Abstract
To determine whether white-collar workers treated for hypertension who are exposed to psychosocial stressors at work have a higher prevalence of uncontrolled hypertension than unexposed workers, this study conducted three waves of data collection over a 5-year period (repeated cross-sectional design). The study sample was composed of 464 white-collar workers treated for hypertension. At each collection time, ambulatory blood pressure (ABP) was measured every 15 min during the workday. Uncontrolled hypertension was defined as a mean daytime systolic ABP ≥135 mmHg and/or diastolic ABP ≥85 mmHg for non-diabetic participants and systolic ABP ≥125 mmHg and/or diastolic ABP ≥75 mmHg for diabetic participants. Job strain was evaluated with Karasek’s demand–latitude model using validated scales for psychological demands and decision latitude. Prevalence ratios (PR) and 95% confidence intervals (CI) were estimated using generalized estimating equations, adjusting for sociodemographic and lifestyle-related risk factors. Men with job strain (high demands and low latitude) and active jobs (high demands and high latitude) had a higher prevalence of uncontrolled hypertension (PR job strain = 1.46, 95% CI: 1.07–1.98 and PR active = 1.47, 95% CI: 1.12–1.94). When considered separately, high demands were associated with a higher prevalence of uncontrolled hypertension in both men (PR highest tertile = 1.60, 95% CI: 1.25–2.06) and women (PR highest tertile = 1.60, 95% CI: 1.03–2.47). Workers exposed to psychosocial stressors at work according to the demand–latitude model had a higher prevalence of uncontrolled hypertension. Reducing these frequent exposures could help to reduce the burden of uncontrolled hypertension.
Similar content being viewed by others
Introduction
High blood pressure (BP) is the leading risk factor for cardiovascular disease (CVD) [1]. CVD risk is increased by more than twofold in the presence of hypertension [2]. Approximately 60% of individuals will receive hypertensive medication during their lifetime [3]. According to national surveys in Canada and the United States, 20–40% of adults receiving pharmacologic treatment for hypertension have uncontrolled hypertension [4, 5]. Uncontrolled hypertension can lead to serious consequences for the cardiovascular system, including increased incident heart failure [6], chronic kidney disease [7], and cardiovascular mortality [8].
Prospective epidemiological studies have identified psychosocial stressors at work as important risk factors for BP elevation and hypertension [9,10,11,12,13] and for CVD incidence and recurrence [14, 15]. However, little is known about the effect of these stressors on the BP of workers treated for hypertension. Karasek’s demand–latitude model is the most widely used model to define these stressors. This model postulates that a combination of high psychological job demands and low job control (i.e., job strain) increases the risk of developing stress-related health problems. Only one previous study examined the effect of job strain on uncontrolled hypertension, and it found no association [16]. However, this study was conducted exclusively among men and used casual BP measurements [16]. Because casual BP measurements lack validity and precision [17], especially for assessing the effect of psychosocial stressors at work on BP [10], the effect of these stressors on hypertension control in men and women treated for hypertension is yet unknown.
The objective of this study of white-collar workers treated for hypertension was to examine, for the first time, whether those exposed to psychosocial stressors at work had a higher prevalence of uncontrolled hypertension, measured using ambulatory BP (ABP), than unexposed workers.
Methods
Study design and population
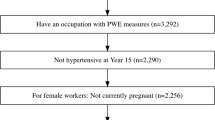
The study design and population are described elsewhere [18, 19]. Briefly, the study relied on a repeated cross-sectional design, which is well suited for dynamic populations such as work organizations as it accommodates the addition of new participants over multiple study time points. The study population was composed of white-collar public insurance workers from three institutions in Quebec City, Canada. The workers from each institution were located at the same worksite. Their main professional activities were planning and providing insurance services to the general population. Data were collected at three time points: at baseline (2000–2004), 3 years later (2004–2006), and 5 years later (2006–2009). All eligible employees were invited to participate at each time point. Participation rates for each collection point ranged between 80% and 86%. The study was approved by the Research Center of the CHU de Québec ethical review board, and all participants provided their informed consent.
The current analyses were restricted to participants who reported using antihypertensive medication (n = 480) at one or more time points. A minimum of 20 ABP readings were required, in concordance with current recommendations [20]. A total of 753 observations met these criteria. Seven observations were excluded due to missing information on psychosocial stressors at work, and 25 observations were excluded because of missing information on covariates. Four observations were excluded due to insufficient working hours (≤21 h) to prevent possible misclassification due to insufficient exposure to psychosocial stressors at work.
Complete data were available for 464 workers and were included in the present analyses. The workers comprising our study population participated in one (n = 263), two (n = 149), or all three (n = 52) time points, for a total of 717 observations. The prevalence of uncontrolled hypertension was calculated using the number of observations as the denominator.
Psychosocial stressors at work
Psychosocial stressors at work were evaluated according to the demand–latitude model using validated scales. Both components of the model, psychological demands and decision latitude, were assessed with the French version of the Job Content Questionnaire (JCQ) [21]. The consistency, reliability, and validity of this instrument have been demonstrated [22, 23]. Psychological demands were measured using five items related to the characteristics of the job load, such as the work pace, the difficulty of the tasks performed, and the frequency of interruptions and conflicting tasks. Decision latitude was evaluated using six items related to the level of decision-making autonomy, learning opportunities and use of intellectual skills. The participants rated each item on a 4-point Likert-type scale. Responses were summed to obtain a total score for psychological demands and decision latitude. Tertile-based variables were created for psychological demands and decision latitude [11]. To examine the effect of job strain, we used cut-offs for high psychological demands (≥24) and low decision latitude (≤72), based on the medians for the general working population of Québec [24]. The passive group comprised workers with low demands and low latitude, the active group comprised workers with high demands and high latitude, and the job strain group comprised workers with high demands and low latitude. Other workers were classified as unexposed.
Ambulatory blood pressure
ABP was measured using the validated Spacelabs 90207 oscillometric device (Produits Médicaux Spacelabs, St-Laurent, Québec, Canada) [25, 26]. In a research office at the participant’s workplace, the device was placed on the participant’s non-dominant arm if the BP difference measured on both arms was less than 10 mmHg. Otherwise, the device was installed on the arm with the highest BP values. ABP was defined as the mean of all readings taken every 15 min and recorded by the Spacelabs monitor during regular working hours. The participants were white-collar workers whose tasks were mainly performed from a seated position. To minimize motion artifacts, clear instructions were given to participants in the case that the monitor performed a reading while they were in a standing position (i.e., they were instructed to stop walking and rest their arm at their side). Uncontrolled hypertension was defined as a mean daytime systolic ABP ≥135 mmHg and/or diastolic ABP ≥85 mmHg for non-diabetic participants and systolic ABP ≥125 mmHg and/or diastolic ABP ≥75 mmHg for diabetic participants [27].
Sociodemographic characteristics and lifestyle-related risk factors
The participants completed a self-reported questionnaire. This questionnaire measured age, gender, education, smoking status, alcohol intake, family history of CVD, and self-reported diabetes. The following categories for age were created: <40 years, 40–49 years, or ≥50 years. Education was categorized as follows: less than college completed, college completed, or university completed. Occupation was categorized as follows: clerical/technician, professional, and executive. Smoking was defined as smoking at least one cigarette daily. Alcohol intake over the past 12 months was classified into three categories: <1 drink weekly, 1–5 drinks weekly, or ≥6 drinks weekly. Family history of CVD was based on the declaration by the participant of a cardiovascular event, such as angina, myocardial infarction, coronary revascularization, or stroke, suffered by their father, mother, brother, or sister before the age of 60 years. The risk factors listed above were assessed using validated protocols [24, 28]. Weight (kg) and height (cm) were measured by a trained research assistant. Body mass index (BMI) was calculated by dividing the participant’s weight in kilograms by their height in meters squared.
Statistical analyses
First, descriptive statistics were computed. Categorical values were expressed as proportions and continuous values in means with standard deviations (SD). Prevalence ratios of uncontrolled hypertension with 95% CIs were computed with generalized estimating equations (GEE) using robust Poisson regression [29]. GEE takes into account individual changes in job strain exposure, covariates, and hypertension control over time and within-subject correlations due to repeated measurements. Models were adjusted for sociodemographic and cardiovascular risk factors (age, education, and family history of CVD) as well as for lifestyle and BP-related risk factors (smoking, BMI, physical inactivity, alcohol intake, and diabetes). Tertiles of psychological demands and decision latitude were analyzed separately and mutually adjusted. Because a priori evidence suggested the plausibility of a gender interaction in the relationship between job strain and uncontrolled hypertension [10, 30,31,32], results were presented separately for men and women. Data from all three time points were pooled. The stability of the association between job strain and the prevalence of uncontrolled hypertension at each time point was examined by entering interaction terms between exposure and time. The p values suggested a constant effect over time (p = 0.29 for men and p = 0.90 for women). A sensitivity analysis was conducted including work hours as a covariate and yielded similar estimates (Supplementary file). Statistical analyses with a two-tailed significance level were conducted using the statistical software package SAS, version 9.4.
Results
Table 1 presents a description of the study population. The participants’ mean age in years was 51.6 (SD = 6.6) for men and 49.6 (SD = 6.3) for women. The prevalence of job strain was 21.3% and was nearly two times higher among women (27.5% vs 15.0%) than men. The mean ABP was 132.7/84.1 mmHg (SD = 11.2/7.9) in men and 126.8/79.6 mmHg (SD = 11.4/8.4) in women. The prevalence of uncontrolled hypertension based on ABP monitoring was 49% and was higher in men than in women (61.6% vs 36.9%).
Table 2 presents the prevalence of uncontrolled hypertension according to job strain exposure. Among men, the prevalence of uncontrolled hypertension was higher in those exposed to job strain (PR = 1.46, 95% CI: 1.07–1.98). The prevalence of uncontrolled hypertension was also higher in those with active jobs (PR = 1.47, 95% CI: 1.12–1.94). In women, there was no association between job strain and the prevalence of uncontrolled hypertension.
Table 3 presents the prevalence of uncontrolled hypertension according to exposure to psychological demands and decision latitude. Both men and women in the highest tertile of psychological demands had a higher prevalence of uncontrolled hypertension after adjustment for decision latitude and sociodemographic and lifestyle-related risk factors. Men in the highest tertile of exposure for psychological demands had a 60% increase in the prevalence of uncontrolled hypertension (PR = 1.60, 95% CI: 1.25–2.06). Women with the same level of exposure to psychological demands also had a 60% increase in the prevalence of uncontrolled hypertension (PR = 1.60, 95% CI: 1.03–2.47). Exposure to low decision latitude was not associated with a statistically significant increase in uncontrolled hypertension in either men or women.
Discussion
In the present study of middle-aged workers treated for hypertension, men exposed to job strain and those with active jobs had a higher prevalence of uncontrolled hypertension than unexposed men. High demands at work were associated with a higher prevalence of uncontrolled hypertension in both men and women.
Uncontrolled hypertension among treated patients is a major public health issue. In the present study, nearly one out of two treated participants (49%) had this condition. This prevalence is noticeably higher than that reported in a previous Canadian study, in which 18% of patients being treated for hypertension had uncontrolled hypertension [5]. The elevated prevalence observed in the present study could be explained by the use of ABP measurements. Indeed, a previous large-scale European study showed that 31% of apparently well-controlled hypertensives at the clinic have uncontrolled hypertension according to ABP monitoring [33]. Therefore, ABP monitoring should be considered the preferred method for accurately assessing uncontrolled hypertension among treated patients.
The findings of the present study suggest that psychosocial stressors at work are important contributors to the alarmingly high prevalence of uncontrolled hypertension among treated patients. Prior to the present study, evidence on this topic was scarce. Mezuk et al. [16] found no association between job strain and BP control in a US sample of aging working men. In that study, the effect of job strain exposure was examined in combination with other work stressors, which could have diluted the effect and thus limits comparison with our results. Moreover, the use of casual BP could also have led to an underestimation of the effect of job strain [10, 19]. A previous study conducted by our group used ABP measurements and reported a higher prevalence of uncontrolled hypertension among workers exposed to psychosocial stressors according to Siegrist’s effort-reward imbalance model [19]. Karasek’s demand–latitude model and the effort-reward imbalance model cover different aspects of the psychosocial environment. The demand–latitude model focuses on task-level characteristics, while Siegrist’s model focuses on broader socioeconomic conditions, such as salary, promotion prospects, and job stability. The present findings provide complementary evidence supporting the effect of adverse psychosocial stressors at work on poor hypertension control among treated workers.
Karasek’s demand–latitude model poses that workers exposed to job strain (a combination of high psychological demands and low decision latitude) are the most vulnerable to developing work-stress-related adverse health effects [34]. The findings of the present study are consistent with this hypothesis, showing a 46% increase in the prevalence of uncontrolled hypertension among men exposed to job strain after sociodemographic and lifestyle-related risk factors were controlled. A higher prevalence of uncontrolled hypertension was also observed among men in active jobs, which are characterized by high psychological demands and high decision latitude. This finding does not fully correspond to Karasek’s proposition [34]. This result may partly be explained by the fact that in some situations, higher autonomy over work may not compensate for the pressure of increased psychological demands at work [35]. The worse cardiovascular profile for active workers observed in the present study is consistent with some previous evidence [31, 36,37,38].
In our study, low decision latitude had no effect on hypertension control in either men or women. This is consistent with some [31, 37, 38], but not all [10], previous studies documenting the effect of this particular exposure on BP. In comparison, high psychological demands were associated with a 60% increase in the prevalence of uncontrolled hypertension among men and women. Comparisons with previous studies should be made with caution because the current study is the first to examine the independent effect of decision latitude and psychological demands on uncontrolled hypertension in a sample composed exclusively of treated workers.
Gender differences have been observed in terms of the adverse impact of high job strain on BP elevation [11] and CVD incidence [39], which is consistent with our results. A recent study conducted among treated workers suggests that job strain could be associated with the rate pressure product (systolic BP × heart rate) in women [40]. Gender differences may be explained by different occupational trajectories among women than among men, which result in less continuous exposure to adverse psychosocial stressors at work [10]. In addition, factors such as marital strain and family responsibilities may interact with psychological demands at work and contribute to explaining the relative importance of this specific work factor on women’s BP control. One previous study showed an interaction between low marital cohesion and high job strain in the elevation of BP among women [41]. Similarly, previous studies have observed that combined exposure to high family responsibilities and high job strain tended to have a greater effect on BP than job strain alone [42, 43].
Limitations should be mentioned. First, the duration of exposure was not taken into account. However, previous studies have shown that, if anything, the deleterious effect of psychosocial exposures is stronger when duration of exposure is considered [10, 15]. Moreover, the possibility of selection bias cannot be entirely ruled out despite the high participation rate at each time point. In the present study, information on the type and number of antihypertensive agents being taken and on treatment adherence was not available. Psychosocial stressors at work could reduce adherence to health recommendations among workers with CVD [44]. However, controlling for adherence would lead to overadjustment because adherence could result from the psychosocial stressors under study (intermediate factor). Finally, because the study population was composed of white-collar workers, generalization of our findings should be restricted to workers sharing similar occupations. It should, however, be noted that the deleterious effect of psychosocial stressors at work on BP was previously observed in different occupational groups (i.e., nurses, bus drivers) [10]. In addition, the proportion of workers exposed to job strain in the present study (21% in the total sample) was comparable to that in other industrialized countries [45]. The composition of our study population had the advantage of minimizing potential confounding from physical work constraints that may influence BP at work.
This study also has several strengths. First, the present study examined, for the first time, the association between psychosocial stressors at work based on the demand–latitude model and uncontrolled hypertension among both men and women. In addition, BP was measured using ambulatory monitoring, which is the gold standard method for assessing hypertension [17, 27]. Daytime ABP was used, which had the advantage of minimizing biases due to low participation or incomplete BP data [46], as supported by the high participation rates obtained at multiple measurement points. It should be noted that a recent systematic review suggested that the deleterious effect of psychosocial stressors at work on BP is of a comparable magnitude whether BP was measured at work, at home, over 24 h or during the daytime [10]. A large set of potential confounders, including known hypertension risk factors, were taken into consideration, minimizing the possibility of strong confounding. Finally, validated scales were used to assess job strain [22, 23], minimizing the possibility of information bias.
The current study has both clinical and public health implications. First, there is a need for increased clinical awareness regarding the negative effect of these work stressors on BP control. The identification of treated patients who are exposed to work stressors could contribute to improving their BP management. For example, ABP monitoring would give a more accurate assessment of BP control than office or home BP measurement. Second, at the population level, preventive interventions that aim to reduce exposure to job strain through organizational changes could be relevant strategies for decreasing the burden of uncontrolled hypertension.
Conclusion
The current study is the first to evaluate the effect of psychosocial stressors at work, based on the demand–latitude model, on the prevalence of uncontrolled hypertension in treated workers using ABP measures. The prevalence of uncontrolled hypertension was higher among workers exposed to psychosocial stressors at work, as described by this model, than among unexposed workers. Addressing these frequent and modifiable adverse workplace exposures should be considered for at-risk and hypertensive patients. Workplace interventions that reduce the prevalence of psychosocial stressors at work could improve BP control at the population level.
References
Bromfield S, Muntner P. High blood pressure: the leading global burden of disease risk factor and the need for worldwide prevention programs. Curr Hypertens Rep. 2013;15:134–6.
Vasan RS, Larson MG, Leip EP, Evans JC, O’Donnell CJ, Kannel WB, et al. Impact of high-normal blood pressure on the risk of cardiovascular disease. N. Engl J Med. 2001;345:1291–7.
Vasan RS, Beiser A, Seshadri S, Larson MG, Kannel WB, D’agostino RB, et al. Residual lifetime risk for developing hypertension in middle-aged women and men: The Framingham Heart Study. JAMA. 2002;287:1003–10.
Gu Q, Burt VL, Dillon CF, Yoon S. Trends in antihypertensive medication use and blood pressure control among United States adults with hypertension: the National Health and Nutrition Examination Survey, 2001 to 2010. Circulation. 2012;126:2105–14.
McAlister FA, Wilkins K, Joffres M, Leenen FH, Fodor G, Gee M, et al. Changes in the rates of awareness, treatment and control of hypertension in Canada over the past two decades. CMAJ. 2011;183:1007–13.
Iyer AS, Ahmed MI, Filippatos GS, Ekundayo OJ, Aban IB, Love TE, et al. Uncontrolled hypertension and increased risk for incident heart failure in older adults with hypertension: findings from a propensity-matched prospective population study. J Am Soc Hypertens. 2010;4:22–31.
Agarwal R, Pappas MK, Sinha AD. Masked uncontrolled hypertension in CKD. J Am Soc Nephrol. 2016;27:924–32.
Zhou D, Xi B, Zhao M, Wang L, Veeranki SP. Uncontrolled hypertension increases risk of all-cause and cardiovascular disease mortality in US adults: the NHANES III Linked Mortality Study. Sci Rep. 2018;8:9418.
Babu GR, Jotheeswaran AT, Mahapatra T, Mahapatra S, Kumar A Sr., Detels R, et al. Is hypertension associated with job strain? A meta-analysis of observational studies. Occup Environ Med. 2014;71:220–7.
Gilbert-Ouimet M, Trudel X, Brisson C, Milot A, Vezina M. Adverse effects of psychosocial work factors on blood pressure: systematic review of studies on demand-control-support and effort-reward imbalance models. Scand J Work Environ Health. 2014;40:109–32.
Landsbergis PA, Dobson M, Koutsouras G, Schnall P. Job strain and ambulatory blood pressure: a meta-analysis and systematic review. Am J Public Health. 2013;103:e61–71.
Nyberg ST, Fransson EI, Heikkila K, Alfredsson L, Casini A, Clays E, et al. Job strain and cardiovascular disease risk factors: meta-analysis of individual-participant data from 47,000 men and women. PLoS ONE. 2013;8:e67323.
Munakata M. Clinical significance of stress-related increase in blood pressure: current evidence in office and out-of-office settings. Hypertens Res. 2018;41:553–69.
Kivimaki M, Nyberg ST, Batty GD, Fransson EI, Heikkila K, Alfredsson L, et al. Job strain as a risk factor for coronary heart disease: a collaborative meta-analysis of individual participant data. Lancet. 2012;380:1491–7.
Aboa-Eboule C, Brisson C, Maunsell E, Masse B, Bourbonnais R, Vezina M, et al. Job strain and risk of acute recurrent coronary heart disease events. JAMA. 2007;298:1652–60.
Mezuk B, Kershaw KN, Hudson D, Lim KA, Ratliff S. Job strain, workplace discrimination, and hypertension among older workers: The Health and Retirement Study. Race Soc Probl. 2011;3:38–50.
Mancia G, Parati G. Office compared with ambulatory blood pressure in assessing response to antihypertensive treatment: a meta-analysis. J Hypertens. 2004;22:435–45.
Trudel X, Gilbert-Ouimet M, Milot A, Duchaine CS, Vezina M, Laurin D, et al. Cohort profile: The PROspective Quebec (PROQ) study on work and health. Int J Epidemiol. 2018;47:693a–i.
Trudel X, Milot A, Gilbert-Ouimet M, Duchaine C, Guenette L, Dalens V, et al. Effort-reward imbalance at work and the prevalence of unsuccessfully treated hypertension among white-collar workers. Am J Epidemiol. 2017;186:456–62.
Cloutier L, Daskalopoulou SS, Padwal RS, Lamarre-Cliche M, Bolli P, McLean D, et al. A new algorithm for the diagnosis of hypertension in Canada. Can J Cardiol. 2015;31:620–30.
Karasek R, Brisson C, Kawakami N, Houtman I, Bongers P, Amick B. The Job Content Questionnaire (JCQ): an instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol. 1998;3:322–55.
Larocque B, Brisson C, Blanchette C. Internal consistency, factorial validity and discriminant validity of the French version of the psychological demands and decision latitude scales of the Karasek “Job Content Questionnaire”. Rev Epidemiol Sante Publique. 1998;46:371–81.
Brisson C, Blanchette C, Guimont C, Dion G, Moisan J, Vézina M, et al. Reliability and validity of the French version of the 18-item Karasek Job Content Questionnaire. Work Stress. 1998;12:322–36.
Daveluy C, Pica L, Audet N, Courtemanche R, Lapointe F. Quebec health and social survey. 2nd ed. Québec: Institut de la statistique du Québec; 2000.
O’Brien E, Coats A, Owens P, Petrie J, Padfield PL, Littler WA, et al. Use and interpretation of ambulatory blood pressure monitoring: recommendations of the British Hypertension Society. BMJ. 2000;320:1128–34.
O’Brien E, Mee F, Atkins N, O’Malley K. Accuracy of the SpaceLabs 90207 determined by the British Hypertension Society protocol. J Hypertens. 1991;9:573–4.
Leung AA, Nerenberg K, Daskalopoulou SS, McBrien K, Zarnke KB, Dasgupta K, et al. Hypertension Canada’s 2016 Canadian Hypertension Education Program Guidelines for blood pressure measurement, diagnosis, assessment of risk, prevention, and treatment of hypertension. Can J Cardiol. 2016;32:569–88.
Daveluy C, Chénard L, Levasseur M, Emond A. Et votre coeur, ca va? Enquête québécoise sur la santé cardiovasculaire [Quebec survey on cardiovascular health] 1990. Montreal: Ministere de la Santé et des Services sociaux, gouvernement du Québec;1994.
Knol MJ, Le Cessie S, Algra A, Vandenbroucke JP, Groenwold RH. Overestimation of risk ratios by odds ratios in trials and cohort studies: alternatives to logistic regression. CMAJ. 2012;184:895–9.
Duchaine C, Ndjaboue R, Levesque M, Vezina M, Trudel X, Gilbert-Ouimet M, et al. Psychosocial work factors and social inequalities in psychological distress: a population-based study. BMC Public Health. 2017;17:91.
Trudel X, Brisson C, Milot A. Job strain and masked hypertension. Psychosom Med. 2010;72:786–93.
Brisson C, Gilbert-Ouimet M, Duchaine C, Trudel X, Vézina M. Workplace interventions aiming to improve psychosocial work factors and related health. Siegrist J., Wahrendorf M. (eds) In: Work stress and health in a globalized economy. Springer; 2016:333–63.
Banegas JR, Ruilope LM, de la Sierra A, de la Cruz JJ, Gorostidi M, Segura J, et al. High prevalence of masked uncontrolled hypertension in people with treated hypertension. Eur Heart J. 2014;35:3304–12.
Karasek RA Jr. Job demands, job decision latitude, and mental strain: Implications for job redesign. Adm Sci Q. 1979;24:285–308.
Trudel X, Brisson C, Milot A, Masse B, Vezina M. Psychosocial work environment and ambulatory blood pressure: independent and combined effect of demand-control and effort-reward imbalance models. Occup Environ Med. 2013;70:815–22.
Riese H, Van Doornen LJ, Houtman IL, De Geus EJ. Job strain in relation to ambulatory blood pressure, heart rate, and heart rate variability among female nurses. Scand J Work Environ Health. 2004;30:477–85.
Grzywacz JG, Alterman T, Gabbard S, Shen R, Nakamoto J, Carroll DJ, et al. Job control, psychological demand, and farmworker health: evidence from the national agricultural workers survey. J Occup Environ Med. 2014;56:66–71.
Uchiyama S, Kurasawa T, Sekizawa T, Nakatsuka H. Job strain and risk of cardiovascular events in treated hypertensive Japanese workers: hypertension follow-up group study. J Occup Health. 2005;47:102.
Backe EM, Seidler A, Latza U, Rossnagel K, Schumann B. The role of psychosocial stress at work for the development of cardiovascular diseases: a systematic review. Int Arch Occup Environ Health. 2012;85:67–79.
Kimura G, Inoue N, Mizuno H, Izumi M, Nagatoya K, Ohtahara A, Munakata M, Workplace Hypertension Co-operative Study by 29 Rosai Hospitals belonging to the Japan Organization of Occupational H, Safety. Increased double product on Monday morning during work. Hypertens Res. 2017;40:671–4.
Tobe SW, Kiss A, Sainsbury S, Jesin M, Geerts R, Baker B. The impact of job strain and marital cohesion on ambulatory blood pressure during 1 year: the double exposure study. Am J Hypertens. 2007;20:148–53.
Brisson C, Laflamme N, Moisan J, Milot A, Mâsse B, Vézina M. Effect of family responsibilities and job strain on ambulatory blood pressure among white-collar women. Psychosom Med. 1999;61:205–13.
Gilbert-Ouimet M, Brisson C, Milot A, Vezina M. Double exposure to adverse psychosocial work factors and high family responsibilities as related to ambulatory blood pressure at work: a 5-year prospective study in women with white-collar jobs. Psychosom Med. 2017;79:593–602.
Dickson VV, Howe A, Deal J, McCarthy MM. The relationship of work, self-care, and quality of life in a sample of older working adults with cardiovascular disease. Heart lung: J Crit care. 2012;41:5–14.
Brisson C, Aboa-Eboulé C, Leroux I, Gilbert-Ouimet M, Vézina M, Bourbonnais R, E. M. Psychosocial factors at work and heart disease. In: Allan R, editor. Heart & mind: the evolution of cardiac psychology” focused on clinical psychology. New-York: Amerian Psychological Association;2011.
Rothman KJ, Greenland S, Lash TL. Modern epidemiology. Philadelphia: Lippincott Williams & Wilkins; 2008.
Acknowledgements
This research was supported by a grant from the Canadian Institutes of Health Research (grant 57750). CB was a Canadian Institutes of Health Research Investigator, and MGO was supported by a Canadian Institutes of Health Research training award when this work was conducted.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Lavigne-Robichaud, M., Trudel, X., Duchaine, C.S. et al. Job strain and the prevalence of uncontrolled hypertension among white-collar workers. Hypertens Res 42, 1616–1623 (2019). https://doi.org/10.1038/s41440-019-0278-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-019-0278-7