Abstract
Background
Bronchiolitis is the main cause of hospitalization of children younger than 1 year; however, the immune mechanism of bronchiolitis is not completely understood. The aim of this study was to analyze the recovery of immune response after a bronchiolitis episode.
Methods
Forty-nine infants hospitalized with bronchiolitis diagnosis were enrolled. Nasopharyngeal aspirates (NPAs) were processed. Twenty-seven pro-inflammatory biomarkers linked to innate immunity, inflammation, and epithelial damage, as well as nitrites and lipid mediators, were evaluated in the NPA supernatant by ELISA (enzyme-linked immunosorbent assay) and Luminex. Also, 11 genes were analyzed in NPA cells by quantitative PCR.
Results
A widespread statistically significant decline of multiple pro-inflammatory parameters and cytokines were detected in the recovery period after respiratory infection: interferon-α2 (IFNα2), IFNγ, interleukin-10 (IL-10), IL-1β, IL-8, IFN-γ-inducible protein-10, vascular endothelial growth factor, monocyte chemoattractant protein-1, macrophage inflammatory protein-1α (MIP-1α), and MIP-1β. Supporting these results, a decreased nuclear factor-κB gene expression was observed (P = 0.0116). A significant diminution of cysteinyl leukotriene C4 (LTC4) soluble levels (P = 0.0319) and cyclooxygenase-2 (COX-2) gene expression were observed in the recovery sample. In children classified by post-bronchiolitis wheezing, LTC4 remains elevated in the NPA supernatant.
Conclusions
After bronchiolitis, cytokines and biomarkers linked to innate immune response in NPA decrease significantly in the recovery period accompanied by a drop in LTC4 levels; however, this reduction was lower in infants with post-bronchiolitis wheezing.
Similar content being viewed by others
Introduction
Bronchiolitis is one of the most common causes of hospitalization during early infancy; it places a great social and economic burden on healthcare systems and could be responsible for respiratory sequelae.1 This disease is most frequently caused by the respiratory syncytial virus (RSV),2 but rhinovirus (HRV) and others such as human bocavirus (HBoV), adenovirus (ADV), and human metapneumovirus (hMPV) have also been identified as etiologic agents.3
Bronchiolitis usually manifests as rhinitis, followed by airway obstruction with crackles on auscultation and wheezing.4 Hypoxia is one of the main signals of severity.5 The disease is characterized by airway inflammation, increased mucus production, and, sometimes, necrosis of airway epithelial cells.6 The disease is manageable with supportive measures, including oxygen supplementation and administration of fluids.2,3,4,5,6,7 Palivizumab was developed for prophylaxis of RSV-induced bronchiolitis; in spite of its ability to reduce hospitalizations, this treatment is only recommended in infants with risk factors due to its substantial cost.8
For a long time, acute and severe bronchiolitis presenting in early infancy has been associated with the development of respiratory events, such as recurrent wheezing or asthma during childhood;9 however, the immune mechanisms associated with these respiratory disorders remain unknown. In a previous study, we evaluated specific cytokines and parameters linked to T-helper type 2 (Th2) immune response in a bronchiolitis-diagnosed population, suggesting that respiratory viruses might shift immune responses toward Th2 in early life.10
The main purpose of this prospective study was to analyze the evolution of innate and adaptive immune response following an acute episode of bronchiolitis.
Methods
Study design and clinical assessment
This prospective single-site recruitment study was conducted at the secondary public Severo Ochoa Hospital (Leganés, Madrid, Spain). The study population comprises infants younger than 24 months admitted with a diagnosis of bronchiolitis between October 2016 and June 2017. Thus, we enrolled infants <23 months hospitalized with bronchiolitis, which is defined as the initial episode of acute-onset expiratory dyspnea with signs of upper respiratory infection.7 Infants with infiltrates confirmed by chest x-rays without wheezing were defined as pneumonia and they were excluded. Signed informed consent was obtained from the parents or legal guardians, and the study protocol was approved by the Ethics Committee of the Severo Ochoa Hospital, Alfonso X El Sabio University. The study was conducted in accordance with the principles set forth in the Declaration of Helsinki.
During the hospital stay, in the acute episode of bronchiolitis, a nasopharyngeal aspirate (NPA) sample was obtained, and a study questionnaire was filled out by a physician, providing information on clinical and epidemiological variables, family history of asthma and atopic diseases, second-hand smoking, and relation to hospital admission, such as axillary temperature, administration of antibiotic therapy, or need for oxygen supplementation. Disease severity was assessed by need for supplemental oxygen, length of oxygen administration and hospitalization, and intensive care unit (ICU) admission.
Patients were evaluated in a second visit within 2 or 3 months after discharge (recovery period defined as negative viral determination and lack of symptoms) in which a second NPA sample was collected (follow-up sample [FUS]). Moreover, 1 year after an acute episode of bronchiolitis, children were clinically evaluated by a physician who completed a questionnaire on symptoms, exacerbations of respiratory disease (episodes of recurrent wheezing), use of medication, and need for hospitalization.
Sample collection
NPA is a noninvasive method that is very useful in infants. Thus, NPAs were collected at two different time points: at the onset of admission and on the second visit 2–3 months after discharge. In each time point two samples were collected. Samples were obtained in accordance with a standard, routine clinical technique and it is performed by specifically trained staff. Briefly, it consists of washing each nasal cavity with 1 mL of phosphate-buffered saline, and then collecting the sample with a standard mucus extractor.10 At each time point (admission and second visit [FUS]), one of the two samples collected was sent for virology determination to the Respiratory Virus and Influenza Unit at the National Microbiology Center (ISCIII, Madrid, Spain); the other sample was used for immunological testing at the Immunology Department of IIS-Fundación Jiménez Díaz. Samples were processed within 24 h of collection.
NPA processing
For immunological analysis, NPA was filtrated with a 40-µm nylon filter. Then, it was centrifuged, and two phases were obtained: cellular pellet and supernatant. After cellular counting, the pellet was resuspended in 0.7 mL of Qiazol Lysis Reagent (Qiagen, Hilden, Germany) and frozen at –80 °C. The supernatants were directly frozen at –80 °C.
Virus detection
Detection of 16 respiratory viruses was performed as previously described.10 Briefly, these viruses were detected through three RT-nested PCR assays. Influenza A, B, and C viruses were detected in a multiplex PCR assay; a second multiplex PCR was employed to detect parainfluenza viruses, human coronaviruses, enteroviruses, and HRV. In a third multiplex RT-nested PCR-BRQ method, RSV, hMPV, hBoV, and ADV were analyzed.
Immunological analyses in NPA
Total RNA was purified from NPA cellular pellets by using the Chomczynski method.11 RNA was quantified, and 0.5 μg of RNA was reverse-transcribed into complementary DNA. Several genes were evaluated by semiquantitative real-time PCRs (qRT-PCR) on a 7500 Real-Time PCR system (Applied Biosystems). We used specific TaqMan gene expression assay probes for TSLP, IL33, IFNG, IL10, FLG, AREG, IL13, TLR3, IL1RL1, NFKB2, and COX-2 (PTGS2). GAPDH and 18s were chosen as housekeeping genes; 18s was selected due to its stability in the sample, as analyzed in this study. All genes were examined for their relative expression by using the cycle threshold (Ct) value, using the 2−ΔΔCt method.12 The relative gene expression was calculated following these parameters: ΔCt and ΔΔCt, where ΔCt = Cttarget − Ct18s (housekeeping). The fold change for the recovery period was defined as the relative expression compared with the corresponding control, using in this case the value during the acute episode of bronchiolitis like reference or control. It was calculated as follows: 2−ΔΔCt, where ΔΔCt = ΔCtFUS − ΔCtbronchiolitis.
In the NPA supernatant, several cytokines and biomarkers were evaluated. Twenty-four cytokines and chemokines were determined by using a commercially available panel focusing on inflammation, cellular recruitment, and immune response: tumor growth factor-β1 (TGF-β1), interleukin-33 (IL-33), IL-25, epidermal growth factor (EGF), fibroblast growth factor-2 (FGF-2), granulocyte–macrophage colony-stimulating factor (GM-CSF), IFN-α2, IFNγ, IL-10, IL12p70, IL-13, soluble CD40 ligand (sCD40L), IL-17A, IL-9, IL-1β, IL-2, IL-4, IL-5, IL-8, IFN-γ-inducible protein-10 (IP-10), monocyte chemoattractant protein-1 (MCP-1), macrophage inflammatory protein-1α (MIP-1α), MIP-1β, and vascular endothelial growth factor (VEGF). Supernatants of bronchiolitis concentrations were measured, and the samples were followed up according to the manufacturer’s instructions (Magpix, Merck Millipore, Massachusetts). Periostin, TSLP, and ST-2 (IL-33 receptor) were analyzed by ELISA Kit (R&D Systems, Abingdon, UK). The lower detection limit of these assays was between 31 and 62 pg/mL. The intra- and inter-assay coefficients of variation for periostin were 2.19% and 9.99%, and 8.2% and 7.47% for TSLP.
Determination of nitric oxide
Nitrite determination was developed in the supernatant of NPAs by using Total Nitric Oxide and Nitrate/Nitrite Parameter Assay Kit (R&D System, Minneapolis). Endogenous nitrates were reduced to nitrites, and this value was subtracted from the nitrite value.
Arachidonic acid pathway
Prostaglandin E2 (PGE2) and cysteinyl leukotrienes, especially leukotriene C4 (LTC4), were evaluated in the NPA supernatant of samples by using ELISA (Enzo, New York, NY) following the manufacturer’s instructions.
Statistical analysis
Values are expressed as percentages for discrete variables, or as mean and standard deviation, or median and interquartile range or SEM for continuous variables. Comparisons used either X2 or Fisher’s exact test (two-tailed) for categorical variables, and the Mann–Whitney U test for continuous and non-Gaussian variables. Correlations were determined by using Pearson’s or Spearman’s rank-correlation coefficients. Ninety-five percent confidence interval values were also computed, and a probability of P < 0.05 was considered significant. All analyses were performed by using the Statistical Package for the Social Sciences (SPSS), Version 21.0 (IBM Corp., Armonk, NY) and GraphPad Prism 6 (GraphPad Software Inc., San Diego, CA).
Results
Clinical and epidemiological characteristics of the study population
The original population consisted of 99 children with a diagnosis of bronchiolitis; however, only 49 of them attended to the scheduled follow-up visits (2–3 months and 1 year after acute episode of bronchiolitis). For this reason, the final population of this study comprises 49 infants with bronchiolitis diagnosis. Most of them (70%) had a positive respiratory viral detection during acute bronchiolitis episode. RSV was the most frequent virus implicated (65.71%), followed by HRV (42.86%). Other viruses such as ADV, hMPV, or hBoV were identified in some of the remaining infants. In total, 34.29% of infants were co-infected (Table 1).
The median age at admission was 3 months. There was no significant predominance of males (63.26%). A high percentage presented hypoxia, and 18 infants (36%) needed high-flow oxygen and/or ICU admission (Table 1). Seven patients (14%) were born prematurely. None of them developed bronchopulmonary dysplasia. There was no other comorbidity.
Both FUSs, which were collected 2–3 months after acute bronchiolitis episode, were used for immunological analysis and viral detection, showing that all of them were a negative result to viral presence. No respiratory infection was recorded between the initial sample (collected at bronchiolitis time point) and the second sampling (2–3 months after bronchiolitis episode [FUS]) in any of the children included in the study.
During the clinical visit 1 year after discharge, we found that 19 children (38.8%) had experienced at least one episode of wheezing requiring bronchodilator treatment. Of them, seven infants were prescribed inhaled corticosteroids, and two infants (10.53%) needed hospitalization for recurrent wheezing. Seven infants were born prematurely and all of them developed recurrent wheezing in the 12 months after admission for bronchiolitis (Table 1). No atopy history was associated with these cases of post-bronchiolitis wheezing.
Nasal cytokine and chemokine determination by ELISA, Luminex technology, and qRT-PCR
A total of 27 cytokines, chemokines, and other biomarkers were evaluated in NPA from acute episode (basal sample) and from the FUS (second visit 2–3 months after the acute episode) of 49 infants included in the study.
We observed an overall decrease in the levels of pro-inflammatory cytokines and biomarkers, and the differences reached statistical significance in several cytokines and parameters linked to antiviral immune response, such as IFN-α2, IFN-γ, and IP-10 (P = 0.0157, P = 0.0002, and P = 0.0229, respectively); inflammatory and regulatory cytokines such as IL-1β (P = 0.0063), IL-8 (P = 0.0037), IL-10 (P = 0.0004), and VEGF (P = 0.0063); chemokines with monocyte/macrophage chemotactic capacity like MCP-1 (P = 0.0003), MIP-1α (P = 0.0029), and MIP-1β (P = 0.0003) (Fig. 1a).
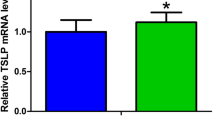
a Cytokine and chemokine levels in NPA supernatants during acute bronchiolitis (BCH), and follow-up sample (FUS obtained during the second visit). This figure only shows biomarkers with statistical differences. *P < 0.05, **P < 0.01, and ***P < 0.001. b Gene expression of several cytokines, biomarkers, receptors, and transcription factors evaluated in cellular pellets of NPA in the period following bronchiolitis (FUS). Data represent expression relative to acute bronchiolitis values. *P < 0.05
No significant differences were found in the rest of the cytokines analyzed: EGF, FGF-2, GM-CSF, sCD40L, IL12p70, IL-17A, and POSTN.
IL-2, IL-5, IL-9, IL-13, IL-25, IL-33, ST-2, TSLP, and TGF-β were not detected in all or in a high percentage of population samples removing them from analysis.
Regarding gene expression levels evaluated in cellular pellets from both samples (basal and FUS) of the total population included (n = 49), a general fall in multiple pro-inflammatory cytokines and chemokine expression was supported by a significant decrease in NFκB2 gene expression (–1.78-fold with respect to the acute bronchiolitis period; P = 0.0116, Fig. 1b), which is the main transcription factor implicated in the trigger of inflammatory response. The rest of the cytokines evaluated (TSLP, POSTN, IL-13, and FLG) were detected in <60% of infants.
Determination of nitrites
Nitrite levels were also determined in the supernatants of NPA during the acute stage of bronchiolitis and in the FUS. A reduction was observed in post-bronchiolitis samples as compared with bronchiolitis (9.68 ± 2.72 vs. 13.86 ± 2.94, respectively), although no significant differences were observed (Fig. 2a).
Expression of pro-inflammatory molecules and lipid mediators in acute bronchiolitis (BCH) and the subsequent period in the supernatant of NPA. a Nitrite levels, b LTC4 soluble levels, c soluble levels of PGE2, and d COX-2 gene expression represented as a value relative to acute bronchiolitis expression. *P < 0.05, **P < 0.01. (FUS: follow-up sample obtained during the second visit within 2–3 months after the acute episode of bronchiolitis.)
Lipid mediators
We observed a significant decrease of LTC4 in FUS with respect to the acute episode (148.94 ± 11.11 vs. 202.41 ± 23.21 pg/mL, respectively; P = 0.0319, Fig. 2b). A reduction in the PGE2 level was observed in FUS, but this change was not statistically significant (3359.4 ± 3184.3 vs. 1226.5 ± 1474 pg/mL; P > 0.05, Fig. 2c). To discern predominant status, we analyzed the LTC4/PGE2 ratio, obtaining a significant increase in FUS relative to the episode of bronchiolitis (0.142 ± 0.028 vs. 0.085 ± 0.016, respectively; P = 0.0425, data not shown).
In addition, COX-2 gene expression was evaluated, and a relevant decrease was observed in FUS as compared with the acute episode of bronchiolitis (2.73-fold; P = 0.005, Fig. 2d).
Evolution and recuperation of immune response after bronchiolitis
We investigated the existence of a relationship between the changes of immune response and subsequent development of wheezing episodes.
Infants who suffered at least one episode of wheezing during the monitoring period showed heterogeneity in their clinical and viral characteristics; however, this population showed a less reduction of LTC4 (P = 0.028; Fig. 3a) maintaining higher levels of LTC4 in the recovery period sample (FUS) than the group without recurrent wheezing.
a Percentage reduction in levels of LTC4 in the NPA supernatant in the FUS-classifying patients attending to develop wheezing after the acute bronchiolitis (BCH) episode. b Levels of PGE2 during acute bronchiolitis (BCH) and FUS (second visit) attending to develop some wheezing episode within 1 year after the bronchiolitis episode. In both cases the results are expressed as mean ± SEM. *P < 0.05. (FUS: follow-up sample obtained during the second visit within 2–3 months after the acute episode of bronchiolitis.)
PGE2 levels were always lower in patients who suffered at least one wheezing episode than patients who did not suffer it, in both time periods (during bronchiolitis and recovery period). The difference was statistically significant when we compared the levels of PGE2 during bronchiolitis and recovery period in patients who never presented wheezing (P = 0.0039; Fig. 3b).
Immunological environment linked to viral infection status
Most of the population has a positive viral detection during bronchiolitis; attending to this analysis, the virus-positive group showed that IP-10, MIP-1α, and MIP-1β levels increased with respect to the group with no viral detection during bronchiolitis episode (9862.6 (2207–67609) vs. 268.1 (94.6–6949) pg/mL, P = 0.0166; 153.6 (68.3–251.2) vs. 33.9 (15.4–44.4) pg/mL, P = 0.0387; 152.4 (46.7–273.9) vs. 20.6 (15.1–51.2) pg/mL, P = 0.0137, respectively). Based on the previously mentioned classification, in the negative viral detection group, the change of soluble values in FUS compared with acute bronchiolitis data was significantly diminished to IL-10 (68.9 (51.3–87.6)% vs. 98.2 (92.5–99.4)%, P = 0.0059) compared with the positive viral group; also, important reductions were observed in MCP-1 (67.9 ± 8.9 vs. 95.1 ± 3.1%) and FGF-2 (40.5 ± 4.6 vs. 61.5 ± 10.9%), although these changes in the negative viral group compared with the positive viral group did not reach statistical significance in recovery time with respect to the acute bronchiolitis period.
No significant differences were observed when immune response between infants with different viral etiology situations, such as coinfection and mono-infection, was compared.
Discussion
To our knowledge, this is the first time that a wide pattern of innate, adaptive immune response and pro-inflammatory molecules, such as nitrites and lipid mediators, have been evaluated in NPAs during and after an episode of severe bronchiolitis in infants. Compared with the acute bronchiolitis period, we observed in the FUS (sample obtained in the second visit between 2 and 3 months after the acute episode) an overall decrease of most cytokines, chemokines, and inflammatory mediators, evidencing significant differences between both time samples in cytokines linked to viral infection, inflammation, and chemokines linked to macrophages independently of the specific virus detected.
During the acute viral infection, chemokines and cytokines play a key role in the recruitment and activation of leukocytes in the lung. Viral-infected epithelial cells produce a plethora of cytokines and chemokines that can induce recruitment and activation of multiple immune cells.13 An increase in cytokine levels with antiviral and immunomodulatory activity, such as IFN-α2, IFN-γ, and IFN-induced chemokines such as IP-10, is observed during a viral infection as corroborated in our study. In addition to these cytokines, MCP-1 (CCL2), MIP-1α (CCL3), and MIP-1β (CCL4) classically characterize the immune response against a respiratory infection with viral etiology, and are associated with severity of disease,14 especially MIP-1α, due to their capacity for eosinophil recruitment, activation, and degranulation in the respiratory tract.15,16 Previous results established that an eosinophilic response to RSV was associated with an increased and prolonged production of MCP-1, MIP-1α, eotaxin, and IP-10 during viral infection.17 In our study, we also obtained a high level of these proteins, but we demonstrate that these high levels are normalized after the acute bronchiolitis episode.
Several studies have proved an inverse relation between innate immune response and clinical severity.18,19 However, some studies have demonstrated the existence of a different cytokine and chemokine pattern in relation to viral etiology.1 In our population, both RSV and HRV were predominant viruses without significant differences in values of soluble biomarkers; differential analyses of cytokines based on the rest of viral etiology could not be performed due to the low analyzed sample size in each group attending to this parameter.
The overall significant decrease that we have observed in nearly half of soluble cytokines and parameters evaluated was accompanied by a substantial reduction in the expression of several genes like amphiregulin or toll-like receptor 3 (TLR3), and nuclear factor-κB (NF-κB). TLR3 recognizes viral transcripts and intermediates, triggering activation of transcription factors such as NF-κB, one of the most important elements in the pro-inflammatory response.20,21,22 Although the reduction of TLR3 was not statistically significant, this result could have an important biological implication. This TLR3–NF-κB pathway has been observed in several cell models of viral infection,23,24 and the results of these studies underscore its key role in pediatric respiratory infection of a viral origin. In our study, other factors and cytokine gene expressions, such as TSLP, POSTN, IL-13, and FLG, were evaluated. However, its expression was detected in a low percentage of population (<60% of infants), which is why we do not perform quantitative analysis as it does not set up a representative population and it could be a confusion factor.
Nitric oxide and its metabolites indirectly reflect an inflammatory status. Although nitric oxide levels diminished, the reduction observed in post-bronchiolitis samples does not reach statistical significance.
The significant change in soluble parameters between acute bronchiolitis and the recovery period was also evidenced in LTC4 levels in NPAs. In a retrospective analysis attending to develop wheezing in the viral clearance period and immune recovery, we observed persistent elevated levels of this lipid mediator in infants who suffered with wheezing compared with the group without symptoms after the acute illness. Changes in the rest of immune parameters evaluated were not statistically significant between both groups (wheezing development or not).
Leukotrienes are inflammatory lipid mediators originated from arachidonic acid by 5-lipooxygenase (5-LO) pathway. These molecules are able to increase vascular permeability, mucus hypersecretion, bronchoconstriction, leukocyte chemotaxis, and airway responsiveness,25 all of which are symptoms shared by asthma and bronchiolitis. Moreover, several manuscripts have reported elevated LTC4 levels in patients with bronchiolitis diagnosis,26,27,28 associating this increase with disease severity. Thus, epidemiological data and these previous evidences suggest a role of bronchiolitis in early life and development of wheezing or asthma;29,30 furthermore, a recent study of our group has demonstrated that severity and frequency of asthma is higher in infants previously hospitalized by viral coinfection bronchiolitis than those by single-infection bronchiolitis.31 However, in this study, no significant differences were observed between single and coinfection in the immunological environment parameters studied.
In our study, LTC4 underwent a less significant decrease in children who suffered wheezing in the 12 months following a bronchiolitis episode compared with infants without wheezing episodes. According to our findings, Da Dalt et al.32 observed that nasal LTC4 levels remained elevated 1 month after the onset of acute bronchiolitis.32 However, these data do not clarify whether elevated LTC4 levels are a cause or a consequence of recurrent wheezing after a viral respiratory infection. One hypothesis is that viral infection produces remodeling of the submucosa, generating susceptibility in nerves and triggering subsequent mast-cell activation associated with a maintained production and release of leukotrienes.33
Eosinophils are one of the main sources of leukotrienes and have been related to enhanced levels of LTC4 in bronchiolitis.34 In our study, eosinophilia could not be evaluated, and perhaps this could be a differentiating characteristic of infants with wheezing after a viral respiratory infection. A deregulation of innate antiviral host defense based on eosinophils is another theory linking bronchiolitis and subsequent development of wheezing.35 Although no statistically significant difference in PGE2 levels was found between samples, the remarkably lower levels in the wheezing group during the acute infection are no less noteworthy. We hypothesized that recurrent wheezing development after a severe bronchiolitis may be related not only to maintained elevated LTC4 levels, but rather to the lower PGE2 levels during the acute infection, as PGE2 can exert anti-inflammatory effects on lower airway inflammation.36
Previous results indicate that the balance between both arms of arachidonic acid, 5-LO, and cyclooxygenase is critical to the resolution or development of lung damage.37 Thus, we measured and have described a significant decrease in COX gene expression in the recovery period. COX-2 gene expression was increased during bronchiolitis episodes, a result found elsewhere.38 This increase likely took place through activation of TLR3 by respiratory viruses;39 thus, the viral clearance that takes place after the acute stage may explain the decrease in PGE2 levels, as well as the lower expression of COX-2 observed in our study during this time.
An important limitation of this study was the reduction of the final population size due to the dropout of patients in the follow-up visit, not obtaining the second sample corresponding to the recovery period, and removing half of the initial population from the analysis of the study.
In conclusion, we have identified changes in the immune response between acute disease and the following recovery period in a population of infants diagnosed with severe bronchiolitis, observing a significant decrease in cytokines and biomarkers linked to innate immune response, some of them with a role in macrophage activation, and accompanied by a drop in pro-inflammatory lipid mediator levels. This pro-inflammatory response was likely mediated by activation of the TLR3–NF-κB pathway. Moreover, we have also identified LTC4 level as a differential element in the development of recurrent wheezing after bronchiolitis. However, more studies will be necessary to clarify the exact mechanism and the role of lipid mediators like LTC4 and PGE2 in evolution of these pathologies.
References
Vandini, S. et al. Immune and inflammatory response in bronchiolitis due to respiratory syncytial virus and rhinovirus infections in infants. Paediatr. Respir. Rev. 24, 60–4 (2017).
Carande, E. J. et al. Viral bronchiolitis management in hospitals in the UK. J. Clin. Virol. 104, 29–33 (2018).
García-García, M. L. et al. Human metapnuemovirus infections in hospitalized children and comparison with other respiratory viruses. 2005–2014 prospective study. PLoS ONE 12, e0173504 (2017).
American Academy of Pediatrics Subcommittee on Diagnosis and Management of Bronchiolitis. Diagnosis and management of bronchiolitis. Pediatrics 118, 1774–93 (2006).
Subhi, R. et al. The prevalence of hypoxaemia among ill children in developing countries: a systematic review. Lancet Infect. Dis. 9, 219–27 (2009).
Chang, A. B. et al. Chronic cough related to acute viral bronchiolitis in children: CHEST Expert Panel Report. Chest 154, 378–82 (2018).
Ralston, S. L. et al. Clinical practice guideline: the diagnosis, management, and prevention of bronchiolitis. Pediatrics 134, e1474–502 (2014).
Higgins, D., Trujillo, C. & Keech, C. Advances in RSV vaccine research and development—a global agenda. Vaccine 34, 2870–5 (2016).
Mansbach, J. M. et al. Children hospitalized with rhinovirus bronchiolitis have asthma-like characteristics. J. Pediatr. 172, 202–4.e1 (2016).
García-García, M. L. et al. Thymic stromal lymphopoietin, IL-33, and periostin in hospitalized infants with viral bronchiolitis. Medicine (Baltim.) 96, e6787 (2017).
Chomczynski, P. & Mackey, K. Short technical reports. Modification of the TRI reagent procedure for isolation of RNA from polysaccharide- and proteoglycan-rich sources. Biotechniques 19, 942–5 (1995).
Livak, K. J. & Schmittgen, T. D. Analysis of relative gene expression data using real-time quantitative PCR and the 2(−Delta Delta C(T)) method. Methods 25, 402–8 (2001).
Ioannidis, I. et al. Plasticity and virus specificity of the airway epithelial cell immune response during respiratory virus infection. J. Virol. 86, 5422–36 (2012).
Tabarani, C. M. et al. Novel inflammatory markers, clinical risk factors and virus type associated with severe respiratory syncytial virus infection. Pediatr. Infect. Dis. J. 32, e437–42 (2013).
Rot, A. et al. RANTES and macrophage inflammatory protein 1 alpha induce the migration and activation of normal human eosinophil granulocytes. J. Exp. Med. 176, 1489–95 (1992).
Harrison, A. M. et al. Respiratory syncytical virus-induced chemokine expression in the lower airways: eosinophil recruitment and degranulation. Am. J. Respir. Crit. Care Med. 159, 1918–24 (1999).
Culley, F. J. et al. Differential chemokine expression following respiratory virus infection reflects Th1- or Th2-biased immunopathology. J. Virol. 80, 4521–7 (2006).
García, C. et al. Decreased innate immune cytokine responses correlate with disease severity in children with respiratory syncytial virus and human rhinovirus bronchiolitis. Pediatr. Infect. Dis. J. 31, 86–9 (2012).
Nicholson, E. G. et al. Robust cytokine and chemokine response in nasopharyngeal secretions: association with decreased severity in children with physician diagnosed bronchiolitis. J. Infect. Dis. 214, 649–55 (2016).
Lay, M. K. et al. Advances in understanding respiratory syncytial virus infection in airway epithelial cells and consequential effects on the immune response. Microbes Infect. 15, 230–42 (2013).
Arruvito, L., Raiden, S. & Geffner, J. Host response to respiratory syncytial virus infection. Curr. Opin. Infect. Dis. 28, 259–66 (2015).
Rudd, B. D. et al. Differential role for TLR3 in respiratory syncytial virus-induced chemokine expression. J. Virol. 79, 3350–7 (2005).
Faksh, A. et al. TLR3 activation increases chemokine expression in human fetal airway smooth muscle cells. Am. J. Physiol. Lung Cell. Mol. Physiol. 310, L202–11 (2016).
Zhan, Q. et al. Double-stranded RNA upregulates the expression of inflammatory mediators in human aortic valve cells through the TLR3-TRIF-noncanonical NF-κB pathway. Am. J. Physiol. Cell Physiol. 312, C407–17 (2017).
Bisgaard, H. Role of leukotrienes in asthma pathophysiology. Pediatr. Pulmonol. 30, 166–76 (2000).
Dimova-Yaneva, D. et al. Eosinophil activation and cysteinyl leukotriene production in infants with respiratory syncytial virus bronchiolitis. Clin. Exp. Allergy 34, 555–8 (2004).
Volovitz, B. et al. The release of leukotrienes in the respiratory tract during infection with respiratory syncytial virus: role in obstructive airway disease. Pediatr. Res. 24, 504–7 (1988).
van Schaik, S. M. et al. Increased production of IFN-gamma and cysteinyl leukotrienes in virus-induced wheezing. J. Allergy Clin. Immunol. 103, 630–6 (1999).
Sigurs, N. et al. Respiratory syncytial virus bronchiolitis in infancy is an important risk factor for asthma and allergy at age 7. Am. J. Respir. Crit. Care Med. 161, 1501–7 (2000).
Sigurs, N. et al. Asthma and allergy patterns over 18 years after severe RSV bronchiolitis in the first year of life. Thorax 65, 1045–52 (2010).
Garcia-Garcia, M. L. et al. Role of viral coinfections in asthma development. PLoS ONE 12, e0189083 (2017).
Da Dalt, L. et al. Nasal lavage leukotrienes in infants with RSV bronchiolitis. Pediatr. Allergy Immunol. 18, 100–4 (2007).
Piedimonte, G. & Simoes, E. A. F. Respiratory syncytial virus and subsequent asthma: one step closer to unravelling the Gordian knot? Eur. Respir. J. 20, 515–7 (2002).
Kim, C. K. et al. Increased levels of BAL cysteinyl leukotrienesinacute [corrected] RSV bronchiolitis. Acta Paediatr. 95, 479–85 (2006).
Rosenberg, H. F. & Domachowske, J. B. Eosinophils, eosinophil ribonucleases, and their role in host defense against respiratory virus pathogens. J. Leukoc. Biol. 70, 691–8 (2001).
Gilroy, D. W. et al. Inducible cyclooxygenase may have anti-inflammatory properties. Nat. Med. 5, 698–701 (1999).
Shirey, K. A. et al. Role of the lipoxygenase pathway in RSV-induced alternatively activated macrophages leading to resolution of lung pathology. Mucosal Immunol. 7, 549–57 (2014).
Seymour, M. L. et al. Rhinovirus infection increases 5-lipoxygenase and cyclooxygenase-2 in bronchial biopsy specimens from nonatopic subjects. J. Infect. Dis. 185, 540–4 (2002).
Yousif, N. M. et al. Activation of EP2 receptor suppresses poly(I:C) and LPS-mediated inflammation in primary microglia and organotypic hippocampal slice cultures: contributing role for MAPKs. Glia 66, 708–24 (2018).
Acknowledgements
We would like to thank all the children and parents who participated in this study, as well as the clinical staff who contributed to the recruitment and collection of samples. We recognize Oliver Shaw, English editor of IIS-FJD, for his revision and editing in English. This study has been partially supported by FIS (Fondo de Investigación Sanitaria-Spanish Health Research Fund) Grants PI15/00048 (IIS-Fundación Jiménez Díaz) and FEDER (Fondo Europeo de Desarrollo Regional); Alfonso X El Sabio University Grant: VIII Convocatoria Santander-UAX; CIBER de Enfermedades Respiratorias (CIBERES), a Carlos III Institute of Health Initiative.
Author information
Authors and Affiliations
Contributions
V.d.P. and B.S. conceived, designed, and wrote the study; M.L.G.-G., C.C. and I.C. were responsible for collecting the NPA samples and clinical data; J.M.R.-M., J.A.C. and I.M. have acquired data and revised the content of the article. All authors participated in discussions, made contributions to the paper, and approved the final version of the paper.
Corresponding author
Ethics declarations
Competing interests
V.d.P. has been a consultant/speaker for AstraZeneca. The other authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sastre, B., García-García, M.L., Calvo, C. et al. Immune recovery following bronchiolitis is linked to a drop in cytokine and LTC4 levels. Pediatr Res 87, 581–587 (2020). https://doi.org/10.1038/s41390-019-0606-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-019-0606-2