Abstract
The prevention of type 2 diabetes mellitus (T2DM) is a target priority for the WHO and the United Nations and is a key priority in the 2018 Berlin Declaration, which is a global call for early actions related to T2DM. Health-care policies advocate that individuals at high risk of developing T2DM undertake lifestyle modification, irrespective of whether the prediabetes phenotype is defined by hyperglycaemia in the postprandial state (impaired glucose tolerance) and/or fasting state (impaired fasting glucose) or by intermediate HbA1c levels. However, current evidence indicates that diabetes prevention programmes based on lifestyle change have not been successful in preventing T2DM in individuals with isolated impaired fasting glucose. We propose that further research is needed to identify effective lifestyle interventions for individuals with isolated impaired fasting glucose. Furthermore, we call for the identification of innovative approaches that better identify people with impaired glucose tolerance, who benefit from the currently available lifestyle-based diabetes prevention programmes.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
International Diabetes Federation. IDF Diabetes Atlas, Ninth Edition 2019 (IDF, 2019).
Herman, W. H. The economic costs of diabetes: is it time for a new treatment paradigm? Diabetes Care. 36, 775–776 (2013).
World Health Organiszation. Global Report on Diabetes (WHO, 2016).
United Nations General Assembly. Political Declaration of the High-Level Meeting of the General Assembly on the Prevention and Control of Non-Communicable Diseases (UN, 2012).
Khunti, K. et al. The Berlin Declaration: a call to improve early actions related to type 2 diabetes. Why is primary care important? Prim. Care Diabetes 12, 383–392 (2018).
American Diabetes Association. Standards of medical care in diabetes — 2017 abridged for primary care providers. Clin. Diabetes 35, 5–26 (2017).
Waugh, N. R., Shyangdan, D., Taylor-Phillips, S., Suri, G. & Hall, B. Screening for type 2 diabetes: a short report for the national screening committee. Health Technol. Assess. 17, 1–90 (2013).
Albright, A. L. & Gregg, E. W. Preventing type 2 diabetes in communities across the U.S.: the National Diabetes Prevention Program. Am. J. Prev. Med. 44, S346–S351 (2013).
Diabetes Prevention Program Research Group. The Diabetes Prevention Program (DPP): description of lifestyle intervention. Diabetes Care 25, 2165–2171 (2002).
Ramachandran, A. et al. The Indian Diabetes Prevention Programme shows that lifestyle modification and metformin prevent type 2 diabetes in Asian Indian subjects with impaired glucose tolerance (IDPP-1). Diabetologica 49, 289–297 (2006).
Knowler, W. C. et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N. Engl. J. Med. 346, 393–403 (2002).
Tuomilehto, J. et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N. Engl. J. Med. 344, 1343–1350 (2001).
Pan, X. R. et al. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance: the Da Qing IGT and Diabetes Study. Diabetes Care. 20, 537–544 (1997).
Lindstrom, J. et al. Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention: follow-up of the Finnish Diabetes Prevention Study. Lancet 368, 1673–1679 (2006).
Li, G. et al. The long-term effect of lifestyle interventions to prevent diabetes in the China Da Qing Diabetes Prevention Study: a 20-year follow-up study. Lancet 371, 1783–1789 (2008).
Diabetes Prevention Program Research Group. 10-year follow-up of diabetes incidence and weight loss in the diabetes prevention program outcomes study. Lancet 374, 1677–1686 (2009).
Gillies, C. L. et al. Pharmacological and lifestyle interventions to prevent or delay type 2 diabetes in people with impaired glucose tolerance: systematic review and meta-analysis. Br. Med. J. 334, 299 (2007).
Barry, E. et al. Efficacy and effectiveness of screen and treat policies in prevention of type 2 diabetes: systematic review and meta-analysis of screening tests and interventions. Br. Med. J. 356, i6538 (2017).
Gong, Q. et al. Morbidity and mortality after lifestyle intervention for people with impaired glucose tolerance: 30-year results of the Da Qing Diabetes Prevention Outcome Study. Lancet Diabetes Endocrinol. 7, 452–461 (2019).
American Diabetes Association. Classification and diagnosis of diabetes: standards of medical care in diabetes—2019. Diabetes Care 42, S13–S28 (2019).
World Health Organization. Definition and Diagnosis of Diabetes Mellitus and Intermediate Hyperglycemia: Report of a WHO/IFG Consultation (WHO, 2006).
Yip, W. C. Y., Sequeira, I. R., Plank, L. D. & Poppitt, S. D. Prevalence of pre-diabetes across ethnicities: a review of impaired fasting glucose (IFG) and impaired glucose tolerance (IGT) for classification of dysglycaemia. Nutrients 9, E1273 (2017).
Eades, C. E., France, E. F. & Evans, J. M. Prevalence of impaired glucose regulation in Europe: a meta-analysis. Eur. J. Public Health 26, 699–706 (2016).
Sentell, T. L., He, G., Gregg, E. W. & Schillinger, D. Racial/ethnic variation in prevalence estimates for United States prediabetes under alternative 2010 American Diabetes Association criteria: 1988-2008. Ethn. Dis. 22, 451–458 (2012).
Anjana, R. M. et al. Prevalence of diabetes and prediabetes in 15 states of India: results from the ICMR-INDIAB population-based cross-sectional study. Lancet Diabetes Endocrinol. 5, 585–596 (2017).
Kosaka, K., Noda, M. & Kuzuya, T. Prevention of type 2 diabetes by lifestyle intervention: a Japanese trial in IGT males. Diabetes Res. Clin. Pract. 67, 152–162 (2005).
Weber, M. B. et al. The stepwise approach to diabetes prevention: results from the D-CLIP randomized controlled trial. Diabetes Care 39, 1760–1767 (2016).
Saito, T. et al. Lifestyle modification and prevention of type 2 diabetes in overweight Japanese with impaired fasting glucose levels: a randomized controlled trial. Arch. Intern. Med. 171, 1352–1360 (2011).
Thankappan, K. R. et al. A peer-support lifestyle intervention for preventing type 2 diabetes in India: a cluster-randomized controlled trial of the Kerala diabetes prevention program. PLoS Med. 15, e1002575 (2018).
Davies, M. J. et al. A community based primary prevention programme for type 2 diabetes integrating identification and lifestyle intervention for prevention: the Let’s Prevent Diabetes cluster randomised controlled trial. Prev. Med. 84, 48–56 (2016).
Wareham, N. J. & Pfister, R. Diabetes: glycated hemoglobin is a marker of diabetes and CVD risk. Nat. Rev. Cardiol. 7, 367–368 (2010).
Aziz, Z., Absetz, P., Oldroyd, J., Pronk, N. P. & Oldenburg, B. A systematic review of real-world diabetes prevention programs: learnings from the last 15 years. Implement. Sci. 10, 172 (2015).
Franco, L. J. et al. Performance of glycated haemoglobin (HbA1c) as a screening test for diabetes and impaired glucose tolerance (IGT) in a high risk population—the Brazilian Xavante Indians. Diabetes Res. Clin. Pract. 106, 337–342 (2014).
Sequeira, I. R. & Poppitt, S. D. HbA1c as a marker of prediabetes: a reliable screening tool or not? Insights Nutr. Metab. 1, 21–29 (2017).
Noble, D., Mathur, R., Dent, T., Meads, C. & Greenhalgh, T. Risk models and scores for type 2 diabetes: systematic review. Br. Med. J. 343, d7163 (2011).
Costa, B. et al. Delaying progression to type 2 diabetes among high-risk Spanish individuals is feasible in real-life primary healthcare settings using intensive lifestyle intervention. Diabetologica 55, 1319–1328 (2012).
Anjana, R. M. et al. Incidence of diabetes and prediabetes and predictors of progression among Asian Indians: 10-year follow-up of the Chennai Urban Rural Epidemiology Study (CURES). Diabetes Care 38, 1441–1448 (2015).
Morris, D. H. et al. Progression rates from HbA1c 6.0-6.4% and other prediabetes definitions to type 2 diabetes: a meta-analysis. Diabetologica 56, 1489–1493 (2013).
Richter, B., Hemmingsen, B., Metzendorf, M. I. & Takwoingi, Y. Development of type 2 diabetes mellitus in people with intermediate hyperglycaemia. Cochrane Database Syst. Rev. 10, CD012661 (2018).
Kanat, M. et al. Distinct beta-cell defects in impaired fasting glucose and impaired glucose tolerance. Diabetes. 61, 447–453 (2012).
Faerch, K., Borch-Johnsen, K., Holst, J. J. & Vaag, A. Pathophysiology and aetiology of impaired fasting glycaemia and impaired glucose tolerance: does it matter for prevention and treatment of type 2 diabetes? Diabetologica 52, 1714–1723 (2009).
Glechner, A. et al. Effects of lifestyle changes on adults with prediabetes: a systematic review and meta-analysis. Prim. Care Diabetes 12, 393–408 (2018).
Faerch, K. et al. Natural history of insulin sensitivity and insulin secretion in the progression from normal glucose tolerance to impaired fasting glycemia and impaired glucose tolerance: the Inter99 study. Diabetes Care 32, 439–444 (2009).
Kanat, M. et al. Impaired early- but not late-phase insulin secretion in subjects with impaired fasting glucose. Acta Diabetol. 48, 209–217 (2011).
Gujral, U. P., Narayan, K. M., Kahn, S. E. & Kanaya, A. M. The relative associations of beta-cell function and insulin sensitivity with glycemic status and incident glycemic progression in migrant Asian Indians in the United States: the MASALA study. J. Diabetes Complicat. 28, 45–50 (2014).
O’Donoghue, G. et al. Phenotypic responses to a lifestyle intervention do not account for inter-individual variability in glucose tolerance for individuals at high risk of type 2 diabetes. Front. Physiol. 10, 317 (2019).
Kantartzis, K. et al. The impact of liver fat vs visceral fat in determining categories of prediabetes. Diabetologica 53, 882–889 (2010).
Borel, A. L. et al. Visceral, subcutaneous abdominal adiposity and liver fat content distribution in normal glucose tolerance, impaired fasting glucose and/or impaired glucose tolerance. Int. J. Obes. 39, 495–501 (2015).
Meyer, C. et al. Different mechanisms for impaired fasting glucose and impaired postprandial glucose tolerance in humans. Diabetes Care. 29, 1909–1914 (2006).
Faerch, K. et al. Impaired fasting glycaemia vs impaired glucose tolerance: similar impairment of pancreatic alpha and beta cell function but differential roles of incretin hormones and insulin action. Diabetologica 51, 853–861 (2008).
Healy, G. N., Dunstan, D. W., Shaw, J. E., Zimmet, P. Z. & Owen, N. Beneficial associations of physical activity with 2-h but not fasting blood glucose in Australian adults. Diabetes Care 29, 2598–2604 (2006).
Viscogliosi, G. et al. Mediterranean dietary pattern adherence: associations with prediabetes, metabolic syndrome, and related microinflammation. Metab. Syndr. Relat. Disord. 11, 210–216 (2013).
Marcinko, K. et al. High intensity interval training improves liver and adipose tissue insulin sensitivity. Mol. Metab. 4, 903–915 (2015).
Marquis-Gravel, G. et al. Intensive lifestyle intervention including high-intensity interval training program improves insulin resistance and fasting plasma glucose in obese patients. Prev. Med. Rep. 2, 314–318 (2015).
Lim, E. L. et al. Reversal of type 2 diabetes: normalisation of beta cell function in association with decreased pancreas and liver triacylglycerol. Diabetologica 54, 2506–2514 (2011).
Steven, S. et al. Weight loss decreases excess pancreatic triacylglycerol specifically in type 2 diabetes. Diabetes Care 39, 158–165 (2016).
Lean, M. E. et al. Primary care-led weight management for remission of type 2 diabetes (DiRECT): an open-label, cluster-randomised trial. Lancet 391, 541–551 (2018).
Taylor, R. Type 2 diabetes: etiology and reversibility. Diabetes Care 36, 1047–1055 (2013).
Armato, J. P., DeFronzo, R. A., Abdul-Ghani, M. & Ruby, R. J. Successful treatment of prediabetes in clinical practice using physiological assessment (STOP DIABETES). Lancet Diabetes Endocrinol. 6, 781–789 (2018).
Christensen, P. et al. Men and women respond differently to rapid weight loss: metabolic outcomes of a multi-centre intervention study after a low-energy diet in 2500 overweight, individuals with pre-diabetes (PREVIEW). Diabetes Obes. Metab. 20, 2840–2851 (2018).
Vistisen, D. et al. Reversion from prediabetes to normoglycaemia and risk of cardiovascular disease and mortality: the Whitehall II cohort study. Diabetologica 62, 1385–1390 (2019).
Abbasi, A. et al. A systematic review of biomarkers and risk of incident type 2 diabetes: an overview of epidemiological, prediction and aetiological research literature. PLoS One. 11, e0163721 (2016).
Walford, G. A. et al. Metabolite profiles of diabetes incidence and intervention response in the Diabetes Prevention Program. Diabetes 65, 1424–1433 (2016).
Dunseath, G. J. et al. Performance evaluation of a self-administered home oral glucose tolerance test kit in a controlled clinical research setting. Diabet. Med. 36, 862–867 (2019).
Bergman, M. et al. Petition to replace current OGTT criteria for diagnosing prediabetes with the 1-hour post-load plasma glucose>/=155mg/dl (8.6mmol/L). Diabetes Res. Clin. Pract. 146, 18–33 (2018).
Poplin, R. et al. Predicting cardiovascular risk factors from retinal fundus photographs using deep learning. Nat. Biomed. Eng. 2, 158–164 (2017).
International Expert Committee. International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care 32, 1327–1334 (2009).
Author information
Authors and Affiliations
Contributions
R.J.T., M.D.C. and T.S. researched data for the article and wrote the article. R.J.T., M.D.C., T.S., K.R.T., P.Z.Z., B.O., D.R.O. and J.E.S. contributed substantially to discussion of the content. All authors reviewed and edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Campbell, M.D., Sathish, T., Zimmet, P.Z. et al. Benefit of lifestyle-based T2DM prevention is influenced by prediabetes phenotype. Nat Rev Endocrinol 16, 395–400 (2020). https://doi.org/10.1038/s41574-019-0316-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41574-019-0316-1
This article is cited by
-
Low-calorie diets for people with isolated impaired fasting glucose
Communications Medicine (2024)
-
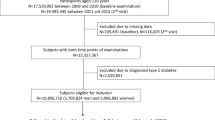
Relationship between BMI and risk of impaired glucose tolerance and impaired fasting glucose in Chinese adults: a prospective study
BMC Public Health (2023)
-
Effect of denosumab on glucose metabolism in postmenopausal osteoporotic women with prediabetes: a study protocol for a 12-month multicenter, open-label, randomized controlled trial
Trials (2023)
-
A nomogram model for predicting 5-year risk of prediabetes in Chinese adults
Scientific Reports (2023)
-
Personalized lifestyle change approaches for preventing type 2 diabetes in people with prediabetes
International Journal of Diabetes in Developing Countries (2023)