Abstract
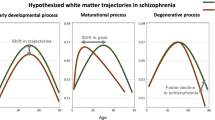
Subtle alterations in white matter microstructure are observed in youth at clinical high risk (CHR) for psychosis. However, the timing of these changes and their relationships to the emergence of psychosis remain unclear. Here, we track the evolution of white matter abnormalities in a large, longitudinal cohort of CHR individuals comprising the North American Prodrome Longitudinal Study (NAPLS-3). Multi-shell diffusion magnetic resonance imaging data were collected across multiple timepoints (1–5 over 1 year) in 286 subjects (aged 12–32 years): 25 CHR individuals who transitioned to psychosis (CHR-P; 61 scans), 205 CHR subjects with unknown transition outcome after the 1-year follow-up period (CHR-U; 596 scans), and 56 healthy controls (195 scans). Linear mixed effects models were fitted to infer the impact of age and illness-onset on variation in the fractional anisotropy of cellular tissue (FAT) and the volume fraction of extracellular free water (FW). Baseline measures of white matter microstructure did not differentiate between HC, CHR-U and CHR-P individuals. However, age trajectories differed between the three groups in line with a developmental effect: CHR-P and CHR-U groups displayed higher FAT in adolescence, and 4% lower FAT by 30 years of age compared to controls. Furthermore, older CHR-P subjects (20+ years) displayed 4% higher FW in the forceps major (p < 0.05). Prospective analysis in CHR-P did not reveal a significant impact of illness onset on regional FAT or FW, suggesting that transition to psychosis is not marked by dramatic change in white matter microstructure. Instead, clinical high risk for psychosis—regardless of transition outcome—is characterized by subtle age-related white matter changes that occur in tandem with development.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Code availability
The Matlab function fitlme was used to perform linear mixed effects (LME) models with bootstrapping confidence intervals. This code is publicly accessible.
References
Di Biase MA, Pantelis C, Zalesky A White Matter Pathology in Schizophrenia. Neuroimaging in Schizophrenia. Springer2020, pp 71-91.
Saito J, Hori M, Nemoto T, Katagiri N, Shimoji K, Ito S, et al. Longitudinal study examining abnormal white matter integrity using a tract‐specific analysis in individuals with a high risk for psychosis. Psychiatry Clin Neurosci. 2017;71:530–541.
Tomyshev AS, Lebedeva IS, Akhadov TA, Omelchenko MA, Rumyantsev AO, Kaleda VG. Alterations in white matter microstructure and cortical thickness in individuals at ultra-high risk of psychosis: A multimodal tractography and surface-based morphometry study. Psychiatry Res: Neuroimaging. 2019;289:26–36.
Peters B, Schmitz N, Dingemans P, Van Amelsvoort T, Linszen D, De Haan L, et al. Preliminary evidence for reduced frontal white matter integrity in subjects at ultra-high-risk for psychosis. Schizophrenia Res. 2009;111:192–193.
Cho KIK, Shenton ME, Kubicki M, Jung WH, Lee TY, Yun J-Y, et al. Altered thalamo-cortical white matter connectivity: Probabilistic tractography study in clinical-high risk for psychosis and first-episode psychosis. Schizophrenia Bull. 2016;42:723–731.
Karlsgodt KH, Niendam TA, Bearden CE, Cannon TD. White matter integrity and prediction of social and role functioning in subjects at ultra-high risk for psychosis. Biol psychiatry. 2009;66:562–569.
Wang C, Ji F, Hong Z, Poh J, Krishnan R, Lee J, et al. Disrupted salience network functional connectivity and white-matter microstructure in persons at risk for psychosis: findings from the LYRIKS study. Psychological Med. 2016;46:2771–2783.
Epstein KA, Cullen KR, Mueller BA, Robinson P, Lee S, Kumra S. White matter abnormalities and cognitive impairment in early-onset schizophrenia-spectrum disorders. J Am Acad Child Adolesc Psychiatry. 2014;53:362–372. e361-362
Katagiri N, Pantelis C, Nemoto T, Zalesky A, Hori M, Shimoji K, et al. A longitudinal study investigating sub-threshold symptoms and white matter changes in individuals with an ‘at risk mental state’(ARMS). Schizophrenia Res. 2015;162:7–13.
Fitzsimmons J, Rosa P, Sydnor VJ, Reid BE, Makris N, Goldstein JM, et al. Cingulum bundle abnormalities and risk for schizophrenia. Schizophrenia Res. 2020;215:385–391.
Krakauer K, Nordentoft M, Glenthøj B, Raghava J, Nordholm D, Randers L, et al. White matter maturation during 12 months in individuals at ultra‐high‐risk for psychosis. Acta Psychiatr Scandinavica. 2018;137:65–78.
Kristensen TD, Mandl RC, Raghava JM, Jessen K, Jepsen JRM, Fagerlund B, et al. Widespread higher fractional anisotropy associates to better cognitive functions in individuals at ultra‐high risk for psychosis. Hum brain Mapp. 2019;40:5185–5201.
Tomyshev A, Lebedeva I, Akhadov T, Omel’chenko M, Ublinskii M, Semenova N, et al. MRI study for the features of brain conduction pathways in patients with an ultra-high risk of endogenous psychoses. Bull Exp Biol Med. 2017;162:425–429.
Peters BD, de Haan L, Dekker N, Blaas J, Becker HE, Dingemans PM, et al. White matter fibertracking in first-episode schizophrenia, schizoaffective patients and subjects at ultra-high risk of psychosis. Neuropsychobiology. 2008;58:19–28.
Peters BD, Dingemans PM, Dekker N, Blaas J, Akkerman E, van Amelsvoort TA, et al. White matter connectivity and psychosis in ultra-high-risk subjects: a diffusion tensor fiber tracking study. Psychiatry Res. 2010;181:44–50.
Schmidt A, Lenz C, Smieskova R, Harrisberger F, Walter A, Riecher-Rössler A, et al. Brain diffusion changes in emerging psychosis and the impact of state-dependent psychopathology. Neurosignals. 2015;23:71–83.
Fusar-Poli P, Cappucciati M, Borgwardt S, Woods SW, Addington J, Nelson B, et al. Heterogeneity of psychosis risk within individuals at clinical high risk: a meta-analytical stratification. JAMA psychiatry. 2016;73:113–120.
Chung Y, Cannon TD. Brain imaging during the transition from psychosis prodrome to schizophrenia. J Nerv Ment Dis. 2015;203:336–341.
Takahashi T, Wood SJ, Yung AR, Soulsby B, McGorry PD, Suzuki M, et al. Progressive gray matter reduction of the superior temporal gyrus during transition to psychosis. Arch Gen Psychiatry. 2009;66:366–376.
Cannon TD, Chung Y, He G, Sun D, Jacobson A, van Erp TGM, et al. Progressive reduction in cortical thickness as psychosis develops: a multisite longitudinal neuroimaging study of youth at elevated clinical risk. Biol psychiatry. 2015;77:147–157.
Pantelis C, Velakoulis D, McGorry PD, Wood SJ, Suckling J, Phillips LJ, et al. Neuroanatomical abnormalities before and after onset of psychosis: a cross-sectional and longitudinal MRI comparison. Lancet. 2003;361:281–288.
Takahashi T, Wood SJ, Yung AR, Phillips LJ, Soulsby B, McGorry PD, et al. Insular cortex gray matter changes in individuals at ultra-high-risk of developing psychosis. Schizophrenia Res. 2009;111:94–102.
Ziermans TB, Schothorst PF, Schnack HG, Koolschijn PCM, Kahn RS, van Engeland H, et al. Progressive structural brain changes during development of psychosis. Schizophrenia Bull. 2012;38:519–530.
Borgwardt SJ, McGuire PK, Aston J, Gschwandtner U, Pflüger MO, Stieglitz R-D, et al. Reductions in frontal, temporal and parietal volume associated with the onset of psychosis. Schizophrenia Res. 2008;106:108–114.
Walter A, Studerus E, Smieskova R, Kuster P, Aston J, Lang UE, et al. Hippocampal volume in subjects at high risk of psychosis: a longitudinal MRI study. Schizophrenia Res. 2012;142:217–222.
Sun D, Phillips L, Velakoulis D, Yung A, McGorry PD, Wood SJ, et al. Progressive brain structural changes mapped as psychosis develops in ‘at risk’individuals. Schizophrenia Res. 2009;108:85–92.
Chung Y, Addington J, Bearden CE, Cadenhead K, Cornblatt B, Mathalon DH, et al. Use of machine learning to determine deviance in neuroanatomical maturity associated with future psychosis in youths at clinically high risk. JAMA psychiatry. 2018;75:960–968.
Carletti F, Woolley JB, Bhattacharyya S, Perez-Iglesias R, Fusar Poli P, Valmaggia L, et al. Alterations in white matter evident before the onset of psychosis. Schizophrenia Bull. 2012;38:1170–1179.
Rigucci S, Santi G, Corigliano V, Imola A, Rossi-Espagnet C, Mancinelli I, et al. White matter microstructure in ultra-high risk and first episode schizophrenia: a prospective study. Psychiatry Res: Neuroimaging. 2016;247:42–48.
Peters BD, Szeszko PR, Radua J, Ikuta T, Gruner P, DeRosse P, et al. White matter development in adolescence: diffusion tensor imaging and meta-analytic results. Schizophrenia Bull. 2012;38:1308–1317.
Lebel C, Beaulieu C. Longitudinal development of human brain wiring continues from childhood into adulthood. J Neurosci. 2011;31:10937–10947.
Takahashi N, Sakurai T, Davis KL, Buxbaum JD. Linking oligodendrocyte and myelin dysfunction to neurocircuitry abnormalities in schizophrenia. Prog Neurobiol. 2011;93:13–24.
Roussos P, Haroutunian V Schizophrenia: susceptibility genes and oligodendroglial and myelin related abnormalities. Front Cell Neurosci. 2014;8:1–7.
Karayumak SC, Bouix S, Ning L, James A, Crow T, Shenton M, et al. Retrospective harmonization of multi-site diffusion MRI data acquired with different acquisition parameters. NeuroImage. 2019;184:180–200.
Cropley VL, Klauser P, Lenroot RK, Bruggemann J, Sundram S, Bousman C, et al. Accelerated gray and white matter deterioration with age in schizophrenia. Am J Psychiatry. 2016;174:286–295.
Di Biase MA, Cropley VL, Cocchi L, Fornito A, Calamante F, Ganella EP et al. Linking cortical and connectional pathology in schizophrenia. Schizophrenia Bull. 2018; sby121.
Pasternak O, Sochen N, Gur Y, Intrator N, Assaf Y. Free water elimination and mapping from diffusion MRI. Magn Reson Med. 2009;62:717–730.
Addington J, Liu L, Brummitt K, Bearden CE, Cadenhead KS, Cornblatt BA et al. North American Prodrome Longitudinal Study (NAPLS 3): methods and baseline description. Schizophrenia Res. 2020. In Press.
McGlashan T, Walsh B, Woods S The psychosis-risk syndrome: handbook for diagnosis and follow-up. USA: Oxford University Press 2010.
Miller TJ, McGlashan TH, Rosen JL, Cadenhead K, Ventura J, McFarlane W, et al. Prodromal assessment with the structured interview for prodromal syndromes and the scale of prodromal symptoms: predictive validity, interrater reliability, and training to reliability. Schizophrenia Bull. 2003;29:703–715.
First MB, Gibbon M The Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I) and the Structured Clinical Interview for DSM-IV Axis II Disorders (SCID-II). In: Hersen M, Haynes SN, Goldstein G, Heiby EM, Hilsenroth MJ, Beers SR et al. (eds). Comprehensive Handbook of Psychological Assessment, vol. 2: Personality Assessment. John Wiley & Sons Inc: New Jersey, 2004, pp 134-143.
Ning L, Bonet-Carne E, Grussu F, Sepehrband F, Kaden E, Veraart J, et al. Cross-scanner and cross-protocol multi-shell diffusion MRI data harmonization: Algorithms and results. NeuroImage. 2020;221:117128.
Jenkinson M, Beckmann CF, Behrens TE, Woolrich MW, Smith SM. Fsl. NeuroImage. 2012;62:782–790.
Andersson JL, Sotiropoulos SN. An integrated approach to correction for off-resonance effects and subject movement in diffusion MR imaging. NeuroImage. 2016;125:1063–1078.
Andersson JL, Graham MS, Zsoldos E, Sotiropoulos SN. Incorporating outlier detection and replacement into a non-parametric framework for movement and distortion correction of diffusion MR images. NeuroImage. 2016;141:556–572.
Jahanshad N, Kochunov PV, Sprooten E, Mandl RC, Nichols TE, Almasy L, et al. Multi-site genetic analysis of diffusion images and voxelwise heritability analysis: a pilot project of the ENIGMA-DTI working group. NeuroImage. 2013;81:455–469.
Avants BB, Epstein CL, Grossman M, Gee JC. Symmetric diffeomorphic image registration with cross-correlation: evaluating automated labeling of elderly and neurodegenerative brain. Med image Anal. 2008;12:26–41.
Smith SM, Jenkinson M, Johansen-Berg H, Rueckert D, Nichols TE, Mackay CE, et al. Tract-based spatial statistics: voxelwise analysis of multi-subject diffusion data. NeuroImage. 2006;31:1487–1505.
Ilin A, Raiko T. Practical approaches to principal component analysis in the presence of missing values. J Mach Learn Res. 2010;11:1957–2000.
Winkler AM, Ridgway GR, Webster MA, Smith SM, Nichols TE. Permutation inference for the general linear model. NeuroImage. 2014;92:381–397.
Smith SM Nichols TE. Threshold-free cluster enhancement: addressing problems of smoothing, threshold dependence and localisation in cluster inference. NeuroImage. 2009;44:83–98.
Smith SM, Nichols TE, Vidaurre D, Winkler AM, Behrens TE, Glasser MF, et al. A positive-negative mode of population covariation links brain connectivity, demographics and behavior. Nat Neurosci. 2015;18:1565–1567.
Taquet M, Smith SM, Prohl AK, Peters JM, Warfield SK, Scherrer B et al. A structural brain network of genetic vulnerability to psychiatric illness. Molecular Psychiatry. 2020: 1–12.
Dev SI, Nguyen TT, McKenna BS, Sutherland AN, Bartsch H, Theilmann RJ, et al. Steeper slope of age-related changes in white matter microstructure and processing speed in bipolar disorder. Am J Geriatr Psychiatry. 2017;25:744–752.
van Velzen LS, Kelly S, Isaev D, Aleman A, Aftanas LI, Bauer J, et al. White matter disturbances in major depressive disorder: a coordinated analysis across 20 international cohorts in the ENIGMA MDD working group. Mol Psychiatry. 2020;25:1511–1525.
Hawco C, Voineskos AN, Radhu N, Rotenberg D, Ameis S, Backhouse FA, et al. Age and gender interactions in white matter of schizophrenia and obsessive compulsive disorder compared to non-psychiatric controls: commonalities across disorders. Brain imaging Behav. 2017;11:1836–1848.
Yeatman JD, Wandell BA, Mezer AA. Lifespan maturation and degeneration of human brain white matter. Nat Commun. 2014;5:4932–4932.
Miller EK, Cohen JD. An integrative theory of prefrontal cortex function. Annu Rev Neurosci. 2001;24:167–202.
Nakajima R, Kinoshita M, Shinohara H, Nakada M. The superior longitudinal fascicle: reconsidering the fronto-parietal neural network based on anatomy and function. Brain imaging Behav. 2020;14:2817–2830.
Barbu MC, Spiliopoulou A, Colombo M, McKeigue P, Clarke T-K, Howard DM, et al. Expression quantitative trait loci-derived scores and white matter microstructure in UK Biobank: a novel approach to integrating genetics and neuroimaging. Trans Psychiatry. 2020;10:55.
Tomassy GS, Dershowitz LB, Arlotta P. Diversity matters: a revised guide to myelination. Trends Cell Biol. 2016;26:135–147.
Di Biase MA, Zhang F, Lyall A, Kubicki M, Mandl RC, Sommer IE et al. Neuroimaging auditory verbal hallucinations in schizophrenia patient and healthy populations. Psychological Med. 2019: 1–10.
Tang Y, Pasternak O, Kubicki M, Rathi Y, Zhang T, Wang J, et al. Altered cellular white matter but not extracellular free water on diffusion MRI in individuals at clinical high risk for psychosis. Am J Psychiatry. 2019;176:820–828.
Becker MP, Collins PF, Lim KO, Muetzel RL, Luciana M. Longitudinal changes in white matter microstructure after heavy cannabis use. Dev Cogn Neurosci. 2015;16:23–35.
McGorry PD, Hartmann JA, Spooner R, Nelson B. Beyond the “at risk mental state” concept: transitioning to transdiagnostic psychiatry. World Psychiatry. 2018;17:133–142.
Woods SW, Powers AR III, Taylor JH, Davidson CA, Johannesen JK, Addington J, et al. Lack of diagnostic pluripotentiality in patients at clinical high risk for psychosis: specificity of comorbidity persistence and search for pluripotential subgroups. Schizophrenia Bull. 2018;44:254–263.
Fusar-Poli P, Rutigliano G, Stahl D, Davies C, De Micheli A, Ramella-Cravaro V, et al. Long-term validity of the at risk mental state (ARMS) for predicting psychotic and non-psychotic mental disorders. Eur Psychiatry. 2017;42:49–54.
Webb JR, Addington J, Perkins DO, Bearden CE, Cadenhead KS, Cannon TD, et al. Specificity of incident diagnostic outcomes in patients at clinical high risk for psychosis. Schizophrenia Bull. 2015;41:1066–1075.
Acknowledgements
MADB was supported by an Australian National Health and Medical Research Council (NHMRC) Investigator Grant (1175754). This study was supported by a National Alliance for Research on Schizophrenia & Depression (NARSAD) Brain and Behavior Research Foundation Young Investigator Award (to AEL) and by the National Institute of Mental Health (grant K01 MH115247-01A1 to AEL; grants R01MH108574, R01MH102377, R01MH074794, P41EB015902 to OP; grant U01MH081984 to JA; grant U01MH081928 to WSS; grant U01MH081944 to KSC; grant U01MH081902 to TDC and CEB; grant U01MH082004 to DOP; grant U01MH082022 to SWW; grant U01MH076989 to DHM; grant U01MH081857 to BAC; and, grant U01MH109977 to MES).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Di Biase, M.A., Cetin-Karayumak, S., Lyall, A.E. et al. White matter changes in psychosis risk relate to development and are not impacted by the transition to psychosis. Mol Psychiatry 26, 6833–6844 (2021). https://doi.org/10.1038/s41380-021-01128-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41380-021-01128-8
This article is cited by
-
Baseline symptom-related white matter tracts predict individualized treatment response to 12-week antipsychotic monotherapies in first-episode schizophrenia
Translational Psychiatry (2024)
-
Matrix metalloproteinase 9 (MMP-9) activity, hippocampal extracellular free water, and cognitive deficits are associated with each other in early phase psychosis
Neuropsychopharmacology (2024)
-
Psychosis spectrum illnesses as disorders of prefrontal critical period plasticity
Neuropsychopharmacology (2023)
-
Age-associated alterations in thalamocortical structural connectivity in youths with a psychosis-spectrum disorder
Schizophrenia (2023)
-
Characterization of the extracellular free water signal in schizophrenia using multi-site diffusion MRI harmonization
Molecular Psychiatry (2023)