Abstract
Background/objectives
Associations between patterns of food intake and health in people with multiple sclerosis (MS) are of increasing global interest; however, Australian data are lacking. This study aimed to assess the dietary habits and associations with health outcomes of Australians with MS.
Subjects/methods
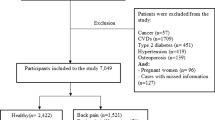
This cross-sectional study used 2016 survey data from the Australian MS Longitudinal Study, including the Dietary Habits Questionnaire, Hospital Anxiety and Depression Scale, Assessment of Quality of Life, Fatigue Severity Scale, Patient-Determined Disease Steps Scale and 13 MS symptoms scales. Regression models were constructed using directed acyclic graphs.
Results
Almost all (94.3%) of the 1490 participants reported making an effort to eating healthy with 21.2% following one or more specific diets, although often not strictly. Overall, 7.9% reported not eating meat, 8.1% reported not consuming dairy, and 4.0% consumed neither food group. A healthier diet score was associated with better mental, physical and total quality of life, and lower depression, and pain scores, and fewer cognition, vision and bowel symptoms. Higher reported fibre, fruit, vegetable and healthy fat scores were positively associated with most health outcomes.
Conclusions
Healthier overall diet scores and higher fibre, fruit and vegetable scores were associated with better health outcomes in this sample of Australians adults with MS. However, the proportion of participants avoiding dairy and meat, or adhering to a specific MS diet was much lower than previously reported. Prospective dietary studies are needed to further understand whether dietary change is feasible and affects health outcomes over time.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Losy J. Is MS an inflammatory or primary degenerative disease? J Neural Transm. 2013;120:1459–62. https://doi.org/10.1007/s00702-013-1079-9.
Tettey P, Simpson S, Taylor B, Ponsonby AL, Lucas RM, Dwyer T, et al. An adverse lipid profile and increased levels of adiposity significantly predict clinical course after a first demyelinating event. J Neurol Neurosurg Psychiatry. 2017;88:395–401. https://doi.org/10.1136/jnnp-2016-315037.
Weinstock-Guttman B, Zivadinov R, Horakova D, Havrdova E, Qu J, Shyh G, et al. Lipid profiles are associated with lesion formation over 24 months in interferon-beta treated patients following the first demyelinating event. J Neurol Neurosurg Psychiatry. 2013;84:1186–91. https://doi.org/10.1136/jnnp-2012-304740.
Katz Sand I. The role of diet in multiple sclerosis: mechanistic connections and current evidence. Curr Nutr Rep. 2018;7:150–60. https://doi.org/10.1007/s13668-018-0236-z.
Riccio P, Rossano R. Nutrition facts in multiple sclerosis. ASN Neuro. 2015;7. https://doi.org/10.1177/1759091414568185.
Dopkins N, Nagarkatti PS, Nagarkatti M. The role of gut microbiome and associated metabolome in the regulation of neuroinflammation in multiple sclerosis and its implications in attenuating chronic inflammation in other inflammatory and autoimmune disorders. Immunology. 2018;154:178–85. https://doi.org/10.1111/imm.12903.
Kirby TO, Ochoa-Repáraz J. The gut microbiome in multiple sclerosis: a potential therapeutic avenue. Med Sci. 2018;6:69.
Esposito S, Bonavita S, Sparaco M, Gallo A, Tedeschi G. The role of diet in multiple sclerosis: a review. Nutr Neurosci. 2018;21:377–90. https://doi.org/10.1080/1028415X.2017.1303016.
Beckett JM, Bird ML, Pittaway JK, Ahuja KD. Diet and multiple sclerosis: scoping review of web-based recommendations. Interact J Med Res. 2019;8:e10050. https://doi.org/10.2196/10050.
Gascoyne CR, Simpson S Jr, Chen J, van der Mei I, Marck CH. Modifiable factors associated with depression and anxiety in multiple sclerosis. Acta Neurol Scand. 2019;140:204–11. https://doi.org/10.1111/ane.13132.
Balto JM, Ensari I, Hubbard EA, Khan N, Barnes JL, Motl RW. Individual and co-occurring SNAP risk factors: smoking, nutrition, alcohol consumption, and physical activity in people with multiple sclerosis. Int J MS Care. 2016;18:298–304. https://doi.org/10.7224/1537-2073.2016-040.
Taylor BV, Palmer A, Simpson S Jr., Lucas R, NZMSPS study group, Simmons RD. et al. Assessing possible selection bias in a national voluntary MS longitudinal study in Australia. Mult Scler. 2013;19:1627–31. https://doi.org/10.1177/1352458513481511.
McKellar S, Horsley P, Chambers R, Bauer JD, Vendersee P, Clarke C, et al. Development of the Diet Habits Questionnaire for use in cardiac rehabilitation. Aust J Prim Health. 2008;14:43–7. https://doi.org/10.1071/PY08035.
Hadgkiss EJ, Jelinek GA, Weiland TJ, Pereira NG, Marck CH, van der Meer DM. The association of diet with quality of life, disability, and relapse rate in an international sample of people with multiple sclerosis. Nutr Neurosci. 2015;18:125–36. https://doi.org/10.1179/1476830514Y.0000000117.
Richardson J, Iezzi A, Khan MA, Maxwell A. Validity and reliability of the Assessment of Quality of Life (AQoL)-8D multi-attribute utility instrument. Patient Patient-Cent Outcomes Res. 2014;7:85–96.
Spinhoven P, Ormel J, Sloekers PP, Kempen GI, Speckens AE, Van Hemert AM. A validation study of the Hospital Anxiety and Depression Scale (HADS) in different groups of Dutch subjects. Psychol Med. 1997;27:363–70.
Learmonth Y, Dlugonski D, Pilutti L, Sandroff B, Klaren R, Motl R. Psychometric properties of the fatigue severity scale and the modified fatigue impact scale. J Neurological Sci. 2013;331:102–7.
Krupp LB, LaRocca NG, Muir-Nash J, Steinberg AD. The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol. 1989;46:1121–3.
Learmonth YC, Motl RW, Sandroff BM, Pula JH, Cadavid D. Validation of patient determined disease steps (PDDS) scale scores in persons with multiple sclerosis. BMC Neurol. 2013;13:37. https://doi.org/10.1186/1471-2377-13-37.
Hohol M, Orav E, Weiner H. Disease steps in multiple sclerosis: a simple approach to evaluate disease progression. Neurology. 1995;45:251–5.
World Health Organization. Body mass index. 2017.
Pink B. Socio-economic indexes for areas (SEIFA). Canberra: Australian Bureau of Statistics; 2011.
StataCorp. Stata statistical software. College Station, TX: StataCorp LP; 2015.
Williamson E, Aitken Z, Lawrie J, Dharmage S, Burgess J, Forbes A. An introduction to causal diagrams for confounder selection. Respirology. 2014;19. https://doi.org/10.1111/resp.12238.
Fitzgerald KC, Tyry T, Salter A, Cofield SS, Cutter G, Fox RJ, et al. A survey of dietary characteristics in a large population of people with multiple sclerosis. Mult Scler Relat Disord. 2018;22:12–18. https://doi.org/10.1016/j.msard.2018.02.019.
Mische LJ, Mowry EM. The evidence for dietary interventions and nutritional supplements as treatment options in multiple sclerosis: a review. Curr Treat Options Neurol. 2018;20:8. https://doi.org/10.1007/s11940-018-0494-5.
Barnard E, Brown CR, Weiland TJ, Jelinek GA, Marck CH. Understanding barriers, enablers, and long-term adherence to a health behavior intervention in people with multiple sclerosis. Disabil Rehabil. 2020;42:822–32. https://doi.org/10.1080/09638288.2018.1510550.
Hendrie G, Baird D, Golley S, Noakes M. CSIRO Healthy Diet Score 2016. Commonwealth Scientific and Industrial Research Organisation; 2016.
Taylor KL, Hadgkiss EJ, Jelinek GA, Weiland TJ, Pereira NG, Marck CH, et al. Lifestyle factors, demographics and medications associated with depression risk in an international sample of people with multiple sclerosis. BMC Psychiatry. 2014;14:327. https://doi.org/10.1186/s12888-014-0327-3.
Marck CH, De Livera AM, Weiland TJ, Jelinek PL, Neate SL, Brown CR, et al. Pain in people with multiple sclerosis: associations with modifiable lifestyle factors, fatigue, depression, anxiety, and mental health quality of life. Front Neurol. 2017;8:461. https://doi.org/10.3389/fneur.2017.00461.
Jelinek PL, Simpson S Jr., Brown CR, Jelinek GA, Marck CH, De Livera AM, et al. Self-reported cognitive function in a large international cohort of people with multiple sclerosis: associations with lifestyle and other factors. Eur J Neurol. 2019;26:142–54. https://doi.org/10.1111/ene.13784.
Ercolini D, Fogliano V. Food design to feed the human gut microbiota. J Agric Food Chem. 2018;66:3754–8. https://doi.org/10.1021/acs.jafc.8b00456.
Melo HM, Santos LE, Ferreira ST. Diet-derived fatty acids, brain inflammation, and mental health. Front Neurosci. 2019;13:265. https://doi.org/10.3389/fnins.2019.00265.
Tettey P, Simpson S Jr., Taylor B, Blizzard L, Ponsonby AL, Dwyer T, et al. An adverse lipid profile is associated with disability and progression in disability, in people with MS. Mult Scler. 2014;20:1737–44. https://doi.org/10.1177/1352458514533162.
Stampanoni Bassi M, Iezzi E, Buttari F, Gilio L, Simonelli I, Carbone F, et al. Obesity worsens central inflammation and disability in multiple sclerosis. Mult Scler. 2020;26:1237–46. https://doi.org/10.1177/1352458519853473.
Tredinnick AR, Probst YC. Evaluating the effects of dietary interventions on disease progression and symptoms of adults with multiple sclerosis: an umbrella review. Adv Nutr. 2020;11:1603–15. https://doi.org/10.1093/advances/nmaa063.
Shamriz O, Mizrahi H, Werbner M, Shoenfeld Y, Avni O, Koren O. Microbiota at the crossroads of autoimmunity. Autoimmun Rev. 2016;15:859–69. https://doi.org/10.1016/j.autrev.2016.07.012.
Weiland TJ, Jelinek GA, Marck CH, Hadgkiss EJ, van der Meer DM, Pereira NG, et al. Clinically significant fatigue: prevalence and associated factors in an international sample of adults with multiple sclerosis recruited via the internet. PLoS ONE. 2015;10:e0115541. https://doi.org/10.1371/journal.pone.0115541.
Marck CH, Jelinek PL, Weiland TJ, Hocking JS, De Livera AM, Taylor KL, et al. Sexual function in multiple sclerosis and associations with demographic, disease and lifestyle characteristics: an international cross-sectional study. BMC Neurol. 2016;16:210. https://doi.org/10.1186/s12883-016-0735-8.
Fitzgerald KC, Tyry T, Salter A, Cofield SS, Cutter G, Fox R, et al. Diet quality is associated with disability and symptom severity in multiple sclerosis. Neurology. 2018;90:e1–11. https://doi.org/10.1212/WNL.0000000000004768.
Riemann-Lorenz K, Eilers M, von Geldern G, Schulz KH, Kopke S, Heesen C. Dietary interventions in multiple sclerosis: development and pilot-testing of an Evidence Based Patient Education Program. PLoS ONE. 2016;11:e0165246. https://doi.org/10.1371/journal.pone.0165246.
Hempel S, Graham GD, Fu N, Estrada E, Chen AY, Miake-Lye I, et al. A systematic review of the effects of modifiable risk factor interventions on the progression of multiple sclerosis. Mult Scler. 2017;23:513–24. https://doi.org/10.1177/1352458517690271.
Westhoek H, Lesschen JP, Rood T, Wagner S, De Marco A, Murphy-Bokern D, et al. Food choices, health and environment: effects of cutting Europe’s meat and dairy intake. Glob Environ Change. 2014;26:196–205. https://doi.org/10.1016/j.gloenvcha.2014.02.004.
Hebert JR, Clemow L, Pbert L, Ockene IS, Ockene JK. Social desirability bias in dietary self-report may compromise the validity of dietary intake measures. Int J Epidemiol. 1995;24:389–98. https://doi.org/10.1093/ije/24.2.389.
Acknowledgements
The authors thank all the participants in the Australian Multiple Sclerosis Longitudinal Study for their support and willingness to complete the surveys.
Funding
This study was supported by Multiple Sclerosis Research Australia. CHM was funded by an Early Career Fellowship from the National Health and Medical Research Council (ID: 1120014) and a Fellowship from Multiple Sclerosis Research Australia (ID 20-216).
Author information
Authors and Affiliations
Contributions
CHM and IvdM were responsible for formulating the research questions and designing the study. IvdM and JC were responsible for data collection, management and cleaning. CHM analysed the data and drafted the manuscript. YP, BT and IvdM contributed to writing and editing the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
YP was a participant in the study but was not involved in the data management or data analysis. The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Marck, C.H., Probst, Y., Chen, J. et al. Dietary patterns and associations with health outcomes in Australian people with multiple sclerosis. Eur J Clin Nutr 75, 1506–1514 (2021). https://doi.org/10.1038/s41430-021-00864-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-021-00864-y
This article is cited by
-
Study protocol for an online lifestyle modification education course for people living with multiple sclerosis: the multiple sclerosis online course (MSOC)
BMC Neurology (2023)
-
Higher diet quality is associated with short and long-term benefits on SF-6D health state utilities: a 5-year cohort study in an international sample of people with multiple sclerosis
Quality of Life Research (2023)
-
Social determinants of health in multiple sclerosis
Nature Reviews Neurology (2022)
-
MIND Diet Adherence Might be Associated with a Reduced Odds of Multiple Sclerosis: Results from a Case–Control Study
Neurology and Therapy (2022)