Abstract
Evidence from literature, including the BRIDGES study, indicates that germline protein truncating variants (PTVs) in FANCM confer moderately increased risk of ER-negative and triple-negative breast cancer (TNBC), especially for women with a family history of the disease. Association between FANCM missense variants (MVs) and breast cancer risk has been postulated. In this study, we further used the BRIDGES study to test 689 FANCM MVs for association with breast cancer risk, overall and in ER-negative and TNBC subtypes, in 39,885 cases (7566 selected for family history) and 35,271 controls of European ancestry. Sixteen common MVs were tested individually; the remaining rare 673 MVs were tested by burden analyses considering their position and pathogenicity score. We also conducted a meta-analysis of our results and those from published studies. We did not find evidence for association for any of the 16 variants individually tested. The rare MVs were significantly associated with increased risk of ER-negative breast cancer by burden analysis comparing familial cases to controls (OR = 1.48; 95% CI 1.07–2.04; P = 0.017). Higher ORs were found for the subgroup of MVs located in functional domains or predicted to be pathogenic. The meta-analysis indicated that FANCM MVs overall are associated with breast cancer risk (OR = 1.22; 95% CI 1.08–1.38; P = 0.002). Our results support the definition from previous analyses of FANCM as a moderate-risk breast cancer gene and provide evidence that FANCM MVs could be low/moderate risk factors for ER-negative and TNBC subtypes. Further genetic and functional analyses are necessary to clarify better the increased risks due to FANCM MVs.
Similar content being viewed by others
Introduction
Since the discovery of the high-risk breast cancer predisposition genes BRCA1 and BRCA2, extensive efforts have tried to identify additional breast cancer predisposition genes. Many candidate genes have been proposed but replication studies have been confirmatory for only few of them [1]. Recently, two large case-control studies were conducted in which several established and candidate breast cancer predisposition genes were tested. The BRIDGES study from the Breast Cancer Association Consortium (BCAC) tested 34 genes in 60,466 women with breast cancer and 53,461 controls [2]. In the second study, 28 genes were tested among 32,247 women with breast cancer and 32,544 unaffected women from US population-based studies in the CARRIERS consortium [3]. Results from both studies were concordant in confirming that germline protein truncating variants (PTVs) in BRCA1, BRCA2 and PALB2 are associated with high-risk of breast cancer, that PTVs in CHEK2 and ATM confer moderate risk especially for the ER-positive disease subtype, and that PTVs in RAD51C, RAD51D and BARD1 are moderate risk variants for ER-negative breast cancer. Lack of evidence of association was detected for PTVs in the great majority of the other tested candidate genes, but for one—namely FANCM—some evidence for association with ER-negative breast cancer was observed [2].
The association between a FANCM PTV and breast cancer risk was initially investigated in 2013 [4]. Since then, many case-control studies have been conducted, most based on the testing the three most common PTVs. Specifically, p.Gln1701* (c.5101 C > T) and p.Gly1906Alafs*12 (c.5791 C > T), which are expected to cause the loss of the FAAP24 binding domain in the FANCM protein C-terminus, were reported by a study of Finnish women as moderate risk variants for ER-negative and triple-negative breast cancer (TNBC) [5, 6]. In a large study of Caucasian women, we observed that the p.Arg658* (c.1972C > T), the third most common PTV, located in the protein N-terminus, was associated with moderate risk for ER-negative and TNBC subtypes, but the evidence of association for p.Gly1906Alafs*12 was inconclusive, and no evidence was observed for p.Gln1701* [7]. Overall, these and other studies [8, 9]—reviewed in Peterlongo et al. (2021)—indicate that FANCM PTVs are potential risk variants for ER-negative and TNBC subtypes; more precisely, they suggest that each PTV confers an increase risk with magnitude that may vary depending on its position in the gene or on the population genetic background [10].
While PTVs in breast cancer predisposition genes are usually considered bona fide pathogenic, missense variants (MVs) are often referred to as “variants of uncertain significance”. Their effect on protein function and cancer risk is generally unknown and difficult to estimate. Several in silico tools that predict pathogenicity of MVs have been developed that, together with additional evidence, such as frequency data, segregation analyses and functional assays, allow some MVs to be classified. However, MVs are often so infrequent that they have to be combined overall, or in subgroups based on their location in the gene domains or pathogenicity prediction score, in order to generate evidence of pathogenicity. MVs in several established and candidate breast cancer predisposition genes have been tested for association with breast cancer risk in many studies. To date, the potential association between FANCM MVs and breast cancer risk has been investigated by three studies in which all the rare variants were combined in burden analyses. Two studies were conducted using familial breast cancer cases with no BRCA1 or BRCA2 pathogenic variants and controls from the general population. The first, based on the analysis of 1207 cases and 1199 controls from France, did not find clear evidence of association with FANCM MVs (OR = 1.6; 95% CI 0.9–2.8) [11]. The second study, including 5770 cases and 5741 population-matched controls predominantly of European ancestry reported a statistically significant association with an OR of 1.50 (95% CI 1.16–1.93) [12]. In the third analysis, which was part of the BRIDGES study, rare FANCM MVs (allele frequency <0.1%) were tested in population- and family-based studies combined and separately. An association with breast cancer risk was found when comparing cases selected for family history of breast cancer and controls, with an OR estimate of 1.22 (95% CI 1.05–1.42) [2]. In the present study, we analysed further the BRIDGES data derived from the FANCM sequencing in women of European ancestry from population- and family-based studies. Specifically, we assessed 673 rare MVs with allele frequency <0.1% that were combined in burden analyses, but we also assessed individually 16 common MVs with allele frequency ≥0.1%. The burden analyses were based on the MVs’ gene domain location, and their pathogenicity prediction score. Analyses were conducted to assess associations with overall breast cancer but also the ER-negative and TNBC disease subtypes.
Materials and methods
Study sample
In this work we included women affected with breast cancer (cases) and unaffected women (controls) from 40 studies participating in the BRIDGES project (Supplementary Table S1), as previously described [2]. All 40 studies were approved by the relevant ethical review board and used appropriate consent procedures. Twenty-eight studies included cases unselected for breast cancer family history and are defined as “population-based studies”. The remaining 12 studies included cases selected because they had a family history of breast cancer, and are defined as “family-based studies”. All women included in this study were of European ancestry and older than 18 years at breast cancer diagnosis (cases) or interview (controls). We excluded women who, having a family history for breast cancer, were eligible for the BRCA1 and BRCA2 test and at the moment of the study enrollment were known to carry a pathogenic variant in these genes. We also excluded all carriers of FANCM PTVs and all women with one or more unknown FANCM MV genotypes. Thus, a total of 39,885 breast cancer cases (of which 91.6% were invasive cases, 6.2% in situ cases, and 2.2% cases of unknown invasiveness) and 35,271 controls were included in this study. Of the cases, 32,083 (80.4%) were from population-based studies and 7566 (19.0%) were from family-based studies; for the remaining 236 cases (0.6%) this information was not available. Of all cases, 5880 had ER-negative breast cancer and 2176 had TNBC.
Sequencing, variant calling and classification
The FANCM gene was included in a panel of 34 established and putative breast cancer predisposition genes that were sequenced in the context of the BRIDGES project [2]. Details of library preparation, next generation sequencing, variant calling, quality control procedures, and variant classification were described previously [2]. The FANCM MVs included in the present analyses were defined as common if their allelic frequency in controls was ≥0.1% and defined as rare if their allelic frequency in controls was <0.1%. The exact positions of FANCM functional and binding domains were derived from to UniProt database and published literature [13,14,15] (Fig. 1). Pathogenicity scores were assigned to each MV using the in silico prediction tools BayesDel [16], Combined Annotation Dependent Depletion (CADD) [17], Helix [18] and Rare Exome Variant Ensemble Learner (REVEL) [19]. The following cut-off were used to classify MVs as pathogenic: BayesDel score with MaxAF >0.069, CADD phred-scaled score ≥30, Helix score >0.50 and REVEL score >0.50.
Functional and binding domains (MPH1, ATP-dependent DNA helicase; MHF, domain of interaction with the Histone Fold 1 and 2 (MHF1/2); MM1, motif of interaction with FANCF within the Fanconi Anemia core complex; MM2, motif of interaction with RecQ-Mediated genome Instability protein 1 (RMI1); MM3, highly conserved motif of still unknown function; FAAP24, domain of interaction with the Fanconi Anemia core complex-Associated Protein 24) are shown in dark grey and their boundaries indicated. The MVs are shown according to their position, the number of carriers in cases and controls, and by their in silico scores of pathogenicity according to BayesDel, CADD, Helix and REVEL tools; in grey are MVs predicted benign by all the tools; in black, MVs predicted pathogenic by one tool; in blue; MVs predicted pathogenic by two tools; in red, MVs predicted pathogenic by three or four tools.
Statistical analyses
To test the association between FANCM MVs and breast cancer risk, we performed logistic regression analyses adjusting for country. Common MVs were tested individually by deriving allelic odds ratios (ORs) with their corresponding 95% confidence intervals (CIs) and P values (P). Multiple testing correction was applied using Benjamini and Hochberg procedure [20]. Rare MVs were tested by burden analyses deriving ORs (with 95% CIs) comparing variant carriers with non-carriers. In this case, heterozygous and homozygous carriers were not distinguished as the number of homozygous carriers was too small to be analysed separately. We first combined all rare variants together then grouped them based on their location within functional or binding domains and by pathogenicity score. Statistical analyses for both common and rare MVs were conducted using the full sample, and separately for population- or family-based studies, and for ER-negative and TNBC case subgroups (each compared to controls) separately. Finally, we performed a fixed-effect meta-analysis combining the OR that we derived in the analysis of family-based studies with the ORs derived by the two previously published studies conducted using familial cases [11, 12]. All statistical analyses were performed using STATA version 15.1 (StataCorp LLC, College Station, Texas, USA). All tests were two-sided and P < 0.05 were considered statistically significant.
Results
A total of 689 unique FANCM MVs, of which 16 were common and 673 were rare, were detected in at least one woman from our study sample (Supplementary Table S2). All 16 common MVs were tested individually for association with breast cancer risk (Supplementary Table S3). Of these 16 MVs, seven showed a possible association (P < 0.05) with breast cancer risk or a protective effect in some of the case groups tested. But none were statistically significant after correction for multiple testing (Supplementary Table S3).
The 673 rare MVs are described and represented, based on their gene location, pathogenicity score according to four in silico tools, and the numbers of variant carriers in cases and controls, in Fig. 1. The burden analyses including all the rare 673 FANCM MVs did not indicate any statistically significant association with breast cancer risk either in the analysis of combined population- and family-based studies or when these groups were analysed separately (Table 1). The only significant association, with OR = 1.48 (95% CI 1.07–2.04; P = 0.017), was found with ER-negative breast cancer in the analysis of family-based studies. These analyses were repeated with subgroups of the variants. We firstly considered the subgroup of the 372 MVs located within the FANCM functional or binding domains but found no evidence of association. We then excluded the 76 MVs located in the FAAP24 domain and found that the 296 remaining MVs were associated with TNBC in familial studies with an OR = 2.27 (95% CI 1.15–4.47; P = 0.017). We further selected among the 296 MVs the 61 MVs predicted to be pathogenic by at least one of the four in silico tools used and found an association with TNBC with an OR = 3.51 (95% CI 1.07–11.44; P = 0.038) in the familial studies (Table 1).
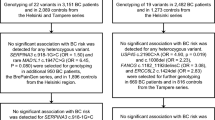
Finally, we considered the two studies published so far testing the association between FANCM MVs and breast cancer risk conducted using familial designs and excluding carriers of BRCA1 or BRCA2 pathogenic variants [11, 12]. Thus, we performed a meta-analysis combining results from these studies with those from our analysis and found that all FANCM MVs combined were associated with familial breast cancer risk with OR = 1.22 (95% CI 1.08–1.38; P = 0.002, Fig. 2).
Discussion
In this study, we re-analysed the BRIDGES FANCM sequencing data assessing the breast cancer risk effects of 689 unique MVs in 39,885 European breast cancer cases and 35,271 controls from population- and family-based studies. According to their allele frequencies, these MVs were analysed either individually or by burden analyses, in the latter case combined in groups considering their gene domain location or their pathogenicity score. Also, the cases were analysed in different combinations, by study-design, and overall and for ER-negative or TNBC clinical subtypes.
Sixteen common MVs with an allele frequency ≥0.1% were analysed individually but we did not find evidence for association for any of these variants. The remaining 673 MVs were rare, with an allele frequency <0.1%. The best approach to study the risks conferred by these variants is that of combining single variant data in burden analysis and of conducting meta-analyses of different studies. Overall, our results and those from the previously conducted studies [2, 11, 12], indicate that FANCM MVs are associated with familial breast cancer risk, suggesting that these variants are low-risk susceptibility variants for breast cancer. This observation was confirmed by the meta-analysis of our and the published results [11, 12] showing that these variants were associated with familial breast cancer risk (OR = 1.22, Fig. 2). However, as studies with statistically significant results have increased likelihood of being published, we cannot exclude that this result is affected by the presence of publication bias. It is also interesting to note that a higher OR estimate, indicating moderately increased risk, was derived for the 296 MVs located within functional or binding domains excluding those in the FAAP24 (OR = 2.27, Table 1), and for the subgroup of 61 variants that among the 296 were predicted to be pathogenic by at least one of the in silico tools we used (OR = 3.51, Table 1). Further studies based on in vitro assays should be conducted to test if any of these MVs is functionally deleterious allowing to better clarify their risk effect on breast cancer. It should be noted that in the present study, as well as in the previously published ones, the association of FANCM MVs was only found in family-based studies. While this supports the hypothesis that FANCM MVs are breast cancer risk factors, the ORs we found in this study are an overestimate of the risks these variants confer. The lack of associations of FANCM MVs with breast cancer risk in the analyses of only population-based studies could be explained by the presence of other unmeasured risk variants aggregating in families that may interact with FANCM MVs. Results from the analysis of family- and population-based studies combined are similar to those of the analysis of only population-based studies as familial cases represent only the 19% of all the cases included.
In conclusion, our data suggest that at least some of the FANCM MVs—in particular those located in some gene domains and classified as pathogenic in silico—could be risk variants for ER-negative breast cancer in familial settings. Larger association studies and, functional assays may be helpful to better clarify these MVs effects on breast cancer risk. Overall, our results showed that perturbation of the FANCM gene has an impact on breast cancer risk, reinforcing the knowledge that FANCM is a breast cancer gene predisposing especially to develop ER-negative and TNBC disease subtypes.
Data availability
The datasets analysed in the current study are available via the BCAC Data Access Co-ordinating Committee (bcac@medschl.cam.ac.uk) upon reasonable request. Summary-level genotype data are available via http://bcac.ccge.medschl.cam.ac.uk and in Supplementary Table S2. Individual-level data are available via the BCAC Data Access Co-ordinating Committee (bcac@medschl.cam.ac.uk).
References
Easton DF, Pharoah PD, Antoniou AC, Tischkowitz M, Tavtigian SV, Nathanson KL, et al. Gene-panel sequencing and the prediction of breast-cancer risk. N Engl J Med. 2015;372:2243–57.
Breast Cancer Association C, Dorling L, Carvalho S, Allen J, Gonzalez-Neira A, Luccarini C, et al. Breast Cancer Risk Genes - Association Analysis in More than 113,000 Women. N Engl J Med. 2021;384:428–39.
Hu C, Hart SN, Gnanaolivu R, Huang H, Lee KY, Na J, et al. A Population-Based Study of Genes Previously Implicated in Breast Cancer. N Engl J Med. 2021;384:440–51.
Gracia-Aznarez FJ, Fernandez V, Pita G, Peterlongo P, Dominguez O, de la Hoya M, et al. Whole exome sequencing suggests much of non-BRCA1/BRCA2 familial breast cancer is due to moderate and low penetrance susceptibility alleles. PLoS ONE. 2013;8:e55681.
Kiiski JI, Pelttari LM, Khan S, Freysteinsdottir ES, Reynisdottir I, Hart SN, et al. Exome sequencing identifies FANCM as a susceptibility gene for triple-negative breast cancer. Proc Natl Acad Sci U S A. 2014;111:15172–7.
Kiiski JI, Tervasmaki A, Pelttari LM, Khan S, Mantere T, Pylkas K, et al. FANCM mutation c.5791C>T is a risk factor for triple-negative breast cancer in the Finnish population. Breast Cancer Res Treat. 2017;166:217–26.
Figlioli G, Bogliolo M, Catucci I, Caleca L, Lasheras SV, Pujol R, et al. The FANCM:p.Arg658* truncating variant is associated with risk of triple-negative breast cancer. NPJ Breast Cancer. 2019;5:38.
Neidhardt G, Hauke J, Ramser J, Gross E, Gehrig A, Muller CR, et al. Association Between Loss-of-Function Mutations Within the FANCM Gene and Early-Onset Familial Breast Cancer. JAMA Oncol. 2017;3:1245–8.
Peterlongo P, Catucci I, Colombo M, Caleca L, Mucaki E, Bogliolo M, et al. FANCM c.5791C>T nonsense mutation (rs144567652) induces exon skipping, affects DNA repair activity and is a familial breast cancer risk factor. Hum Mol Genet. 2015;24:5345–55.
Peterlongo P, Figlioli G, Deans AJ, Couch FJ. Protein truncating variants in FANCM and risk for ER-negative/triple negative breast cancer. NPJ Breast Cancer. 2021;7:130.
Girard E, Eon-Marchais S, Olaso R, Renault AL, Damiola F, Dondon MG, et al. Familial breast cancer and DNA repair genes: Insights into known and novel susceptibility genes from the GENESIS study, and implications for multigene panel testing. Int J Cancer. 2019;144:1962–74.
Li N, Lim BWX, Thompson ER, McInerny S, Zethoven M, Cheasley D, et al. Investigation of monogenic causes of familial breast cancer: data from the BEACCON case-control study. NPJ Breast Cancer. 2021;7:76.
Deans AJ, West SC. FANCM connects the genome instability disorders Bloom’s Syndrome and Fanconi Anemia. Mol Cell. 2009;36:943–53.
UniProt C. UniProt: the universal protein knowledgebase in 2021. Nucleic Acids Res. 2021;49:D480–D9.
Walden H, Deans AJ. The Fanconi anemia DNA repair pathway: structural and functional insights into a complex disorder. Annu Rev Biophys. 2014;43:257–78.
Feng BJ. PERCH: A Unified Framework for Disease Gene Prioritization. Hum Mutat. 2017;38:243–51.
Kircher M, Witten DM, Jain P, O’Roak BJ, Cooper GM, Shendure J. A general framework for estimating the relative pathogenicity of human genetic variants. Nat Genet. 2014;46:310–5.
Vroling B, Heijl S. White paper: The Helix Pathogenicity Prediction Platform2021 April 01, 2021:[arXiv:2104.01033 p.]. https://ui.adsabs.harvard.edu/abs/2021arXiv210401033V.
Ioannidis NM, Rothstein JH, Pejaver V, Middha S, McDonnell SK, Baheti S, et al. REVEL: An Ensemble Method for Predicting the Pathogenicity of Rare Missense Variants. Am J Hum Genet. 2016;99:877–85.
Benjamini Y, Hochberg Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. J R Stat Soc Ser B (Methodol). 1995;57:289–300.
Acknowledgements
We thank all the individuals who took part in these studies and all the researchers, clinicians, technicians and administrative staff who have enabled this work to be carried out.
ABCS thanks the Blood bank Sanquin, The Netherlands. ABCTB Investigators: Christine Clarke, Deborah Marsh, Rodney Scott, Robert Baxter, Desmond Yip, Jane Carpenter, Alison Davis, Nirmala Pathmanathan, Peter Simpson, J. Dinny Graham, Mythily Sachchithananthan. Samples are made available to researchers on a non-exclusive basis. BIGGS thanks Niall McInerney, Gabrielle Colleran, Andrew Rowan, Angela Jones. The BREOGAN study would not have been possible without the contributions of the following: Manuela Gago-Dominguez, Jose Esteban Castelao, Angel Carracedo, Victor Muñoz Garzón, Alejandro Novo Domínguez, Maria Elena Martinez, Sara Miranda Ponte, Carmen Redondo Marey, Maite Peña Fernández, Manuel Enguix Castelo, Maria Torres, Manuel Calaza (BREOGAN), José Antúnez, Máximo Fraga and the staff of the Department of Pathology and Biobank of the University Hospital Complex of Santiago-CHUS, Instituto de Investigación Sanitaria de Santiago, IDIS, Xerencia de Xestion Integrada de Santiago-SERGAS; Joaquín González-Carreró and the staff of the Department of Pathology and Biobank of University Hospital Complex of Vigo, Instituto de Investigacion Biomedica Galicia Sur, SERGAS, Vigo, Spain. The BSUCH study acknowledges the Principal Investigator, Barbara Burwinkel, and, thanks Peter Bugert, Medical Faculty Mannheim. CCGP thanks Styliani Apostolaki, Anna Margiolaki, Georgios Nintos, Maria Perraki, Georgia Saloustrou, Georgia Sevastaki, Konstantinos Pompodakis. CNIO-BCS thanks Guillermo Pita, Charo Alonso, Nuria Álvarez, Pilar Zamora, Primitiva Menendez, the Human Genotyping-CEGEN Unit (CNIO). FHRISK and PROCAS thank NIHR for funding. The GENICA Network: Dr Margarete Fischer-Bosch-Institute of Clinical Pharmacology, Stuttgart, and University of Tübingen, Germany [RH, Hiltrud Brauch, Wing-Yee Lo], Department of Internal Medicine, Johanniter GmbH Bonn, Johanniter Krankenhaus, Bonn, Germany [YDK, Christian Baisch], Institute of Pathology, University of Bonn, Germany [Hans-Peter Fischer], Molecular Genetics of Breast Cancer, Deutsches Krebsforschungszentrum (DKFZ), Heidelberg, Germany [Ute Hamann], Institute for Prevention and Occupational Medicine of the German Social Accident Insurance, Institute of the Ruhr University Bochum (IPA), Bochum, Germany [Thomas Brüning, Beate Pesch, Sylvia Rabstein, Anne Lotz]; and Institute of Occupational Medicine and Maritime Medicine, University Medical Center Hamburg-Eppendorf, Germany [Volker Harth]. HEBCS thanks Johanna Kiiski, Carl Blomqvist, Taru A. Muranen, Kristiina Aittomäki, Kirsimari Aaltonen, Karl von Smitten, Irja Erkkilä, Outi Malkavaara. HEBON Investigators are J. Margriet Collée, Frans B. L. Hogervorst, Maartje J. Hooning, Carolien M. Kets, Peter Devilee, Christi J. van Asperen, Matti A. Rookus, Marjanka K. Schmidt, Cora M. Aalfs, Muriel A. Adank, Margreet G. E. M. Ausems, Marinus J. Blok, Encarna B. Gómez Garcia, Bernadette A. M. Heemskerk-Gerritsen, Antoinette Hollestelle, Agnes Jager, Linetta B. Koppert, Marco Koudijs, Mieke Kriege, Hanne E. J. Meijers-Heijboer, Arjen R. Mensenkamp, Thea M. Mooij, Jan C. Oosterwijk, Ans M. W. van den Ouweland, Frederieke H. van der Baan, Annemieke H. van der Hout, Lizet E. van der Kolk, Rob B. van der Luijt, Carolien H. M. van Deurzen, Helena C. van Doorn, Klaartje van Engelen, Liselotte P. van Hest, Theo A. M. van Os, Senno Verhoef, Maartje J. Vogel & Juul T. Wijnen. HMBCS thanks Peter Hillemanns, Hans Christiansen and Johann H. Karstens. HUBCS thanks Darya Prokofyeva and Shamil Gantsev. KARMA and SASBAC thank the Swedish Medical Research Counsel. KBCP thanks Eija Myöhänen. kConFab/AOCS wish to thank Heather Thorne, Eveline Niedermayr, all the kConFab research nurses and staff, the heads and staff of the Family Cancer Clinics, and the Clinical Follow Up Study (which has received funding from the NHMRC, the National Breast Cancer Foundation, Cancer Australia, and the National Institute of Health (USA)) for their contributions to this resource, and the many families who contribute to kConFab. MARIE thanks Petra Seibold, Nadia Obi, Sabine Behrens, Ursula Eilber and Muhabbet Celik. MASTOS thanks all the study participants and express appreciation to the doctors: Yiola Marcou, Eleni Kakouri, Panayiotis Papadopoulos, Simon Malas and Maria Daniel, as well as to all the nurses and volunteers who provided valuable help towards the recruitment of the study participants. MBCSG (Milan Breast Cancer Study Group): Bernard Peissel, Jacopo Azzollini, Erica Rosina, Daniela Zaffaroni, Irene Feroce, Mariarosaria Calvello, Aliana Guerrieri Gonzaga, Monica Marabelli, Davide Bondavalli and the personnel of the Cogentech Cancer Genetic Test Laboratory. The MCCS was made possible by the contribution of many people, including the original investigators, the teams that recruited the participants and continue working on follow-up, and the many thousands of Melbourne residents who continue to participate in the study. The following are NBCS Collaborators: KKS (PhD), A-LB-D (Prof Em.), ITG (Prof), KSO (Assoc. prof.), OE (MD), BN (MD), JG (MD), OSBREAC and GIGA (MSc). The OFBCR thanks Teresa Selander, Nayana Weerasooriya and Steve Gallinger. ORIGO thanks E. Krol-Warmerdam, and J. Blom for patient accrual, administering questionnaires, and managing clinical information. PBCS thanks Louise Brinton, Mark Sherman, Neonila Szeszenia-Dabrowska, Beata Peplonska, Witold Zatonski, Pei Chao, Michael Stagner. The RBCS thanks Jannet Blom, Saskia Pelders, Wendy J.C. Prager – van der Smissen, and the Erasmus MC Family Cancer Clinic. SBCS thanks Sue Higham, Helen Cramp, Dan Connley, Ian Brock, Sabapathy Balasubramanian and Malcolm W.R. Reed. We thank the SEARCH and EPIC teams. SKKDKFZS thanks all study participants, clinicians, family doctors, researchers and technicians for their contributions and commitment to this study. SZBCS thanks Ewa Putresza. UBCS thanks all study participants as well as the ascertainment, laboratory, analytics and informatics teams at Huntsman Cancer Institute and Intermountain Healthcare. We thank Justin Williams, Brandt Jones, Myke Madsen, Stacey Knight and Kerry Rowe for their important contributions to this study.
Funding
This study was supported by Associazione Italiana Ricerca sul Cancro (AIRC; IG22860) to Paolo Peterlongo and by a fellowship from Fondazione Umberto Veronesi to Gisella Figlioli. BCAC is funded by the European Union’s Horizon 2020 Research and Innovation Programme (grant numbers 634935 and 633784 for BRIDGES and B-CAST respectively), and the PERSPECTIVE I&I project, funded by the Government of Canada through Genome Canada and the Canadian Institutes of Health Research, the Ministère de l’Économie et de l’Innovation du Québec through Genome Québec, the Quebec Breast Cancer Foundation. The EU Horizon 2020 Research and Innovation Programme funding source had no role in study design, data collection, data analysis, data interpretation or writing of the report. Additional funding for BCAC is provided via the Confluence project which is funded with intramural funds from the National Cancer Institute Intramural Research Program, National Institutes of Health. The BRIDGES panel sequencing was supported by the European Union Horizon 2020 research and innovation program BRIDGES (grant number, 634935) and the Wellcome Trust (v203477/Z/16/Z). The ABCS study was supported by the Dutch Cancer Society [grants NKI 2007-3839; 2009 4363]. The work of the BBCC was partly funded by ELAN-Fond of the University Hospital of Erlangen. For BIGGS, ES is supported by NIHR Comprehensive Biomedical Research Centre, Guy’s & St. Thomas’ NHS Foundation Trust in partnership with King’s College London, United Kingdom. IT is supported by the Oxford Biomedical Research Centre. The BREast Oncology GAlician Network (BREOGAN) is funded by Acción Estratégica de Salud del Instituto de Salud Carlos III FIS PI12/02125/Cofinanciado and FEDER PI17/00918/Cofinanciado FEDER; Acción Estratégica de Salud del Instituto de Salud Carlos III FIS Intrasalud (PI13/01136); Programa Grupos Emergentes, Cancer Genetics Unit, Instituto de Investigacion Biomedica Galicia Sur. Xerencia de Xestion Integrada de Vigo-SERGAS, Instituto de Salud Carlos III, Spain; Grant 10CSA012E, Consellería de Industria Programa Sectorial de Investigación Aplicada, PEME I + D e I + D Suma del Plan Gallego de Investigación, Desarrollo e Innovación Tecnológica de la Consellería de Industria de la Xunta de Galicia, Spain; Grant EC11-192. Fomento de la Investigación Clínica Independiente, Ministerio de Sanidad, Servicios Sociales e Igualdad, Spain; and Grant FEDER-Innterconecta. Ministerio de Economia y Competitividad, Xunta de Galicia, Spain. The BSUCH study was supported by the Dietmar-Hopp Foundation, the Helmholtz Society and the German Cancer Research Center (DKFZ). CCGP is supported by funding from the University of Crete. The CECILE study was supported by Fondation de France, Institut National du Cancer (INCa), Ligue Nationale contre le Cancer, Agence Nationale de Sécurité Sanitaire, de l’Alimentation, de l’Environnement et du Travail (ANSES), Agence Nationale de la Recherche (ANR). The CNIO-BCS was supported by the Instituto de Salud Carlos III, the Red Temática de Investigación Cooperativa en Cáncer and grants from the Asociación Española Contra el Cáncer and the Fondo de Investigación Sanitario (PI11/00923 and PI12/00070). FHRISK and PROCAS are funded from NIHR grant PGfAR 0707-10031. DGE, AH and WGN are supported by the NIHR Manchester Biomedical Research Centre (IS-BRC-1215-20007). The GC-HBOC is funded by the German Cancer Aid (#110837, #70111850, #70114178, coordinator: RKS, Cologne) and the Federal Ministry of Education and Research (BMBF), Germany (grant no 01GY1901). LIFE Leipzig Research Center for Civilisation Diseases, Universität Leipzig, is funded by means of the European Union, by the European Regional Development Fund (ERDF), and by means of the Free State of Saxony within the framework of the excellence initiative. The GENICA was funded by the Federal Ministry of Education and Research (BMBF) Germany grants 01KW9975/5, 01KW9976/8, 01KW9977/0 and 01KW0114, the Robert Bosch Foundation, Stuttgart, Deutsches Krebsforschungszentrum (DKFZ), Heidelberg, the Institute for Prevention and Occupational Medicine of the German Social Accident Insurance, Institute of the Ruhr University Bochum (IPA), Bochum, as well as the Department of Internal Medicine, Johanniter GmbH Bonn, Johanniter Krankenhaus, Bonn, Germany. Generation Scotland (GENSCOT) received core support from the Chief Scientist Office of the Scottish Government Health Directorates [CZD/16/6] and the Scottish Funding Council [HR03006]. Genotyping of the GS:SFHS samples was carried out by the Genetics Core Laboratory at the Edinburgh Clinical Research Facility, University of Edinburgh, Scotland and was funded by the Medical Research Council UK and the Wellcome Trust (Wellcome Trust Strategic Award “STratifying Resilience and Depression Longitudinally” (STRADL) Reference 104036/Z/14/Z). Funding for identification of cases and contribution to BCAC funded in part by the Wellcome Trust Seed Award “Temporal trends in incidence and mortality of molecular subtypes of breast cancer to inform public health, policy and prevention” Reference 207800/Z/17/Z. The GESBC was supported by the Deutsche Krebshilfe e. V. [70492] and the German Cancer Research Center (DKFZ). The HABCS study was supported by the Claudia von Schilling Foundation for Breast Cancer Research, by the Lower Saxonian Cancer Society, and by the Rudolf Bartling Foundation. The HEBCS was financially supported by the Helsinki University Hospital Research Fund, the Sigrid Juselius Foundation and the Cancer Foundation Finland. The HEBON study is supported by the Dutch Cancer Society grants NKI1998-1854, NKI2004-3088, NKI2007-3756, the Netherlands Organisation of Scientific Research grant NWO 91109024, the Pink Ribbon grants 110005 and 2014-187.WO76, the BBMRI grant NWO 184.021.007/CP46 and the Transcan grant JTC 2012 Cancer 12-054. The HMBCS was supported by a grant from the Friends of Hannover Medical School and by the Rudolf Bartling Foundation. The HUBCS was supported by a grant from the German Federal Ministry of Research and Education (RUS08/017), B.M. was supported by grant 17-44-020498, 17-29-06014 of the Russian Foundation for Basic Research, D.P. was supported by grant 18-29-09129 of the Russian Foundation for Basic Research, E.K was supported by the mega grant from the Government of Russian Federation (2020-220-08-2197), and the study was performed as part of the assignment of the Ministry of Science and Higher Education of the Russian Federation (№АААА-А16-116020350032-1). Financial support for KARBAC was provided through the regional agreement on medical training and clinical research (ALF) between Stockholm County Council and Karolinska Institutet, the Swedish Cancer Society, The Gustav V Jubilee foundation and Bert von Kantzows foundation. The KARMA study was supported by Märit and Hans Rausings Initiative Against Breast Cancer. The KBCP was financially supported by the special Government Funding (VTR) of Kuopio University Hospital grants, Cancer Fund of North Savo, the Finnish Cancer Organizations, and by the strategic funding of the University of Eastern Finland. kConFab is supported by a grant from the National Breast Cancer Foundation, and previously by the National Health and Medical Research Council (NHMRC), the Queensland Cancer Fund, the Cancer Councils of New South Wales, Victoria, Tasmania and South Australia, and the Cancer Foundation of Western Australia. Financial support for the AOCS was provided by the United States Army Medical Research and Materiel Command [DAMD17-01-1-0729], Cancer Council Victoria, Queensland Cancer Fund, Cancer Council New South Wales, Cancer Council South Australia, The Cancer Foundation of Western Australia, Cancer Council Tasmania and the National Health and Medical Research Council of Australia (NHMRC; 400413, 400281, 199600). GCT and PW are supported by the NHMRC. RB was a Cancer Institute NSW Clinical Research Fellow. The MARIE study was supported by the Deutsche Krebshilfe e.V. [70-2892-BR I, 106332, 108253, 108419, 110826, 110828], the Hamburg Cancer Society, the German Cancer Research Center (DKFZ) and the Federal Ministry of Education and Research (BMBF) Germany [01KH0402]. The MASTOS study was supported by “Cyprus Research Promotion Foundation” grants 0104/13 and 0104/17, and the Cyprus Institute of Neurology and Genetics. MBCSG is supported by grants from the Italian Association for Cancer Research (AIRC). The MCCS was further augmented by Australian National Health and Medical Research Council grants 209057, 396414 and 1074383 and by infrastructure provided by Cancer Council Victoria. Cases and their vital status were ascertained through the Victorian Cancer Registry and the Australian Institute of Health and Welfare, including the National Death Index and the Australian Cancer Database. The NBCS has received funding from the K.G. Jebsen Centre for Breast Cancer Research; the Research Council of Norway grant 193387/V50 (to A-LB-D and VNK) and grant 193387/H10 (to A-LB-D and VNK), South Eastern Norway Health Authority (grant 39346 to A-LB-D) and the Norwegian Cancer Society (to A-LB-D and VNK). The Ontario Familial Breast Cancer Registry (OFBCR) was supported by grant U01CA164920 from the USA National Cancer Institute of the National Institutes of Health. The ORIGO study was supported by the Dutch Cancer Society (RUL 1997-1505) and the Biobanking and Biomolecular Resources Research Infrastructure (BBMRI-NL CP16). The PBCS was funded by Intramural Research Funds of the National Cancer Institute, Department of Health and Human Services, USA. Genotyping for PLCO was supported by the Intramural Research Program of the National Institutes of Health, NCI, Division of Cancer Epidemiology and Genetics. The PLCO is supported by the Intramural Research Program of the Division of Cancer Epidemiology and Genetics and supported by contracts from the Division of Cancer Prevention, National Cancer Institute, National Institutes of Health. The RBCS was funded by the Dutch Cancer Society (DDHK 2004-3124, DDHK 2009-4318). The SASBAC study was supported by funding from the Agency for Science, Technology and Research of Singapore (A*STAR), the US National Institute of Health (NIH) and the Susan G. Komen Breast Cancer Foundation. SEARCH is funded by Cancer Research UK [C490/A10124, C490/A16561] and supported by the UK National Institute for Health Research Biomedical Research Centre at the University of Cambridge. The University of Cambridge has received salary support for PDPP from the NHS in the East of England through the Clinical Academic Reserve. SKKDKFZS is supported by the DKFZ. The SMC is funded by the Swedish Cancer Foundation and the Swedish Research Council (VR 2017-00644) grant for the Swedish Infrastructure for Medical Population-based Life-course Environmental Research (SIMPLER). The SZBCS was supported by Grant PBZ_KBN_122/P05/2004 and the program of the Minister of Science and Higher Education under the name “Regional Initiative of Excellence” in 2019-2022 project number 002/RID/2018/19 amount of financing 12,000,000 PLN. UBCS was supported by funding from National Cancer Institute (NCI) grant R01 CA163353 (to NJC) and the Women’s Cancer Center at the Huntsman Cancer Institute (HCI). Data collection for UBCS was supported by the Utah Population Database (UPDB) and Utah Cancer Registry (UCR). The UPDB is supported by HCI (including Huntsman Cancer Foundation, HCF), the University of Utah, and NCI grant P30 CA2014. The UCR is funded by the NCI’s SEER Program, Contract No. HHSN261201800016I, the US Center for Disease Control and Prevention’s National Program of Cancer Registries (Cooperative Agreement No. NU58DP006320), the University of Utah, and HCF.
Author information
Authors and Affiliations
Consortia
Contributions
Conceived the study: GF, AB, PRa, PPe. Statistical analyses: GF, PPe Coordination of the BRIDGES study and funding acquisition: JDen, AMD, DFE, MLus, KMi, PDPP. Administrative support and data management: MKB,QW Provided DNA samples and data: TUA, NNA, HBec, MWB, SBe, JBen, MBerm, MJB, NVB, BBon, BBur, NJC, AC, JEC, MHC, SJC, KCz, PD, TD, CEn, ME, PAF, JDFi, MGa, MG-D, MG-C, AG-N, FGr, PGu, MG, AH, EHah, PHall, UH, PAH, WH, PHi, AHol, MJH, RH, AHow, KHu, AJage, AJak, EKK, Y-DK, VNK, ALin, JLis, JLu, AMan, SMan, SMar, DM, WGN, NOb, MIP, MUR, VRh, MAR, ES, EJS, RKS, MSh, RSi, MCS, MS, RAEMT, IT, TT, LEVDK, EMVV, BWa, XRY Wrote the paper: GF, PRa, PPe Contributed to paper writing: MAA, MKS, ILA, JC-C, HNe, GC-T, DGE, RLM. All authors read and approved the final version of the paper.
Corresponding author
Ethics declarations
Competing interests
MWB conducts research funded by Amgen, Novartis and Pfizer. PAF conducts research funded by Amgen, Novartis and Pfizer; he received Honoraria from Roche, Novartis and Pfizer. All the other authors declare no competing interests.
Ethics approval
All contributing studies were approved by the relevant ethical review boards and used appropriate consent procedures. The research conformed to the principles of the Helsinki Declaration.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Figlioli, G., Billaud, A., Ahearn, T.U. et al. FANCM missense variants and breast cancer risk: a case-control association study of 75,156 European women. Eur J Hum Genet 31, 578–587 (2023). https://doi.org/10.1038/s41431-022-01257-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41431-022-01257-w