explanation for the seasonality of acute upper respiratory tract viral infections. Acta Otolaryngol. 2002;122:183–91.
Choi W-I, Rho BH, Lee M-Y. Male predominance of pneumonia and hospitalization in pandemic influenza A (H1N1) 2009 infection. BMC Res Notes. 2011;4:351.
Torzillo P, Dixon J, Manning K, Hutton S, Gratten M, Hueston L, et al. Etiology of acute lower respiratory tract infection in Central Australian Aboriginal children. Pediatr Infect Dis J. 1999;18:714–21.
Ford JD. Indigenous health and climate change. Am J Public Health. 2012;102:1260–6.
Burgner D, Richmond P. The burden of pneumonia in children: an Australian perspective. Paediatr Respir Rev. 2005;6:94–100.
Skull SA, Andrews RM, Byrnes GB, Campbell DA, Nolan TM, Brown GV, et al. ICD-10 codes are a valid tool for identification of pneumonia in hospitalized patients aged > or = 65 years. Epidemiol Infect. 2008;136:232–40.
kull SA, Andrews RM, Byrnes GB, Campbell DA, Kelly HA, Brown GV, et al. Hospitalized community-acquired pneumonia in the elderly: an Australian case-cohort study. Epidemiol Infect. 2009;137:194–202.
Acknowledgements
This work was supported by a financial grant from the Townsville Hospital and Health Service Study Education Research Trust Account.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics
Ethical approval was obtained from the Townsville Hospital and Health Service Human Research Ethics Committee (HREC/16/QTHS/221) and the Queensland Public Health Act (RD007802) for the data linkage project.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Adegboye, O.A., McBryde, E.S. & Eisen, D.P. Epidemiological analysis of association between lagged meteorological variables and pneumonia in wet-dry tropical North Australia, 2006–2016. J Expo Sci Environ Epidemiol 30, 448–458 (2020). https://doi.org/10.1038/s41370-019-0176-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41370-019-0176-8
Keywords
This article is cited by
-
Neighborhood environmental factors linked to hospitalizations of older people for viral lower respiratory tract infections in Spain: a case-crossover study
Environmental Health (2022)
-
Lagged meteorological impacts on COVID-19 incidence among high-risk counties in the United States—a spatiotemporal analysis
Journal of Exposure Science & Environmental Epidemiology (2022)