Abstract
Membranous nephropathy (MN) is a glomerular disease that can occur at all ages. In adults, it is the most frequent cause of nephrotic syndrome. In ~80% of patients, there is no underlying cause of MN (primary MN) and the remaining cases are associated with medications or other diseases such as systemic lupus erythematosus, hepatitis virus infection or malignancies. MN is an autoimmune disease characterized by a thickening of the glomerular capillary walls due to immune complex deposition. Identification of the phospholipase A2 receptor (PLA2R) as the major antigen in adults in 2009 induced a paradigm shift in disease diagnosis and monitoring and several other antigens have since been characterized. Disease outcome is difficult to predict and around one-third of patients will undergo spontaneous remission. In those at high risk of progression, immunosuppressive therapy with cyclophosphamide plus corticosteroids has substantially reduced the need for kidney replacement therapy. Owing to carcinogenic risk, other treatments (calcineurin inhibitors and CD20-targeted B cell depletion therapy (rituximab)) have been developed. However, disease relapses are frequent when calcineurin inhibitors are stopped and the remission rate with rituximab is lower than with cyclophosphamide, particularly in patients with high PLA2R antibody titres. Other new drugs are already available and antigen-specific immunotherapies are being developed.
Similar content being viewed by others
Introduction
Membranous nephropathy (MN) is a pathologically defined disorder of the kidney glomerulus. The specific lesion is an apparent thickening of the glomerular capillary walls, which results from immune complex formation on the outer aspect of the basement membrane1. The immune deposits consist of immunoglobulin G (IgG), the relevant antigens and complement components, including the membrane attack complex (MAC). The consequence of the immunological conflict is the loss of large amounts of proteins in the urine (proteinuria), which is predominantly mediated by the pathophysiological disturbance of the podocyte structure caused by immune complex deposition and MAC formation. Patients experience a decrease in serum albumin levels and generalized oedema, which define a condition called nephrotic syndrome. Most patients report fatigue as an important symptom. MN accounts for ~30% of cases of nephrotic syndrome in adults and is only surpassed in prevalence among nephrotic non-diabetic glomerular diseases by podocytopathy presenting as focal and segmental glomerulosclerosis lesions in some populations (African and Hispanic American individuals). In ~80% of patients, there is no underlying cause of MN (primary MN (pMN)) and 20% are associated with medications, such as NSAIDs, or other diseases (secondary MN (sMN)) such as lupus (also referred to as systemic lupus erythematosus (SLE)), hepatitis B or hepatitis C, and malignancies1.
Patient outcomes are variable. For a long time, outcome was governed by the rule of thirds, with a third of the patients undergoing spontaneous remission, a third keeping variable levels of proteinuria and the remaining third progressing to advanced kidney failure. However, immunosuppressive therapy has substantially reduced the rate of kidney replacement therapy, which is ~10% with cyclophosphamide treatment but is not yet established for other newer agents such as rituximab1.
Substantial advances in the understanding of MN pathophysiology have occurred in the past two decades, starting with the identification of neutral endopeptidase (NEP), the first discovered human podocyte antigen, which is involved in a rare subset of patients with neonatal allo-immune MN2. This finding paved the way for the characterization of the M-type phospholipase A2 receptor (PLA2R) as another podocyte antigen in 2009. Antibodies to PLA2R are specific for MN and found in ~70% of adult patients with the disease3. This discovery demonstrated that pMN is an autoimmune disease in which the podocyte is both the target of circulating auto-antibodies and probably the main source of the auto-antigen. It induced a paradigm shift in thinking about establishing diagnosis (possibly without a kidney biopsy), predicting outcome and monitoring treatment in patients with pMN, including after transplantation. This discovery resulted in the rapid development of reliable assays for PLA2R antibodies and pMN can be considered as a model of organ-specific autoimmune disease and of personalized medicine. Subsequently, another podocyte antigen, thrombospondin type 1 domain-containing 7A (THSD7A) was identified4. THSD7A accounts for <5% of pMN4.
Owing to the technological advances in combining laser microdissection of glomeruli and mass spectrometry of solubilized digested proteins, several further antigens have been identified such as exostosin 1 (EXT1) and EXT2, protein kinase C-binding protein NELL1 (also known as neural epidermal growth factor like 1 protein), semaphorin 3B (SEMA3B), neural cell adhesion molecule 1 (NCAM1), protocadherin 7 (PCDH7) and serine protease HTRA1 (refs5,6). These antigens, like PLA2R and THSD7A, can be associated with pMN or with a specific ‘cause’ of sMN, such as lupus, other autoimmune disease or cancer, recognizing that the link of causality is not established in many instances. The discovery of different antigens therefore challenges the classification that opposes pMN to sMN and leads to a discussion of an antigen-based classification in which each antigen-associated MN would have its specific immunological profile (IgG subclass), pattern of associated diseases and outcome. Future studies should evaluate whether management should be driven by the antigen specificity as is the case for PLA2R-associated MN, in which positive serology now replaces kidney biopsy and quantitative assessment of PLA2R antibody levels is helpful in predicting response to therapy. Within the coming few years, similar steps forward can be expected for the other antigens (although they are rarer and large patient cohorts will not be recruited). Thus, in this Primer, we adhere to the current nomenclature of pMN and sMN, while being mindful that it will need to be adapted based on evidence from future studies.
Despite these advances, treatment of MN remains controversial. For a long time, cyclophosphamide-based regimens were the standard of care as they have been shown to prevent the occurrence of advanced kidney failure; however, they expose patients to an increased risk of malignancy1,7. Treatment with calcineurin inhibitors (CNIs), such as cyclosporine or tacrolimus, induces a high rate of remission but with a high rate of relapse and renal toxic effects are a concern in prolonged treatment1,7. Therapy protocols with CD20-targeted agents, such as rituximab, are well tolerated but only 60–70% of patients reach persistent clinical remission compared with ~80% for cyclophosphamide and their efficacy in preventing kidney disease progression has not yet been proven1,7. Randomized controlled trials (RCTs) published in the past few years (GEMRITUX8, MENTOR9, STARMEN10 and RI-CYCLO11) have not clarified the dilemma between cyclophosphamide (more toxic) and CD20-targeted therapy (less efficient in the protocols used), which calls for new therapeutic approaches. The lack of RCTs with sufficient statistical power that directly compare these two treatments is a major reason for the enduring uncertainty. Furthermore, the dosage of rituximab is important to consider when effectivity is studied.
In this Primer, we summarize current knowledge of the epidemiology of MN and highlight the major advances that have led to a better understanding of MN pathophysiology, diagnosis and improved patient care. We also identify the major gaps in current knowledge and provide recommendations on how to improve long-term renal prognosis and quality of life.
Epidemiology
Incidence, prevalence and natural history
MN occurs in all regions and all ethnicities. The data on the incidence of MN and MN subtypes remain quite limited as large population-based studies that are representative across diverse international populations are not available. The annual incidence rates of MN are estimated at 10–12 per million in North America and 2–17 per million in Europe7,12,13,14,15. The disease affects individuals of all ages with a mean age of diagnosis at 50–60 years16 and a 2:1 male predominance for unknown reasons17. Whether incidence rates of MN vary between regions or ethnicities remains unclear as most data are from North America and Europe.
pMN is the most common cause of idiopathic nephrotic syndrome in non-diabetic adults worldwide, accounting for 20–37% in most kidney biopsy series and increasing to as high as 58% in adults >65 years of age7,18,19. MN is uncommon in children, accounting for <7% of biopsies13,20,21,22,23,24, and is often associated with other diseases such as hepatitis B24. The percentage of PLA2R-associated MN in adolescents is similar to that of adults.
No good data are available on the prevalence of the various aetiologies of sMN1,25. The main reason is that the epidemiology has varied with time, with infectious causes, such as hepatitis, strongly decreasing with vaccination, whereas others, such as lupus and drug exposure, are increasing.
In some regions, a temporal change in prevalence of MN has been reported18,26,27. A study in China analysed data from kidney biopsy samples of 71,151 patients in 938 hospitals in 282 cities taken over 11 years (2004–2014) encompassing all age groups17. The prevalence of MN increased by 13% annually, whereas the proportions of other major glomerulopathies remained stable. Areas with higher levels of fine particulate matter with diameters ≤2.5 µm (PM2.5) air pollution had the highest rates of MN. In areas with PM2.5 levels >70 μg/m3, each 10 μg/m3 increase in PM2.5 concentration was associated with 14% higher odds for MN. This association was subsequently confirmed by another study in China28. However, whether the increase of MN is connected to a PLA2R-driven mechanism remains unclear as serum PLA2R antibody levels were not measured in most patients in these studies and whether air pollution is a causative risk of MN requires further confirmation.
The natural history of untreated MN has been reported with spontaneous complete remission rates of 20–30% and 10-year renal survival rates of 60–80% in most studies29,30,31. Despite its ‘benign’ presentation characteristics, MN has, for a long time, remained the second or third leading cause of kidney failure among the primary glomerulonephritis types in the USA and Europe32. In patients who continue to have nephrotic syndrome, kidney failure develops in 40–50% over a period of 10 years33. These patients are also at an increased risk of life-threatening thromboembolic and cardiovascular events34.
Genetic factors
MN is not a typical hereditary disease in Mendelian terms but there is growing evidence to support a strong genetic component. Like most autoimmune diseases, MN has a strong association with the class II antigens of the human leukocyte antigen (HLA) system that are encoded by the relevant alleles of the HLA-D locus on chromosome 6. HLA class II molecules are involved in the regulation of immune responses: their expression is mostly limited to antigen-presenting cells, such as B cells, monocytes, macrophages, dendritic cells and Langerhans cells of the skin, and their role is to present peptide antigens to the immune system. Thus, they are associated with autoimmune diseases. It has been known since 1979 and 1989 that MN is strongly associated with HLA-DR3 and HLA-DQA1, respectively, in Caucasian populations35,36. An initial genome-wide association study conducted in three European cohorts including 556 patients of white ancestry found that pMN in adults was strongly correlated with risk alleles in HLA-DQA1 (chromosome 6) and in PLA2R1 (chromosome 2)37. In individuals who were homozygous for the lead risk alleles, the risk of having MN was nearly 80-fold higher than in those who had neither risk allele. Interestingly, the risk allele that is most significantly associated with pMN is localized in an intron of the gene; thus, this allele is not expected to change PLA2R antigen auto-reactivity. Further studies did not detect mutations or rare variants in the sequence and the splice sites of PLA2R1 (ref.38). Thus, it is unlikely that the immune reaction is triggered by a change in antigen sequence or conformation. It is more probable that post-translational modifications or increased expression of PLA2R antigen in podocytes or other cells have an important role.
A similar strong correlation between risk alleles of PLA2R1 and HLA-DQA1 and the risk of developing MN was found in a large Chinese cohort that included 1,112 patients with pMN and 1,020 healthy individuals39. Patients with both risk alleles had an >11-fold increased risk of developing MN. The presence of risk alleles was also correlated to PLA2R antibodies.
Two studies performed in Chinese cohorts revealed different HLA class II alleles associated with an increased risk of MN40,41 and proposed that HLA associations may differ between ethnicities. This was corroborated in the largest international genetic study of MN performed to date. The study involved cohorts from East Asia (1,632 biopsy specimen-diagnosed cases and 3,209 controls) and of European ancestry (2,150 biopsy specimen-diagnosed cases and 5,829 controls) and found ethnic differences in HLA locus associations, defining DRB1*1501 as a major risk allele in East Asian individuals, DQA1*0501 in European individuals and DRB1*0301 in both ethnicities42. The PLA2R1 locus presented the most strongly associated non-HLA signals. In addition, two previously unreported loci, NFKB1 and IRF4, which are both linked to inflammatory pathways, were identified. Genome-wide association study loci account for 32% and 25% of disease risk in East Asian and European individuals, respectively.
In addition to their likely role of presenting PLA2R antigen to the immune system, HLA-D alleles may also be modifiers of MN. Although DRB1*1501 is a major risk allele for the disease, DRB1*1502, which differs from DRB1*1501 by a single amino acid, is not. However, DRB1*1502 has a strong predictive value when associated with HLA risk alleles, being associated with a lower estimated glomerular filtration rate (GFR) and a higher risk of kidney failure43. No data are available concerning genetic predisposition for the other antigens or sMN.
Mechanisms/pathophysiology
In the past 20 years, considerable advances have occurred in the understanding of the pathophysiology of MN with the description of the first podocyte antigens in neonatal2 and adult3 MN. These discoveries revealed the central role of the podocyte in MN pathogenesis. This section describes the classical antigens NEP, PLA2R and THSD7A, the newly reported potential antigens, the autoimmune reactions that lead to the development of antibodies, and the downstream events that lead to nephropathy.
Antigens
NEP
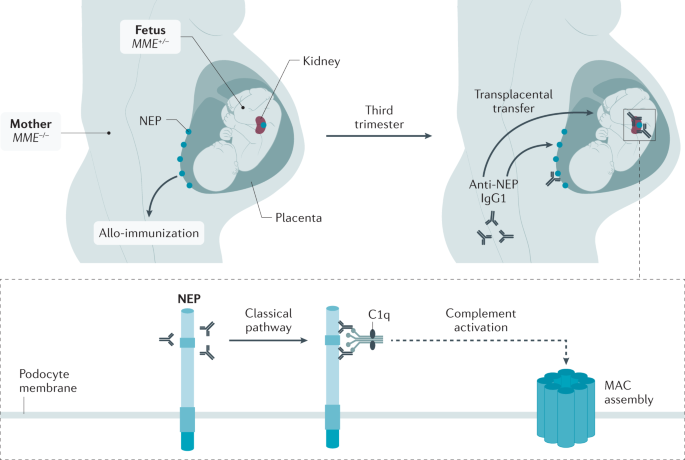
In the 1970s, studies in the Heymann nephritis rat model of MN established the basis of MN pathophysiology. The studies showed that rats express megalin both in the proximal tubular brush-border and in podocytes and that actively or passively introduced megalin antibodies induced the aggregation of immune complexes at the basal surface of podocytes. This observation has led to the concept that a podocyte antigen, megalin (now called LRP2), could serve as a target of circulating antibodies leading to the in situ formation of immune complexes44,45,46. In humans, where megalin is not or only weakly present on podocytes36,47 and cannot therefore be the target of circulating antibodies, NEP was identified in 2002 as the responsible antigen in a subset of patients with allo-immune antenatal MN2. In this rare condition, mothers carry a homozygous or compound heterozygous nonsense mutation in MME (encoding NEP), which results in the absence of the protein48 (Fig. 1). During pregnancy, they become immunized to the paternally inherited NEP in the placenta and the resulting maternal IgG antibodies are then transferred to the fetus, which is not NEP-deficient and therefore develops active disease.
Antenatal membranous nephropathy is the result of a homozygous or compound heterozygous nonsense mutation in MME (encoding neutral endopeptidase (NEP)) in the pregnant mother, which results in the absence of NEP. The MME–/– pregnant mother develops allo-imunization against NEP that is expressed by the placenta (via paternal inheritance to the fetus) and recognized as a non-self protein by the mother’s immune system. In the third trimester of pregnancy, NEP antibodies are transferred to the MME+/– fetus and bind to the NEP antigen expressed on podocytes of the fetus, who develops active disease. NEP IgG1 antibodies bind to epitopes on NEP and activate the classical complement pathway through binding of complement component C1q to the NEP IgG1 antibodies, leading to the formation of C5b–9 (membrane attack complex of complement (MAC)). MAC insertion into the podocyte membrane induces cell damage. No podocyte damage occurs in fetuses from mothers producing only IgG4, which does not bind C1q and therefore fails to activate the complement cascade.
NEP is a membrane-bound zinc-dependent endopeptidase and is involved in the catabolism of regulatory peptides with vasoactive properties49,50. NEP is expressed in numerous tissues and its membrane form is naturally present on human podocytes at the sole of their foot processes51. Maternal production of complement-fixing NEP IgG1, which also inhibits NEP enzyme activity, is necessary for the disease to develop52. This suggests that some toxic effects of NEP antibodies may be associated with alterations of glomerular haemodynamics, endothelial permeability or tubular function. Analysis of these very rare cases strongly supports the idea that the circulating antibodies react with an intrinsic component of the podocyte membrane. Moreover, these observations suggest that similar truncating mutations of other podocyte antigens could lead to allo-immunization and renal disease in infants.
PLA2R
PLA2R is the most frequently targeted auto-antigen in MN (up to 80% of pMN cases) (Table 1). The antigen was initially identified by mass spectrometric analysis of an electrophoretic gel band that corresponded to a glycoprotein recognized by serum from patients with idiopathic (primary) MN but not by serum from patients with proteinuria or healthy controls3. PLA2R is a transmembrane glycoprotein abundantly expressed by the human podocyte3, present at the level of the foot process as well as on the apical surface, where it can be shed into the urine in vesicular structures during disease53. Its specific role in the glomerulus is not known. As some small mammals lack constitutive podocyte PLA2R expression, PLA2R may not be essential to podocyte function. Initially identified as a receptor for secreted phospholipase A2 enzymes54, PLA2R might bind and internalize these small and potentially toxic enzymes that pass through the glomerular basement membrane (GBM). The extracellular domain of PLA2R comprises 10 domains: an N-terminal cysteine-rich (CysR) domain, a fibronectin 2 domain and eight C-type lectin-like domains (CTLD) that harbour distinct humoral epitopes.
The auto-antibodies that form against PLA2R initially target the N-terminal immunodominant CysR region and a short amino acid sequence in this domain has been shown to stimulate the production of very high-affinity antibodies55. In most patients, epitope spreading and the production of antibodies to distal regions of the extracellular domain occurs, including CTLD1, CTLD7 and CTLD8 (refs56,57). The detection of epitope spreading in a patient seems to confer an inferior prognosis compared with individuals who have CysR antibodies only58, although this notion has been challenged57. The predominant antibodies to PLA2R are of the IgG4 subclass but other subclasses, such as IgG1 and IgG3, are present in lower amounts3,59. Quantification of the overall titre of PLA2R antibodies has been a useful tool in monitoring the immune response to therapy in PLA2R-associated MN13 and the decline and disappearance of PLA2R antibodies has been termed immunological remission and precedes and predicts clinical remission.
THSD7A
Thrombospondin type 1 domain-containing 7A (THSD7A) is a multidomain transmembrane glycoprotein expressed by the podocyte that serves as an auto-antigen in 2–3% of patients with MN60. Similar to PLA2R, it was identified by performing mass spectrometry on native, deglycosylated or proteolysed protein bands detectable by human auto-antibodies. Its presence in the glomerulus had not been demonstrated before its discovery as an MN target antigen, although it is now recognized as a conserved basal component of the podocyte, localizing directly between the slit diaphragm and the GBM61. No immunodominant epitope has been discovered and auto-antibodies seem to target multiple regions of the protein, including the N terminus62. Several cases of THSD7A-associated MN have been found in which a malignancy overexpresses THSD7A and may initiate the immune response that then causes MN in the kidney63,64. There are fewer data on using THSD7A antibodies than on PLA2R antibodies for monitoring of disease but THSD7A antibodies, similar to PLA2R antibodies, tend to decline with immunosuppressive treatment and their disappearance is associated with eventual clinical remission.
New and putative antigens
Laser microdissection of glomeruli followed by mass spectrometry has been used to identify novel antigens in MN65. The basic premise in the identification of an antigen is that the novel antigen has accumulated in the glomeruli (immune deposits) compared with other proteins and is unique to a subset of MN. Confirmation of the novel antigen is then provided by immunohistochemistry and/or immunofluorescence studies that show granular subepithelial staining of the novel antigen along the capillary walls, followed by confocal immunofluorescence studies that show co-localization of the novel antigen with IgG along the capillary walls, ideally elution of IgG from frozen biopsy material to show that the deposited IgG is specific for the novel antigen and, finally, serum western blot analysis to show that circulating antibodies to the novel antigen are present in the serum.
Six candidate antigens have been discovered using these techniques in the past few years (Table 1). Putative antigens EXT1 and EXT2 were discovered in 2019, NELL1 and SEMA3B in 2020, and PCDH7, HTRA1 and NCAM1 in 2021. EXT1 and EXT2 were the first novel proteins found in a subset of patients with MN. Granular EXT1 and EXT2 deposits were detected in MN secondary to autoimmune disease, mostly lupus65. Patients with MN associated with EXT1 and EXT2 deposits were young, predominantly female and their kidney biopsy samples showed features of MN usually associated with an autoimmune disease such as a full-house pattern of immunoglobulin on immunofluorescence studies, tubuloreticular inclusions in the endothelial cells and mesangial deposits. However, antibodies to EXT1 and EXT2 have yet to be found and these proteins are considered putative antigens. Positive staining for EXT1 and/or EXT2 is found in 30–40% of pure lupus MN (LMN; also referred to class V lupus nephropathy) and in around the same percentage of mixed class lupus nephropathy, that is, class III or class IV associated with class V. Patients with LMN and positive staining for EXT1 or EXT2 have fewer chronicity features, including glomerulosclerosis, tubular atrophy and interstitial fibrosis, and also have a better prognosis than those who are negative for EXT1 and EXT2 (refs66,67).
NELL1 seems to be the second most common antigen following PLA2R. It is present in most patients with MN and no underlying disease association (pMN) but is also present in some patients with malignancy (sMN)68,69. One of the unique features of kidney biopsy samples is that staining for NELL1 can be segmental in some of the glomeruli69,70.
SEMA3B is another unique antigen in that it is primarily present in children (<2 years of age) and young adults. In children, kidney biopsy samples also show IgG staining along the tubular basement membrane. Interestingly, the tubular basement membrane deposits are negative for SEMA3B71. NCAM1 was identified as an antigen in both pMN and LMN72. Patients with NCAM1-associated LMN were younger, predominantly female and had a history of lupus, all of which are distinct features from those seen in the usual patients with MN. Similar to LMN associated with EXT1 and EXT2, NCAM1-associated LMN is not restricted to pure class V LMN but is also present in some patients with LMN who also have proliferative lupus nephritis.
PCDH7-associated MN is present in patients with a mean age of 63 years, close to that of the most common form of MN73. Most patients seem to not have an associated underlying disease but ~20% of patients with PCDH7-associated MN have a history of malignancy. Kidney biopsy samples lack complement deposits on immunofluorescence study. In addition, non-nephrotic-range proteinuria (proteinuria <3 g/day) is observed and remission follows conservative management in some patients with PCDH7-associated MN.
HTRA1-associated MN is present in patients with a mean age of 67 years and characterized by an IgG4-dominant subclass in the immune deposits without association to another disease except for anti-neutrophil cytoplasmic antibody-associated vasculitis in 1 of 14 patients74. Sera from two patients reacted by immunoblotting with glomerular extracts and with recombinant human HTRA1 under reducing and non-reducing conditions. Longitudinal sampling in these two patients suggests that HTRA1 antibody levels are correlated with clinical activity.
Whether these new antigens are true antigens or biomarkers is controversial as they have only been characterized in the past few years. As described, each antigen-associated MN has its own specific features, including demographic characteristics, immunopathological and sometimes morphological features, and associated diseases. The minimal definition of an antigen is the presence of the relevant antibodies in the blood and, ideally, in biopsy samples. Although co-localization of antigen and antibody by confocal microscopy is suggestive, definitive evidence of the reactivity of the deposited antibody against the potential antigen requires elution experiments that are hampered by the small size of the tissue specimen. Among the new potential antigens, such demonstration has only been achieved for PCDH7 (ref.73). Further evidence of the pathogenic effect of the antibodies can be provided by correlation of antibody levels with clinical course, early recurrence in the transplanted kidney and development of experimental models. A few cases showing the parallel outcomes of immunological and clinical activity have been reported69,71,73,74. No observation of early recurrence after transplantation has been reported and animal models are not yet available.
Of note, more than a decade after the discovery of PLA2R, the only experimental model of PLA2R-associated MN is with the mouse antigen75 and evidence of pathogenicity in humans mostly relies on early recurrence after transplantation76,77 and time-course measurement of PLA2R antibody levels that precedes proteinuria78,79. Yet, the discovery of the role of the PLA2R antibody in MN has induced a paradigm shift in patient care, showing the way for future well-conducted clinical studies that aim to define the diagnostic and predictive values of potential antigens involved in MN. The pathophysiology of these new antigens is essentially unknown and will require further studies.
Exogenous antigens
Exogenous proteins, whether they are present or not in humans, can induce the production of allo-antibodies or xeno-antibodies, respectively. Important features of these proteins are their specific physicochemical properties that may lead to their trapping in the GBM. The first observation implicating a food antigen was reported in children with cationic bovine serum albumin (BSA)-related MN80. This observation was also inspired by an experimental model81,82. Some patients, mostly infants, with MN had high serum titres of anti-BSA antibodies reacting with one peptide region of BSA but not with human serum albumin. Only infants had circulating cationic BSA, which could interact with the negatively charged glomerular capillary wall. Why cationic BSA was formed is not known but differences in food processing or in the intestinal microbiota might be responsible for BSA modifications.
Other food antigens or non-dietary antigens from the environment might also be involved in MN. Extremely rare forms of allo-immune MN have been described in children affected with rare lysosomal storage diseases (mucopolysaccharidosis type VI and Pompe disease) receiving enzyme replacement therapy83,84. Because of the absence of enzymes, therapeutic proteins are potential allo-antigens that trigger immunization.
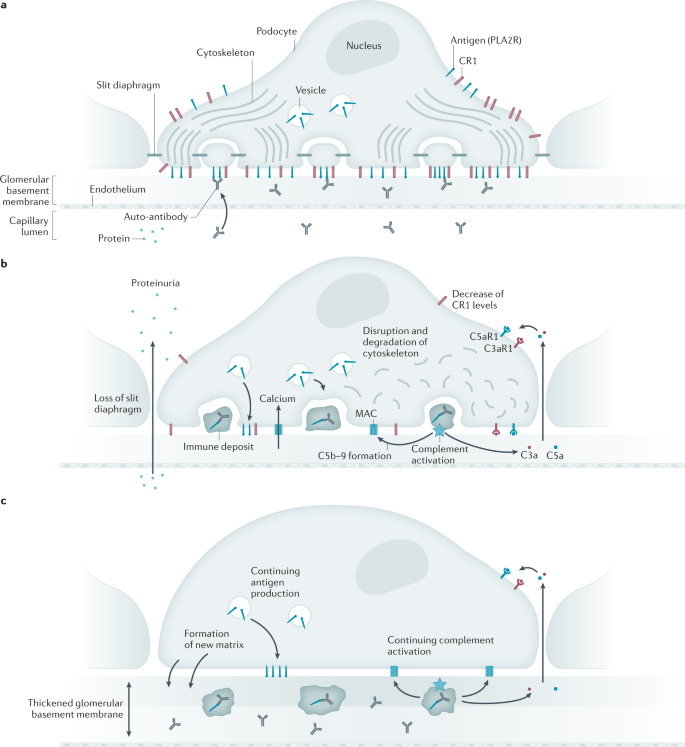
Autoimmune reactions
Regardless of the target antigen, the common denominator in MN is the accumulation of discrete deposits containing immunoglobulin and antigen that form and expand beneath the basal surface of the podocyte (Fig. 2). The mechanisms underlying the loss of tolerance to these self-antigens are not well understood but likely involve genetic factors, heightened expression of target antigens owing to polymorphisms in regulatory elements, upregulation by environmental factors, or even pathologic and dysregulated production of the antigen as might occur in malignancy. It is also not known why some patients have circulating antibodies well before the onset of nephrotic syndrome and even proteinuria85.
a | At the initiation of the humoral autoimmune response, the podocyte expresses phospholipase A2 receptor (PLA2R) and complement inhibitors such as complement receptor 1 (CR1) at the cell surface and has a cytoskeleton reflective of the differentiated podocyte state, with interdigitating foot processes bridged by slit diaphragms. Circulating auto-antibodies begin to target PLA2R on the basal aspect of the podocyte. Ongoing synthesis and delivery of PLA2R to the cell surface enables continued deposit formation and growth in the presence of circulating auto-antibodies. b | Immune deposits (stage 1) containing antigen and immunoglobulin form beneath the podocyte, where they begin to activate complement. The terminal complement components C5b–9 (membrane attack complex (MAC)) insert into the podocyte membrane and enable calcium influx, which initiates several maladaptive pathways. C3a and C5a generated by the complement cascade bind to and activate their cognate receptors C3aR1 and C5aR1, stimulating pathways that lead to the degradation of cytoskeletal elements. CR1 is downregulated, which enables complement-mediated cytotoxicity. The result is the simplification of the podocyte cyto-architecture, loss of slit diaphragms and increased flux of protein into the urinary space. PLA2R continues to be produced by the podocyte, leading to an increased mass of the immune deposits and ongoing complement activation. c | With ongoing injury, the podocyte secretes additional extracellular matrix components between (stage 2) and around (stage 3) the immune deposits, leading to the increased overall thickness of the glomerular basement membrane.
Several studies suggest an overall dysregulated immune phenotype in MN86,87 characterized by a decreased proportion of regulatory T cells among all lymphocyte subpopulations in untreated patients with MN88. Numbers of plasma cells and regulatory B cells were statistically higher in patients with MN compared with healthy individuals or individuals with non-immune kidney disease and the amount of in vitro-expanded PLA2R-specific memory B cells could be correlated with circulating PLA2R antibody titres89. The specific site at which the immune response to PLA2R is initiated remains speculative90 but intrarenal B cells in tertiary lymphoid follicles have been noted91,92. These tertiary follicles could represent the propagation of the immune response triggered by PLA2R shed from podocytes as exosomes into the tubular lumen93 and later captured by intrarenal dendritic cells. The observation that the risk of recurrence after kidney transplantation is dependent on the donor’s gene variants of HLA-D and PLA2R1 can be seen as further evidence of a kidney-based source of antigen exposure90.
The paradigm of podocyte injury induced by the subepithelial immune deposits was elucidated in the experimental rat model of Heymann nephritis94. In this model, activation of the complement system and assembly of the terminal complement components C5b–9 were both necessary to induce podocyte injury and proteinuria. In the absence of complement-activating IgG or factors such as complement component C6, subepithelial deposits would form but no further injury would occur. Evidence for complement activation in human MN has been circumstantial and based on the consistent presence of specific complement factors within the subepithelial deposits. In routine immunofluorescence staining, IgG and C3 are present but C1q is usually weak or absent, suggesting that the classical complement pathway activation has a minor role in established disease. However, the fact that early deposits contain more IgG1 and IgG3 whereas later-stage deposits are enriched in IgG4 suggests that the classical complement pathway might initiate disease, which is then propagated by the alternative pathway or the lectin pathway95. The consistent presence of C4 (ref.96) and of mannan-binding lectin (MBL) in many97 but not all98 patients with MN implicates the lectin pathway, but many components of the alternative pathway are also detected when assayed by mass spectrometric techniques99. The common final pathway is thought to involve the insertion of C5b–9 (also known as the MAC) channels into the podocyte membrane. This breach of cell integrity causes sublethal cell injury and the activation of maladaptive pathways causing cytoskeletal disassembly, loss of slit diaphragms and, over time, the production of normal and ectopic basement membrane elements100.
Mouse models using passive transfer of human or rabbit antibodies to PLA2R75 or THSD7A101,102 have been developed but they have not yet convincingly established a definite role for complement. Sophisticated co-culture models, such as the glomerulus-on-a-chip, hold promise for investigating the harmful effects of human anti-podocyte antibodies103. In a culture model of PLA2R-expressing podocytes, PLA2R IgG4 antibodies, especially those bearing glycan chains that lack terminal galactose residues, stimulated the lectin pathway through MBL and MBL-associated serine proteases to cause podocyte injury104. A novel finding from this work is the upregulation of receptors for C3a and C5a on the podocyte, also observed in human MN biopsy specimens, that may augment the cytotoxicity instigated by C5b–9 through cytoskeletal degradation in response to the anaphylatoxins generated by subepithelial activation of complement.
Research continues into non-complement-dependent mechanisms, for example, direct interference in normal pathways by the auto-antibodies. THSD7A antibodies seem likely to have direct effects on the slit diaphragm structure and function102,103 given the close association of THSD7A with this structure. Intermolecular epitope spreading to intracellular antigens105 or complement regulatory factors106 may also augment the injury process.
Nephropathy
The downstream effects of injury caused by the subepithelial deposits are enormous, starting with the failure of the glomerular filtration barrier owing to the complement-mediated podocyte injury and the spilling of massive amounts of protein into more distal nephron segments. One consequence of delivery of these large amounts of protein, including specific proteases, to the distal nephron is the activation of the epithelial sodium channel ENaC, which is responsible for sodium reabsorption in the collecting duct, causing volume overload, weight gain, and localized oedema or generalized anasarca. The imbalance of promoters and inhibitors of the coagulation system in the setting of increased urinary losses and hepatic synthesis favours the thrombophilic state, which is more pronounced in MN than in other nephrotic disorders for as yet unknown reasons107,108. Deep vein thromboses, renal vein thrombosis and pulmonary embolism are all potential consequences of the nephrotic state in MN and are associated with the severity of hypoalbuminaemia108,109. Other consequences of the nephrotic state include mixed hyperlipidaemia, vitamin D deficiency and a general state of immunosuppression due to urinary loss of innate and humoral immune effectors such as complement factors and immunoglobulins. Similar to other glomerular diseases with sustained proteinuria over months to years, renal function can decline with progressive tubular atrophy and interstitial fibrosis33. Patients who develop end-stage MN and receive a kidney transplant are at risk of recurrence of the disease in the allograft if the circulating antibodies are still present or recur after transplantation.
Diagnosis, screening and prevention
Adults
Clinical presentation
Nephrotic syndrome, defined as proteinuria >3.5 g per day and serum albumin <3.5 g/dl (when measured by bromocresol green) or <3.0 g/dl (when measured by bromocresol purple or immunonephelometric methods), respectively, is present in around two-thirds of patients with MN at presentation and can be severe1,110. The other third of patients present with asymptomatic proteinuria, usually ≤3.5 g per day. In most patients, GFR is normal and urinary sediment is unremarkable, although microscopic haematuria may be present in <25% of patients. Hypertension at presentation is uncommon (<20% of patients), which explains why most patients do not tolerate high-dose angiotensin II blockade. Thromboembolic events are reported in up to 8% of patients, with renal vein thrombosis accounting for 30% (Box 1). Hyperlipidaemia is common and characterized by an increase in total and LDL cholesterol and a decrease in HDLs, which is associated with a markedly increased risk of both myocardial infarction and coronary death compared with that of healthy individuals as well as with an increased risk for thromboembolism111. Rare cases of crescentic MN, usually presenting with proteinuria >3.5 g per day, haematuria and reduced GFR, in the absence of anti-neutrophil cytoplasmic antibodies or GBM antibodies, have been reported112.
Histopathology
Kidney biopsy is the standard diagnostic approach for MN. On light microscopy, early stages of MN may show normal-appearing GBMs113. At later stages, basement membrane spikes and pinholes can be seen on silver methenamine and periodic acid-Schiff stains (Fig. 3).
a | Light microscopy image showing thickened glomerular basement membranes (arrows; periodic acid-Schiff stain, 40×). b | Immunofluorescence microscopy image showing granular staining for IgG along the capillary walls (40×). c | Electron microscopy image showing subepithelial electron-dense deposits (black arrows) and basement membrane material between the electron-dense deposits (white arrows; 4,800×). d | Immunofluorescence microscopy image showing staining for phospholipase A2 receptor (PLA2R) along the capillary walls (40×).
Proliferative features, such as mesangial and endocapillary proliferation, are typically absent113. In very rare cases, a concurrent crescentic pattern of injury is observed. In immunofluorescence microscopy, diffuse and granular staining for IgG, C3, and κ and λ light chains is seen along the capillary walls in pMN. In electron microscopy, numerous electron-dense deposits are seen in the basement membrane beneath the podocytes that show extensive foot process effacement even at the early stages. These subepithelial deposits are separated by expansions of basement membrane material or covered with extracellular matrix at later stages114.
Four stages are defined according to the location of the subepithelial deposits and matrix accumulation: stage 1, sparse small deposits without thickening of the GBM; stage 2, more extensive subepithelial deposits with the formation of basement membrane spikes between the deposits and thickening of the GBM; stage 3, a combination of stage 2 with deposits completely surrounded by basement membrane (intramembranous deposits); and stage 4, incorporation of deposits in the GBM, which are irregularly thickened (burned-out disease). In stage 4, the deposits are often fading, becoming less electron dense.
Features suggestive of sMN include mesangial or endocapillary proliferation; a full-house pattern of immunoglobulin staining, including staining for IgA and C1q on immunofluorescence microscopy; mesangial and/or subendothelial electron-dense deposits or deposits along the tubular basement membrane and vessel walls; substructures in the deposits; and endothelial tubuloreticular inclusions on electron microscopy115. The presence of scant superficially scattered subepithelial deposits on electron microscopy suggests drug-associated or malignancy-associated sMN. Staining for IgG subclasses may help in differentiating pMN from sMN. IgG1, IgG2 and IgG3 predominate in class V lupus nephritis, whereas IgG4 is the prevailing subclass associated with variable amounts of IgG1 in PLA2R-associated and THSD7A-associated pMN69,71,116. The prevailing subclass in MN associated with newly characterized antigens is IgG1 (ref.117). In early reports in malignancy-associated sMN, IgG4 staining was usually absent118. However, one study found no differences in the IgG subclass distribution between patients with pMN and those with malignancy-associated sMN119. Furthermore, levels of antigen-specific IgG4 antibodies were not different between primary and malignancy-associated sMN and levels of all IgG subclasses did not differ between these groups.
Staining of kidney biopsy samples for PLA2R can also diagnose PLA2R-associated MN in patients who have negative PLA2R antibody serology80. This might occur if serum samples are collected when the patient is in immunological remission either spontaneously or following immunosuppressive therapy or PLA2R antibody serology may be falsely negative early in the disease course owing to the phenomenon of the kidney behaving like a ‘sink’120. In this scenario, circulating PLA2R antibodies bind to the target antigens on the podocyte and are rapidly cleared from the blood. Only when the antibody production rate exceeds the buffering capacity of the kidney will seropositivity become apparent. Hence, serial assessment of PLA2R antibody levels should be performed in patients with positive glomerular PLA2R staining who are initially seronegative but have persistent proteinuria12. By contrast, positive PLA2R antibody serology and negative glomerular PLA2R staining are uncommon121,122 and very likely reflect differences in staining techniques123.
Indications for kidney biopsy
Kidney biopsy is costly and can result in major complications123,124,125,126,127. Given the high specificity of PLA2R antibodies in patients with MN and the fact that PLA2R antibodies have not been detected in other glomerular diseases or healthy individuals, deferral of a kidney biopsy has been suggested in patients who have nephrotic syndrome and PLA2R antibodies12,19. This proposal has been supported by a study that showed that, in patients with preserved kidney function (eGFR >60 ml/min/1.73 m2), no evidence of secondary cause (Box 2) and no diabetes mellitus, a positive serum PLA2R antibody titre equals a 100% probability of diagnosing MN and is therefore a reliable non-invasive method for the diagnosis of pMN128. In these patients, kidney biopsy did not provide any valuable information that altered treatment. This non-invasive diagnostic approach might be especially important for those at high risk of complications or in whom a kidney biopsy is contraindicated129. However, if kidney function is impaired or the patient has evidence of a potential secondary cause for MN, including diabetes mellitus, a kidney biopsy is needed to exclude concomitant kidney disease (for example, underlying diabetic nephropathy, acute interstitial nephritis or crescentic glomerulonephritis) and to estimate the extent of interstitial fibrosis and tubular atrophy, which may add useful information to guide management. Box 2 provides guidelines for the evaluation of associated conditions in patients with MN regardless of serology. The non-invasive diagnostic approach is supported by the new Kidney Disease: Improving Global Outcomes (KDIGO) guidelines on the management of glomerular disease130. In patients with a PLA2R− biopsy sample, staining for THSD7A, EXT1, EXT2, NELL1, NCAM1, SEMA3B, PCDH7 and HTRA1 antibodies should be performed depending on age, immunofluorescence pattern (segmental) and associated condition (autoimmunity).
pMN, sMN and a new antigen-based classification
In ~80% of patients, MN appears without an underlying cause and presents as a kidney-specific autoimmune disease. The target antigen in ~70% of patients is PLA2R, followed, in decreasing percentages, by NELL1, PCDH7, THSD7A, HTRA1 and SEMA3B (mainly in children and young adults), NCAM1, and unknown in the remaining 10–15% of patients with pMN. In ~20% of patients, MN occurs in association with other clinical conditions and is categorized as sMN5. Patients with pMN and those with sMN have similar clinical renal presentations.
However, this dichotomization of MN into primary and secondary has been challenged5,131. The complexity arises from the fact that clinical findings of the presence of antibodies do not accurately align with the definitions of pMN and sMN. Some patients with apparently sMN are also positive for PLA2R antibodies, most commonly those with hepatitis B virus (HBV) or hepatitis C virus (HCV) infection or sarcoidosis132,133,134,135. Whether these patients have true sMN or coincidental PLA2R-associated MN with a secondary disease is unclear. The facts that patients may enter spontaneous remission without treatment of the secondary cause or that treatment of the secondary cause does not result in remission of MN support the view that these antibodies occur coincidentally136. The same is true for patients with THSD7A-associated MN, for which an association with malignancy exists64,137. In these patients, remission has been observed with treatment of the malignancy alone63,64,137,138, but most patients with THSD7A-associated MN, with or without concomitant malignancy, respond to immunosuppression therapy139,140. In addition, most patients with NELL1-associated MN present without evidence of concomitant disease, but a concomitant malignancy is present in some of these patients68,69,137. Thus, a new molecular classification for MN based on target antigen has been proposed5,131. Future studies should enable the proposition of a better disease classification based on the presence of antibodies and the antigen specificity as well as the proven association (or not) with an underlying cause.
PLA2R antibody assays and identification of other target antigens
Various assays are available to detect PLA2R antibodies. The most commonly used assay is the ELISA commercialized by Euroimmun, which is 99.6% specific and enables the quantification of PLA2R antibody levels. The indirect immunofluorescence assay (IFA) from the same provider is a bit more sensitive than the ELISA and is 100% specific but does not enable quantitative assessment141. The currently recommended reference ranges for the ELISA assay are <14 relative units (RU)/ml (negative), 14–20 RU/ml (borderline) and >20 RU/ml (positive). Improved sensitivity without affecting specificity has been suggested by reducing the cut-off from 20 RU/ml to 2 RU/ml (refs142,143) or by using a combination of IFA and ELISA128. In this study, all patients with ELISA values >2 RU/ml and <20 RU/ml and a positive IFA had MN confirmed on biopsy. An addressable laser bead immunoassay, showing similar performance to the IFA assay, has been developed but is not clinically available144. ELISA and IFA remain less sensitive than western blot analysis (not used in clinical practice) and antigen staining of the kidney biopsy sample121,145. Thus, these techniques may fail to detect PLA2R antibodies in patients with proven PLA2R-associated MN.
An indirect immunofluorescence assay for THSD7A antibodies is commercially available (Euroimmun) but tests for NELL1, NCAM1, SEMA3B, PCDH7 and HTRA1 antibodies have not yet been developed. However, antibodies specific for the antigens are commercially available and can be used for the detection of antigen after retrieval in paraffin-embedded kidney biopsy samples117.
MN and malignancies
The prevalence of malignancy in patients with MN is estimated at 6–22%, most commonly occurring in patients >60 years of age with most cancers discovered before or at the time of the diagnosis of MN146; whether these are coincidental events or represent an aetiological association is unclear. Three criteria to ascertain an aetiological association have been proposed: remission occurs after complete removal of the tumour, renal relapse accompanies recurrence of the neoplasia, and the detection of tumour antigens and antitumor antibodies within subepithelial immune deposits147. However, clinical application of this paradigm can be difficult, in part because culprit antigens are generally unknown. Although fulfilment of these criteria provides strong support for an aetiological link, especially in patients with THSD7A-associated MN, their absence does not refute it.
The role of malignancy in patients with MN who are PLA2R antibody positive is debatable148. PLA2R antibody positivity has been reported in a minority of patients with MN associated with solid tumours but, in one study, no patient with PLA2R-associated MN went into remission with malignancy treatment alone, suggesting a coincidental process rather than a causal relation131. However, 10% of the patients tested negative for all seven known antigens associated with MN and 25% of these had a malignancy131. In a large series of 91 patients with NELL1-associated MN, 33% had an associated malignancy68. Patients with NELL1-associated MN were older than patients with PLA2R-associated MN (mean age 66.8 ± 10.8 years versus 56.4 ± 13.9 years, respectively) and patients with NELL1-associated MN with malignancy were significantly older than patients with NELL1-associated MN without malignancy (71.0 ± 8.6 years versus 65.0 ± 10.5 years; P = 0.01). By contrast, in a study from China that included 15 patients with NELL1-associated MN (median age 49 years, range 44–50 years), no association with malignancy was found149.
In practice, we recommend that patients who present with MN should undergo a thorough evaluation for possible occult malignancy, especially if they are negative for PLA2R antibodies or positive for THSD7A or NELL1 antibodies. The evaluation should consist of most age-appropriate screening tests, including colon cancer screening, mammography, kidney ultrasonography, a prostate-specific antigen assay in men and a chest radiograph (or a chest CT in patients at high risk) (Box 2; Supplementary Box 1)134. Ongoing vigilance is necessary because the diagnosis of cancer may not be immediately obvious.
Children
MN rarely affects children (0.1 cases per 100,000 per year)150. However, its frequency may be underestimated in this age group as children <10–12 years of age with nephrotic-range proteinuria are usually treated empirically with oral glucocorticoids without performing a renal biopsy. As childhood progresses, MN as a cause of nephrotic syndrome becomes more frequent, increasing from 1–2% at ages 1–5 years to 18–22% at ages 18–20 years. A rare form of congenital MN that is limited to only a few families worldwide is caused by a maternal homozygous mutation in MME, which encodes NEP52,151. The SEM3B-associated form of pMN typically occurs in children (even <2 years of age) and in young adults70. BSA-related MN should also be considered in children <5 years of age80.
Similar to adults, particularly in regions with endemic HBV infection, young children presented with HBV-associated MN that is responsive to anti-viral treatment152. This form of MN has decreased steeply with widespread vaccination against HBV152. In adolescents, MN can occur in patients, typically female, with renal involvement secondary to SLE (class V lupus nephritis). At this age, pMN also occurs, especially but not exclusively associated with PLA2R153.
When MN is diagnosed in a child, the most likely causes must be identified, taking into account the child’s age153. Briefly, the congenital NEP form of MN must be suspected in neonates; the BSA-related form in infants; the SEMA3B form in children aged 1–3 years; the enzyme replacement therapy form in children with a metabolic disease receiving recombinant human arylsulfatase B or α-glucosidase;154 the HBV-associated form in children living in areas with endemic HBV infection, particularly in those aged 5–7 years; and either SLE or primary forms of MN driven by one of the known antigens, particularly PLA2R, in children aged >10–12 years. In addition to SEMA3B-associated MN, the actual incidence of MN involving other known antigens in children still needs to be investigated; forms of MN associated with THSD7A have been described as well as a single patient each with NCAM1-associated and with EXT1 and EXT2-associated forms of MN.
The outcome of pMN in children is unpredictable and spontaneous remission occurs in ~30% of patients. Overall, prognosis in paediatric forms of MN seems better than in adults153. In a retrospective study of 217 children with pMN, after a median follow-up of 45 (23.5–74.0) months, the cumulative kidney survival rates at 5 years and 10 years after renal biopsy were 95.3% and 67.8%, respectively155.
Low-income regions
In low-income settings, patients with nephrotic syndrome due to MN often present with late-stage disease, sometimes with complications156. The presence of vascular thrombosis might prevent a kidney biopsy as patients need immediate therapeutic anticoagulation. Lack of specialist facilities limits the ability to fully evaluate these patients, including investigations to rule out secondary causes of MN, serological testing and kidney biopsy. Special attention needs to be given to rule out locally prevalent infections such as HBV or HCV. According to the Global Kidney Health Atlas, laboratory facilities for assessment of urinary protein levels or albumin creatinine ratios were available in <5% and <55% and renal pathology services were available in only 12% and 46% of low-income and lower-middle-income regions, respectively157. Even where pathology is available, immunofluorescence microscopy, PLA2R staining or electron microscopy are not routinely performed in many centres.
Prevention
Infections with HBV, HCV or HIV are important preventable causes of MN. Of these, HBV infection can be prevented with a vaccine. According to the WHO, the prevalence of HBV infection is above the global median of 3.5% in sub-Saharan Africa, Southeast Asia, and Central Asia and exceeds 10% in several African regions. Universal HBV vaccination has effectively eliminated HBV-associated MN in high-income regions25. However, vaccination coverage remains dismal in low-income regions, with only 6% coverage in the WHO African region158.
Ingestion of heavy metals is associated with the development of MN. Heavy metals are often identified as contaminants in indigenous medications in India and China159. Better regulation of their use can help prevent MN. A study from China18 identified a strong association between air pollution and the increasing prevalence of MN. These data identify important gaps in our knowledge of the broader environmental determinants of this condition. The findings highlight the need to develop sustainable approaches to address the preventable causes of MN through actions that regulate the use of indigenous medicines and address emerging environmental challenges160.
Management
The initial non-immunosuppressive treatment of patients with pMN is guided by the complaints and (expected) complications at presentation and depends on the severity of proteinuria. Intensive monitoring enables the estimation of whether the patient is at risk of progressive kidney function deterioration. Immunosuppressive therapy, targeting the abnormal autoimmune response, should be considered in patients at risk. The introduction of a quantitative ELISA assay to measure antibody levels (only available for PLA2R antibodies) has enabled improved risk prediction and treatment guidance. For the time being, treatment approaches overall do not differ for the pMN forms associated with different antigens but most data are available for PLA2R-associated MN, which can facilitate more tailored management in patients with this form of MN. In patients with sMN, treatment of the underlying cause is warranted; however, patients with sMN who do not respond should receive therapy as proposed for pMN.
Supportive treatment of nephrotic syndrome
In nephrotic syndrome, oedema formation is dependent on water and sodium retention. Oedema contributes to immobility, fatigue, discomfort, skin blistering, infections and anxiety. Treatment is empirical and not evidence based161. Initial treatment includes a sodium-restricted diet and loop diuretics (furosemide or bumetanide). In patients with insufficient response, a second diuretic is added (thiazide, acetazolamide or a potassium-sparing diuretic). Theoretically, amiloride should be most advantageous in view of the evidence of increased activation of collecting duct ENaC162. In clinical practice, combinations of diuretics are often effective and the choice is guided by serum electrolyte levels and adverse effects of medications (Box 1). Patients with severe oedema often require hospital admission for treatment with intravenous diuretics, sometimes supplemented with albumin infusions161. In patients with hyponatraemia, water restriction is advised. After attaining sodium balance, blood pressure treatment should continue, targeting a blood pressure of 125–130/75–80 mmHg (refs130,163). Angiotensin-converting enzyme inhibitors and/or angiotensin receptor blockers are preferred as they have antiproteinuric effects and evidence suggests that their use may increase spontaneous remission rates in patients with pMN164.
Patients with nephrotic syndrome often develop hypercholesterolaemia. Guidelines advise the use of statin therapy in patients with persistent proteinuria and hypercholesterolaemia, especially in patients >50 years of age, to provide cardiovascular protection130. The use of statins in MN is further supported by their suggested role in the prevention of venous thromboembolic events165.
Indeed, patients with MN are at high risk of venous and arterial thrombotic events and the incidence is highest within 6–12 months after disease onset165. Thus, already at the time of presentation and diagnosis, prophylactic anticoagulation must be considered, taking into account individual patient characteristics, disease severity, and patient and family history (Supplementary Box 2). Most guidelines suggest the use of early, prophylactic anticoagulation according to algorithms that consider all parameters that affect the risk of thrombotic events and bleeding130. Treatment with warfarin is often used as standard therapy; however, there are good arguments to start treatment with low-molecular-weight heparin (at low to moderate dose intensity) at the time of diagnosis and switch to warfarin after 3 months if nephrotic syndrome persists166. In patients who are not candidates for warfarin or are treated with low-intensity low-molecular-weight heparin and have other risk factors for atherosclerotic vascular events, the use of aspirin must be considered167. The use of the new class of direct-acting oral anticoagulant drugs for thrombosis prophylaxis in nephrotic syndrome cannot be recommended168. Direct-acting oral anticoagulant drugs have not been studied in nephrotic syndrome and some patients with nephrotic syndrome developed thrombosis while using them169. High protein binding, the contribution of renal clearance to drug elimination, and the role of CYP3A4 and p-glycoprotein in drug metabolism (interfering with the kinetics of CNIs) could all affect their use in nephrotic syndrome168.
Immunosuppressive therapy
Cyclophosphamide and corticosteroids
Long before the identification of pathogenic antigens and specific auto-antibodies, pMN was recognized as an immune-mediated kidney disease, which fostered the use of prednisolone and other immunosuppressive drugs. RCTs showed that a combination of an alkylating agent (preferably cyclophosphamide) and prednisolone attenuated the progression to kidney failure in patients with MN170. However, the 2012 KDIGO guidelines did not recommend the unrestricted use of this therapy in patients with MN163. First, ~40% of untreated patients do not progress to kidney failure and many develop spontaneous proteinuria remission. Second, treatment with cyclophosphamide and corticosteroids is associated with considerable adverse effects (Box 1). Thus, it was advocated to restrict cyclophosphamide-based therapy to patients with MN and a high risk of kidney failure171. The guideline used persistent proteinuria of >4 g per day after 6 months of non-immunosuppressive therapy as the criterion of high risk. This criterion is not very accurate as the rate of spontaneous remission in these patients can be 45%8. The optimization of therapy (in terms of risk–efficacy balance) in patients with MN requires the early and accurate identification of patients who will progress to kidney failure (or will develop severe complications of nephrotic syndrome) and the introduction of effective, less toxic and alternative immunosuppressive therapies.
Risk prediction
Serum creatinine levels and proteinuria are the oldest biomarkers to estimate the risk of progressive disease associated with increased cardiovascular morbidity and mortality, and ultimately leading to kidney failure. Many other reported biomarkers lack sensitivity and/or specificity and have not been validated172 (Table 2). Baseline serum creatinine levels (cut-off value 1.5 mg/dl) identify patients at high risk relatively late at a time when kidney function is already compromised. While patients with persistent non-nephrotic proteinuria do not develop renal insufficiency173,174, nephrotic syndrome by itself is not an accurate prognostic biomarker as 40–45% of patients with nephrotic syndrome do not progress. One study showed that no less than 22% of patients with baseline proteinuria >12 g/day develop spontaneous remission164. Monitoring the course of kidney function and proteinuria during follow-up improves risk prediction164,175,176. The Toronto risk score combines kidney function and proteinuria parameters. This score has been validated and showed good performance177 but it can only be calculated after 12–24 months of follow-up. Measurement of low-molecular-weight proteins in urine at baseline provided similar accuracy as the Toronto risk score178. PLA2R antibody levels had no added value in a prognostic model that included proteinuria and serum creatinine levels but, in univariate analysis, high PLA2R antibody levels were specific (>80%) for predicting progression, with positive predictive values of 77% for 150–300 RU/ml and 87% for >300 RU/ml (ref.179).
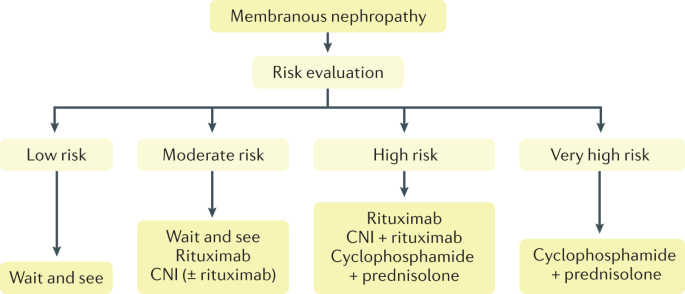
On the basis of biomarker assessment, the KDIGO 2021 guideline defines four risk categories: low, moderate, high and very high risk130 (Table 3). Although the disease characteristics of most patients may not perfectly fit one category and risk classification is not very accurate and partly based on low-quality data, the classification provides guidance in patient management. Because patients are seen at various phases of the disease, some entering immunological remission while others having increasing immunological activity, one cannot rely on a snapshot measurement of PLA2R antibody levels and proteinuria to predict the risk of progression but rather on the trajectory of these variables180. Thus, risk evaluation is a dynamic process and it is important to re-evaluate risk prediction at 3 months and 6 months after diagnosis as the changes in PLA2R antibody levels and clinical parameters may affect treatment indications. For example, a severe nephrotic syndrome with persistently high PLA2R antibody levels at 3 months will prompt starting immunosuppressive treatment. Further studies are needed to define more specific biomarkers that would predict progression at baseline ideally from the urine via exosomes, although the varying time points of sampling in the natural history of the disease will probably make interpretation difficult.
CNIs and CD20-targeted therapy
The introduction of novel immunosuppressive agents offered hope for effective, less toxic therapy in patients with pMN. CNIs, such as cyclosporine and tacrolimus, indirectly affect B cell function and were proven effective in preventing immunological rejection after kidney transplantation. In addition, experimental studies suggested that CNIs directly target the podocyte, thereby reducing proteinuria181. The development of CD20 antibody treatments, such as rituximab, enabled effective depletion of B cells and thus the selective targeting of antibody production.
Both CNIs and rituximab, alone or in combination, are considered less toxic than cyclophosphamide and prednisolone. A review of clinical trials concluded that CNIs increased the likelihood of partial and complete proteinuria remission compared with no treatment (72–75% versus 22%)170. Additionally, remission rates at 12-month follow-up were comparable and numerically higher than those of cyclophosphamide treatment (CNIs 71–89%; cyclophosphamide 65–77%); however, the disease relapses after withdrawal of CNIs in most patients. In one RCT, relapses within 12 months after remission occurred in 40% of patients treated with tacrolimus and in 7% of patients treated with cyclophosphamide182. The efficacy of rituximab was also studied in RCTs. In the GEMRITUX trial, after 23 months of follow-up, the remission rate was 66% in patients treated with rituximab (total dose 750 mg/m2) and 45% in those who received conservative treatment8. In the MENTOR trial, although rituximab (total dose 4 g) was non-inferior to cyclosporine in inducing remission at 12 months after treatment start, more patients who received rituximab maintained remission at 12 months after withdrawal of therapy (60% versus 20%)9. In the STARMEN trial, although sequential therapy with tacrolimus (for 6 months) and rituximab (single dose 375 mg/m2) was inferior in inducing remission than the combination of cyclophosphamide and prednisolone (84% versus 58% at 24 months), the single dose of rituximab prevented relapse after withdrawal of tacrolimus10. The most recent RI-CYCLO trial compared rituximab (total dose 2 g) with cyclical cyclophosphamide and corticosteroids11. This study was underpowered and included mostly patients at moderate risk with low anti-PLA2R antibody levels. Although the authors concluded that the study provided “no signal of more benefit or less harm associated with rituximab”, the per-protocol analysis showed a significantly lower complete remission rate at 12 months in patients treated with rituximab than patients treated with cyclophosphamide and corticosteroids (13% versus 34%; OR 0.28, 95% CI 0.08–0.95). Subgroup analysis suggested superiority of cyclophosphamide treatment in men and in patients with increased proteinuria and decreased serum albumin levels.
Thus, there is evidence that CNIs and rituximab (alone or in combination) induce remission of proteinuria, which should translate into improved renal outcomes, although this has not yet been proven. However, overall failure rates with these agents are 30–35%, raising controversies on the ideal dosage and best protocol. Some data suggest that cyclophosphamide is more effective in patients at high risk183. The guidelines argue against the use of CNIs or rituximab in patients with deteriorating or decreased GFR; however, other data with rituximab are encouraging184.
Individualized treatment
Risk biomarkers, clinical characteristics, adverse effects, and patient and physician preferences can all be used to individualize therapy in patients with MN (Fig. 4). Patients at low risk do not need immunosuppressive therapy130. Patients at moderate risk can receive rituximab or a CNI — the controversial use of CNI in this indication is to decrease the duration of proteinuria in those with a high potential of spontaneous remission. In patients at high risk, single-agent rituximab treatment is now established in addition to combinations of cyclophosphamide and prednisolone. However, the long-term benefit on kidney function of CD20 antibody therapy remains unclear and its efficacy to induce immunological remission seems to be reduced in patients with very high antibody titres183, although this view has been challenged185. Patients at very high risk should receive a combination of cyclophosphamide and prednisolone.
In patients with primary membranous nephropathy (MN), efforts must be made to estimate the risk of kidney function deterioration using clinical criteria (Table 2) and risk classification (Table 3). As the risk profile will change during the follow-up period, risk should be evaluated regularly. Immunosuppressive therapy should not be used in patients at low risk. By contrast, patients at very high risk should receive the most effective but also most toxic therapy with cyclophosphamide and prednisolone. Different treatment options can be considered in patients at moderate and high risk, guided by patient and physician preference, expected adverse effects, therapy reimbursement, and other factors. Although calcineurin inhibitor (CNI) monotherapy is probably less effective, it is an option in patients at moderate risk of progression. CNIs shorten the period of proteinuria and can be used in a regimen combined with rituximab. Adapted from ref.130, KDIGO 2021 Clinical Practice Guideline for the Management of Glomerular Diseases.
In the individual patient, the ultimate choice of treatment requires a discussion of benefits and risks considering the expected burden of adverse effects (Supplementary Box 3; Supplementary Tables). Future studies should define the best dosage and protocols adapted to the patient and integrate the new advances in the field of immunotherapy, including new CD20 antibodies, belimumab (a monoclonal antibody that inhibits the B cell-activating factor (BAFF)), anti-plasma cell therapy and anti-complement therapy. These new agents should be discussed in patients with refractory disease in expert centres.
Monitoring immunosuppressive therapy
Immunosuppressive therapy is usually given according to standard treatment protocols of therapy dosing and duration130. Patients should be monitored for adverse effects (Box 1) and therapy efficacy is ascertained by improvements in proteinuria, serum albumin levels and (if applicable) serum creatinine levels. Clinical response to cyclophosphamide or rituximab is notably slow and partial remission of proteinuria only develops after 6–18 months, often after withdrawal of therapy10,78. Thus, in patients with persistent nephrotic syndrome but stable eGFR after 6 months, no change in treatment is required.
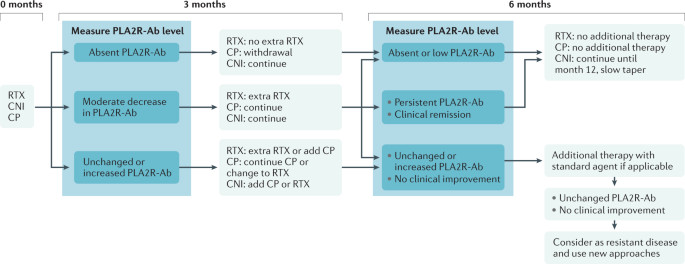
In PLA2R-associated MN, measurement of PLA2R antibody levels aids treatment decisions (Fig. 5). Cyclophosphamide was more effective than rituximab in inducing immunological remission in patients with high PLA2R antibody levels186, which explains the low (30%) remission rate after one dose of rituximab in patients with high antibody levels79. Treatment should induce immunological remission. The disappearance of PLA2R antibodies (using the IFA; when using ELISA, the titre should fall below 2 RU/ml) predicted remission of proteinuria, whereas persistence of PLA2R antibodies after therapy was associated with progressive disease78,187.
In patients with phospholipase A2 receptor (PLA2R)-associated primary membranous nephropathy, regular evaluation of the course of PLA2R antibody (PLA2R-Ab) levels after the start of immunosuppressive therapy enables the optimization of immunosuppressive therapy in the individual patient. Immunological remission is the goal of therapy. The disappearance of antibodies can be used to taper or withdraw therapy, whereas persistence or increasing antibody levels should lead to continuation of therapy or to switching to an alternative drug regimen. No validated cut-off values exist. A negative immunofluorescence assay result or PLA2R ELISA titre <2 RU/ml defines the absence of PLA2R-Ab. When measuring PLA2R-Ab at regular intervals (every 2–3 months), a large decrease of antibody levels (>50%) to values <50 RU/ml may be sufficient as an initial response criterion. CNI, calcineurin inhibitor; CP, cyclophosphamide; RTX, rituximab. Adapted from ref.130, KDIGO 2021 Clinical Practice Guideline for the Management of Glomerular Diseases.
Children
Given the rarity of paediatric MN, children with MN should be managed in expert centres and treatment should be targeted. Secondary forms of MN require management of the underlying condition (for example, HBV infection or SLE)188. Primary forms of MN, especially in adolescents, can be treated similarly to adults. Supportive therapy with inhibitors of the renin–angiotensin system and low-salt diet is essential. A key difference to the situation in adults is that many children, especially if <10–12 years old, are diagnosed with MN after already having received oral prednisolone for 4–8 weeks. Treatment with CNIs or rituximab follows the same dosing regimen employed for adults. When these therapies are available, cyclophosphamide is rarely used189.
Low-income regions
In resource-poor settings, patients often do not present until the disease has progressed to a severe nephrotic state and/or a complication has occurred, for example, vascular thrombosis or infection such as pneumonia. This prevents the timely initiation of non-immunosuppressive antiproteinuric therapies with drugs that block the renin–angiotensin system. The lack of specialist nephrologists limits the application of personalized medicine principles such as individualizing evidence-based therapies according to the patient’s risk status190. Finally, the full range of treatments may not be available because a drug (for example, rituximab) is not marketed in the country or is too expensive. New treatments that are currently under investigation and monitoring approaches, such as PLA2R antibody assays, are likely to further increase treatment costs and therapeutic inequity. Treatment compliance can be a problem and contribute to suboptimal responses.
Potential solutions include a resource-sensitive adaptation of clinical practice guidelines by global organizations such as KDIGO and ISN191, using information technology tools to support the implementation of standard treatment pathways through the available workforce via linking with expert centres by international cooperations (for example, through ISN Sister Centers programmes or Project ECHO), greater use of generic compounds and clinical trials of therapies to optimize the risk–benefit balance (for example, eliminating methylprednisolone pulses in the Ponticelli regimen). Advocacy is needed for greater involvement of low-resource regions in clinical trials of novel therapies with the commitment to make these treatments available as has been done for HIV therapeutics and SARS-CoV-2 vaccination.
Patients with a kidney allograft
Patients with pMN who do not tolerate or do not respond to immunosuppressive therapy will develop kidney failure and need kidney replacement therapy. Kidney transplantation is considered the best treatment option provided there are no contraindications for this surgical procedure. Apart from the routine pretransplant evaluation, in patients with pMN, the risk for recurrent disease after kidney transplantation should be assessed and discussed. In these patients, the histological recurrence rate is 50–60% and the clinical recurrence rate is 30–40%192,193,194,195,196,197. Increased age, short waiting time to receiving the transplant, heavy proteinuria at pretransplant evaluation, and corticosteroid-free maintenance immunosuppression after transplantation are associated with an increased risk of recurrence192,193,197,198. Recurrence rates are approximately threefold higher after transplantation of an organ from a living related donor195,196, compatible with the observation that the risk of recurrence is dependent on donor HLA-D and PLA2R1 variants90.
Pretransplant and post-transplant measurement of PLA2R antibody levels aids patient management (Supplementary Box 4). The most critical step is to unequivocally establish that MN is associated with PLA2R. In PLA2R-associated MN, the pretransplantation presence of PLA2R antibodies, especially at high titres, is associated with a high risk of recurrence, whereas undetectable PLA2R antibody levels predict a low risk195,197,199. A gradual decrease and disappearance of PLA2R antibodies after transplantation are associated with a reduced risk of recurrence (25% versus 71%)195. Although PLA2R antibody level measurement is therefore helpful, there are pitfalls and exceptions to the rule (Supplementary Box 4).
Rituximab treatment is effective in patients with recurrent MN following kidney transplantation193,197. Most patients (>80%) respond with complete or partial remission of proteinuria, which is preceded by the disappearance of the antibodies in patients who are PLA2R antibody positive. In 20–30% of patients, recurrent disease is non-progressive193. Thus, rituximab should be withheld in patients with persistent proteinuria at <1 g/day. There is no evidence-based benefit on the post-transplant outcome of treatment with rituximab before transplantation.
Quality of life
According to the WHO, health-related quality of life (HRQOL) is defined as “an individual’s perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns”200. This broad concept encompasses multiple dimensions, including a person’s physical health, psychological status, level of independence, social relationships and personal beliefs200. Systematic reviews have shown that various measures for quality of life (for example, Short Form Health Survey (SF-36); EuroQoL 5 dimensions (EQ-5D); Kidney Disease Quality of Life Instrument (KDQOL)) have been used in patients with chronic kidney disease201,202. However, data on the quality of life in patients with MN are limited203.
Patients with MN have impaired quality of life and functioning compared with age-matched and gender-matched individuals in the general population204,205, which may be further exacerbated by symptoms, for example, fatigue and oedema, and treatment burden206. Some unique features of MN can also affect quality of life such as the increased risk of thrombotic events.
A study by the Cure Glomerulonephropathy Network (CureGN) involving 478 children and 1,115 adults with glomerular diseases, including MN, found that oedema, female sex, weight (obesity) and estimated GFR correlated with decrements in HRQOL domains203. The findings also indicated that HRQOL was similar across different types of primary glomerular disease203. Another study conducted in patients with primary glomerular disease found that HRQOL was lower compared with healthy controls and was associated with proteinuria205.
The need to include patient goals and preferences in the shared decision-making and assessment of interventions and care is increasingly recognized207. This is particularly relevant in MN because of the lack of well-defined tools for risk stratification to help with treatment decisions. Patient-reported outcomes, which reflect how patients feel and function, are assessed and reported directly by patients to provide a quantitative assessment of the effects of disease and treatment from the patient perspective208,209. However, patient-reported outcomes are infrequently reported in trials in patients with MN. HRQOL is an example of a patient-reported outcome; however, other outcomes are also important to patients, which may be implemented in research, practice and policy.
As part of the Standardized Outcomes in Nephrology – Glomerular Disease (SONG-GD) initiative, 134 patients with glomerular disease from Australia, the USA, the UK and Hong Kong identified and prioritized outcomes of importance and discussed the reasons for their choices. The highest-ranked patient-reported outcomes were life participation (defined as the ability to do meaningful activities), fatigue, anxiety, family impact and the ability to work210. The prioritization was driven by constraints on patients’ day-to-day existence, impaired agency and control over health, and threats to future health and their family210.
Further data on quality of life in patients with MN are needed, which may be gathered through routine measurement and reporting of HRQOL in research and clinical practice. Additionally, more evidence on interventions to improve quality of life and other patient-important outcomes, including life participation, fatigue, depression and anxiety, and the ability to work, is required. Ultimately, this may help to improve the care and outcomes of patients living with MN.
Outlook
Despite the tremendous progress made over the past two decades, considerable gaps in our understanding of MN remain (Box 3). The application of new technologies and opportunities to adopt investigative strategies from other disciplines will enable a continued exponential growth in our understanding of MN. The use of mass spectrometric techniques, initially used to subtype the deposits of renal amyloidosis, has led to an unprecedented discovery of new antigens in MN and this progress should continue with the identification of additional target antigens in paediatric, adult idiopathic and secondary forms of MN in addition to a better understanding of the similarities and differences in complement and matrix proteins involved in the disease subtypes. Mass spectrometric imaging can surpass the resolution of more conventional glomerular laser capture approaches by limiting analysis to even more defined regions of the cell or GBM211,212.
Our ability to interrogate human and experimental biospecimens has become much more sophisticated. Advances in microscopy and cell labelling now include multiplexed immunofluorescence imaging technology for analysis of a large number of antigens or biomarkers (including complement components) and super-resolution imaging of the altered filtration barrier and molecules comprising the subepithelial deposits213. Single-cell RNA sequencing of human biopsy samples or experimental tissues can offer in-depth analysis of injury and repair pathways of all glomerular cell types as well as of downstream tubular and renal parenchymal and immune cells214. Similarly, single-cell RNA sequencing of circulating lymphocyte populations can characterize blood signatures of active disease, remission and progression, which could be used for patient monitoring and to define the antigen-specific B cell and T cell repertoire and their associated B cell and T cell receptors. These molecular data and computational analyses will further the efforts to develop novel antigen-specific or epitope-specific therapies, such as chimeric autoantibody receptor T cells that could target autoantibody-producing B cells215, or to develop the use of antigen-derived peptides coupled to MHC class II to study or target T cells216. Targeted multi-omics of the urine217 should continue to be developed, with special emphasis on shed complement and matrix components to characterize signatures of active disease, remission and progression that enable better correlation of this ‘liquid biopsy’ with defined molecular features of kidney tissue.
High-resolution genetic data assembled from global registries of MN and control populations should be examined in the context of atlases of tissue-specific epigenetic regulatory elements and should be matched using machine learning approaches with records of phenotypic variation using information stored in electronic health records218. If this is possible at a large enough scale, previously unrecognized associations, susceptibilities and disease pathways in MN may come to light.
These knowledge gaps and new technologies should be prioritized in the next 5–10 years to focus on three major areas. First, understanding how genetic makeup, immune phenotype and exposures coalesce to cause disease initiation should be an overarching research goal, which in turn may lead to better prognostication, precision-guided therapeutics and monitoring, and avoidance of conditions that lead to relapse. Second, research should continue into the specific molecular mechanisms and pathways that cause glomerular injury and, in some individuals, rapid progression of parenchymal damage with ongoing proteinuria. Third, the field needs to move from broad immunosuppression of disease activity, which brings with it risks of infection and other substantial adverse effects, to more personalized and targeted therapeutics. Inhibition of the complement system seems to be the next therapeutic frontier in MN but further molecular understanding of the underlying pathological mechanisms could lead to even more novel ways to limit injury or stimulate reparative pathways. Our understanding of and ability to manipulate the immune system in MN is in its infancy but advances in immunology, oncology and infectious diseases (especially with the global emphasis on understanding the response to SARS-CoV-2) will drive our ability to rapidly interrogate the immune system in MN.
It is likely that substantial progress will be made in the therapeutic armamentarium in the near future, including new regimens to decrease the toxic effects of cyclophosphamide and corticosteroids, improving the use of CD20 antibodies with humanized, more potent molecules, such as obinutuzumab219, and new therapeutic approaches (anti-BAFF, anti-plasma cell and anti-complement therapy), which should be discussed in patients with resistant disease.
At present, the therapeutic armamentarium has already been enriched with new drugs. CD20-targeted humanized antibodies (ofatumumab, obinutuzumab and ocrelizumab) are now available. They induce prolonged B cell depletion with a very low risk of immunization219. These are currently mostly indicated in patients who have developed serum sickness with rituximab and in those with refractory or multi-relapsing MN220,221,222. One can predict a growing role for these more potent biotherapies as ~30% of patients treated with rituximab will not undergo clinical remission and relapses are frequent.
Belimumab is a human IgG1λ monoclonal antibody that inhibits BAFF, thereby affecting B cell proliferation and survival223. Because rituximab increases the circulating levels of BAFF, combination therapy with belimumab could be considered224. Belimumab was used successfully in patients with lupus. At the end of a 2-year RCT, the renal response was better in patients who received belimumab plus standard therapy than in those who received standard therapy alone225. Belimumab was used with some efficacy in patients with MN in a small open-label, prospective, single-arm study226 but further studies are needed.
Biotherapies targeting plasma cells must be seriously considered. Indeed, the relatively low rate of sustained complete remission in patients treated with rituximab is usually attributed to the involvement of CD19–CD20−CD38+CD138+ long-lived memory plasma cells that are niched naturally in the bone marrow and ectopically in the native and inflamed kidney. These non-proliferating plasma cells lacking CD19 and CD20 markers provide the basis for humoral memory and refractory autoimmune diseases227. These cells are targeted by anti-CD38 antibodies, which are used in ongoing trials (NCT04145440)228. Immunoadsorption and plasmapheresis have been used by several groups to enhance the depletion of circulating THSD7A antibodies and PLA2R antibodies in patients with severe MN229,230. Refractory disease is a current indication.
There is a strong interest in anti-complement therapies in glomerular diseases. MN seems to be among the most suitable for these treatments as complement is considered the main mediator of proteinuria, at least in experimental models. There are two windows of opportunity for anti-complement therapy: early before immunosuppressive drugs reach full efficacy and later in patients with partial or no remission. Several compounds targeting the lectin pathway and the alternative pathway are in early-phase trials231.
New drugs are urgently needed but preclinical models of the disease remain limited in their ability to assess the efficacy of novel therapeutics. The development of MN models using rodents with humanized components of the immune system may enable a more effective translation and relevance to human disease. The field has come to understand how human IgG4 PLA2R antibodies can activate the lectin pathway of complement activation using human podocytes grown in standard culture models104 but such single-cell-type in vitro systems ignore the complex interplay of closely apposed cell types within the glomerulus. New model systems, such as the glomerulus-on-a-chip that combines podocytes with endothelium in a microfluidic flow chamber103 or induced pluripotent stem cells (from healthy individuals or patients) in vascularized organoid cultures232, have the potential to enable a better understanding of the cell–cell interactions that drive disease and are amenable to high-throughput screening of compound libraries for drug discovery.
The future is bright for research into the pathogenesis and treatment of MN in all its forms and we encourage clinicians, scientists, patients, industry and regulatory agencies to come together with innovative and forward-reaching approaches. The involvement of patients both in defining the gaps and contributing to registries, biorepositories and research themes will be key to our common success.
References
Couser, W. G. Primary membranous nephropathy. Clin. J. Am. Soc. Nephrol. 12, 983–997 (2017).
Debiec, H. et al. Antenatal membranous glomerulonephritis due to anti-neutral endopeptidase antibodies. N. Engl. J. Med. 346, 2053–2060 (2002). A landmark article that reports the first description of a podocyte antigen involved in a rare subset of neonatal MN.
Beck, L. H. et al. M-type phospholipase A2 receptor as target antigen in idiopathic membranous nephropathy. N. Engl. J. Med. 361, 11–21 (2009). A landmark article that first characterizes the major antigen in adult MN, leading to a paradigm shift in the diagnosis and monitoring of patients.
Tomas, N. M. et al. Thrombospondin type-1 domain-containing 7A in idiopathic membranous nephropathy. N. Engl. J. Med. 371, 2277–2287 (2014). The first report of an antigen found to be associated with cancer in a subset of patients.
Ronco, P. & Debiec, H. Membranous nephropathy: current understanding of various causes in light of new target antigens. Curr. Opin. Nephrol. Hypertens. 30, 287–293 (2021).
Sethi, S. New ‘antigens’ in membranous nephropathy. J. Am. Soc. Nephrol. 32, 268–278 (2021).
Cattran, D. C. & Brenchley, P. E. Membranous nephropathy: integrating basic science into improved clinical management. Kidney Int. 91, 566–574 (2017).
Dahan, K. et al. Rituximab for severe membranous nephropathy: a 6-month trial with extended follow-up. J. Am. Soc. Nephrol. 28, 348–358 (2017).
Fervenza, F. C. et al. Rituximab or cyclosporine in the treatment of membranous nephropathy. N. Engl. J. Med. 381, 36–46 (2019). This landmark randomized clinical trial provides the first comparison of rituximab and cyclosporine.
Fernández-Juárez, G. et al. The STARMEN trial indicates that alternating treatment with corticosteroids and cyclophosphamide is superior to sequential treatment with tacrolimus and rituximab in primary membranous nephropathy. Kidney Int. 99, 986–998 (2021). This important randomized clinical trial provides the first comparison of cyclophosphamide (with corticosteroids) with a sequential combination of tacrolimus and rituximab.
Scolari, F. et al. Rituximab or cyclosphamide in the treatment of membranous nephropathy. J. Am. Soc. Nephrol. 32, 972–982 (2021).
De Vriese, A. S., Glassock, R. J., Nath, K. A., Sethi, S. & Fervenza, F. C. A proposal for a serology-based approach to membranous nephropathy. J. Am. Soc. Nephrol. 28, 421–430 (2017).
Kumar, V. et al. Antibodies to m-type phospholipase A2 receptor in children with idiopathic membranous nephropathy. Nephrology 20, 572–575 (2015).
Debiec, H. & Ronco, P. Immunopathogenesis of membranous nephropathy: an update. Semin. Immunopathol. 36, 381–397 (2014).
McGrogan, A., Franssen, C. F. & de Vries, C. S. The incidence of primary glomerulonephritis worldwide: a systematic review of the literature. Nephrol. Dial. Transplant. 26, 414–430 (2011).
Rychlik, I. et al. The Czech registry of renal biopsies. Occurrence of renal diseases in the years 1994-2000. Nephrol. Dial. Transplant. 19, 3040–3049 (2004).
Hogan, S. L., Muller, K. E., Jennette, J. C. & Falk, R. J. A review of therapeutic studies of idiopathic membranous glomerulopathy. Am. J. Kidney Dis. 25, 862–875 (1995).
Xu, X. et al. Long-term exposure to air pollution and increased risk of membranous nephropathy in China. J. Am. Soc. Nephrol. 27, 3739–3746 (2016).
Ronco, P. & Debiec, H. Pathophysiological advances in membranous nephropathy: time for a shift in patient’s care. Lancet 385, 1983–1992 (2015).
Arapovic, A. et al. Epidemiology of 10-year paediatric renal biopsies in the region of southern Croatia. BMC Nephrol. 21, 65 (2020).
Chen, A. et al. Idiopathic membranous nephropathy in pediatric patients: presentation, response to therapy, and long-term outcome. BMC Nephrol. 8, 11 (2007).
Eddy, A. A. & Symons, J. M. Nephrotic syndrome in childhood. Lancet 362, 629–639 (2003).
Nie, S. et al. The spectrum of biopsy-proven glomerular diseases among children in China: a national, cross-sectional survey. Clin. J. Am. Soc. Nephrol. 13, 1047–1054 (2018).
Johnson, R. J. & Couser, W. G. Hepatitis B infection and renal disease: clinical, immunopathogenetic and therapeutic considerations. Kidney Int. 37, 663–676 (1990).
Moroni, G. & Ponticelli, C. Secondary membranous nephropathy. a narrative review. Front. Med. 7, 611317 (2020).
Xu, X., Nie, S., Ding, H. & Hou, F. F. Environmental pollution and kidney diseases. Nat. Rev. Nephrol. 14, 313–324 (2018).
Narasimhan, B. et al. Characterization of kidney lesions in Indian adults: towards a renal biopsy registry. J. Nephrol. 19, 205–210 (2006).
Li, J. et al. Primary glomerular nephropathy among hospitalized patients in a national database in China. Nephrol. Dial. Transpl. 33, 2173–2181 (2018).
Schieppati, A. et al. Prognosis of untreated patients with idiopathic membranous nephropathy. N. Engl. J. Med. 329, 85–89 (1993).
Ponticelli, C. et al. A 10-year follow-up of a randomized study with methylprednisolone and chlorambucil in membranous nephropathy. Kidney Int. 48, 1600–1604 (1995).
Jha, V. et al. A randomized, controlled trial of steroids and cyclophosphamide in adults with nephrotic syndrome caused by idiopathic membranous nephropathy. J. Am. Soc. Nephrol. 18, 1899–1904 (2007).
Maisonneuve, P. et al. Distribution of primary renal diseases leading to end-stage renal failure in the United States, Europe, and Australia/New Zealand: results from an international comparative study. Am. J. Kidney Dis. 35, 157–165 (2000).
Troyanov, S. et al. Idiopathic membranous nephropathy: definition and relevance of a partial remission. Kidney Int. 66, 1199–1205 (2004).
Fervenza, F. C., Sethi, S. & Specks, U. Idiopathic membranous nephropathy: diagnosis and treatment. Clin. J. Am. Soc. Nephrol. 3, 905–919 (2008).
Klouda, P. T. et al. Strong association between idiopathic membranous nephropathy and HLA-DRW3. Lancet 2, 770–771 (1979).
Vaughan, R. W., Demaine, A. G. & Welsh, K. I. A DQA1 allele is strongly associated with idiopathic membranous nephropathy. Tissue Antigens 34, 261–269 (1989).
Stanescu, H. C. et al. Risk HLA-DQA1 and PLA(2)R1 alleles in idiopathic membranous nephropathy. N. Engl. J. Med. 364, 616–626 (2011).
Coenen, M. J. et al. Phospholipase A2 receptor (PLA2R1) sequence variants in idiopathic membranous nephropathy. J. Am. Soc. Nephrol. 24, 677–683 (2013).
Lv, J. et al. Interaction between PLA2R1 and HLA-DQA1 variants associates with anti-PLA2R antibodies and membranous nephropathy. J. Am. Soc. Nephrol. 24, 1323–1329 (2013).
Le, W. B. et al. HLA-DRB1*15:01 and HLA-DRB3*02:02 in PLA2R-Related membranous nephropathy. J. Am. Soc. Nephrol. 28, 1642–1650 (2017).
Cui, Z. et al. MHC class II risk alleles and amino acid residues in idiopathic membranous nephropathy. J. Am. Soc. Nephrol. 28, 1651–1664 (2017).
Xie, J. et al. The genetic architecture of membranous nephropathy and its potential to improve non-invasive diagnosis. Nat. Commun. 11, 1600 (2020). The most extensive multi-ethnic genome-wide association study performed in membranous nephropathy revealing the complexity of HLA-D alleles associated with membranous nephropathy in different ethnic populations and signals in the NF-κB and interferon pathways.
Wang, H. Y. et al. HLA class II alleles differing by a single amino acid associate with clinical phenotype and outcome in patients with primary membranous nephropathy. Kidney Int. 94, 974–982 (2018).
Van Damme, B. J., Fleuren, G. J., Bakker, W. W., Vernier, R. L. & Hoedemaeker, P. J. Experimental glomerulonephritis in the rat induced by antibodies directed against tubular antigens. V. Fixed glomerular antigens in the pathogenesis of heterologous immune complex glomerulonephritis. Lab. Invest. 38, 502–510 (1978).
Couser, W. G., Steinmuller, D. R., Stilmant, M. M., Salant, D. J. & Lowenstein, L. M. Experimental glomerulonephritis in the isolated perfused rat kidney. J. Clin. Invest. 62, 1275–1287 (1978).
Kerjaschki, D. & Farquhar, M. G. Immunocytochemical localization of the Heymann nephritis antigen (GP330) in glomerular epithelial cells of normal Lewis rats. J. Exp. Med. 157, 667–686 (1983).
Prabakaran, T. et al. Receptor-mediated endocytosis of α-galactosidase A in human podocytes in Fabry disease. PLoS ONE 6, e25065 (2011).
Debiec, H. et al. Role of truncating mutations in MME gene in feto-maternal allo-immunization and neonatal glomerulopathies. Lancet 364, 1252–1259 (2004).
Turner, A. J., Isaac, R. E. & Coates, D. The neprilysin (NEP) family of zinc metalloendopeptidases: genomics and function. Bioessays 23, 261–269 (2001).
Lu, B. et al. The control of microvascular permeability and blood pressure by neutral endopeptidase. Nat. Med. 3, 904–907 (1997).
Platt, J. L., Tucker, W. L. & Michael, A. F. Stages of renal ontogenesis identified by monoclonal antibodies reactive with lymphohematopoietic differentiation antigens. J. Exp. Med. 157, 155–172 (1983).
Vivarelli, M. et al. Genetic homogeneity but IgG subclass-dependent clinical variability of alloimmune membranous nephropathy with anti-neutral endopeptidase antibodies. Kidney Int. 87, 602–609 (2015).
Hogan, M. C. et al. Subfractionation, characterization, and in-depth proteomic analysis of glomerular membrane vesicles in human urine. Kidney Int. 85, 1225–1237 (2014).
Ancian, P., Lambeau, G., Mattei, M. G. & Lazdunski, M. The human 180-kDa receptor for secretory phospholipases A2. Molecular cloning, identification of a secreted soluble form, expression, and chromosomal localization. J. Biol. Chem. 270, 8963–8970 (1995).
Fresquet, M. et al. Identification of a major epitope recognized by PLA2R autoantibodies in primary membranous nephropathy. J. Am. Soc. Nephrol. 26, 302–313 (2015).
Seitz-Polski, B. et al. Epitope spreading of autoantibody response to PLA2R associates with poor prognosis in membranous nephropathy. J. Am. Soc. Nephrol. 27, 1517–1533 (2016).
Reinhard, L. et al. Clinical relevance of domain-specific phospholipase A2 receptor 1 antibody levels in patients with membranous nephropathy. J. Am. Soc. Nephrol. 31, 197–207 (2020).
Seitz-Polski, B. et al. Phospholipase A2 receptor 1 epitope spreading at baseline predicts reduced likelihood of remission of membranous nephropathy. J. Am. Soc. Nephrol. 29, 401–408 (2018).
Kanigicherla, D. et al. Anti-PLA2R antibodies measured by ELISA predict long-term outcome in a prevalent population of patients with idiopathic membranous nephropathy. Kidney Int. 83, 940–948 (2013).
Godel, M., Grahammer, F. & Huber, T. B. Thrombospondin type-1 domain-containing 7A in idiopathic membranous nephropathy. N. Engl. J. Med. 372, 1073 (2015).
Herwig, J. et al. Thrombospondin type 1 domain-containing 7A localizes to the slit diaphragm and stabilizes membrane dynamics of fully differentiated podocytes. J. Am. Soc. Nephrol. 30, 824–839 (2019).
Seifert, L. et al. The most N-terminal region of THSD7A Is the predominant target for autoimmunity in THSD7A-associated membranous nephropathy. J. Am. Soc. Nephrol. 29, 1536–1548 (2018).
Hoxha, E. et al. A mechanism for cancer-associated membranous nephropathy. N. Engl. J. Med. 374, 1995–1996 (2016).
Hoxha, E. et al. An indirect immunofluorescence method facilitates detection of thrombospondin type 1 domain-containing 7A-specific antibodies in membranous nephropathy. J. Am. Soc. Nephrol. 28, 520–531 (2017).
Sethi, S. et al. Exostosin 1/exostosin 2-associated membranous nephropathy. J. Am. Soc. Nephrol. 30, 1123–1136 (2019). This article reports the first use of a technological leap combining microdissection of glomeruli and mass spectrometry for the identification of the first biomarker of lupus membranous nephropathy.
Ravindran, A. et al. In patients with membranous lupus nephritis, exostosin-positivity and exostosin-negativity represent two different phenotypes. J. Am. Soc. Nephrol. 32, 695–706 (2021).
Saidi, M. et al. The exostosin immunohistochemical status differentiates lupus membranous nephropathy subsets with different outcomes. Kidney Int. Rep. 6, 1977–1980 (2021).
Caza, T. et al. NELL1 is a target antigen in malignancy-associated membranous nephropathy. Kidney Int. 99, 967–976 (2021).
Sethi, S. et al. Neural epidermal growth factor-like 1 protein (NELL-1) associated membranous nephropathy. Kidney Int. 97, 163–174 (2020). This article reports the identification of the second prevalent antigen (after PLA2R) in MN using glomerular microdissection followed by mass spectrometry.
Kudose, S. et al. The clinicopathologic spectrum of segmental membranous glomerulopathy. Kidney Int. 99, 247–255 (2021).
Sethi, S. et al. Semaphorin 3B-associated membranous nephropathy is a distinct type of disease predominantly present in pediatric patients. Kidney Int. 98, 1253–1264 (2020).
Caza, T. et al. Neural cell adhesion molecule 1 is a novel autoantigen in membranous lupus nephritis. Kidney Int. 100, 171–181 (2021).
Sethi, S. et al. Protocadherin 7-associated Membranous Nephropathy. J. Am. Soc. Nephrol. 32, 1249–1261 (2021).
Al-Rabadi, L. F. et al. Serine protease HTRA1 as a novel target antigen in primary membranous nephropathy. J. Am. Soc. Nephrol. https://doi.org/10.1681/ASN.2020101395 (2021).
Meyer-Schwesinger, C. et al. A novel mouse model of phospholipase A2 receptor 1-associated membranous nephropathy mimics podocyte injury in patients. Kidney Int. 97, 913–919 (2020).
Blosser, C. D., Ayalon, R., Nair, R., Thomas, C. & Beck, L. H. Jr. Very early recurrence of anti-Phospholipase A2 receptor-positive membranous nephropathy after transplantation. Am. J. Transplant. 12, 1637–1642 (2012).
Stahl, R., Hoxha, E. & Fechner, K. PLA2R autoantibodies and recurrent membranous nephropathy after transplantation. N. Engl. J. Med. 363, 496–498 (2010).
Beck, L. H. Jr et al. Rituximab-induced depletion of anti-PLA2R autoantibodies predicts response in membranous nephropathy. J. Am. Soc. Nephrol. 22, 1543–1550 (2011).
Ruggenenti, P. et al. Anti-phospholipase A2 receptor antibody titer predicts post-rituximab outcome of membranous nephropathy. J. Am. Soc. Nephrol. 26, 2545–2558 (2015).
Debiec, H. et al. Early-childhood membranous nephropathy due to cationic bovine serum albumin. N. Engl. J. Med. 364, 2101–2110 (2011). A landmark article that identifies the first food antigen involved in rare cases of membranous nephropathy in children.
Border, W. A., Ward, H. J., Kamil, E. S. & Cohen, A. H. Induction of membranous nephropathy in rabbits by administration of an exogenous cationic antigen. J. Clin. Invest. 69, 451–461 (1982).
Adler, S. G., Wang, H., Ward, H. J., Cohen, A. H. & Border, W. A. Electrical charge. Its role in the pathogenesis and prevention of experimental membranous nephropathy in the rabbit. J. Clin. Invest. 71, 487–499 (1983).
Hunley, T. E. et al. Nephrotic syndrome complicating α-glucosidase replacement therapy for Pompe disease. Pediatrics 114, e532–e535 (2004).
Debiec, H. et al. Allo-immune membranous nephropathy and recombinant aryl sulfatase replacement therapy: a need for tolerance induction therapy. J. Am. Soc. Nephrol. 25, 675–680 (2013).
Burbelo, P. D. et al. Detection of PLA2R autoantibodies before the diagnosis of membranous nephropathy. J. Am. Soc. Nephrol. 31, 208–217 (2020).
Cremoni, M. et al. Th17-immune response in patients with membranous nephropathy is associated with thrombosis and relapses. Front. Immunol. 11, 574997 (2020).
Motavalli, R. et al. Altered Th17/Treg ratio as a possible mechanism in pathogenesis of idiopathic membranous nephropathy. Cytokine 141, 155452 (2021).
Rosenzwajg, M. et al. B- and T-cell subpopulations in patients with severe idiopathic membranous nephropathy may predict an early response to rituximab. Kidney Int. 92, 227–237 (2017).
Cantarelli, C. et al. A comprehensive phenotypic and functional immune analysis unravels circulating anti-phospholipase A2 receptor antibody secreting cells in membranous nephropathy patients. Kidney Int. Rep. 5, 1764–1776 (2020).
Berchtold, L. et al. HLA-D and PLA2R1 risk alleles associate with recurrent primary membranous nephropathy in kidney transplant recipients. Kidney Int. 99, 671–685 (2021).
Segerer, S. & Schlondorff, D. B cells and tertiary lymphoid organs in renal inflammation. Kidney Int. 73, 533–537 (2008).
Kolovou, K. et al. B-cell oligoclonal expansions in renal tissue of patients with immune-mediated glomerular disease. Clin. Immunol. 217, 108488 (2020).
Prunotto, M. et al. Proteomic analysis of podocyte exosome-enriched fraction from normal human urine. J. Proteom. 82, 193–229 (2013).
Kerjaschki, D. & Neale, T. J. Molecular mechanisms of glomerular injury in rat experimental membranous nephropathy (Heymann nephritis). J. Am. Soc. Nephrol. 7, 2518–2526 (1996).
Huang, C. C. et al. IgG subclass staining in renal biopsies with membranous glomerulonephritis indicates subclass switch during disease progression. Mod. Pathol. 26, 799–805 (2013).
Val-Bernal, J. F., Garijo, M. F., Val, D., Rodrigo, E. & Arias, M. C4d immunohistochemical staining is a sensitive method to confirm immunoreactant deposition in formalin-fixed paraffin-embedded tissue in membranous glomerulonephritis. Histol. Histopathol. 26, 1391–1397 (2011).
Hayashi, N. et al. Glomerular mannose-binding lectin deposition in intrinsic antigen-related membranous nephropathy. Nephrol. Dial. Transplant. 33, 832–840 (2018).
Bally, S. et al. Phospholipase A2 receptor-related membranous nephropathy and mannan-binding lectin deficiency. J. Am. Soc. Nephrol. 27, 3539–3544 (2016).
Ravindran, A. et al. Proteomic analysis of complement proteins in membranous nephropathy. Kidney Int. Rep. 5, 618–626 (2020).
Cybulsky, A. V., Quigg, R. J. & Salant, D. J. Experimental membranous nephropathy redux. Am. J. Physiol. Ren. Physiol. 289, F660–F671 (2005).
Tomas, N. M. et al. Autoantibodies against thrombospondin type 1 domain-containing 7A induce membranous nephropathy. J. Clin. Invest. 126, 2519–2532 (2016).
Tomas, N. M. et al. A heterologous model of thrombospondin type 1 domain-containing 7A-associated membranous nephropathy. J. Am. Soc. Nephrol. 28, 3262–3277 (2017).
Petrosyan, A. et al. A glomerulus-on-a-chip to recapitulate the human glomerular filtration barrier. Nat. Commun. 10, 3656 (2019).
Haddad, G. et al. Altered glycosylation of IgG4 promotes lectin complement pathway activation in anti-PLA2R1 associated membranous nephropathy. J. Clin. Invest. 131, e140453 (2021). This article provides the first demonstration of the pathogenic role of modified IgG4 specific for PLA2R in lectin pathway activation.
Ghiggeri, G. M. et al. Multi-autoantibody signature and clinical outcome in membranous nephropathy. Clin. J. Am. Soc. Nephrol. 15, 1762–1776 (2020).
Seikrit, C., Ronco, P. & Debiec, H. Factor H autoantibodies and membranous nephropathy. N. Engl. J. Med. 379, 2479–2481 (2018).
Barbour, S. J. et al. Disease-specific risk of venous thromboembolic events is increased in idiopathic glomerulonephritis. Kidney Int. 81, 190–195 (2012).
Kerlin, B. A., Ayoob, R. & Smoyer, W. E. Epidemiology and pathophysiology of nephrotic syndrome-associated thromboembolic disease. Clin. J. Am. Soc. Nephrol. 7, 513–520 (2012).
Lionaki, S. et al. Venous thromboembolism in patients with membranous nephropathy. Clin. J. Am. Soc. Nephrol. 7, 43–51 (2012).
Cattran D. C. et al. (eds) National Kidney Foundation’s Primer on Kidney Diseases 7th Edn 188–197 (Elsevier, 2018).
Agrawal, S., Zaritsky, J. J., Fornoni, A. & Smoyer, W. E. Dyslipidaemia in nephritic syndrome: mechanisms and treatment. Nat. Rev. Nephrol. 14, 57–70 (2018).
Rodriguez, E. F. et al. Membranous nephropathy with crescents: a series of 19 cases. Am. J. Kidney Dis. 64, 66–73 (2014).
Fogo, A. B., Lusco, M. A., Najafian, B. & Alpers, C. E. Atlas of renal pathology: membranous nephropathy. Am. J. Kidney Dis. 66, e43–e45 (2015).
Beck, L. H., Fervenza, F. C. In Molecular Mechanisms in the Pathogenesis of Idiopathic Nephrotic Syndrome (ed. Kaneko, K.) 181–205 (Springer Japan, 2016).
Markowitz, G. S. Membranous glomerulopathy: emphasis on secondary forms and disease variants. Adv. Anat. Pathol. 8, 119–125 (2001).
Kuroki, A. et al. Glomerular and serum IgG subclasses in diffuse proliferative lupus nephritis, membranous lupus nephritis, and idiopathic membranous nephropathy. Intern. Med. 41, 936–942 (2002).
Ronco, P., Plaisier, E. & Debiec, H. Advances in membranous nephropathy. J. Clin. Med. 10, 607 (2021).
Qu, Z. et al. Absence of glomerular IgG4 deposition in patients with membranous nephropathy may indicate malignancy. Nephrol. Dial. Transplant. 27, 1931–1937 (2012).
von Haxthausen, F. et al. Antigen-specific IgG subclasses in primary and malignancy-associated membranous nephropathy. Front. Immunol. 9, 3035 (2018).
van de Logt, A. E., Hofstra, J. M. & Wetzels, J. F. Serum anti-PLA2R antibodies can be initially absent in idiopathic membranous nephropathy: seroconversion after prolonged follow-up. Kidney Int. 87, 1263–1264 (2015).
Debiec, H. & Ronco, P. PLA2R autoantibodies and PLA2R glomerular deposits in membranous nephropathy. N. Engl. J. Med. 364, 689–690 (2011).
Svobodova, B., Honsova, E., Ronco, P., Tesar, V. & Debiec, H. Kidney biopsy is a sensitive tool for retrospective diagnosis of PLA2R-related membranous nephropathy. Nephrol. Dial. Transplant. 28, 1839–1844 (2013).
Luo, J., Zhang, W., Su, C., Zhou, Z. & Wang, G. Seropositive PLA2R-associated membranous nephropathy but biopsy-negative PLA2R staining. Nephrol. Dial. Transplant. https://doi.org/10.1093/ndt/gfaa239 (2020).
Poggio, E. D. et al. Systematic review and meta-analysis of native kidney biopsy complications. Clin. J. Am. Soc. Nephrol. 15, 1595–1602 (2020).
Pombas, B. et al. Risk factors associated with major complications after ultrasound-guided percutaneous renal biopsy of native kidneys. Kidney Blood. Press. Res. 45, 122–130 (2020).
Palsson, R. et al. Bleeding complications after percutaneous native kidney biopsy: results from the Boston Kidney Biopsy cohort. Kidney Int. Rep. 5, 511–518 (2020).
Atwell, T. D. et al. The timing and presentation of major hemorrhage after 18,947 image-guided percutaneous biopsies. Am. J. Roentgenol. 205, 190–195 (2015).
Bobart, S. A. et al. Noninvasive diagnosis of primary membranous nephropathy using phospholipase A2 receptor antibodies. Kidney Int. 95, 429–438 (2019).
Bobart, S. A. et al. Kidney biopsy is required for nephrotic syndrome with PLA2R+ and normal kidney function: the Con View. Kidney 360, 890–893 (2020).
Kidney Disease: Improving Global Outcomes (KDIGO) Glomerular Diseases Work Group. KDIGO 2021 Clinical Practice Guideline for the Management of Glomerular Diseases. Kidney Int. 100, S1–S276 (2021). A milestone for the management of glomerular diseases.
Bobart, S. A. et al. A target antigen-based approach to the classification of membranous nephropathy. Mayo Clin. Proc. 96, 577–591 (2021).
Larsen, C. P. et al. Determination of primary versus secondary membranous glomerulopathy utilizing phospholipase A2 receptor staining in renal biopsies. Mod. Pathol. 26, 709–715 (2013).
Stehle, T. et al. Phospholipase A2 receptor and sarcoidosis-associated membranous nephropathy. Nephrol. Dial. Transplant. 30, 1047–1050 (2015).
Xie, Q. et al. Renal phospholipase A2 receptor in hepatitis B virus-associated membranous nephropathy. Am. J. Nephrol. 41, 345–353 (2015).
Berchtold, L. et al. Efficacy and safety of rituximab in hepatitis B virus-associated PLA2R-positive membranous nephropathy. Kidney Int. Rep. 3, 486–491 (2018).
Qin, W. et al. Anti-phospholipase A2 receptor antibody in membranous nephropathy. J. Am. Soc. Nephrol. 22, 1137–1143 (2011).
Hanset, N. et al. Podocyte antigen staining to identify distinct phenotypes and outcomes in membranous nephropathy: a retrospective multicenter cohort study. Am. J. Kidney Dis. 76, 624–635 (2020).
Zhang, Z. et al. Duodenal schwannoma as a rare association with membranous nephropathy: a case report. Am. J. Kidney Dis. 73, 278–280 (2019).
Zaghrini, C. et al. Novel ELISA for thrombospondin type 1 domain-containing 7A autoantibodies in membranous nephropathy. Kidney Int. 95, 666–679 (2019).
Sharma, S. G. & Larsen, C. P. Tissue staining for THSD7A in glomeruli correlates with serum antibodies in primary membranous nephropathy: a clinicopathological study. Mod. Pathol. 31, 616–622 (2018).
Schlumberger, W. et al. Differential diagnosis of membranous nephropathy with autoantibodies to phospholipase A2 receptor 1. Autoimmun. Rev. 13, 108–113 (2014).
Timmermans, S. A. et al. Evaluation of anti-PLA2R1 as measured by a novel ELISA in patients with idiopathic membranous nephropathy: a cohort study. Am. J. Clin. Pathol. 142, 29–34 (2014).
Liu, Y. et al. Serum anti-PLA2R antibody as a diagnostic biomarker of idiopathic membranous nephropathy: the optimal cut-off value for Chinese patients. Clin. Chim. Acta 476, 9–14 (2018).
Behnert, A. et al. Antiphospholipase A2 receptor autoantibodies: a comparison of three different immunoassays for the diagnosis of idiopathic membranous nephropathy. J. Immunol. Res. 2014, 143274 (2014).
Pourcine, F. et al. Prognostic value of PLA2R autoimmunity detected by measurement of anti-PLA2R antibodies combined with detection of PLA2R antigen in membranous nephropathy. A single-centre study over 14 years. PLoS ONE 12, e0173201 (2017).
Plaisier, E. & Ronco, P. Screening for cancer in patients with glomerular diseases. Clin. J. Am. Soc. Nephrol. 15, 886–888 (2020).
Cambier, J. F. & Ronco, P. Onco-nephrology: glomerular diseases with cancer. Clin. J. Am. Soc. Nephrol. 7, 1701–1712 (2012).
Timmermans, S. A. et al. Anti-phospholipase A2 receptor antibodies and malignancy in membranous nephropathy. Am. J. Kidney Dis. 62, 1223–1225 (2013).
Wang, G. et al. Neural epidermal growth factor-Like 1 protein-positive membranous nephropathy in Chinese patients. Clin. J. Am. Soc. Nephrol. 8, 727–735 (2021).
Ayalon, R. & Beck, L. H. Jr Membranous nephropathy: not just a disease for adults. Pediatr. Nephrol. 30, 31–39 (2015).
Debiec, H., Ronco, P. & Vivarelli, M. Congenital membranous nephropathy due to fetomaternal anti-neutral endopeptidase alloimmunization. Orphanet https://www.orpha.net/consor/cgi-bin/OC_Exp.php?lng=EN&Expert=69063 (2020).
Bhimma, R. & Coovadia, H. M. Hepatitis B virus-associated nephropathy. Am. J. Nephrol. 24, 198–211 (2004).
Safar-Boueri, L., Piya, A., Beck, L. H. Jr & Ayalon, R. Membranous nephropathy: diagnosis, treatment, and monitoring in the post-PLA2R era. Pediatr. Nephrol. 36, 19–30 (2021).
Debiec, H. et al. Allo-immune membranous nephropathy and recombinat arylsulfatase replacement therapy: a need for tolerance induction therapy. J. Am. Soc. Nephrol. 25, 675–680 (2014).
Wang, R. et al. Long-term renal survival and related risk factors for primary membranous nephropathy in Chinese children: a retrospective analysis of 217 cases. J. Nephrol. 34, 589–596 (2021).
Ramachandran R. & Jha, V. in Glomerulonephritis (eds Trachtman H., Hogan J. J., Herlitz L. & Lerma E. V.) (Springer, 2020).
Htay, H. et al. Global access of patients with kidney disease to health technologies and medications: findings from the Global Kidney Health Atlas project. Kidney Int. Suppl. 8, 64–73 (2018).
Hepatitis B Foundation. World Health Organization. Addressing Hepatitis B in Africa. Hepatitis B Foundation https://www.hepb.org/blog/addressing-hepatitis-b-africa/ (2020).
Kumar, M. N. et al. Membranous nephropathy associated with indigenous Indian medications containing heavy metals. Kidney Int. Rep. 5, 1510–1514 (2020).
Landrigan, P. J. et al. The Lancet Commission on pollution and health. Lancet 391, 462–512 (2018).
Gupta, S., Pepper, R. J., Ashman, N. & Walsh, S. B. Nephrotic syndrome: oedema formation and its treatment with diuretics. Front. Physiol. 9, 1868 (2019).
Hinrichs, G. R., Jensen, B. L. & Svenningsen, P. Mechanisms of sodium retention in nephrotic syndrome. Curr. Opin. Nephrol. Hypertens. 29, 207–212 (2020).
Kidney Disease: Improving Global Outcomes (KDIGO) Glomerulonephritis Work Group. KDIGO clinical practice guideline for glomerulonephritis. Kidney Int. Suppl. 2, 186–197 (2012).
Polanco, N. et al. Spontaneous remission of nephrotic syndrome in idiopathic membranous nephropathy. J. Am. Soc. Nephrol. 2, 697–704 (2020).
Pincus, K. J. & Hynicka, L. M. Prophylaxis of thromboembolic events in patients with nephrotic syndrome. Ann. Pharmacother. 47, 725–734 (2013).
Medjeral-Thomas, N. et al. Retrospective analysis of a novel regimen for the prevention of venous thromboembolism in nephrotic syndrome. Clin. J. Am. Soc. Nephrol. 9, 478–483 (2014).
Hofstra, J. M. & Wetzels, J. F. M. Should aspirin be used for primary prevention of thrombotic events in patients with membranous nephropathy? Kidney Int. 89, 981–983 (2016).
Sexton, D. J. et al. Direct-acting oral anticoagulants as prophylaxis against thromboembolism in the nephrotic syndrome. Kidney Int. Rep. 3, 784–793 (2018).
Reynolds, M. L., Nachman, P. H., Mooberry, M. J., Crona, D. J. & Derebail, V. K. Recurrent venous thromboembolism in primary membranous nephropathy despite direct Xa inhibitor therapy. J. Nephrol. 32, 669–672 (2019).
van de Logt, A. E., Hofstra, J. M. & Wetzels, J. F. Pharmacological treatment of primary membranous nephropathy in 2016. Expert Rev. Clin. Pharmacol. 9, 1463–1478 (2016).
van den Brand, J. A., van Dijk, P. R., Hofstra, J. M. & Wetzels, J. F. Long-term outcomes in idiopathic membranous nephropathy using a restrictive treatment strategy. J. Am. Soc. Nephrol. 25, 150–158 (2014).
Reichert, L. J., Koene, R. A. & Wetzels, J. F. Prognostic factors in idiopathic membranous nephropathy. Am. J. Kidney Dis. 31, 1–11 (1998).
Hladunewich, M. A., Troyanov, S., Calafati, J. & Cattran, D. C. Metropolitan Toronto Glomerulonephritis Registry. The natural history of the non-nephrotic membranous nephropathy patient. Clin. J. Am. Soc. Nephrol. 4, 1417–1422 (2009).
Hoxha, E., Harendza, S., Pinnschmidt, H., Panzer, U. & Stahl, R. A. PLA2R antibody levels and clinical outcome in patients with membranous nephropathy and non-nephrotic range proteinuria under treatment with inhibitors of the renin-angiotensin system. PLoS ONE 9, e110681 (2014).
Pei, Y., Cattran, D. & Greenwood, C. Predicting chronic renal insufficiency in idiopathic membranous glomerulonephritis. Kidney Int. 42, 960–966 (1992).
Howman, A. et al. Immunosuppression for progressive membranous nephropathy: a UK randomised controlled trial. Lancet 381, 744–751 (2013).
Cattran, D. C. et al. Validation of a predictive model of idiopathic membranous nephropathy: its clinical and research implications. Kidney Int. 51, 901–907 (1997).
van den Brand, J. A., Hofstra, J. M. & Wetzels, J. F. Prognostic value of risk score and urinary markers in idiopathic membranous nephropathy. Clin. J. Am. Soc. Nephrol. 7, 1242–1248 (2012).
van de Logt, A. E. et al. Anti-PLA2R1 antibodies as prognostic biomarker in membranous nephropathy. Kidney Int. Rep. 6, 1677–1686 (2021).
Lerner, G. B., Virmani, S., Henderson, J. M., Francis, J. M. & Beck, L. H. Jr. A conceptual framework linking immunology, pathology, and clinical features in primary membranous nephropathy. Kidney Int. 100, 289–300 (2021).
Faul, C. et al. The actin cytoskeleton of kidney podocytes is a direct target of the antiproteinuric effect of cyclosporine A. Nat. Med. 14, 931–938 (2008).
Ramachandran, R. et al. Two-year follow-up study of membranous nephropathy treated with tacrolimus and corticosteroids versus cyclical corticosteroids and cyclophosphamide. Kidney Int. Rep. 2, 610–616 (2017).
van de Logt, A. E. et al. Immunological remission in PLA2R-antibody-associated membranous nephropathy: cyclophosphamide versus rituximab. Kidney Int. 93, 1016–1017 (2018).
Hanset, N. et al. Rituximab in patients with phospholipase A2 receptor-associated membranous nephropathy and severe CKD. Kidney Int. Rep. 5, 331–338 (2019).
Dahan, K. et al. Retreatment with rituximab for membranous nephropathy with persistently elevated titers of anti-phospholipase A2 receptor antibody. Kidney Int. 95, 233–234 (2019).
van de Logt, A. E. et al. The bias between different albumin assays may affect clinical decision-making. Kidney Int. 95, 1514–1517 (2019).
Bech, A. P., Hofstra, J. M., Brenchley, P. E. & Wetzels, J. F. Association of anti-PLA2R antibodies with outcomes after immunosuppressive therapy in idiopathic membranous nephropathy. Clin. J. Am. Soc. Nephrol. 9, 1386–1392 (2014).
Filler, G. et al. Another case of HBV associated membranous glomerulonephritis resolving on lamivudine. Arch. Dis. Child. 88, F154–F156 (2003).
O’Shaughnessy, M. M. et al. Treatment patterns among adults and children with membranous nephropathy in the Cure Glomerulonephropathy Network (CureGN). Kidney Int. Rep. 4, 1725–1734 (2019).
Riaz, P. et al. Workforce capacity for the care of patients with kidney failure across world countries and regions. BMJ Glob. Health 6, e004014 (2021).
Jha, V. et al. Understanding kidney care needs and implementation strategies in low- and middle-income countries: conclusions from a “Kidney Disease: Improving Global Outcomes” (KDIGO) controversies conference. Kidney Int. 90, 1164–1174 (2016).
Cosio, F. G. & Cattran, D. C. Recent advances in our understanding of recurrent primary glomerulonephritis after kidney transplantation. Kidney Int. 91, 304–314 (2017).
Grupper, A. et al. Recurrent membranous nephropathy after kidney transplantation: treatment and long-term implications. Transplantation 100, 2710–2716 (2016).
Seitz-Polski, B. et al. Prediction of membranous nephropathy recurrence after transplantation by monitoring of anti-PLA2R1 (M-type phospholipase A2 receptor) autoantibodies: a case series of 15 patients. Nephrol. Dial. Transplant. 29, 2334–2342 (2014).
Quintana, L. F. et al. Antiphospholipase A2 receptor antibody levels predict the risk of posttransplantation recurrence of membranous nephropathy. Transplantation 99, 1709–1714 (2015).
Andrésdóttir, M. B. & Wetzels, J. F. Increased risk of recurrence of membranous nephropathy after related donor kidney transplantation. Am. J. Transplant. 12, 265–266 (2012).
Gupta, G. et al. Pre-transplant phospholipase A2 receptor autoantibody concentration is associated with clinically significant recurrence of membranous nephropathy post-kidney transplantation. Clin. Transplant. 30, 461–469 (2016).
Batal, I. et al. Association of HLA typing and alloimmunity with posttransplantation membranous nephropathy: a multicenter case series. Am. J. Kidney Dis. 76, 374–383 (2020).
Kattah, A. et al. Anti-phospholipase A2 receptor antibodies in recurrent membranous nephropathy. Am. J. Transplant. 15, 1349–1359 (2015).
WHO. Programme on Mental Health. WHOQOL User Manual (World Health Organization, 1998).
Wyld, M., Morton, R. L., Hayen, A., Howard, K. & Webster, A. C. A systematic review and meta-analysis of utility-based quality of life in chronic kidney disease treatments. PLoS Med. 9, e1001307 (2012).
Chuasuwan, A., Pooripussarakul, S., Thakkinstian, A., Ingsathit, A. & Pattanaprateep, O. Comparisons of quality of life between patients underwent peritoneal dialysis and hemodialysis: a systematic review and meta-analysis. Health Qual. Life. Outcomes 18, 191 (2020).
Canetta, P. A. et al. Health-related quality of life in glomerular disease. Kidney Int. 95, 1209–1224 (2019).
Cattran, D. Management of membranous nephropathy: when and what for treatment. J. Am. Soc. Nephrol. 16, 1188–1194 (2005).
Libório, A. B. et al. Proteinuria is associated with quality of life and depression in adults with primary glomerulopathy and preserved renal function. PLoS ONE 7, e37763 (2012).
Floege, J. et al. Management and treatment of glomerular diseases (part 1): conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) controversies conference. Kidney Int. 95, 268–280 (2019).
Murphy, S. L. et al. Longitudinal changes in health-related quality of life in primary glomerular disease: results from the CureGN study. Kidney Int. Rep. 5, 1679–1689 (2020).
Center for Drug Evaluation and Research, Center for Devices and Radiological Health and Center for Biologics Evaluation and Research. Guidance for Industry. Patient-Reported Outcome Measures: Use in Medical Product Development To Support Labeling Claims (FDA, 2009).
Bansal, D., Bhagat, A., Schifano, F. & Gudala, K. Role of patient-reported outcomes and other efficacy endpoints in the drug approval process in Europe (2008-2012). J. Epidemiol. Glob. Health 5, 385–395 (2015).
Carter, S. A. et al. Identifying outcomes important to patients with glomerular disease and their caregivers. Clin. J. Am. Soc. Nephrol. 15, 673–684 (2020).
Henkel, C. & Hoffmann, P. (Eds) MALDI Imaging. Biochim. Biophys. Acta 1865, 725–978 (2017).
Neumann, E. K., Djambazova, K. V., Caprioli, R. M. & Spraggins, J. M. Multimodal imaging mass spectrometry: next generation molecular mapping in biology and medicine. J. Am. Soc. Mass. Spectrom. 31, 2401–2415 (2020).
Unnersjö-Jess, D., Scott, L., Blom, H. & Brismar, H. Super-resolution stimulated emission depletion imaging of slit diaphragm proteins in optically cleared kidney tissue. Kidney Int. 89, 243–247 (2016).
Park, J., Liu, C. L., Kim, J. & Susztak, K. Understanding the kidney one cell at a time. Kidney Int. 96, 862–870 (2019).
Ellebrecht, C. T. et al. Reengineering chimeric antigen receptor T cells for targeted therapy of autoimmune disease. Science 353, 179–184 (2016).
Wraith, D. Autoimmunity: antigen-specific immunotherapy. Nature 530, 422–423 (2016).
Abedini, A. et al. Urinary single-cell profiling captures the cellular diversity of the kidney. J. Am. Soc. Nephrol. 32, 614–627 (2021).
Unlu, G. et al. GRIK5 genetically regulated expression associated with eye and vascular phenomes: discovery through iteration among biobanks, electronic health records, and Zebrafish. Am. J. Hum. Genet. 104, 503–519 (2019).
Reddy, V. et al. Obinutuzumab induces superior B-cell cytotoxicity to rituximab in rheumatoid arthritis and systemic lupus erythematosus patient samples. Rheumatology 56, 1227–1237 (2017).
Klomjit, N., Fervenza, F. C. & Zand, L. Successful treatment of patients with refractory PLA2 R-associated membranous nephropathy with obinutuzumab: a report of 3 cases. Am. J. Kidney Dis. 76, 883–888 (2020).
Podestà, M. A., Ruggiero, B., Remuzzi, G. & Ruggenenti, P. Ofatumumab for multirelapsing membranous nephropathy complicated by rituximab-induced serum- sickness. BMJ Case. Rep. 13, e232896 (2020).
Schmidt, T., Schulze, M., Harendza, S. & Hoxha, E. Successful treatment of PLA2R1-antibody positive membranous nephropathy with ocrelizumab. J. Nephrol. 34, 603–606 (2021).
Samy, E., Wax, S., Huard, B., Hess, H. & Schneider, P. Targeting BAFF and APRIL in systemic lupus erythematosus and other antibody-associated diseases. Int. Rev. Immunol. 36, 3–19 (2017).
Mahévas, M. et al. Efficacy, safety and immunological profile of combining rituximab with belimumab for adults with persistent or chronic immune thrombocytopenia: results from a prospective phase 2b trial. Haematologica https://doi.org/10.3324/haematol.2020.259481 (2020).
Furie, R. et al. Two-year, randomized, controlled trial of belimumab in lupus nephritis. N. Engl. J. Med. 383, 1117–1128 (2020).
Barrett, C. et al. Effect of belimumab on proteinuria and anti-phospholipase A2 receptor autoantibody in primary membranous nephropathy. Nephrol. Dial. Transplant. 35, 599–606 (2020).
Crickx, E., Weill, J. C., Reynaud, C. A. & Mahévas, M. Anti-CD20-mediated B-cell depletion in autoimmune diseases: successes, failures and future perspectives. Kidney Int. 97, 885–893 (2020).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT04145440 (2021).
Weinmann-Menke, J. et al. Treatment of membranous nephropathy in patients with THSD7A antibodies using immunoadsorption. Am. J. Kidney Dis. 74, 849–852 (2019).
Podestà, M. A. et al. Accelerating the depletion of circulating anti-phospholipase A2 receptor antibodies in patients with severe membranous nephropathy: preliminary findings with double filtration plasmapheresis and ofatumumab. Nephron 144, 30–35 (2020).
Zipfel, P. F. et al. Complement inhibitors in clinical trials for glomerular diseases. Front. Immunol. 10, 2166 (2019).
Low, J. H. et al. Generation of human PSC-derived kidney organoids with patterned nephron segments and a de novo vascular network. Cell Stem. Cell 25, 373–387 (2019).
Maas, R. J. et al. Kidney injury molecule-1 and neutrophil gelatinase-associated lipocalin as prognostic markers in idiopathic membranous nephropathy. Ann. Clin. Biochem. 53, 51–57 (2016).
van den Brand, J. A., Hofstra, J. M. & Wetzels, J. F. Low-molecular-weight proteins as prognostic markers in idiopathic membranous nephropathy. Clin. J. Am. Soc. Nephrol. 6, 2846–2853 (2011).
Acknowledgements
L.B. acknowledges institutional funding for the Glomerular Disease Center at Boston Medical Center in support of the preparation of this manuscript. J.W. acknowledges support from grants from the Dutch Kidney Foundation (grant nrNSN 17PhD12), funding from European Union Seventh Framework Programme FP7/2007-2013 grant 305608: European Consortium for High-Throughput Research in Rare Kidney Diseases. V.J. acknowledges research grants from Baxter Healthcare, GSK, and NephroPlus and honoraria/speaker fees from Baxter Healthcare and AstraZeneca (all monies paid to the employer). P.R. acknowledges support from grants from the National Research Agency: MNaims (ANR-17-CE17-0012-01) and SeroNegMN (ANR-20-CE17-0017-01). F.C.F. acknowledges unrestricted research grants from Genentech Inc., Roche and MorphoSys for research on Membranous Nephropathy (all funds paid to the institution). M.V., P.R. and J.W. acknowledge the European Rare Kidney Disease Network (ERKNet). A.T. is supported by a National Health and Medical Research Council Investigator Award (1197324). F.F.H. acknowledges support from the Clinical Innovation Research Program of Guangzhou Regenerative Medicine and Health Guangdong Laboratory (2018GZR0201003).
Author information
Authors and Affiliations
Contributions
Introduction (P.R.); Epidemiology (P.R. and F.F.H.); Mechanisms/pathophysiology (L.B., H.D. and S.S.); Diagnosis/screening/prevention (F.C.F., V.J. and M.V.); Management (V.J., M.V. and J.W.); Quality of life (V.J. and A.T.); Outlooks (P.R. and L.B.); Overview of the Primer (P.R.).
Corresponding author
Ethics declarations
Competing interests
L.B. is co-inventor on the patent “Diagnostics for Membranous Nephropathy” and has received consultancy fees from Alexion, Ionis, Genentech and Visterra for topics related to membranous nephropathy as well as research support from Sanofi Genzyme and Pfizer. P.R. has received consultancy fees from Alexion and MorphoSys for topics related to membranous nephropathy. F.C.F. has received consultancy fees from Alexion and MorphoSys for topics related to membranous nephropathy. F.F.H. has received consultancy fees from AbbVie and AstraZeneca. J.W. has received consultancy fees from Novartis and MorphoSys for topics related to membranous nephropathy. The other authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Disease Primers thanks L. Barisoni, S. Maruyama and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Glossary
- Podocytopathy
-
A disease of the podocyte, the main glomerular cell controlling the filtration of proteins.
- Glomerular filtration rate
-
(GFR). The most reliable parameter to assess renal function and can be evaluated with formulas (eGFR) or measured (mGFR).
- Heymann nephritis
-
A model of membranous nephropathy developed by Walter Heymann in the rat in the 1950s that is still the most reliable experimental model for human membranous nephropathy.
- Allo-immunization
-
Immunization against a non-self human antigen (protein or sugar) as occurs after blood transfusions or in case of Rhesus incompatibility during pregnancy, resulting in the production of allo-antibodies.
- Epitope spreading
-
Diffusion of the immune response to additional epitopes on the same molecule or different molecules.
- Full-house pattern
-
Immunofluorescence studies show staining for IgA, IgG, IgM, C1q, C3, κ and λ light chains.
- Xeno-antibodies
-
Production of xeno-antibodies results from immunization against a non-self, non-human antigen (protein or sugar); a process termed xeno-immunization.
- Anaphylatoxins
-
One of several proteolytic fragments generated by complement activation that promote acute inflammation and mediation of the immune response.
- Anasarca
-
Severe and generalized form of oedema, with subcutaneous tissue swelling, that usually involves the cavities of the body.
- Thrombophilic state
-
A pathological condition that predisposes to thrombosis.
Rights and permissions
About this article
Cite this article
Ronco, P., Beck, L., Debiec, H. et al. Membranous nephropathy. Nat Rev Dis Primers 7, 69 (2021). https://doi.org/10.1038/s41572-021-00303-z
Accepted:
Published:
DOI: https://doi.org/10.1038/s41572-021-00303-z
This article is cited by
-
PLA2R-positive membranous nephropathy in IgG4-related disease
BMC Nephrology (2024)
-
Serum uric acid level is associated with glomerular ischemic lesions in patients with primary membranous nephropathy: an analytical, cross-sectional study
Scientific Reports (2024)
-
A guide to complement biology, pathology and therapeutic opportunity
Nature Reviews Immunology (2024)
-
Significance of the total renal chronicity score in predicting renal outcome in PLA2R-associated membranous nephropathy
Journal of Nephrology (2024)
-
Causal association between cardiovascular proteins and membranous nephropathy: a bidirectional Mendelian randomization
International Urology and Nephrology (2024)