Abstract
Objective
Type 2 diabetes mellitus (T2D) prevalence continues to increase, and age of incidence continues to decrease. More information is needed to target interventions to the ages where they can be most effective. The objective of this study was to explore the degree to which the association between diet and T2D incidence changes through adulthood.
Methods
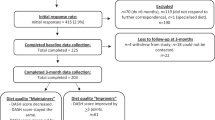
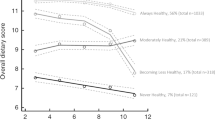
Participants were a large number (N = 2818) of community living adults in Canberra and Queanbeyan, Australia across three cohorts; young (20–24 followed to 32–36), mid-life (40–44 followed to 52–56) and late-life (60–64 followed to 72–76). Self-report dietary pattern scores at baseline and diabetes incidence across 12 years follow-up were measured, alongside confounders of caloric intake, sex, smoking status, years of education, hypertension, BMI and physical activity.
Results
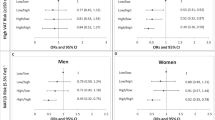
Cox proportional hazards indicated that neither Western nor Prudent dietary pattern scores were significantly associated with T2D incidence when confounders were included in the model. Unadjusted estimates suggested a positive association between Western dietary pattern scores and subsequent diabetes incidence (HR = 1.40, 95% CI [1.18, 1.64]). Compared with the mid-life cohort, a higher Western dietary pattern score posed a lower risk for incident T2D in the young cohort (unadjusted HR = 0.46, 95% CI [0.22, 0.96]), who also had significantly lower BMI and higher physical activity. No such significant effects were found for the late-life cohort.
Conclusions
Our findings indicate that mid-life may be a period of heightened vulnerability to the effects of an unhealthy diet on diabetes risk, but this effect is attenuated when risk factors related to diet, such as adiposity, are taken into account.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Walsh EI, Jacka FN, Butterworth P, Anstey KJ, Cherbuin N. The association between Western and Prudent dietary patterns and fasting blood glucose levels in type 2 diabetes and normal glucose metabolism in older Australian adults. Heliyon. 2017;3:e00315.
Hu FB. Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol. 2002;13:3–9.
Cherbuin N, Walsh E. Sugar in mind: untangling a sweet and sour relationship beyond type 2 diabetes. Front Neuroendocrinol. 2019;54:100769.
Qi L, Cornelis MC, Zhang C, Van Dam RM, Hu FB. Genetic predisposition, Western dietary pattern, and the risk of type 2 diabetes in men. Am J Clin Nutr. 2009;89:1453–8.
Ha K, Joung H, Song Y. Inadequate fat or carbohydrate intake was associated with an increased incidence of type 2 diabetes mellitus in Korean adults: a 12-year community-based prospective cohort study. Diabetes Res Clin Pract. 2019;148:254–61.
Montonen J, Knekt P, Härkänen T, Järvinen R, Heliövaara M, Aromaa A, et al. Dietary patterns and the incidence of type 2 diabetes. Am J Epidemiol. 2005;161:219–27.
Kahn SE, Hull RL, Utzschneider KM. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature. 2006;444:840.
Walsh E, Burns R, Abhayaratna W, Anstey K, Cherbuin N. Physical activity and blood glucose effects on weight gain over 12 years in Middle-aged adults. J Obes Chronic Dis. 2018;2:20–5.
Arnetz L, Ekberg NR, Alvarsson M. Sex differences in type 2 diabetes: focus on disease course and outcomes. Diabetes Metab Syndr Obes. 2014;7:409.
Vlassopoulos A, Lean ME, Combet E. Influence of smoking and diet on glycated haemoglobin and ‘pre-diabetes’ categorisation: a cross-sectional analysis. BMC Public Health. 2013;13:1013.
van der Meer JB, Mackenbach JP. The care and course of diabetes: differences according to level of education. Health Policy. 1999;46:127–41.
Neuhouser ML, Miller DL, Kristal AR, Barnett MJ, Cheskin LJ. Diet and exercise habits of patients with diabetes, dyslipidemia, cardiovascular disease or hypertension. J Am Coll Nutr. 2002;21:394–401.
Schellevis FG, van der Velden J, van de Lisdonk E, Van Eijk JTM, van Weel CV. Comorbidity of chronic diseases in general practice. J Clin Epidemiol. 1993;46:469–73.
Kautzky-Willer A, Harreiter J, Pacini G. Sex and gender differences in risk, pathophysiology and complications of type 2 diabetes mellitus. Endocr Rev. 2016;37:278–316.
Lloyd-Jones DM, Evans JC, Levy D. Hypertension in adults across the age spectrum: current outcomes and control in the community. JAMA. 2005;294:466–72.
Howarth N, Huang TT, Roberts S, Lin B, McCrory M. Eating patterns and dietary composition in relation to BMI in younger and older adults. Int J Obes. 2007;31:675.
Hughes VA, Frontera WR, Roubenoff R, Evans WJ, Singh MAF. Longitudinal changes in body composition in older men and women: role of body weight change and physical activity. Am J Clin Nutr. 2002;76:473–81.
Walsh E, Shaw J, Cherbuin N. Trajectories of BMI change impact glucose and insulin metabolism. Nutr, Metab Cardiovascular Dis. 2018;28:243–51.
Partridge L. Dietary protein, metabolism and aging. Annu Rev Biochem. 2016;85:5–34.
Satija A, Bhupathiraju SN, Rimm EB, Spiegelman D, Chiuve SE, Borgi L, et al. Plant-based dietary patterns and incidence of type 2 diabetes in US men and women: results from three prospective cohort studies. PLoS Med. 2016;13:e1002039.
Chen L, Magliano DJ, Zimmet PZ. The worldwide epidemiology of type 2 diabetes mellitus—present and future perspectives. Nat Rev Endocrinol. 2012;8:228–36.
Anstey KJ, Christensen H, Butterworth P, Easteal S, Mackinnon A, Jacomb T, et al. Cohort profile: the PATH through life project. Int J Epidemiol. 2012;41:dyr025.
Baghurst KI, Record SJ. A computerised dietary analysis system for use with diet diaries or food frequency questionnaires. Community Health Stud. 1984;8:11–8.
Jacka FN, Cherbuin N, Anstey KJ, Butterworth P. Dietary patterns and depressive symptoms over time: examining the relationships with socioeconomic position, health behaviours and cardiovascular risk. PLoS ONE. 2014;9:e87657.
Paulweber B, Valensi P, Lalic N, Greaves C, McKee M, Kissimova-Skarbek K, et al. A European evidence-based guideline for the prevention of type 2 diabetes. Horm Metab Res. 2010;42:S3–36.
Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32(Suppl 1):S498–504.
Therneau TM, Grambsch PM. Modeling survival data: extending the Cox model. New York: Springer Science & Business Media; 2013.
Samocha-Bonet D, Campbell LV, Mori TA, Croft KD, Greenfield JR, Turner N, et al. Overfeeding reduces insulin sensitivity and increases oxidative stress, without altering markers of mitochondrial content and function in humans. PLoS ONE. 2012;7:e36320.
Basu R, Dalla Man C, Campioni M, Basu A, Klee G, Toffolo G, et al. Effects of age and sex on postprandial glucose metabolism: differences in glucose turnover, insulin secretion, insulin action, and hepatic insulin extraction. Diabetes. 2006;55:2001–14.
Agus A, Denizot J, Thevenot J, Martinez-Medina M, Massier S, Sauvanet P, et al. Western diet induces a shift in microbiota composition enhancing susceptibility to Adherent-Invasive E. coli infection and intestinal inflammation. Sci Rep. 2016;6:19032.
Neustadt J. Western diet and inflammation. Integr Med. 2006;5:15.
Riccardi G, Rivellese AA. Effects of dietary fiber and carbohydrate on glucose and lipoprotein metabolism in diabetic patients. Diabetes care. 1991;14:1115–25.
Magliano DJ, Barr EL, Zimmet PZ, Cameron AJ, Dunstan DW, Colagiuri S, et al. Glucose indices, health behaviours and incidence of diabetes in Australia: the AusDiab study. Diabetes Care. 2007;31:267–72.
Asghari G, Rezazadeh A, Hosseini-Esfahani F, Mehrabi Y, Mirmiran P, Azizi F. Reliability, comparative validity and stability of dietary patterns derived from an FFQ in the Tehran Lipid and Glucose Study. Br J Nutr. 2012;108:1109–17.
Borland SE, Robinson SM, Crozier SR, Inskip HM. Stability of dietary patterns in young women over a 2-year period. Eur J Clin Nutr. 2008;62:119.
Lassale C, Guilbert C, Keogh J, Syrette J, Lange K, Cox D. Estimating food intakes in Australia: validation of the Commonwealth Scientific and Industrial Research Organisation (CSIRO) food frequency questionnaire against weighed dietary intakes. J Hum Nutr Dietetics. 2009;22:559–66.
Australian Bureau of Statistics. 4719.0—Overweight and obesity in adults, Australia, 2004-05. Canberra, Australia: Australian Bureau of Statistics; 2005.
Acknowledgements
The authors are grateful to Anthony Jorm, Helen Christensen, Bryan Rogers, Keith Dear, Simon Easteal, Chantal Reglade Meslin, Jerome Maller, Patricia Jacomb, Karen Maxwell, Kristine Kuh and the PATH project interviewers.
Funding
This work was supported the National Health and Medical Research Council [grant numbers 973302, 179805, 157125, 1063907 and 1100579]. At the time of writing, NC’s Fellowship was funded by the Australian Research Council [grant number 120100227]. PB’s Research Fellowship was funded by the Australian Research Council [FT13101444]], KJA’s NHMRC Fellowship #1102694. FNJ was supported by an NHMRC Career Development Fellowship (2) [1108125].
Author information
Authors and Affiliations
Contributions
EW contributed to the design of the study, provided methodological input, conducted the statistical analyses and contributed to all aspects of manuscript preparation and submission. FNJ and PB generated the dietary patterns, provided methodological input and contributed to writing and editing of the manuscript. KJA contributed to the design of the study, provided methodological input and contributed to writing and editing of the manuscript. NC contributed to the design of the study, provided methodological input and theoretical expertise and contributed to all aspects of manuscript preparation and submission.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects/patients were approved by the Australian National University Human Research Ethics Committee. Written informed consent was obtained from all participants.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Walsh, E.I., Jacka, F.N., Butterworth, P. et al. Midlife susceptibility to the effects of poor diet on diabetes risk. Eur J Clin Nutr 75, 85–90 (2021). https://doi.org/10.1038/s41430-020-0673-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-020-0673-9