Abstract
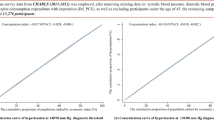
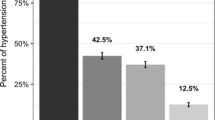
With an aim to examine the socio-economic inequalities in prevalence, awareness, treatment, and control of hypertension, this study analyzed 14,823 adults, 15 years or older with blood pressure measured, in the 2016 Nepal Demographic Health Survey. Multi-variable logistic regression and Lorenz curves were used to explore the inequalities. The prevalence of hypertension was 19.5% (95% CI: 18.3–20.7). Further, of the total hypertensive, the prevalence of hypertension awareness, treatment and control was 40.0% (95% CI: 37.5–42.6), 20.2% (95% CI: 18.0–22.2) and 10.5% (95% CI: 8.8–12.2), respectively. Participants with secondary (OR: 1.45, 95% CI: 1.20–1.76) and higher education (OR:1.42, 95% CI: 1.10–1.83), compared to those with no education/preschool, and those in urban residency (OR: 1.28, 95% CI: 1.09–1.50) compared to rural areas, and in province-4 (OR: 1.50, 95% CI: 1.14–1.96) and province-5 (OR: 1.34, 95% CI: 1.04–1.72), compared to province-1, had higher odds of being hypertensive. Household wealth status showed a positive association with prevalence, awareness, and treatment of hypertension (p-trend < 0.001). Those from richest category were 1.7 times more likely to be hypertensive, were more aware of hypertension (3.2 times), received treatment (5.1 times), and had controlled hypertension (1.6 times), compared to the poorest category. Adjusting for body mass index, completely ameliorate the effect on hypertension prevalence (p-trend = 0.57) and altered nominally awareness (p-trend < 0.0001), treatment (p-trend < 0.0001), and control (p-trend = 0.099). Urban hypertensive females, at the lowest wealth quintile, received poor care services; only 12% were aware of their hypertension status, 7% received treatment, and only 4% had controlled hypertension. These socio-economic inequalities warrant interventions aiming at preventing hypertension and increasing coverage of services for those higher at risk. Future studies need to explore socio-economic and geographic disparities in disease burden and cascade of services.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
WHO. Global status report on noncommunicable diseases 2010. Geneva: World Health Organization; 2011.
WHO. Causes of death 2008: data sources and methods. Geneva: Department of Health Statistics and Informatics, World Health Organization; 2011. http://www.who.int/healthinfo/global_burden_disease/cod_2008_sources_methods.pdf.
Vaidya A, Pathak RP, Pandey MR. Prevalence of hypertension in Nepalese community triples in 25 years: a repeat cross-sectional study in rural Kathmandu. Indian Heart J. 2012;64:128–31.
Vaidya A, Pokharel PK, Nagesh S, Karki P, Kumar S, Majhi S. War veterans of Nepal and their blood pressure status: a population-based comparative study. J Hum Hypertens. 2007;21:900–3.
Pandey M, Dhungel S. Prevalence of hypertension in an urban community of Nepal. JNMA. 1983;21:1–5.
Chataut J, Adhikari RK, Sinha NP. The prevalence of and risk factors for hypertension in adults living in central development region of Nepal. Kathmandu. Univ Med J. 2011;9:13–8.
WHO. Nepal STEPS noncommunicable disease risk factors survey 2005. Geneva: World Health Organization; Society for Local Integrated Development Nepal; Central Bureau of Statistics, Nepal; Government of Nepal; 2005.
Aryal KK, Neupane S, Mehata S, Vaidya A, Singh S, Paulin F, et al. Non communicable diseases risk factors: STEPS Survey Nepal 2013. Kathmandu: Nepal Health Research Council (NHRC); 2014.
Marmot M, Friel S, Bell R, Houweling TA, Taylor S. Closing the gap in a generation: health equity through action on the social determinants of health. Lancet. 2008;372:1661–9.
Hosseinpoor AR, Bergen N, Mendis S, Harper S, Verdes E, Kunst A, et al. Socioeconomic inequality in the prevalence of noncommunicable diseases in low-and middle-income countries: results from the World Health Survey. BMC Public Health. 2012;12:474.
Moser KA, Agrawal S, Smith GD, Ebrahim S. Socio-demographic inequalities in the prevalence, diagnosis and management of hypertension in India: analysis of nationally-representative survey data. PLoS ONE. 2014;9:e86043.
Busingye D, Arabshahi S, Subasinghe AK, Evans RG, Riddell MA, Thrift AG. Do the socioeconomic and hypertension gradients in rural populations of low-and middle-income countries differ by geographical region? A systematic review and meta-analysis. Int J Epidemiol. 2014;43:1563–77.
Subramanian S, Corsi DJ, Subramanyam MA, Davey Smith G. Jumping the gun: the problematic discourse on socioeconomic status and cardiovascular health in India. Int J Epidemiol. 2013;42:1410–26.
Grotto I, Huerta M, Sharabi Y. Hypertension and socioeconomic status. Curr Opin Cardiol. 2008;23:335–9.
Hoang VM, Byass P, Dao LH, Nguyen TK, Wall S. Risk factors for chronic disease among rural Vietnamese adults and the association of these factors with sociodemographic variables: findings from the WHO STEPS survey in rural Vietnam, 2005. Prev Chronic Dis. 2007;4:A22.
Grotto I, Huerta M, Grossman E, Sharabi Y. Relative impact of socioeconomic status on blood pressure lessons from a large-scale survey of young adults. Am J Hypertens. 2007;20:1140–5.
Le C, Chongsuvivatwong V, Geater A. Contextual socioeconomic determinants of cardiovascular risk factors in rural south-west China: a multilevel analysis. BMC Public Health. 2007;7:72.
Gregory CO, Dai J, Ramirez-Zea M, Stein AD. Occupation is more important than rural or urban residence in explaining the prevalence of metabolic and cardiovascular disease risk in Guatemalan adults. J Nutr. 2007;137:1314–9.
CBS. National Population and Housing Census 2011 (National Report). Central Bureau of Statistics, National Planning Commission Secretariat, Government of Nepal; Kathmandu 2012.
Mehata S, Shrestha N, Mehta R, Vaidya A, Rawal LB, Bhattarai N, et al. Prevalence, awareness, treatment and control of hypertension in Nepal: data from nationally representative population-based cross-sectional study. J Hypertens. 2018;36:000-.
Ministry of Health and Population Nepal, New ERA. Nepal demographic and health survey, 2016. Kathmandu: Population Division, Ministry of Health and Population; 2016.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289:2560–71.
WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157.
Jeon Y-J, Kim CR, Park J-S, Choi K-H, Kang MJ, Park SG, et al. Health inequalities in hypertension and diabetes management among the poor in urban areas: a population survey analysis in south Korea. BMC Public Health. 2016;16:492.
Christiani Y, Byles J, Tavener M, Dugdale P. Assessing socioeconomic inequalities of hypertension among women in Indonesia’s major cities. J Hum Hypertens. 2015;29:683.
Biswas T, Islam MS, Linton N, Rawal LB. Socio-economic inequality of chronic non-communicable diseases in Bangladesh. PLoS ONE. 2016;11:e0167140.
Kennedy BP, Kawachi I, Prothrow-Stith D. Income distribution and mortality: cross sectional ecological study of the Robin Hood index in the United States. BMJ. 1996;312:1004–7.
Jadoo M. Geospatial analysis with PROC GMAP. North Carolina, USA. https://www.analyticsncsuedu/sesug/2016/RV-278_Final_PDFpdf.
Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Himmelfarb CD, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71:e127–e248.
Prince MJ, Ebrahim S, Acosta D, Ferri CP, Guerra M, Huang Y, et al. Hypertension prevalence, awareness, treatment and control among older people in Latin America, India and China: a 10/66 cross-sectional population-based survey. J Hypertens. 2012;30:177–87.
Ogunsina K, Dibaba DT, Akinyemiju T. Association between life-course socio-economic status and prevalence of cardio-metabolic risk ractors in five middle-income countries. J Glob Health. 2018;8:2.
Bishwajit G. Nutrition transition in South Asia: the emergence of non-communicable chronic diseases. F1000Research. 2015;4:8.
Tripathy JP, Thakur JS, Jeet G, Chawla S, Jain S. Alarmingly high prevalence of hypertension and pre-hypertension in North India-results from a large cross-sectional STEPS survey. PLoS ONE. 2017;12:e0188619.
Mishra SR, Neupane D, Bhandari PM, Khanal V, Kallestrup P. Burgeoning burden of non-communicable diseases in Nepal: a scoping review. Glob Health. 2015;11:32.
Asian Development Bank. Poverty in Nepal: ADB. Mandaluyong, Philippines. https://www.adb.org/countries/nepal/poverty.
Allen L, Williams J, Townsend N, Mikkelsen B, Roberts N, Foster C, et al. Socioeconomic status and non-communicable disease behavioural risk factors in low-income and lower-middle-income countries: a systematic review. Lancet Glob Health. 2017;5:e277–e89.
Razak F, Subramanian S. Commentary: Socioeconomic status and hypertension in low-and middle-income countries: can we learn anything from existing studies? Int J Epidemiol. 2014;43:1577–81.
Xiaohui H. Urban-rural disparity of overweight, hypertension, undiagnosed hypertension, and untreated hypertension in China. Asia Pac J Public Health. 2008;20:159–69.
Zhai S, McGarvey ST. Temporal changes and rural-urban differences in cardiovascular disease risk factors and mortality in China. Hum Biol. 1992;64:807–19.
Acharya M, Acharya B, Sharma S. Women in Nepal: country briefing paper. Manila: Asian Development Bank; 1999.
Ghimire S, Shrestha N, Callahan K. Barriers to dietary salt reduction among hypertensive patients. J Nepal Health Res Counc. 2018;16:124–30.
Neupane D, Shrestha A, Mishra SR, Bloch J, Christensen B, McLachlan CS, et al. Awareness, prevalence, treatment, and control of hypertension in western Nepal. Am J Hypertens. 2017;30:907–13.
Karmacharya BM, Koju RP, LoGerfo JP, Chan KCG, Mokdad AH, Shrestha A, et al. Awareness, treatment and control of hypertension in Nepal: findings from the Dhulikhel Heart Study. Heart Asia. 2017;9:1–8.
Kathmandu Post. 744 new local units come into effect Kathmandu: Kathmandu Post; 2018. http://kathmandupost.ekantipur.com/news/2017-03-15/744-new-local-units-come-into-effect.html.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Mishra, S.R., Ghimire, S., Shrestha, N. et al. Socio-economic inequalities in hypertension burden and cascade of services: nationwide cross-sectional study in Nepal. J Hum Hypertens 33, 613–625 (2019). https://doi.org/10.1038/s41371-019-0165-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-019-0165-3
This article is cited by
-
Why is there a gap in self-rated health among people with hypertension in Zambia? A decomposition of determinants and rural‒urban differences
BMC Public Health (2024)
-
Cascade of diabetes care in Bangladesh, Bhutan and Nepal: identifying gaps in the screening, diagnosis, treatment and control continuum
Scientific Reports (2023)
-
Association of socio-demographic characteristics with hypertension awareness, treatment, and control in Bangladesh
Journal of Human Hypertension (2023)
-
Determinants affecting utilisation of health services and treatment for children under-5 in rural Nepali health centres: a cross-sectional study
BMC Public Health (2022)
-
An analytical model of population level uncontrolled hypertension management: a care cascade approach
Journal of Human Hypertension (2022)