Abstract
Objectives
To report how peak inflating pressure (PIP), tidal volume (VT) and low-tidal volume alarms are affected by maximum allowed inflating pressure (Pmax) during volume guarantee (VG) ventilation.
Study design
Ventilation data were analysed with 1 Hz sampling rate from 25 neonates receiving synchronised intermittent positive pressure ventilation with VG for >12 h.
Results
The difference between Pmax and PIP (Pdiff) ranged between 5 and 20 mbar (median = 11 mbar) despite a protocol to keep Pmax 5 mbar above the “working PIP”. Pmax was reached in 5.2% of inflations. Computational modelling demonstrated that had Pdiff been kept at 5 mbar more consistently, >10% of inflations would have reached Pmax. The frequency of low-tidal volume alarms showed inverse correlation with Pdiff.
Conclusions
It is difficult to implement a simple Pmax strategy due to variability of PIP. Setting Pmax close to the “working PIP” limits VT delivery and triggers frequent alarms.
Similar content being viewed by others
Introduction
Traditionally, ill neonates were ventilated using time cycled pressure-limited ventilation (TCPLV) [1]. However, if a constant peak inflating pressure (PIP) is used it will cause large tidal volumes when a baby takes a large breath or cries during an inflation, or the lung compliance improves [2]. To avoid large fluctuations in tidal volume, volume-targeted ventilation (VTV), also called volume guarantee (VG), is used. During VG ventilation a target tidal volume (VTset) is set, usually between 4 and 6 mL/kg. The ventilator then adjusts the PIP for each inflation to maintain the expired tidal volume (VTe) at a set level (VTset) [3]. A recent Cochrane review reported that VTV significantly reduces the rates of neonatal death and bronchopulmonary dysplasia, pneumothorax, hypocarbia, days of ventilation, periventricular leukomalacia with or without grade 3 or 4 intraventricular haemorrhage, compared with TCPLV without any obvious complications [4].
During VG a maximum inflating pressure (Pmax) is set to prevent the PIP going inadvertently high. If Pmax is set too low, it limits the PIP and tidal volume delivery and causes frequent “low-tidal volume” alarms [5]. If Pmax is set too high, there may be a delay in recognising important clinical events such as slippage of the endotracheal tube, significant air leak or change in the lung’s compliance. It has been recommended Pmax should initially be set about 5 mbar above the “working PIP” used to deliver VTset and if VTset is not reached Pmax should be increased in small steps [1]. In another review an initial Pmax of ~25–30 mbar was recommended with a later adjustment to at least 5–10 mbar above the “working PIP”, allowing the ventilator flexibility to deliver the target VTset during variable spontaneous breaths, changing endotracheal tube (ETT) leaks or untriggered inflations [3]. A problem with setting Pmax is that although there are data about accuracy of the delivered tidal volume during VG ventilation [2, 6, 7] details of how PIP varies as a baby breathes, cries, splints against an inflation, the ETT position, or leak around it, changes and the effect of the Pmax are unknown. It is also unclear how well a Pmax can be determined by observing the baby and ventilator because there are limited data about the variation in PIP during VG [2, 6].
In this study we investigated, (1) the variation in PIP; (2) the effect of setting the Pmax at different levels; and (3) how the difference between Pmax and the PIP affected the tidal volume and ventilator alarms.
Patients and methods
Patients
Ventilator data were collected as part of a service evaluation, authorised by the Research & Development Department of Cambridge University Hospitals (registration number: 4572). The primary purpose was to assess ventilator alarms. The need for an ethical review was waived. The findings have been published [8]. Data were collected anonymously from 60 infants ventilated with VN500 ventilators (Dräger, Lübeck, Germany) in the Rosie Hospital, Cambridge, between September 2015 and July 2016. The ventilator circuit used a Fisher and Paykel MR850 humidifier with Evaqua 2 circuit (Fisher & Paykel Healthcare, Auckland, New Zealand). For this study, recordings were only considered if synchronised intermittent positive pressure ventilation (SIPPV), also called assist control (AC) ventilation, was used with VG and leak-compensation continuously for at least 12 h. We excluded one where the baby received muscle relaxant. Altogether, 25 infants were included with different gestational ages and weights. (Table 1). Infants were ventilated for various problems including respiratory distress syndrome, sepsis, pneumothorax, patent ductus arteriosus, pulmonary haemorrhage, necrotising enterocolitis and intestinal obstruction. The local guideline recommends using 4–6 mL/kg tidal volume and to keep Pmax 5 mbar above the “working PIP”, but without specific instructions as to how to adjust it. The time for the pressure to reach PIP (slope time) was set at 0.08 s in all cases and the inspiratory time was 0.33 s or longer. Therefore, tidal volume delivery could not be limited by the inspiratory time only by Pmax.
Data retrieval and analysis
Ventilator data were downloaded to a laptop via a cable attached to one ventilator communication port using software developed by the Research & Development Department of Dräger. It is only for experimental and scientific purposes and not commercially available. It downloads flow and airway pressure data at 100 Hz and all other ventilator parameters at 1 Hz sampling rate. All data are time-stamped with millisecond precision. At each second the tidal volume and pressure are recorded for the last full inflation before the time-stamp. Changes in ventilator settings are all recorded. Alarms are recorded when triggered. Data are exported as comma-separated value (.csv) text files.
Data analysis used Python (version 3.5.3, https://www.python.org) and add-on packages. Anaconda (Continuum Analytics, http://docs.continuum.io/anaconda/pkg-docs) was installed on a MacBook Pro 2014 version, 2.6 GHz i5 processor and 8 Gb RAM memory. Programming was done using IPython Notebook (version 5.3.0 http://ipython.org/notebook.html). Data were represented, manipulated and analysed using the NumPy (version 1.12.1 http://www.numpy.org) and pandas (version 0.20.1 http://pandas.pydata.org). Statistical analysis was performed using SciPy (version 0.19.0, www.scipy.org). Visualisation used matplotlib (version 2.0.2, http://matplotlib.org). All the software is open-source and freely available. An IPython notebook containing and explaining all steps of data processing and statistical analysis can be viewed on GitHub code repository at https://github.com/belteki/Pmax.
Results
We analysed ventilator inflations from 25 neonates recorded continuously for >12 h. With SIPPV, most patient breaths trigger synchronised ventilator inflations. The median recording time was 50 h with a total of 60 ventilator days recorded. We collected data on >5 million inflations. For 1.7% of inflations data on one or more ventilator parameters were missing and for 0.09% the tidal volume was over 20 mL/kg or the respiratory rate was over 125/min. They likely represent an open circuit or flow sensor problem, so these data were excluded. Data about the set and delivered ventilation parameters are shown for each recording in Table 2 and Supplementary Table 1.
Variability of peak inflating pressure
In most recordings the PIP showed large breath-by-breath variability as it was changed by the VG algorithm in response to fluctuations in spontaneous tidal volumes, patient–ventilator interactions or variable ETT leak. Fig. 1a–f shows a recording where Pmax was set 5 mbar above “working pressure” (Supplementary Figures 1 and 2 show similar graphs as Fig. 1a, d, respectively, for all recordings). PIP frequently reached the set Pmax and the delivered VT was then limited. Pmax was between 20 and 30 mbar in eight recordings (32%), between 30 and 40 mbar in 14 recordings (56%) and >40 mbar in three recordings (12%). In some cases when Pmax was set at 40 mbar or higher, the working pressure was high and so the high Pmax was required; moreover, it was still frequently reached by the PIP (DG043, DG060, see Supplementary Figure 1). In other cases, the Pmax was set at >15 mbar above the usual PIP (e.g., DG027, DG051_1, and DG057). In recordings when PIP frequently reached Pmax, the median VT was significantly below the target value for longer periods (e.g., DG033 and DG060, Supplementary Figure 2).
Short- and long-term variability of PIP during SIPPV–VG ventilation shown for one baby. a Variability of PIP during VG ventilation. The ventilator was sampled with 1 Hz over a period of 38.5 h; therefore, this graph is based >130,000 data points but due to resolution of the image and the pressure measurements, not every data point is shown separately. The median PIP of this recording was 5 mbar below the Pmax. However, due its variability, the PIP frequently reached Pmax when inflation stopped and delivery of tidal volume could have been limited. b Variability of the mandatory leak-compensated tidal volume (VTmand) in the same recording, sampled with 1 Hz frequency. The target VT is also shown. The VTmand is highly variable and sometimes exceeds 10 mL/kg due to the infant making deep breaths. c Graph showing median of the PIP aggregated over 1-min periods. Each data point represents the median of 60 measurements taken at 1 Hz sampling rate, removing most of short-term variability. However, occasionally even the 1-min median values of PIP reached Pmax (arrows). d Graph showing median VTmand aggregated over 1-min periods. It shows that on average the VG delivered the set VT very well. When Pmax was reached tidal volume delivery was also limited. e 1-h medians of PIP demonstrate long-term changes in inflating pressure. Over a longer time, the median PIP remained well below the Pmax. f 1-h medians of VTmand. The long-term average of the tidal volume is very close to the targeted value
The median difference between Pmax and the actual PIP (Pdiff) ranged between 5 and 20 mbar in the individual recordings (group median = 11 mbar) despite the unit’s guideline to keep Pmax 5 mbar above the working PIP (Table 2). Overall, Pdiff was <10 mbar in 43.1% of inflations, <5 mbar in 16.1 % and the PIP reached Pmax in 5.2% (Fig. 2a). Therefore, despite keeping the Pmax > 10 mbar above PIP overall in most recordings, the PIP reached Pmax in many inflations. These data illustrate that due to large variation in PIP during VG ventilation it is not easy for clinicians to define a “working pressure” and use it to set the Pmax.
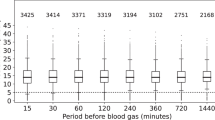
a Histogram showing the number of inflations for different levels of Pdiff (the difference between Pmax and PIP) in the >5 million inflations analysed in the 25 recordings. b Boxplot showing the distribution of VTdiff (the difference between the actual tidal volume and the set tidal volume) for inflations with different Pdiff (Pmax–PIP) ranges. Horizontal lines mark median values. Boxes represent interquartile ranges, error bars represent 5th and 95th centiles. Median VTdiff was close to zero for all ranges of Pdiff less than 20 mbar. c Histogram showing the number of inflations for different levels of VTdiff. The actual VT deviates from the targeted VT by less than 1 mL/kg in >80% of the inflations. d Boxplot showing the distribution of PIP for various levels of VTdiff. When VTdiff is large (the VT exceeds the targeted value), PIP is usually relatively low. See manuscript for more explanation. Horizontal lines mark median values. Boxes represent interquartile ranges, error bars represent 5th and 95th centiles
Effect of P max on tidal volume delivery and low-tidal volume alarms
The tidal volume varied from breath to breath as each baby breathed and the ventilator adjusted the PIP. However, when averaged over long periods, VT was very close to the set target: the median VTdiff (the difference between the actual and target tidal volume) was <0.5 mL/kg in each recording (Table 2). Tidal volume delivery was stable even when Pmax was substantially higher than the PIP: the median VTdiff was <0.1 mL/kg and VTdiff had similar variability for all ranges of Pdiff < 20 mbar. When Pdiff was >20 mbar, the median of VTdiff was still only 0.45 mL/kg, but its variability was larger (Fig. 2b). During inflations where the VT was larger than the VTset the PIP was relatively low (Fig. 2c, d), suggesting the large breaths were due to the baby actively breathing from the circuit and so the VG reduced the PIP.
When PIP reached the Pmax, VT was frequently lower than the target. The proportion of inflations where Pmax limited tidal volume delivery by >1 mL/kg varied between 0% and 8.5% in the recordings. The percentage of inflations limited by Pmax in each recording showed inverse correlation with the median Pdiff (Spearman’s correlation: r = −0.79, 95% confidence interval (CI): −0.91, −0.58, p < 0.001). During the recordings Pmax was changed infrequently (median = 0.65 times daily) and the frequency of changes was not closely related to the PIP variability.
The number of low-tidal volume alarms ranged between 0.1 and 22.5/h. Their frequency had a strong inverse correlation with Pdiff (r = −0.71, 95% CI: −0.86, −0.44, p < 0.001). Therefore, the lower the Pmax, the more inflations failed to reach the target tidal volume due to PIP being limited by Pmax, and more low-tidal volume alarms sounded.
How to set P max level and effect of how often to change it
We were interested in how the proportion of inflations reaching Pmax would be affected by the frequency of staff adjusting Pmax and also by the level Pmax was set above this observed PIP. To investigate this, we considered a range of scenarios for adjusting Pmax between 2-hourly to once a day. We also considered scenarios of Pmax being 5–15 mbar above the most frequently observed PIP (the statistical mode of PIP) over the observation period. These were modelled from our recordings by building 11 × 12 = 131 computational models and analysing how frequently Pmax would have been reached in each case. The results are shown on Fig. 3 and Supplementary Table 2. When Pmax was 5 mbar above the mode of PIP, Pmax limited >10% of the inflations. Increasing Pmax to 10 mbar above the mode of PIP reduced the number of such inflations. The number of inflations limited by Pmax did not change significantly whether the Pmax setting was adjusted 2 or 12 hourly. In other words, reviewing and adjusting Pmax more frequently would not have reduced the proportion of inflations when Pmax is reached.
A calculation of the percentage of inflations which would reach Pmax when it was set at 5, 10 or 15 mbar over the observed PIP and also the influence of changing the Pmax at different intervals between 2 and 24 h. Graph was produced by computational modelling using the collected ventilator data and hypothetical Pmax levels. See manuscript text for detailed explanation
Discussion
One decision when using VTV is to determine the Pmax setting. Our study of SIPPV–VG ventilation with the Dräger VN500 ventilator showed that PIP fluctuates significantly during VG as the babies breathe. Due to this variability the “working PIP” can be difficult to determine and a local protocol of keeping Pmax 5 mbar over the working PIP can be difficult to implement even if the Pmax is reviewed frequently. Moreover, we showed that if Pmax is set only 5 mbar above what is clinically considered to be the working PIP, delivery of tidal volume will be limited frequently and low-tidal volume alarms will be triggered. These effects can be considerably reduced by increasing the Pmax higher above the working PIP.
However, there are several concerns about keeping the Pmax at a higher level. Some clinicians are cautious because they are concerned about barotrauma. It is now considered that volutrauma and atelectotrauma are more damaging to the lungs than barotrauma and that a high PIP with a VT in the normal range is unlikely to injure the lungs [9,10,11,12,13,14]. With VG the PIP only increases when the VT is below the target. Our analysis showed that on average, the VT is very close to the target (within 0.1 mL/kg) even for those inflations when the Pmax is 15–20 mbar above actual PIP. In addition, during VG the VN500 ventilator has a safety programme which stops ventilator inflation immediately if the VTi is >130% of the target VT [1]. For these reasons, during VG a high PIP is very unlikely to cause a high-tidal volume. When the tidal volume does rise significantly above the target VT this is due to the baby actively taking a breath that is higher than VTset. When it happens during consecutive inflations, the VG protocol of the ventilator progressively reduces the PIP; therefore, most inflations with high-tidal volume are associated with low PIP not a high one [2, 3].
Another potential concern is that as VTV usually targets the expiratory tidal volume, if there is a large leak around the endotracheal tube the effective tidal volume (volume in the lungs at the end of inflation) will be somewhat larger than VTset due to the expiratory component of the leak [1]. Some clinicians may want to avoid this by keeping Pmax relatively low. However, this will result in frequent ventilator alarms as the PIP will quickly reach Pmax if VTe is below VTset due to excessive leak. In our study this was not a concern as we used the leak-compensated mode of the VN500 ventilator [15]. However, leak-compensated volume targeting may not be available on other ventilators or they may use different algorithms.
The most significant concern about setting the Pmax high is potentially delayed recognition of significant clinical events such as slippage of the endotracheal tube, pneumothorax or worsening lung compliance. The recommendation of keeping Pmax 5 mbar above working PIP is not based on safety studies or clinical evidence and in the absence of clinical outcomes our study also cannot make recommendations as to a particular Pmax level. There will always be a trade-off between potentially delayed recognition of clinical events on one side and limited tidal volume delivery and frequent alarms. Frequent alarms represent a clinical risk due to alarm fatigue [8] and staff failing to address the cause of the alarm. We suggest that Pmax level has to be determined by local protocol with consideration given to NICU setup, nurse numbers and usual patient population. Moreover, it is unlikely that one single recommendation would be ideal for all NICU patients as older preterm babies with evolving or established bronchopulmonary dysplasia are prone to splinting of the chest and have more variable PIP than preterm infants on the first couple days of life [3, 16, 17]. If PIP frequently reaches Pmax, clinicians should assess the baby and ventilator to see if there are correctable reasons for a high PIP. If no cause is found, other than very stiff lungs, then the Pmax can be increased.
The main strength of our study is we collected ventilation data at 1 Hz and analysed more than 5 million inflations. Previous studies presented much sparser data [2, 16, 18]. In addition, using computational modelling we were able to consider multiple scenarios with the Pmax set at different levels and reviewed with different frequencies.
Our study has several limitations. First, we studied retrospectively a convenience sample of infants with a wide range of gestations, weights and diagnoses. Secondly, we only collected ventilator data from the Dräger VN500 ventilator in SIPPV/AC mode using leak-compensated VG and our local protocol for setting the VT and Pmax. Other ventilators and other NICU protocols might find different effects. Finally, we did not study clinical outcomes. Further research with other ventilators and clinical outcomes are warranted to test the settings of Pmax on VG ventilation.
References
Keszler M, Abubakar KM. Volume guarantee ventilation. Clin Perinatol. 2007;34:107–16.
McCallion N, Lau R, Morley CJ, Dargaville PA. Neonatal volume guarantee ventilation: effects of spontaneous breathing, triggered and untriggered inflations. Arch Dis Child Fetal Neonatal Ed. 2008;93:F36–9.
Klingenberg C, Wheeler KI, Davis PG, Morley CJ. A practical guide to neonatal volume guarantee ventilation. J Perinatol. 2011;31:575–85.
Klingenberg C, Wheeler KI, McCallion N, Morley CJ, Davis PG. Volume-targeted versus pressure-limited ventilation in neonates. Cochrane Database Syst Rev. 2017;10:CD003666.
Belteki G and Morley CJ. Frequency, duration and cause of ventilator alarms on a neonatal intensive care unit. Arch Dis Child Fetal Neonatal Ed. 2018;103:F307–F311.
Keszler M, Abubakar K. Volume guarantee ventilation during surgical closure of patent ductus arteriosus. Am J Perinatol. 2015;32:23–6.
Farrell O, Perkins EJ, Black D, Miedema M, Paul JD, Pereira-Fantini PM, et al. Volume guaranteed? Accuracy of a volume-targeted ventilation mode in infants. Arch Dis Child Fetal Neonatal Ed. 2018;103:F120–F125.
Belteki G, Morley CJ. Frequency, duration and cause of ventilator alarms on a neonatal intensive care unit. Arch Dis Child Fetal Neonatal Ed. 2018;103:F307–F311.
Slutsky AS. Ventilator-induced lung injury: from barotrauma to biotrauma. Respir Care. 2005;50:646–59.
Lista G, Colnaghi M, Castoldi F, Condo V, Reali R, Compagnoni G, et al. Impact of targeted-volume ventilation on lung inflammatory response in preterm infants with respiratory distress syndrome (RDS). Pediatr Pulmonol. 2004;37:510–4.
Bjorklund LJ, Ingimarsson J, Curstedt T, John J, Robertson B, Werner O, et al. Manual ventilation with a few large breaths at birth compromises the therapeutic effect of subsequent surfactant replacement in immature lambs. Pediatr Res. 1997;42:348–55.
Hernandez LA, Peevy KJ, Moise AA, Parker JC. Chest wall restriction limits high airway pressure-induced lung injury in young rabbits. J Appl Physiol (1985). 1989;66:2364–8.
Dreyfuss D, Saumon G. Role of tidal volume, FRC, and end-inspiratory volume in the development of pulmonary edema following mechanical ventilation. Am Rev Respir Dis. 1993;148:1194–203.
Dreyfuss D, Saumon G. Ventilator-induced lung injury: lessons from experimental studies. Am J Respir Crit Care Med. 1998;157:294–323.
Szakmar E, Morley CJ, Belteki G. Leak compensation during volume guarantee with the Drager Babylog VN500 Neonatal Ventilator. Pediatr Crit Care Med. 2018. https://doi.org/10.1097/PCC.0000000000001638.
Keszler M, Nassabeh-Montazami S, Abubakar K. Evolution of tidal volume requirement during the first 3 weeks of life in infants <800 g ventilated with volume guarantee. Arch Dis Child Fetal Neonatal Ed. 2009;94:F279–82.
Keszler M, Sant’Anna G. Mechanical ventilation and bronchopulmonary dysplasia. Clin Perinatol. 2015;42:781–96.
Abubakar KM, Keszler M. Patient–ventilator interactions in new modes of patient-triggered ventilation. Pediatr Pulmonol. 2001;32:71–5.
Acknowledgements
We thank Thomas Krueger, Kreske Brunckhorst and the engineers of Dräger Medical for help with exporting from the ventilator and Dr. Amanda Ogilvy-Stuart for critically reading our manuscript.
Funding
The authors have no funding sources relevant to this article to disclose.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Szakmar, E., Morley, C.J. & Belteki, G. Analysis of peak inflating pressure and inflating pressure limit during neonatal volume guaranteed ventilation. J Perinatol 39, 72–79 (2019). https://doi.org/10.1038/s41372-018-0228-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-018-0228-2