Abstract
Background
Height and body mass index (BMI) are associated with higher ovarian cancer risk in the general population, but whether such associations exist among BRCA1/2 mutation carriers is unknown.
Methods
We applied a Mendelian randomisation approach to examine height/BMI with ovarian cancer risk using the Consortium of Investigators for the Modifiers of BRCA1/2 (CIMBA) data set, comprising 14,676 BRCA1 and 7912 BRCA2 mutation carriers, with 2923 ovarian cancer cases. We created a height genetic score (height-GS) using 586 height-associated variants and a BMI genetic score (BMI-GS) using 93 BMI-associated variants. Associations were assessed using weighted Cox models.
Results
Observed height was not associated with ovarian cancer risk (hazard ratio [HR]: 1.07 per 10-cm increase in height, 95% confidence interval [CI]: 0.94–1.23). Height-GS showed similar results (HR = 1.02, 95% CI: 0.85–1.23). Higher BMI was significantly associated with increased risk in premenopausal women with HR = 1.25 (95% CI: 1.06–1.48) and HR = 1.59 (95% CI: 1.08–2.33) per 5-kg/m2 increase in observed and genetically determined BMI, respectively. No association was found for postmenopausal women. Interaction between menopausal status and BMI was significant (Pinteraction < 0.05).
Conclusion
Our observation of a positive association between BMI and ovarian cancer risk in premenopausal BRCA1/2 mutation carriers is consistent with findings in the general population.
Similar content being viewed by others
Background
Ovarian cancer is the fifth leading cause of cancer deaths in US women, due to its typically advanced stage at presentation.1,2 Furthermore, unlike breast or colorectal cancer, there is no proven screening method for ovarian cancer to identify early disease and initiate treatment to improve survival.3,4 Family history, oral contraceptive use, parity, body mass index (BMI), and genetic variants are potentially useful in estimating lifetime risk.1 In particular, inherited BRCA1 and BRCA2 mutations are associated with increased lifetime risk of ovarian cancer and account for ~10–15% of overall disease incidence.5,6,7 However, among mutation carriers, age at diagnosis is variable. Penetrance of BRCA1/2 mutations is likely modified by other genetic variants and lifestyle or reproductive factors.8,9 Investigation of these factors could aid in implementation of strategies to reduce ovarian cancer risk among mutation carriers.
Both height and BMI are quantitative traits with substantial genetic bases. In recent genome-wide association studies (GWAS), numerous genetic variants were found to be associated with these traits.10,11 In the general population, both height and BMI appear to be positively but inconsistently associated with risk of ovarian cancer.12,13,14 Previous studies also showed that the association between BMI and ovarian cancer was stronger in premenopausal women.12,15,16 Because of differences in age at onset and tumour histology/grade, risk factors for ovarian cancer might be different for BRCA1/2 mutation carriers than women in the general population.17 Only one case–control study, with 469 ovarian cancer cases, has examined anthropometric measurements in BRCA1/2 mutation carriers and found that neither height nor BMI were related to ovarian cancer risk.18 Larger, adequately powered studies are needed to assess whether a relationship between either height or BMI and ovarian cancer risk exists for BRCA1/2 mutation carriers, and whether the direction of association is concordant with that in the general population.
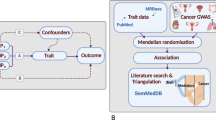
Mendelian randomisation (MR) methods use genetic markers associated with a trait as an instrumental variable (IV) to assess their potential relationship with a disease outcome.19,20,21 Compared to traditional epidemiologic approaches, MR can reduce biases such as reverse causation and residual confounding, which can interfere with causal interpretations. However, the MR approach requires that the genetic variants are associated with the exposure, the variants are not or only weakly associated with confounding factors in the causal pathway, and the variants only affect disease risk through the exposure (i.e. absence of pleiotropic effects).20,21 To the degree that these assumptions are met, the MR approach can strengthen the evidence for a causal relationship between exposure and disease.
Herein, using traditional epidemiologic and MR methods, we conducted analyses of height and BMI and their association with ovarian cancer risk in the Consortium of Investigators for the Modifiers of BRCA1/2 (CIMBA) with 22,588 participants. We examined heterogeneity of these associations with respect to the mutation carried (BRCA1 vs BRCA2), menopausal status, tumour histology, and tumour grade.
Methods
Characteristics of the CIMBA consortium and information on specific genotyping protocols are provided in Supplementary Methods and were described previously.22,23,24
Selection of genetic variants
From the latest publications of the Genetic Investigation of Anthropometric Traits, we identified single-nucleotide polymorphisms (SNPs) associated with height or BMI at genome-wide significance level (P < 5 × 10−8).11,25 SNPs with low imputation quality (<0.5) were excluded, leaving 586 SNPs for height and 93 for BMI. Supplementary Tables 1 and 2 provide additional details on these SNPs.
Statistical analysis
Calculation of the height and BMI genetic scores (GS) was described in detail previously.24 Briefly, we calculated the weighted sums of all of the height- and BMI-associated variants under additive models, which do not include interactions between variants. Namely, we used the formulas: \({\mathrm{Height - GS}} = \mathop {\sum}\nolimits_{i = 1}^{586} {\beta _{XGi}{\mathrm{SNP}}_i}\) and \({\mathrm{BMI - GS}} = \mathop {\sum}\nolimits_{i = 1}^{93} {\beta _{XGi}{\mathrm{SNP}}}\), where βXGi is the literature-reported per-allele magnitude of association of the ith SNP for height and BMI, respectively. A scaling factor was calculated by regressing each GS against its respective trait among non-case carriers. The corresponding regression coefficients were β0 (intercept = 165.455) and β1 (slope = 5.217) for height and β0 (22.607) and β1 (5.523) for BMI. In the present study, BMI-GS was scaled to BMI at the date of questionnaire, rather than BMI at age 18 years, as previous GWAS were based on BMI measurements in middle-aged adults.
We subsequently modelled each scaled GS against ovarian cancer risk using weighted Cox models. Our primary outcome of interest was ovarian cancer diagnosis, with individuals censored for breast cancer diagnosis, risk-reducing bilateral salpingo-oophorectomy, death, or end of follow-up, whichever occurred first. Owing to the study design of CIMBA, weights in the model were applied for cases and non-cases based on previously observed incidence of ovarian cancer in BRCA1/2 carriers.26,27 We applied a robust sandwich variance-estimation approach to the risk estimates to account for non-independence among multiple carriers per family. In addition, we performed subgroup analyses by BRCA1/2 mutations and menopausal status. Menopausal status was defined as a time-varying covariate, coded as premenopausal from birth until age at natural menopause or bilateral salpingo-oophorectomy. For individuals with missing age at menopause, we imputed the age as 50 years. Imputing missing age at menopause as 46 years did not materially change the results. The mean and median ages at natural menopause in this population were 46 and 48 years, respectively. All analyses were adjusted for the first eight principal components (to account for ethnicity and population stratification), birth cohort, and country of enrolment. Additional analyses assessed the associations of height and BMI with ovarian cancer subgroups by histological type (serous vs. non-serous) and by tumour grade (well or moderately differentiated tumours vs. poorly or undifferentiated).
In addition, phenotype associations with each individual height and BMI variant were assessed and pooled using inverse variance-weighted meta-analysis. The individual associations were obtained by first extracting βXGi for each SNP i, which represents the per-allele magnitude of association with height or BMI from previous GWAS. Next, we calculated βYGi and \(SE\left( {\beta _{YGi}} \right)\) using multivariate-adjusted weighted Cox models for each SNP using the CIMBA data, where ovarian cancer risk is predicted by genotype G (with G = 0, 1, 2 for the allele corresponding to greater height or BMI), principal components, birth cohort, BRCA mutation, and country of enrolment. The overall causal association (βYX) is calculated using inverse-variance weighted estimate of each variant’s effect: \(\beta _{YX} = \frac{{\mathop {\sum }\nolimits_i \beta _{XGi}\beta _{YGi}SE(\beta _{YGi})^{ - 2}}}{{\mathop {\sum }\nolimits_i \beta _{XGi}^2SE(\beta _{YGi})^{ - 2}}}\). Standard error was estimated as \(SE_{YX} = \sqrt {\frac{1}{{\mathop {\sum }\nolimits_i \beta _{XGi}^2SE(\beta _{YGi})^{ - 2}}}}\) using the Burgess’s method.19,28 Egger’s test was used to assess for possible pleiotropic effects of the variants (i.e. whether variants influence the outcome through other pathways), to ensure that this assumption held.29
Finally, in participants with available data on height and BMI, we conducted a formal IV analysis using the method of two-stage residual inclusion regression.30 In stage one, observed height or BMI was regressed against the corresponding GS, principal components, birth cohort, country, and mutation status. In the second stage, we used a Cox model to fit ovarian cancer risk against height or BMI, birth cohort, country, mutation status, and residuals from stage one. Variance estimates were obtained through 10,000 boot-straps (see details in Supplementary Methods). In these individuals, we also analysed the association between observed measurements of height or BMI and ovarian cancer risk using weighted Cox models, adjusted for established ovarian cancer risk factors, including birth cohort, menopausal status, age at menarche (years), and parity (continuous). The BMI values used were obtained at the date of questionnaire, usually close to the date of genetic testing and recalled for BMI at age 18 years.
In models with menopausal status as time-varying variable, the test for heterogeneity by menopausal status was essentially a test of the proportional hazards assumption. All analyses were performed using SAS 9.4 (SAS Institute, Cary, NC) and Stata 14.0 (StataCorp, College Station, TX). A two-sided P-value < 0.05 was considered statistically significant unless stated otherwise.
Results
Demographic and clinical characteristics
Characteristics for the 22,588 individuals in the CIMBA consortium, comprising 14,676 BRCA1 and 7912 BRCA2 mutation carriers, are shown in Table 1. We documented 2923 women with ovarian cancer (BRCA1: 2319; BRCA2: 604). Compared with non-cases, participants who developed ovarian cancer were more often parous women, were younger at first live birth, and were from earlier birth cohorts. At the date of questionnaire/interview, height measurement was available for 7657 participants and BMI measurement for 7516 participants. Most tumours for BRCA1/2 mutation carriers were invasive, of serous, poorly, or undifferentiated grade, and stages 3 or 4 at diagnosis, characteristics which are consistent with prior reports.31
Observed and predicted height on risk of ovarian cancer
In the survival modelling of ovarian cancer risk, age was used as the underlying timescale and the numbers of individuals retained in the analysis were 20535, 14647, 7375, and 2832 at ages 30, 40, 50, and 60 years, respectively, suggesting that statistical power for the late age is limited. After adjustment for birth cohort, country of enrolment, mutation, menopausal status, and principal components, a nonsignificant association was found for observed height and ovarian cancer risk (hazard ratio (HR) = 1.07 per 10-cm increase, 95% confidence interval (CI): 0.94–1.23, P = 0.31) (Table 2). We found broadly consistent associations of height in both BRCA1 and BRCA2 mutation carriers by menopausal status and by tumour histological type and grade.
The height GS was significantly associated with height in all participants, in ovarian cancer cases, and in non-case participants (all P < 10−24) (Supplementary Table 3). Overall, approximately 13.4% of the variation in height was explained by the height GS. Besides height, we found weaker associations between the height GS and body weight and age at menarche.
In MR analysis, height GS had a nonsignificant positive association with ovarian cancer risk, HR = 1.02 per 10-cm increase in genetically predicted height, 95% CI: 0.85–1.23, P = 0.82 (Table 3). We found similar associations by subgroups of mutation, menopausal status, and tumour grade.
Combining the effects of all 586 height-associated variants using inverse-variance weighted meta-analysis, we obtained similar findings (HR = 1.02, 95% CI: 0.83–1.26, P = 0.83) (λ). Among the SNPs that were combined, there was a low degree of heterogeneity (I2 = 0%). Examining small-study effects using Egger’s test did not suggest likely pleiotropic effects. In the two-stage residual inclusion analysis, the estimated relative risk was larger though with wide CIs, which overlapped with those derived using other methods (HR = 1.20, 95% CI: 0.86–1.69, P = 0.29).
Observed and predicted BMI on risk of ovarian cancer
After multivariable adjustment, we found a nonsignificant positive association between BMI at the date of questionnaire completion and ovarian cancer risk, HR = 1.04 per 5-kg/m2 increase in BMI, 95% CI: 0.95–1.14, P = 0.42 (Table 4). In a pre-specified analysis, the association between BMI and ovarian cancer risk was stronger in premenopausal women (HR = 1.25, 95% CI: 1.06–1.48; P = 0.009), whereas no association was found in postmenopausal women (HR = 0.98, 95% CI: 0.88–1.10), with significant interaction (P = 0.02). We found that BMI was a significant predictor of non-serous ovarian cancer risk (HR = 1.25, 95% CI: 1.06–1.49) but not for serous ovarian cancer (HR = 0.98, 95% CI: 0.84–1.15).
Similar to BMI at the date of questionnaire completion, we detected a significant interaction of BMI in young adulthood and menopausal status (P = 0.01), with a stronger association for premenopausal women (HR = 1.34, 95% CI: 0.97–1.84) compared with postmenopausal women (HR = 0.82, 95% CI: 0.65–1.04).
BMI-GS was strongly associated with BMI at both the date of questionnaire completion and young adulthood (Supplementary Table 4). Overall, the BMI-GS explained 2.6% of the variation in BMI at the date of questionnaire completion and 1.7% of the variation in young adulthood BMI. We found associations between the BMI-GS and height and age at menarche, though the strength of the association was weaker than the association with BMI.
In the entire consortium, the BMI-GS had a nonsignificant positive association with ovarian cancer risk with a HR = 1.10 per 5-kg/m2 of genetically predicted BMI, 95% CI: 0.86–1.42, P = 0.44 (Table 5). We found heterogeneity by menopausal status (P = 0.006). BMI-GS was positively associated with ovarian cancer risk in premenopausal women (HR = 1.59, 95% CI: 1.08–2.33) but not in postmenopausal women (HR = 0.80, 95% CI: 0.58–1.11). BMI-GS also tended to be more associated with non-serous (HR = 1.60, 95% CI: 0.83–3.08) than serous tumours (HR = 0.92, 95% CI: 0.59–1.43).
We found similar results when we statistically combined the associations of the 93 BMI-associated variants, with an overall HR = 1.12, 95% CI: 0.86–1.46. Heterogeneity was low (I2 = 15.9%), indicating a low likelihood of pleiotropic associations. Using the two-stage residual inclusion approach, we found a generally similar association (HR = 1.37, 95% CI: 0.84–2.24, P = 0.21).
Individual SNPs and ovarian cancer risk
We found 22 height-associated and 4 BMI-associated SNPs that were nominally associated with ovarian cancer risk (P < 0.05; Table 6). None of these SNPs were significantly associated with ovarian cancer risk after correcting for multiple testing. We cross-checked these identified SNPs with the most up-to-date list of ovarian cancer susceptibility SNPs and did not find any overlaps.32
Discussion
Using data from a large international consortium of BRCA1/2 mutation carriers, we found no statistically significant association between height and ovarian cancer risk. Interestingly, we observed interactions between BMI (both observed and genetically predicted) and menopausal status on ovarian cancer risk, with increasing BMI associated with increased risk in premenopausal but not in postmenopausal women.
Our finding of a positive association between BMI and overall ovarian cancer risk in BRCA1 and BRCA2 mutation carriers is corroborated by several prior studies in the general population.12,14,15,33 One MR analysis using 77 BMI-associated SNPs, conducted in the general population, found that each 1-standard deviation (SD) increment in genetically-predicted adult BMI corresponded to an odds ratio (OR) of 1.35 (95% CI: 1.05–1.72).34 We found that 5-kg/m2 (about 1 SD) increment in genetically predicted BMI was associated with an HR = 1.10 (95% CI: 0.86–1.42) in mutation carriers. However, the association of BMI with ovarian cancer risk is likely to vary by menopausal status. In the general population, significant differential association of BMI with ovarian cancer risk by menopausal status has been found in some studies15,16,35,36 but not in others.12,37 A pooled analysis of 47 epidemiologic studies with 25,157 ovarian cancer cases showed that the relative risk per 5-kg/m2 increase in BMI was 1.12 (95% CI: 1.07–1.17) in premenopausal women and 1.08 (95% CI: 1.04–1.12) in postmenopausal women.12 The largest single cohort study, with 3686 ovarian cancer cases, found that the HR per 5-kg/m2 increase in BMI was 1.21 (99% CI: 1.09–1.33) in premenopausal and 1.07 (99% CI: 1.02–1.12) in postmenopausal women.15 An MR analysis conducted in the general population also observed stronger associations for non-high-grade serous carcinomas in premenopausal women (OR = 1.62, 95% CI: 0.88–3.01) compared with postmenopausal hormone replacement therapy (HRT) users (OR = 1.26, 95% CI: 0.57–2.82) and postmenopausal HRT non-users (OR = 1.17, 95% CI: 0.61–2.24), though no formal statistical tests examining heterogeneity were performed.14 Similarly, we found in BRCA1/2 mutation carriers that 5-kg/m2 increment in genetically predicted BMI was associated with an HR = 1.59 (95% CI: 1.08–2.33) for premenopausal ovarian cancer and an HR = 0.80 (95% CI: 0.58-1.11) for postmenopausal ovarian cancer. Studies that have not demonstrated significant variation by menopausal status tended to show that the positive association between BMI and ovarian cancer risk was primarily among those who had never used HRT.12 Taken together, our results and previous literature are suggestive that higher BMI may increase ovarian cancer risk in premenopausal women but not in postmenopausal women.
In addition, several studies that had sufficient numbers of cases to evaluate the relationship between BMI and ovarian cancer risk by histologic subtype have shown significant heterogeneity. Observational studies in the Ovarian Cancer Cohort Consortium found stronger associations between BMI and endometrioid (OR = 1.17 per 5-kg/m2, 95% CI: 1.11–1.23) or mucinous ovarian cancer (OR = 1.19, 95% CI: 1.06–1.32) but no association with serous ovarian cancer (OR = 0.98, 95% CI: 0.94–1.02).16 A more recent MR analysis in the same consortium using a genetic score comprised of 87 SNPs showed that a genetically predicted BMI had a stronger association with endometrioid (OR = 1.17, 95% CI: 0.87–1.59) or mucinous ovarian cancer (OR = 1.18, 95% CI: 0.84–1.67) than high-grade serous cancer (OR = 1.06, 95% CI: 0.89–1.27), though the 95% CIs for these estimates were largely overlapping.14 Consistent with findings in the general population, our study in BRCA1/2 mutation carriers showed that BMI was positively associated with non-serous ovarian cancer (HR = 1.25 per 5-kg/m2, 95% CI: 1.06–1.49 in observed BMI and HR = 1.60, 95% CI: 0.83–3.08, per 5-kg/m2 in genetically predicted BMI), of which endometrioid is a major subtype. Of note, obesity is an established risk factor for endometrial cancer.38 However, subsequent studies with greater number of cases of different ovarian cancer subtypes are needed to assess whether the effect of obesity truly differs by tumour subtype.
Our finding of a nonsignificant positive association between height and ovarian cancer risk is also consistent with prior epidemiological studies in the general population.12,37,39 In the general population, 5-cm increment in height was associated with a 7% increase (95% CI: 5–9%) in ovarian cancer risk,12 and 5-cm increment in genetically predicted height was associated with a 6% (95% CI: 1–11%) increase in ovarian cancer risk.39 The associations for observed height did not differ significantly between ovarian histological types,2,12 while genetically predicted height had a stronger association with clear cell (OR = 1.20, 95% CI: 1.04–1.38) or low-grade/borderline serous ovarian cancers (OR = 1.15, 95% CI: 1.01–1.30) compared to high-grade serous (OR = 1.05, 95% CI: 0.99–1.11).39 We did not find statistically significant heterogeneity by histology in our study of mutation carriers, though point estimates varied across histology.
Several biological mechanisms potentially explain the associations observed in our study. Overweight/obese women are more likely to have anovulatory cycles and fertility issues, particularly when caused by polycystic ovarian syndrome (PCOS), and thus have an increased risk of ovarian cancer.40,41 The association of PCOS with ovarian cancer risk was mainly confined to premenopausal women.42 Some studies have suggested that BRCA1/2 mutation carriers may have subclinical ovarian insufficiency, which could mediate the relationship between obesity-related infertility and increased ovarian cancer risk.43 Obesity itself also creates a proinflammatory state and adipocyte-secreted inflammatory markers have been implicated in ovarian cancer development.44 Circulating levels of oestradiol, androgen, and progesterone have also been implicated in the risk of ovarian cancer.45,46 One study in BRCA1/2 mutation carriers showed higher oestradiol levels during each menstrual cycle compared with non-carriers, supporting the potential role of sex hormones in ovarian tumorigenesis in this population.47 Obese premenopausal women tend to have lower circulating levels of progesterone compared with normal weight women.48 Higher progesterone levels may reduce ovarian cancer risk, through upregulation of p53, leading to tumour cell apoptosis.46,49,50,51 Taken together, these pathways may explain the association of higher BMI with premenopausal ovarian cancer risk. In addition, height has been associated with higher levels of circulating insulin-like growth factor-1 (IGF-1),52,53 a pathway that has been implicated in tumour transformation and may exert antiapoptotic and mitogenic effects.54,55 Moreover, BRCA1 may directly interact with the IGF-1 pathway to mediate cancer risk.56
Our study has several strengths, including large sample size, genetic scores utilising most identified height and BMI variants, several MR methods, and consistent findings between observed and genetically predicted phenotypes. Several limitations of our study should be considered. First, even with a large sample size, the CIs for most risk estimates were wide, which limits inferences about causation. While both the height- and BMI-GS were clearly associated with their respective traits, they were only able to explain 13.4% and 2.6% of the variation, respectively. This reduced the statistical precision of our risk estimates. During the preparation of our manuscript, a new genome-wide meta-analysis57 found a substantial number of new genetic loci related to height and BMI, increasing the amount of variation that could be explained for these two traits to 24.6% and 6.0%, respectively, although the variation that could be explained when examining these SNPs in a validation cohort was 14.0% and 2.3%. This is comparable to the amount of variation that could be explained using the set of genetic variants in our study. Including these additional SNPs may be able to improve the precision of our estimates for both height and BMI. Moreover, the inclusion of rare variants to strengthen the height and BMI genetic instruments should also be considered in future studies.58 Our study did not explicitly examine whether adding height or BMI (either observed or genetically predicted) to existing polygenic risk scores for ovarian cancer could further refine risk prediction. Histology was only available in a subset of ovarian cancer patients, which limits our capacity to understand subtype-specific effects of BMI and height. Our study only included women of European ancestry, which may preclude generalisation to women of other racial/ethnic groups.
In summary, our study suggests that higher BMI may be causally associated with ovarian cancer risk in BRCA1/2 carriers, possibly more so for premenopausal women. BMI could be used to identify premenopausal women at elevated risk of ovarian cancer. Our finding of a stronger association between BMI and non-serous ovarian cancer warrants confirmation in future studies.
References
Salehi, F., Dunfield, L., Phillips, K. P., Krewski, D. Vanderhyden, B. C. Risk factors for ovarian cancer: an overview with emphasis on hormonal factors. J. Toxicol. Environ. Health B Crit. Rev. 11, 301–321 (2008).
Wentzensen, N., Poole, E. M., Trabert, B., White, E., Arslan, A. A., Patel, A. V. et al. Ovarian cancer risk factors by histologic subtype: an analysis from the Ovarian Cancer Cohort Consortium. J. Clin. Oncol. 34, 2888–2898 (2016).
Rauh-Hain, J. A., Krivak, T. C., Del Carmen, M. G., Olawaiye, A. B. Ovarian cancer screening and early detection in the general population. Rev. Obstet. Gynecol. 4, 15–21 (2011).
Jacobs, I. J., Menon, U., Ryan, A., Gentry-Maharaj, A., Burnell, M., Kalsi, J. K. et al. Ovarian cancer screening and mortality in the UK Collaborative Trial of Ovarian Cancer Screening (UKCTOCS): a randomised controlled trial. Lancet 387, 945–956 (2016).
Neff, R. T., Senter, L. Salani, R. BRCA mutation in ovarian cancer: testing, implications and treatment considerations. Ther. Adv. Med. Oncol. 9, 519–531 (2017).
King, M. C., Marks, J. H., Mandell, J. B. & New York Breast Cancer Study Group. Breast and ovarian cancer risks due to inherited mutations in BRCA1 and BRCA2. Science 302, 643–646 (2003).
Kuchenbaecker, K. B., Hopper, J. L., Barnes, D. R., Phillips, K. A., Mooij, T. M., Roos-Blom, M. J. et al. Risks of breast, ovarian, and contralateral breast cancer for BRCA1 and BRCA2 mutation carriers. JAMA 317, 2402–2416 (2017).
Friebel, T. M., Domchek, S. M. & Rebbeck, T. R. Modifiers of cancer risk in BRCA1 and BRCA2 mutation carriers: systematic review and meta-analysis. J. Natl Cancer Inst. 106, https://doi.org/10.1093/jnci/dju091 (2014).
Gayther, S. A., Russell, P., Harrington, P., Antoniou, A. C., Easton, D. F. Ponder, B. A. The contribution of germline BRCA1 and BRCA2 mutations to familial ovarian cancer: no evidence for other ovarian cancer-susceptibility genes. Am. J. Hum. Genet. 65, 1021–1029 (1999).
Lango Allen, H., Estrada, K., Lettre, G., Berndt, S. I., Weedon, M. N., Rivadeneira, F. et al. Hundreds of variants clustered in genomic loci and biological pathways affect human height. Nature 467, 832–838 (2010).
Locke, A. E., Kahali, B., Berndt, S. I., Justice, A. E., Pers, T. H., Day, F. R. et al. Genetic studies of body mass index yield new insights for obesity biology. Nature 518, 197–206 (2015).
Collaborative Group on Epidemiological Studies of Ovarian Cancer. Ovarian cancer and body size: individual participant meta-analysis including 25,157 women with ovarian cancer from 47 epidemiological studies. PLoS Med. 9, e1001200 (2012).
Beehler, G. P., Sekhon, M., Baker, J. A., Teter, B. E., McCann, S. E., Rodabaugh, K. J. et al. Risk of ovarian cancer associated with BMI varies by menopausal status. J. Nutr. 136, 2881–2886 (2006).
Dixon, S. C., Nagle, C. M., Thrift, A. P., Pharoah, P. D., Pearce, C. L., Zheng, W. et al. Adult body mass index and risk of ovarian cancer by subtype: a Mendelian randomization study. Int. J. Epidemiol. 45, 884–895 (2016).
Bhaskaran, K., Douglas, I., Forbes, H., dos-Santos-Silva, I., Leon, D. A. Smeeth, L. Body-mass index and risk of 22 specific cancers: a population-based cohort study of 5.24 million UK adults. Lancet 384, 755–765 (2014).
Olsen, C. M., Nagle, C. M., Whiteman, D. C., Ness, R., Pearce, C. L., Pike, M. C. et al. Obesity and risk of ovarian cancer subtypes: evidence from the Ovarian Cancer Association Consortium. Endocr. Relat. Cancer 20, 251–262 (2013).
Cunningham, J. M., Cicek, M. S., Larson, N. B., Davila, J., Wang, C., Larson, M. C. et al. Clinical characteristics of ovarian cancer classified by BRCA1, BRCA2, and RAD51C status. Sci. Rep. 4, 4026 (2014).
McGee, J., Kotsopoulos, J., Lubinski, J., Lynch, H. T., Rosen, B., Tung, N. et al. Anthropometric measures and risk of ovarian cancer among BRCA1 and BRCA2 mutation carriers. Obesity (Silver Spring) 20, 1288–1292 (2012).
Burgess, S., Butterworth, A. Thompson, S. G. Mendelian randomization analysis with multiple genetic variants using summarized data. Genet. Epidemiol. 37, 658–665 (2013).
Paternoster, L., Tilling, K. Davey Smith, G. Genetic epidemiology and Mendelian randomization for informing disease therapeutics: conceptual and methodological challenges. PLoS Genet. 13, e1006944 (2017).
VanderWeele, T. J., Tchetgen Tchetgen, E. J., Cornelis, M. Kraft, P. Methodological challenges in mendelian randomization. Epidemiology 25, 427–435 (2014).
Couch, F. J., Wang, X., McGuffog, L., Lee, A., Olswold, C., Kuchenbaecker, K. B. et al. Genome-wide association study in BRCA1 mutation carriers identifies novel loci associated with breast and ovarian cancer risk. PLoS Genet. 9, e1003212 (2013).
Rebbeck, T. R., Mitra, N., Wan, F., Sinilnikova, O. M., Healey, S., McGuffog, L. et al. Association of type and location of BRCA1 and BRCA2 mutations with risk of breast and ovarian cancer. JAMA 313, 1347–1361 (2015).
Qian, F., Wang, S., Mitchell, J., McGuffog, L., Barrowdale, D., Leslie, G. et al. Height and body mass index as modifiers of breast cancer risk in BRCA1/2 mutation carriers: a Mendelian randomization study. J. Natl Cancer Inst. https://doi.org/10.1093/jnci/djy132 (2018).
Wood, A. R., Esko, T., Yang, J., Vedantam, S., Pers, T. H., Gustafsson, S. et al. Defining the role of common variation in the genomic and biological architecture of adult human height. Nat. Genet. 46, 1173–1186 (2014).
Antoniou, A., Pharoah, P. D., Narod, S., Risch, H. A., Eyfjord, J. E., Hopper, J. L. et al. Average risks of breast and ovarian cancer associated with BRCA1 or BRCA2 mutations detected in case series unselected for family history: a combined analysis of 22 studies. Am. J. Hum. Genet. 72, 1117–1130 (2003).
Antoniou, A. C., Goldgar, D. E., Andrieu, N., Chang-Claude, J., Brohet, R., Rookus, M. A. et al. A weighted cohort approach for analysing factors modifying disease risks in carriers of high-risk susceptibility genes. Genet Epidemiol. 29, 1–11 (2005).
Bautista, L. E., Smeeth, L., Hingorani, A. D. Casas, J. P. Estimation of bias in nongenetic observational studies using “mendelian triangulation”. Ann. Epidemiol. 16, 675–680 (2006).
Bowden, J., Davey Smith, G. Burgess, S. Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int. J. Epidemiol. 44, 512–525 (2015).
Terza, J. V., Basu, A. Rathouz, P. J. Two-stage residual inclusion estimation: addressing endogeneity in health econometric modeling. J. Health Econ. 27, 531–543 (2008).
Ramus, S. J. Gayther, S. A. The contribution of BRCA1 and BRCA2 to ovarian cancer. Mol. Oncol. 3, 138–150 (2009).
Jones, M. R., Kamara, D., Karlan, B. Y., Pharoah, P. D. P. Gayther, S. A. Genetic epidemiology of ovarian cancer and prospects for polygenic risk prediction. Gynecol. Oncol. 147, 705–713 (2017).
Reeves, G. K., Pirie, K., Beral, V., Green, J., Spencer, E., Bull, D. et al. Cancer incidence and mortality in relation to body mass index in the Million Women Study: cohort study. BMJ 335, 1134 (2007).
Gao, C., Patel, C. J., Michailidou, K., Peters, U., Gong, J., Schildkraut, J. et al. Mendelian randomization study of adiposity-related traits and risk of breast, ovarian, prostate, lung and colorectal cancer. Int. J. Epidemiol. 45, 896–908 (2016).
Liu, Z., Zhang, T. T., Zhao, J. J., Qi, S. F., Du, P., Liu, D. W. et al. The association between overweight, obesity and ovarian cancer: a meta-analysis. Jpn. J. Clin. Oncol. 45, 1107–1115 (2015).
Schouten, L. J., Rivera, C., Hunter, D. J., Spiegelman, D., Adami, H. O., Arslan, A. et al. Height, body mass index, and ovarian cancer: a pooled analysis of 12 cohort studies. Cancer Epidemiol. Biomark. Prev. 17, 902–912 (2008).
Lahmann, P. H., Cust, A. E., Friedenreich, C. M., Schulz, M., Lukanova, A., Kaaks, R. et al. Anthropometric measures and epithelial ovarian cancer risk in the European Prospective Investigation into Cancer and Nutrition. Int. J. Cancer 126, 2404–2415 (2010).
Cook, L. S., Meisner, A. L. W. & Weiss, N. S. in Cancer Epidemiolgy and Prevention, 4th edn. (eds Thun, M. J., Linet, M. S., Cerhan, J. R., Haiman, C. A., David Schottenfeld, D.) Ch. 47 (Oxford University Press, Oxford, 2018).
Dixon-Suen, S. C., Nagle, C. M., Thrift, A. P., Pharoah, P. D. P., Ewing, A., Pearce, C. L. et al. Adult height is associated with increased risk of ovarian cancer: a Mendelian randomisation study. Br. J. Cancer 118, 1123–1129 (2018).
Schildkraut, J. M., Schwingl, P. J., Bastos, E., Evanoff, A. Hughes, C. Epithelial ovarian cancer risk among women with polycystic ovary syndrome. Obstet. Gynecol. 88(4 Pt 1), 554–559 (1996).
Tworoger, S. S., Fairfield, K. M., Colditz, G. A., Rosner, B. A. Hankinson, S. E. Association of oral contraceptive use, other contraceptive methods, and infertility with ovarian cancer risk. Am. J. Epidemiol. 166, 894–901 (2007).
Yin, W., Falconer, H., Yin, L., Xu, L. & Ye, W. Association between polycystic ovary syndrome and cancer risk. JAMA Oncol. https://doi.org/10.1001/jamaoncol.2018.5188 (2018).
Oktay, K., Kim, J. Y., Barad, D. Babayev, S. N. Association of BRCA1 mutations with occult primary ovarian insufficiency: a possible explanation for the link between infertility and breast/ovarian cancer risks. J. Clin. Oncol. 28, 240–244 (2010).
Iyengar, N. M., Gucalp, A., Dannenberg, A. J. Hudis, C. A. Obesity and cancer mechanisms: tumor microenvironment and inflammation. J. Clin. Oncol. 34, 4270–4276 (2016).
Eliassen, A. H. Hankinson, S. E. Endogenous hormone levels and risk of breast, endometrial and ovarian cancers: prospective studies. Adv. Exp. Med. Biol. 630, 148–165 (2008).
Risch, H. A. Hormonal etiology of epithelial ovarian cancer, with a hypothesis concerning the role of androgens and progesterone. J. Natl Cancer Inst. 90, 1774–1786 (1998).
Widschwendter, M., Rosenthal, A. N., Philpott, S., Rizzuto, I., Fraser, L., Hayward, J. et al. The sex hormone system in carriers of BRCA1/2 mutations: a case-control study. Lancet Oncol. 14, 1226–1232 (2013).
Jain, A., Polotsky, A. J., Rochester, D., Berga, S. L., Loucks, T., Zeitlian, G. et al. Pulsatile luteinizing hormone amplitude and progesterone metabolite excretion are reduced in obese women. J. Clin. Endocrinol. Metab. 92, 2468–2473 (2007).
Bu, S. Z., Yin, D. L., Ren, X. H., Jiang, L. Z., Wu, Z. J., Gao, Q. R. et al. Progesterone induces apoptosis and up-regulation of p53 expression in human ovarian carcinoma cell lines. Cancer 79, 1944–1950 (1997).
Schildkraut, J. M., Calingaert, B., Marchbanks, P. A., Moorman, P. G. Rodriguez, G. C. Impact of progestin and estrogen potency in oral contraceptives on ovarian cancer risk. J. Natl Cancer Inst. 94, 32–38 (2002).
Rodriguez, G. C., Nagarsheth, N. P., Lee, K. L., Bentley, R. C., Walmer, D. K., Cline, M. et al. Progestin-induced apoptosis in the Macaque ovarian epithelium: differential regulation of transforming growth factor-beta. J. Natl Cancer Inst. 94, 50–60 (2002).
Crowe, F. L., Key, T. J., Allen, N. E., Appleby, P. N., Overvad, K., Gronbaek, H. et al. A cross-sectional analysis of the associations between adult height, BMI and serum concentrations of IGF-I and IGFBP-1 -2 and -3 in the European Prospective Investigation into Cancer and Nutrition (EPIC). Ann. Hum. Biol. 38, 194–202 (2011).
Beauchamp, M. C., Yasmeen, A., Knafo, A. Gotlieb, W. H. Targeting insulin and insulin-like growth factor pathways in epithelial ovarian cancer. J. Oncol. 2010, 257058 (2010).
Pollak, M. The insulin and insulin-like growth factor receptor family in neoplasia: an update. Nat. Rev. Cancer 12, 159–169 (2012).
Lukanova, A., Lundin, E., Toniolo, P., Micheli, A., Akhmedkhanov, A., Rinaldi, S. et al. Circulating levels of insulin-like growth factor-I and risk of ovarian cancer. Int. J. Cancer 101, 549–554 (2002).
Werner, H. Bruchim, I. IGF-1 and BRCA1 signalling pathways in familial cancer. Lancet Oncol. 13, e537–e544 (2012).
Yengo, L., Sidorenko, J., Kemper, K. E., Zheng, Z., Wood, A. R., Weedon, M. N. et al. Meta-analysis of genome-wide association studies for height and body mass index in approximately 700000 individuals of European ancestry. Hum. Mol. Genet. 27, 3641–3649 (2018).
Visscher, P. M., Wray, N. R., Zhang, Q., Sklar, P., McCarthy, M. I., Brown, M. A. et al. 10 Years of GWAS discovery: biology, function, and translation. Am. J. Hum. Genet. 101, 5–22 (2017).
Acknowledgements
We thank all the families and clinicians who contributed to the studies; Sue Healey, in particular taking on the task of mutation classification with the late Olga Sinilnikova; Maggie Angelakos, Judi Maskiell, Gillian Dite, Helen Tsimiklis; members and participants in the New York site of the Breast Cancer Family Registry; members and participants in the Ontario Familial Breast Cancer Registry; Vilius Rudaitis and Laimonas Griškevičius; Drs Janis Eglitis, Anna Krilova and Aivars Stengrevics; Yuan Chun Ding and Linda Steele for their work in participant enrollment and biospecimen and data management; Bent Ejlertsen and Anne-Marie Gerdes for the recruitment and genetic counseling of participants; Alicia Barroso, Rosario Alonso and Guillermo Pita; Manoukian Siranoush, Bernard Peissel, Cristina Zanzottera, Milena Mariani, Daniela Zaffaroni, Bernardo Bonanni, Monica Barile, Irene Feroce, Mariarosaria Calvello, Alessandra Viel, Riccardo Dolcetti, Giuseppe Giannini, Laura Papi, Gabriele Lorenzo Capone, Liliana Varesco, Viviana Gismondi, Maria Grazia Tibiletti, Daniela Furlan, Antonella Savarese, Aline Martayan, Stefania Tommasi, Brunella Pilato; the personnel of the Cogentech Cancer Genetic Test Laboratory, Milan, Italy; Ms. JoEllen Weaver and Dr. Betsy Bove; Marta Santamariña, Ana Blanco, Miguel Aguado, Uxía Esperón and Belinda Rodríguez. We thank all participants, clinicians, family doctors, researchers, and technicians for their contributions and commitment to the DKFZ study. Genetic Modifiers of Cancer Risk in BRCA1/2 Mutation Carriers (GEMO) study is a study from the National Cancer Genetics Network UNICANCER Genetic Group, France. We wish to pay a tribute to Olga M. Sinilnikova, who with Dominique Stoppa-Lyonnet initiated and coordinated GEMO until she sadly passed away on the 30 June 2014. The team in Lyon (Olga Sinilnikova, Mélanie Léoné, Laure Barjhoux, Carole Verny-Pierre, Sylvie Mazoyer, Francesca Damiola, Valérie Sornin) managed the GEMO samples until the biological resource centre was transferred to Paris in December 2015 (Noura Mebirouk, Fabienne Lesueur, Dominique Stoppa-Lyonnet). We want to thank all the GEMO collaborating groups for their contribution to this study: Coordinating Centre, Service de Génétique, Institut Curie, Paris, France: Muriel Belotti, Ophélie Bertrand, Anne-Marie Birot, Bruno Buecher, Sandrine Caputo, Anaïs Dupré, Emmanuelle Fourme, Marion Gauthier-Villars, Lisa Golmard, Claude Houdayer, Marine Le Mentec, Virginie Moncoutier, Antoine de Pauw, Claire Saule, Dominique Stoppa-Lyonnet, and Inserm U900, Institut Curie, Paris, France: Fabienne Lesueur, Noura Mebirouk. Contributing Centres: Unité Mixte de Génétique Constitutionnelle des Cancers Fréquents, Hospices Civils de Lyon - Centre Léon Bérard, Lyon, France: Nadia Boutry-Kryza, Alain Calender, Sophie Giraud, Mélanie Léone. Institut Gustave Roussy, Villejuif, France: Brigitte Bressac-de-Paillerets, Olivier Caron, Marine Guillaud-Bataille. Centre Jean Perrin, Clermont–Ferrand, France: Yves-Jean Bignon, Nancy Uhrhammer. Centre Léon Bérard, Lyon, France: Valérie Bonadona, Christine Lasset. Centre François Baclesse, Caen, France: Pascaline Berthet, Laurent Castera, Dominique Vaur. Institut Paoli Calmettes, Marseille, France: Violaine Bourdon, Catherine Noguès, Tetsuro Noguchi, Cornel Popovici, Audrey Remenieras, Hagay Sobol. CHU Arnaud-de-Villeneuve, Montpellier, France: Isabelle Coupier, Pascal Pujol. Centre Oscar Lambret, Lille, France: Claude Adenis, Aurélie Dumont, Françoise Révillion. Centre Paul Strauss, Strasbourg, France: Danièle Muller. Institut Bergonié, Bordeaux, France: Emmanuelle Barouk-Simonet, Françoise Bonnet, Virginie Bubien, Michel Longy, Nicolas Sevenet, Institut Claudius Regaud, Toulouse, France: Laurence Gladieff, Rosine Guimbaud, Viviane Feillel, Christine Toulas. CHU Grenoble, France: Hélène Dreyfus, Christine Dominique Leroux, Magalie Peysselon, Rebischung. CHU Dijon, France: Amandine Baurand, Geoffrey Bertolone, Fanny Coron, Laurence Faivre, Caroline Jacquot, Sarab Lizard. CHU St-Etienne, France: Caroline Kientz, Marine Lebrun, Fabienne Prieur. Hôtel Dieu Centre Hospitalier, Chambéry, France: Sandra Fert Ferrer. Centre Antoine Lacassagne, Nice, France: Véronique Mari. CHU Limoges, France: Laurence Vénat-Bouvet. CHU Nantes, France: Stéphane Bézieau, Capucine Delnatte. CHU Bretonneau, Tours and Centre Hospitalier de Bourges France: Isabelle Mortemousque. Groupe Hospitalier Pitié-Salpétrière, Paris, France: Chrystelle Colas, Florence Coulet, Florent Soubrier, Mathilde Warcoin. CHU Vandoeuvre-les-Nancy, France: Myriam Bronner, Johanna Sokolowska. CHU Besançon, France: Marie-Agnès Collonge-Rame, Alexandre Damette. CHU Poitiers, Centre Hospitalier d’Angoulême and Centre Hospitalier de Niort, France: Paul Gesta. Centre Hospitalier de La Rochelle: Hakima Lallaoui. CHU Nîmes Carémeau, France: Jean Chiesa. CHI Poissy, France: Denise Molina-Gomes. CHU Angers, France: Olivier Ingster; Ilse Coene en Brecht Crombez; Ilse Coene and Brecht Crombez; Alicia Tosar and Paula Diaque; Dr. Sofia Khan, Dr. Taru A. Muranen, Dr. Carl Blomqvist, Dr. Irja Erkkilä and Dr. Virpi Palola; The Hereditary Breast and Ovarian Cancer Research Group Netherlands (HEBON) consists of the following Collaborating Centres: Netherlands Cancer Institute (coordinating centre), Amsterdam, NL: M.A. Rookus, F.B.L. Hogervorst, F.E. van Leeuwen, M.A. Adank, M.K. Schmidt, N.S. Russell, D.J. Jenner; Erasmus Medical Center, Rotterdam, NL: J.M. Collée, A.M.W. van den Ouweland, M.J. Hooning, C.M. Seynaeve, C.H.M. van Deurzen, I.M. Obdeijn, I.A. Boere; Leiden University Medical Center, NL: C.J. van Asperen, P. Devilee, T.C.T.E.F. van Cronenburg; Radboud University Nijmegen Medical Center, NL: C.M. Kets, A.R. Mensenkamp; University Medical Center Utrecht, NL: M.G.E.M. Ausems, M.J. Koudijs; Amsterdam Medical Center, NL: C.M. Aalfs, H.E.J. Meijers-Heijboer; VU University Medical Center, Amsterdam, NL: K. van Engelen, J.J.P. Gille; Maastricht University Medical Center, NL: E.B. Gómez-Garcia, M.J. Blok, M. de Boer; University of Groningen, NL: J.C. Oosterwijk, A.H. van der Hout, M.J. Mourits, G.H. de Bock; The Netherlands Comprehensive Cancer Organisation (IKNL): S. Siesling, J.Verloop; The nationwide network and registry of histopathology and cytopathology in The Netherlands (PALGA): A.W. van den Belt-Dusebout. HEBON thanks the study participants and the registration teams of IKNL and PALGA for part of the data collection; Hong Kong Sanatorium and Hospital; the Hungarian Breast and Ovarian Cancer Study Group members (Janos Papp, Aniko Bozsik, Timea Pocza, Zoltan Matrai, Miklos Kasler, Judit Franko, Maria Balogh, Gabriella Domokos, Judit Ferenczi, Department of Molecular Genetics, National Institute of Oncology, Budapest, Hungary) and the clinicians and patients for their contributions to this study; the Oncogenetics Group (VHIO) and the High Risk and Cancer Prevention Unit of the University Hospital Vall d’Hebron, and the Cellex Foundation for providing research facilities and equipment; the ICO Hereditary Cancer Program team led by Dr. Gabriel Capella; the ICO Hereditary Cancer Program team led by Dr. Gabriel Capella; Dr Martine Dumont for sample management and skilful assistance; Ana Peixoto, Catarina Santos and Pedro Pinto; members of the Center of Molecular Diagnosis, Oncogenetics Department and Molecular Oncology Research Center of Barretos Cancer Hospital; Heather Thorne, Eveline Niedermayr, all the kConFab research nurses and staff, the heads and staff of the Family Cancer Clinics, and the Clinical Follow Up Study (which has received funding from the NHMRC, the National Breast Cancer Foundation, Cancer Australia, and the National Institute of Health (USA)) for their contributions to this resource, and the many families who contributed to kConFab; the KOBRA Study Group; Csilla Szabo (National Human Genome Research Institute, National Institutes of Health, Bethesda, MD, USA); Marie Navratilova, Dita Hanouskova and Eva Machackova (Department of Cancer Epidemiology and Genetics, Masaryk Memorial Cancer Institute and MF MU, Brno, Czech Republic); and Michal Zikan, and Zdenek Kleibl (Oncogynecologic Center and Department of Biochemistry and Experimental Oncology, First Faculty of Medicine, Charles University, Prague, Czech Republic); Anne Lincoln, Lauren Jacobs; the NICCC National Familial Cancer Consultation Service team led by Sara Dishon, the laboratory team led by Dr. Flavio Lejbkowicz, and the research field operations team led by Dr. Mila Pinchev; the investigators of the Australia New Zealand NRG Oncology group; members and participants in the Ontario Cancer Genetics Network; Leigha Senter, Kevin Sweet, Caroline Craven, Julia Cooper, and Michelle O’Conor; Yip Cheng Har, Nur Aishah Mohd Taib, Phuah Sze Yee, Norhashimah Hassan and all the research nurses, research assistants and doctors involved in the MyBrCa Study for assistance in patient recruitment, data collection and sample preparation, Philip Iau, Sng Jen-Hwei and Sharifah Nor Akmal for contributing samples from the Singapore Breast Cancer Study and the HUKM-HKL Study, respectively; the Meirav Comprehensive breast cancer centre team at the Sheba Medical Center; Christina Selkirk; Åke Borg, Håkan Olsson, Helena Jernström, Karin Henriksson, Katja Harbst, Maria Soller, Ulf Kristoffersson; from Gothenburg Sahlgrenska University Hospital: Anna Öfverholm, Margareta Nordling, Per Karlsson, Zakaria Einbeigi; from Stockholm and Karolinska University Hospital: Anna von Wachenfeldt, Annelie Liljegren, Annika Lindblom, Brita Arver, Gisela Barbany Bustinza, Johanna Rantala; from Umeå University Hospital: Beatrice Melin, Christina Edwinsdotter Ardnor, Monica Emanuelsson; from Uppsala University: Hans Ehrencrona, Maritta Hellström Pigg, Richard Rosenquist; from Linköping University Hospital: Marie Stenmark-Askmalm, Sigrun Liedgren; Cecilia Zvocec, Qun Niu; Joyce Seldon and Lorna Kwan; Dr. Robert Nussbaum, Beth Crawford, Kate Loranger, Julie Mak, Nicola Stewart, Robin Lee, Amie Blanco and Peggy Conrad and Salina Chan; Simon Gayther, Susan Ramus, Paul Pharoah, Carole Pye, Patricia Harrington and Eva Wozniak; Geoffrey Lindeman, Marion Harris, Martin Delatycki, Sarah Sawyer, Rebecca Driessen, and Ella Thompson for performing all DNA amplification.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
G.P. received honoraria and grant from Pfizer, Roche, Novartis, Accord, AstraZeneca, Amgen, Accord and Lilly. R.S. served on advisory board for Tesaro, Clovis, Astra Zeneca, Ethicon and Genmab, and speaker’s bureau for Tesaro and Genentech. The other authors declare no competing interests.
Ethics approval and consent to participate
The current work and all contributing studies in CIMBA received approval from the local institutional review board or ethics committee. Written informed consent was provided by all of the participants participating in each individual CIMBA study. The institutional committees that approved individual studies are listed in Supplemental Materials.
Funding
CIMBA: The CIMBA data management and data analysis were supported by Cancer Research – UK grants C12292/A20861, C12292/A11174. ACA is a Cancer Research UK Senior Cancer Research Fellow. G.C.T. and A.B.S. are NHMRC Research Fellows. iCOGS: the European Community’s Seventh Framework Programme under grant agreement No. 223175 (HEALTH-F2-2009-223175) (COGS), Cancer Research UK (C1287/A10118, C1287/A 10710, C12292/A11174, C1281/A12014, C5047/A8384, C5047/A15007, C5047/A10692, C8197/A16565), the National Institutes of Health (CA128978) and Post-Cancer GWAS initiative (1U19 CA148537, 1U19 CA148065 and 1U19 CA148112 - the GAME-ON initiative), the Department of Defence (W81XWH-10-1-0341), the Canadian Institutes of Health Research (CIHR) for the CIHR Team in Familial Risks of Breast Cancer (CRN-87521), and the Ministry of Economic Development, Innovation and Export Trade (PSR-SIIRI-701), Komen Foundation for the Cure, the Breast Cancer Research Foundation, and the Ovarian Cancer Research Fund. The PERSPECTIVE project was supported by the Government of Canada through Genome Canada and the Canadian Institutes of Health Research, the Ministry of Economy, Science and Innovation through Genome Québec, and The Quebec Breast Cancer Foundation. BCFR: UM1 CA164920 from the National Cancer Institute. The content of this manuscript does not necessarily reflect the views or policies of the National Cancer Institute or any of the collaborating centres in the Breast Cancer Family Registry (BCFR), nor does mention of trade names, commercial products, or organisations imply endorsement by the US Government or the BCFR. BFBOCC: Lithuania (BFBOCC-LT): Research Council of Lithuania grant SEN-18/2015. BIDMC: Breast Cancer Research Foundation. BMBSA: Cancer Association of South Africa (PI Elizabeth J. van Rensburg). CNIO: Spanish Ministry of Health PI16/00440 supported by FEDER funds, the Spanish Ministry of Economy and Competitiveness (MINECO) SAF2014-57680-R and the Spanish Research Network on Rare diseases (CIBERER). COH-CCGCRN: Research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health under grant number R25CA112486, and RC4CA153828 (PI: J. Weitzel) from the National Cancer Institute and the Office of the Director, National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. CONSIT: Associazione Italiana Ricerca sul Cancro (AIRC; IG2014 no.15547) to P. Radice. Italian Association for Cancer Research (AIRC; grant no.16933) to L. Ottini. Associazione Italiana Ricerca sul Cancro (AIRC; IG2015 no.16732) to P.P. J.A. is supported by funds from Italian citizens who allocated the 5 × 1000 share of their tax payment in support of the Fondazione IRCCS Istituto Nazionale Tumori, according to Italian laws (INT-Institutional strategic projects ‘5 × 1000’). DEMOKRITOS: European Union (European Social Fund – ESF) and Greek national funds through the Operational Program ‘Education and Lifelong Learning’ of the National Strategic Reference Framework (NSRF) - Research Funding Program of the General Secretariat for Research & Technology: SYN11_10_19 NBCA. Investing in knowledge society through the European Social Fund. DFKZ: German Cancer Research Center. EMBRACE: Cancer Research UK Grants C1287/A10118 and C1287/A11990. D.G.E. and F.L. are supported by an NIHR grant to the Biomedical Research Centre, Manchester. The Investigators at The Institute of Cancer Research and The Royal Marsden NHS Foundation Trust are supported by an NIHR grant to the Biomedical Research Centre at The Institute of Cancer Research and The Royal Marsden NHS Foundation Trust. R.E. and E.B. are supported by Cancer Research UK Grant C5047/A8385. R.E. is also supported by NIHR support to the Biomedical Research Centre at The Institute of Cancer Research and The Royal Marsden NHS Foundation Trust. FCCC: The University of Kansas Cancer Center (P30 CA168524) and the Kansas Bioscience Authority Eminent Scholar Program. A.K.G. was funded by R0 1CA140323, R01 CA214545, and by the Chancellors Distinguished Chair in Biomedical Sciences Professorship. FPGMX: FISPI05/2275 and Mutua Madrileña Foundation (FMMA). GC-HBOC: German Cancer Aid (grant no. 110837, R.K.S.). GEMO: Ligue Nationale Contre le Cancer; the Association ‘Le cancer du sein, parlons-en!’ Award, the Canadian Institutes of Health Research for the ‘CIHR Team in Familial Risks of Breast Cancer’ program and the French National Institute of Cancer (INCa grants 2013-1-BCB-01-ICH-1 and SHS-E-SP 18-015). GEORGETOWN: The Non-Therapeutic Subject Registry Shared Resource at Georgetown University (NIH/NCI grant P30-CA051008), the Fisher Center for Hereditary Cancer and Clinical Genomics Research, and Swing Fore the Cure. G-FAST: Bruce Poppe is a senior clinical investigator of FWO. Mattias Van Heetvelde obtained funding from IWT. HCSC: Spanish Ministry of Health PI15/00059, PI16/01292, and CB-161200301 CIBERONC from ISCIII (Spain), partially supported by European Regional Development FEDER funds. HEBCS: Helsinki University Hospital Research Fund, the Finnish Cancer Society and the Sigrid Juselius Foundation. HEBON: the Dutch Cancer Society grants NKI1998-1854, NKI2004-3088, NKI2007-3756, the Netherlands Organisation of Scientific Research grant NWO 91109024, the Pink Ribbon grants 110005 and 2014-187.WO76, the BBMRI grant NWO 184.021.007/CP46 and the Transcan grant JTC 2012 Cancer 12-054. HRBCP: Hong Kong Sanatorium and Hospital, Dr Ellen Li Charitable Foundation, The Kerry Group Kuok Foundation, National Institute of Health1R 03CA130065, and North California Cancer Center. HUNBOCS: Hungarian Research Grants KTIA-OTKA CK-80745 and OTKA K-112228. ICO: The authors would like to particularly acknowledge the support of the Asociación Española Contra el Cáncer (AECC), the Instituto de Salud Carlos III (organismo adscrito al Ministerio de Economía y Competitividad) and “Fondo Europeo de Desarrollo Regional (FEDER), una manera de hacer Europa” (PI10/01422, PI13/00285, PIE13/00022, PI15/00854, PI16/00563 and CIBERONC) and the Institut Català de la Salut and Autonomous Government of Catalonia (2009SGR290, 2014SGR338 and PERIS Project MedPerCan). IHCC: PBZ_KBN_122/P05/2004. ILUH: Icelandic Association ‘Walking for Breast Cancer Research’ and by the Landspitali University Hospital Research Fund. INHERIT: Canadian Institutes of Health Research for the “CIHR Team in Familial Risks of Breast Cancer” program – grant # CRN-87521 and the Ministry of Economic Development, Innovation and Export Trade – grant # PSR-SIIRI-701. IOVHBOCS: Ministero della Salute and ‘5 × 1000’ Istituto Oncologico Veneto grant. IPOBCS: Liga Portuguesa Contra o Cancro. kConFab: The National Breast Cancer Foundation, and previously by the National Health and Medical Research Council (NHMRC), the Queensland Cancer Fund, the Cancer Councils of New South Wales, Victoria, Tasmania and South Australia, and the Cancer Foundation of Western Australia. MAYO: NIH grants CA116167, CA192393 and CA176785, an NCI Specialized Program of Research Excellence (SPORE) in Breast Cancer (CA116201), and a grant from the Breast Cancer Research Foundation. MCGILL: Jewish General Hospital Weekend to End Breast Cancer, Quebec Ministry of Economic Development, Innovation and Export Trade. M.T. is supported by the European Union Seventh Framework Program (2007Y2013)/European Research Council (Grant No. 310018). MODSQUAD: MH CZ - DRO (MMCI, 00209805), MEYS - NPS I - LO1413 to L.F. and by Charles University in Prague project UNCE204024 (to M.Z.). MSKCC: The Breast Cancer Research Foundation, the Robert and Kate Niehaus Clinical Cancer Genetics Initiative, the Andrew Sabin Research Fund and a Cancer Center Support Grant/Core Grant (P30 CA008748). NAROD: 1R01 CA149429-01. NCI: The Intramural Research Program of the US National Cancer Institute, NIH, and by support services contracts NO2-CP-11019-50, N02-CP-21013-63 and N02-CP-65504 with Westat, Inc, Rockville, MD. NICCC: Clalit Health Services in Israel, the Israel Cancer Association and the Breast Cancer Research Foundation (BCRF), NY. NNPIO: the Russian Foundation for Basic Research (grants 17-54-12007, 17-00-00171 and 18-515-12007). NRG Oncology: U10 CA180868, NRG SDMC grant U10 CA180822, NRG Administrative Office and the NRG Tissue Bank (CA 27469), the NRG Statistical and Data Center (CA 37517) and the Intramural Research Program, NCI. OSUCCG: Ohio State University Comprehensive Cancer Center. PBCS: Italian Association of Cancer Research (AIRC) [IG 2013 N.14477] and Tuscany Institute for Tumors (ITT) grant 2014-2015-2016. SEABASS: Ministry of Science, Technology and Innovation, Ministry of Higher Education (UM.C/HlR/MOHE/06) and Cancer Research Initiatives Foundation. SMC: the Israeli Cancer Association. SWE-BRCA: the Swedish Cancer Society. UCHICAGO: NCI Specialized Program of Research Excellence (SPORE) in Breast Cancer (CA125183), R01 CA142996, 1U01CA161032, P20CA233307, R01 CA228198, American Cancer Society (MRSG-13-063-01-TBG, CRP-10-119-01-CCE), Breast Cancer Research Foundation, Susan G. Komen Foundation (SAC110026), and Ralph and Marion Falk Medical Research Trust, the Entertainment Industry Fund National Women’s Cancer Research Alliance. F.Q. was supported by the Alpha Omega Alpha Carolyn L. Cuckein Student Research Fellowship. UCLA: Jonsson Comprehensive Cancer Center Foundation; Breast Cancer Research Foundation. UCSF: UCSF Cancer Risk Program and Helen Diller Family Comprehensive Cancer Center. UKFOCR: Cancer Research UK. UPENN: Breast Cancer Research Foundation; Susan G. Komen Foundation for the cure, Basser Center for BRCA. UPITT/MWH: Hackers for Hope Pittsburgh. VFCTG: Victorian Cancer Agency, Cancer Australia, National Breast Cancer Foundation. WCP: B.Y.K. is funded by the American Cancer Society Early Detection Professorship (SIOP-06-258-01-COUN) and the National Center for Advancing Translational Sciences (NCATS), Grant UL1TR000124. D.G.E. is supported by the Manchester NIHR Biomedical Research Centre (IS-BRC-1215-20007). TOR: H.R. is funed by NCI, R01 CA063682.
Data availability
Owing to the sensitive nature of the data used in this study, data requests by researchers trained in maintaining human subject confidentiality may be directed to the corresponding author of this study.
Note
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution 4.0 International (CC BY 4.0).
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Qian, F., Rookus, M.A., Leslie, G. et al. Mendelian randomisation study of height and body mass index as modifiers of ovarian cancer risk in 22,588 BRCA1 and BRCA2 mutation carriers. Br J Cancer 121, 180–192 (2019). https://doi.org/10.1038/s41416-019-0492-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-019-0492-8
This article is cited by
-
Systematic review of Mendelian randomization studies on risk of cancer
BMC Medicine (2022)
-
Anthropometric risk factors for ovarian cancer in the NIH-AARP Diet and Health Study
Cancer Causes & Control (2021)
-
Diet, weight management, physical activity and Ovarian & Breast Cancer Risk in women with BRCA1/2 pathogenic Germline gene variants: systematic review
Hereditary Cancer in Clinical Practice (2020)
-
Metformin plus first-line chemotherapy versus chemotherapy alone in the treatment of epithelial ovarian cancer: a prospective open-label pilot trial
Cancer Chemotherapy and Pharmacology (2019)