Abstract
Metabolic syndrome (MetS) increases the risk of cardiovascular diseases and diabetes mellitus. This study is designed to assess the prevalence and determinants of MetS among Nepalese adults from a nationally representative study. This study is based on Stepwise Approach to Surveillance (STEPS) Survey from Nepal. This survey was done among 4200 adults aged 15–69 years from 210 clusters selected proportionately across Nepal’s three ecological zones (Mountain, Hill and Terai). Subsequently, using systematic sampling, twenty households per cluster and one participant per household were selected. The overall prevalence of MetS is 15% and 16% according to Adult Treatment Panel III (ATP III) and International Diabetes Federation (IDF) criteria respectively. A triad of low HDL-C, abdominal obesity and high BP was the most prevalent (8.18%), followed by abdominal obesity, low HDL-C cholesterol and high triglycerides (8%). Less than two percent of participants had all the five components of the syndrome and 19% of participants had none. The prevalence steadily rose across the age group with adults aged 45–69 years having the highest prevalence (28–30%) and comparable prevalence across two definitions of MetS. A notably high burden for females, urban, hill or Terai resident were seen among other factors.
Similar content being viewed by others
Introduction
The inter-related cluster of cardio-metabolic risk factors comprising of elevated fasting glucose, elevated blood pressure, elevated triglycerides (TG), reduced high-density lipoprotein (HDL) and central obesity has been termed Metabolic syndrome (MetS) in the literature1. There is two fold increase in risk for cardiovascular disease and five fold increase in risk for type II diabetes in people with MetS compared to those without syndrome2,3. Hence treatment and prevention of MetS is of paramount importance as a means of lowering the risk of diabetes and cardiovascular disease (CVD).
There is large variation in global prevalence of MetS ranging from 7.1% to 41.6% across studies due to lack of consensus definition of MetS4,5,6. The most commonly used criteria are the International Diabetes Federation adopted in 2005 (IDF)7 and Adult Treatment Panel III (ATPIII) adopted in 20054. Although the mechanism of MetS has not been elucidated fully, various factors such as unhealthy diet, physical inactivity, urbanization and underlying genetic predisposition have been found to be associated with MetS8.
With rapid demographic and epidemiologic transition in Nepal, the burden of non-communicable diseases (NCDs), notably cardiovascular disease (CVD) has escalated to epidemic proportion9. A recent hospital based study conducted in a random sample of indoor patients from tertiary levels hospitals found that 31% of admitted patients suffer from NCDs; with cardiovascular disease and diabetes accounting for 40% and 12% of NCDs respectively10. This hospital based study might not reflect the true prevalence of NCDs at population level in Nepal as utilization of health services remains poor and urban-centric. The absence of routine surveillance and registry system in Nepal has further made it challenging to precisely estimate the burden of MetS11. An earlier prevalence study limited to eastern region of Nepal found one in five Nepalese adults have MetS12. This is comparable to studies from neighboring South Asian countries like India, Pakistan and Bangladesh where nearly a third of population have MetS13,14. None of the studies conducted thus far assessed the attributing factors in occurrence of MetS in Nepal.
The unavailability of nationally representative prevalence estimates and factors attributing on MetS has hindered the development of targeted strategies against MetS. A focus on individual components of MetS is a norm in routine practice, as well as the recently formed Multi-sectoral Action Plan of NCDs from Ministry of Health of Nepal addresses hypertension, diabetes, obesity and raised cholesterol separately while MetS is unaddressed giving the lack of evidence at population level. Hence, it is important to investigate the prevalence and determinants of MetS at entire-population level, using the nationally representative data. This is important for local planning, addressing the population burden via concerted actions on its determinants and targeting the high-risk groups.
Results
This secondary-analysis of the data provided by the nationally representive survey (STEPS Survey), provides the first nationally representative prevalence of MetS among adult population of Nepal. A total of 3729 participants aged 15 to 69 years were assessed for physical and biochemical parameters. The prevalence of metabolic syndrome is 15% and 16% according to ATP III and IDF criteria respectively. Overall, 21% of participants had had three or more risk factors. The most predominant component of MetS in this population was low HDL cholesterol (71%), followed by high blood pressure (26%) and raised triglycerides (25%). A significantly high prevalence of abdominal obesity and low HDL cholesterol was observed among female participants; whereas raised triglycerides, fasting blood sugar and high blood pressure was observed among male participants (Table 1).
A triad of low HDL-C, abdominal obesity and high BP was the most prevalent constituting 8.2% of the total participants, followed by abdominal obesity, low HDL-C cholesterol and high triglycerides at 8% of participants. Less than two percent of participants had all the five components of the syndrome (Table 1). Only 19% of participants had zero risk factors (Fig. 1).
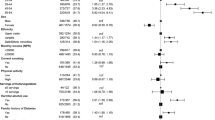
Table 2 presents the independent effect of various covariates on the clustering of MetS components at the individual level using multivariate Poisson regression. The age, education, caste/ethnicity, abnormal waist hip ratio, BMI and place of residence were independently associated with the number of MetS components. Moreover, the cumulative risk of having x number of MetS risk factors or more versus having fewer were 1.28 times higher among participants aged 30–44 years and 1.52 times higher among participants aged 45–69 years compared to 15–29 years. The cumulative risks increased with increase in age and educational level. Participants those who resides in urban areas were 1.13 times more likely to have x or more risk factors compared to rural residence.
Table 3 presents prevalence of MetS assessed using ATP III and IDF criteria. The prevalence was higher among participants aged 45 to 69 years, those who do not have formal education, widowed/divorced/separated, belongs to religious minorities, those who resides in hilly region, and among urban dwellers. Likewise, the higher prevalence was also observed among participants who had abnormal waist hip ratio, and were obese [BMI ≥ 30 kg/m2]. The differences in the prevalence of the MetS using ATP III and IDF criteria can be demonstrated by data from the study. Although both the definition identified approximately 16% of the population as having the MetS, there was a large variability and only 10% of individuals met the criteria for both the definitions (Fig. 2).
In adjusted model, age, gender, abnormal waist hip ratio, BMI, ecological zone, place of residence were the significant predictor of MetS by both the criteria (Table 4).
Using IDF criteria, compared to participants aged 15–29 years, the higher odds of occurrence of MetS was observed among participation aged 30–44 years (AOR: 2.07; 95% CI: 1.31–3.25) and 45–69 years (AOR: 4.52; 95% CI: 2.91–7.03). The odds of occurrence of MetS was significantly higher among female (AOR: 1.44; 95% CI: 1.05–1.97) compared to male counterparts. Likewise, participants who had abnormal waist hip ratio had higher likelihood of MetS compared to normal (AOR: 8.18; 95% CI: 5.93–11.29), and the study also revealed that the higher risk of occurrence of MetS among overweight (AOR: 7.82; 95% CI: 5.78–10.78) and obese (AOR: 14.03; 95% CI: 8.71–22.60) compared to those who had <25 kg/m2 BMI. Also, compared to participants who resides in mountains, the higher likelihood of occurrence among the residence who resides in Terai/the plain (AOR: 2.64; 95% CI: 1.14–6.11) and hill (AOR: 2.41; 95% CI: 1.04–5.63). The higher odds of occurrence of MetS was observed among urban dwellers (AOR: 1.56; 95% CI: 1.14–2.13) compared to rural dwellers.
Discussion
This secondary-analysis of the data provided by the nationally represented survey (STEPS Survey), provides the first nationally representative estimates on prevalence, disaggregated by sub-groups, and factors attributed to MetS among adult population of Nepal. The overall prevalence of metabolic syndrome is 15% and 16% according to ATP III and IDF criteria respectively. Based on our findings, the Nepalese population appears to have a relatively lower burden of MetS compared to overall burden of MetS in South Asia (ATPIII 26.1% and IDF 29.8%) reported by a systematic review15. A triad of central obesity, low HDL-C, and elevated BP was the most prevalent (8.2%) combination of CVD risk factors constituting the syndrome in this population. This was followed by a triad of CVD risk factors, namely central obesity, low HDL-C and elevated triglycerides found in 7.8% of the total participants. The most common MetS component was low HDL cholesterol.
In a multivariable analysis, the risk of MetS increased steadily with age: participants aged 45–69 were 7.08 (ATP III) and 4.52 (IDF) times more likely to suffer from MetS than those who were in the age group 15–29 years. Similar findings were also seen with BMI: participants with BMI ≥ 30 kg/m2 were 9.44 (ATP III) and 14.03 (IDF) times more likely to suffer from MetS than those who had BMI < 25 kg/m2. The prevalence of MetS is higher in females compared to males in Nepal. The association with age, sex and BMI were consistent with previous studies from different countries13,16,17. People living in urban areas were twice more likely to develop MetS compared to rural residents. This might be due to sedentary lifestyles, dietary changes and stress in urban people.
The association of MetS with low physical activity was inconsistent with increased odds of 1.48 and decreased odds of 0.93 according to ATP III and IDP criteria respectively. However, some epidemiologic studies and uncontrolled trials have suggested that increased moderate-to-vigorous physical activity reduces the incidence or prevalence of the MetS18,19,20,21. Insufficient fruit and vegetable intake and cigarette smoking increased the odds of developing MetS in this study. Consumption of fruits and vegetables has been found to reduce diastolic blood pressure22 and risk of type II diabetes mellitus23 and may therefore reduce the risk of MetS. Current smoking was not-significantly associated with lower risk of MetS in our study. Existing evidence for association of MetS with cigarette smoking is inconsistent as well24,25,26. In our study, there was inconsistent evidence of association of alcohol intake and MetS with increased risk according to ATP III criteria and reduced risk according to IDP criteria. Various studies have shown that drinking alcohol is harmful at higher doses however, light to moderate doses is beneficial to health and reduces risk of coronary heart disease, diabetes, stroke and total mortality in adults27,28,29. A recent academic paper by international experts recommended lifestyle changes comprising of increased intake of fruits and vegetables, quitting smoking, moderate consumption of alcohol and physical activity to prevent MetS and improve cardio metabolic health30.
South Asians have a propensity towards less lean muscle mass and more visceral fat mass at a lower BMI and waist circumference compared to western population who tend to carry much of their weight in muscle and subcutaneous fat depots peripherally31,32. Thus South Asians with same body mass index are be at higher risk for metabolic syndrome compared to their western counterparts33. Moreover, comorbid diseases, including T2DM, occur at lower waist circumference in Asian adults34. Thus, ATP III might result in low prevalence figures in Nepalese population due to use of non-specific cut-offs for waist circumference. Moreover, waist circumference is used as only optimal component in ATP III. IDF criteria with waist circumference thresholds specific to Asian population (men 90 cm and women 80 cm) might be therefore more suitable for estimation of metabolic syndrome among adult Nepalese population.
Much of the health care priorities to date in low and middle income countries, including Nepal has been catering to infectious diseases and maternal and child health. A high burden of MetS as we demonstrated in our study and confirmed by other small studies from non-specialist hospital setting necessitates acknowledging the importance of reducing NCD risk factors at population level. The primary goal should be creating environment that facilitates greater physical activity and awareness regarding healthy dietary choices. In addition, the health systems need to be strengthened to reach the populations that are at risk for NCDs. Additionally, alternate models for service delivery and health promotion should be considered to reach unprivileged population with limited access to health care services. These may include mobilization of community health volunteers and mass media campaigns aimed at changing risky lifestyle behaviors.
Nationally, representative data are limited in Nepal and prevalence figures in the earlier studies were estimated using non-comparable sampling design in a section of population. This study is based on a large national sample consisting of both urban and rural populations in Nepal. However, as in any cross-sectional study, we could not establish causality between metabolic syndrome and its determinants. The South Asian population have been shown to be genetically susceptible to central obesity and insulin resistance35. However, the absence of genetic studies in Nepal have limited our understanding of the role of genetic factors in the pathogenesis of metabolic syndrome among Nepalese adults. The STEPS survey did not include information on household wealth or monthly income of participants hence an important determinant of metabolic syndrome could not be assessed among Nepalese population in this study.
Conclusion
Our study demonstrates a high burden of MetS in Nepalese adults with ten percentage increment in prevalence across each age groups fifteen years apart. The prevalence peaked among those aged 45–69 years such as three in ten in this age-group had MetS. A substantial clustering of risk factors was evident with 80.7% having at least one risk factor. A triad of low HDL-C, abdominal obesity and high BP was the most prevalent (8.18%), followed by abdominal obesity, low HDL-C cholesterol and high triglycerides (8%). Female gender, urban, hill or terai resident were particularly at risk.
Methods
Study design and sampling technique
This is a secondary analysis carried out using Non-Communicable Diseases risk factors 2013 data. The detail methodology and report of the survey has been presented elsewhere36. In brief, the survey was a cross sectional study, carried out from January to June 2013, with aim to assesses the risk factors of NCDs at entire population level.
Firstly, out of the 921 Ilakas (an administrative unit at the sub-district level) in Nepal, 70 were selected, which were proportionately distributed across Nepal’s three ecological zones (Mountain, Hill and Terai/Plains) using probability proportionate to population size (PPS) which served as a primary sampling unit (PSU) of the study. Secondly, three clusters, the wards (the smallest administrative units) were selected from each of the PSU using the PPS. A total of 210 clusters were selected served as secondary sampling unit of this study. Subsequently, using systematic sampling, twenty households per cluster were selected. Using Kish method, one participant in each household were selected from the eligible frame (15–69 years). A sample size of 4,200 was used to represent the adult target population aged 15–69 years in Nepal. In order to calculate the required sample size the prevalence of low fruit and vegetable consumption was considered 61.9%, absolute margin of error ±5%, design effect 1.5, response rate 80% and six domains (three age categories and two genders) were considered to obtain nationally representative sample. A detail algorithms of sample size calculation have presented elsewhere36.
Survey implementation
A total of 26 researchers divided into 2 teams were assigned for data collection. Each team was composed of field supervisor, medical laboratory technologist, laboratory technician one each, and ten enumerators having nursing, public health or paramedics background. Their major responsibility was to fill out the questionnaires, carry out physical measurements and collect blood samples. The laboratory technicians were assigned for cold chain maintenance, sample processing, and the recording and reporting of biochemical measurements carried out using wet methods. Medical laboratory technologists were responsible for examining and verifying glucose levels and the value of the lipid profile including sending a 10% blood sample to the reference laboratory for external quality control.
A week-long training was organised in the two weeks prior to the beginning of data collection. The training was led by a STEPS team from WHO headquarters, Geneva and WHO SEARO, New Delhi. The local investigator team also joined the STEPS team as trainers. Prior to the training, the data collection team were oriented on the tools to be used to collect the data. Training focused on interview techniques, sampling process, household and individual selection, the use of the different kinds of templates and forms in the survey, the use and care of PDAs, a detailed explanation of the questionnaire and the technique to be used for physical measurements. The supervisors were also trained on downloading data from the PDAs as well as the troubleshooting of minor issues with the PDAs.
Overall, field operation and quality control was responsibility of field supervisor including coordinate with respective authorities at the field level, ensure completion of sampling frames, and select 20 households from each cluster. Also, the field supervisors were responsible for aggregating the data from individual PDAs to their laptop and forwarding them to the centre via email or by handing them over to the investigators.
Definition of variables
The dependent variable in this analysis was occurrence of metabolic syndrome. The indicators analysed in this study are defined in Table 5. Two major predictor variables were included: individual characteristics: age in years (15–29, 30–44 and 45–69), gender (male and female), education (no formal schooling, primary, secondary and higher level), marital status (never married, currently married and divorced/widowed/separated) and caste/ethnicity, and community characteristics: ecological zone (mountain, hill and terai/plains) and place of residence (urban and rural) in this analysis.
Data processing and analysis
In order to obtain nationally representative estimates, the sampling weights were used. Chi-square statistics was used to assess the difference in risk factors by gender. To reflect clustering within individuals, we considered the number of risk factors that each participant had at the time of the survey (from 0 to 5) and examined the mean number and 95%CIs of risk factors by covariates. We examined the independent effects of covariates on risk factor clustering within individuals by modeling a multivariate Poisson regression model, with the number of risk factors as the dependent variable. All the analysis carried out was using complex survey design; wards were considered as cluster and ecological zones as strata.
Univariate and multivariate logistic regression were used to test associations between predictors and outcome variables using Stata SE 14. Adjusted odd ratio (AOR) was calculated using multiple logistic regression, with all predictors (age, gender, education, marital status, ecological zone and place of residence) included simultaneously in the model in order to assess the predictors of MetS. A p-value < 0.05 was considered as statistically significant.
Ethical Considerations
This study was approved by the ethical review board of the Nepal Health Research Council. An informed written consent was obtained from all the participants. For the participants under the age of 18 years, informed consent from parent/legal guardian was obtained. Waste generated during the laboratory procedures was properly disinfected using aseptic techniques and safely disposed as per protocol. Blood samples were discarded after the biochemical measurements.
References
Alberti, K. G. et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120, 1640–1645 (2009).
Grundy, S. M. Metabolic syndrome pandemic. Arterioscler Thromb Vasc Biol 28, 629–636 (2008).
Wilson, P. W., D’Agostino, R. B., Parise, H., Sullivan, L. & Meigs, J. B. Metabolic syndrome as a precursor of cardiovascular disease and type 2 diabetes mellitus. Circulation 112, 3066–3072 (2005).
Ford, E. S., Giles, W. H. & Dietz, W. H. Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. JAMA 287, 356–359 (2002).
Further Study Of Risk Factors For, S. & Coronary Heart Disease, g. The prevalence of metabolic syndrome in a 11 provinces cohort in China. Zhonghua Yu Fang Yi Xue Za Zhi 36, 298–300 (2002).
Misra, A. & Khurana, L. Obesity and the metabolic syndrome in developing countries. J Clin Endocrinol Metab 93, S9–30 (2008).
Alberti, K. G., Zimmet, P., Shaw, J. & Group, I. D. F. E. T. F. C. The metabolic syndrome–a new worldwide definition. Lancet 366, 1059–1062 (2005).
Misra, A. & Bhardwaj, S. Obesity and the metabolic syndrome in developing countries: focus on South Asians. Nestle Nutr Inst Workshop Ser 78, 133–140 (2014).
World Bank. Non-communicable disease in Nepal-Nepal’s next major health challenge In: NCDs Policy Brief-Nepal. Washington DC, USA: World Bank. (2011. Available at, http://siteresources.worldbank.org/SOUTHASIAEXT/Resources/223546-1296680097256/7707437-1296680114157/NCD_NP_Policy_Feb_2011.pdf. (Accessed 09 March 2018)).
Bhandari, G. P., Angdembe, M. R., Dhimal, M., Neupane, S. & Bhusal, C. State of non-communicable diseases in Nepal. BMC Public Health 14, 23 (2014).
Vaidya, A. Tackling cardiovascular health and disease in Nepal: epidemiology, strategies and implementation. Heart Asia 3, 87–91 (2011).
Sharma, S. K. et al. Prevalence of hypertension, obesity, diabetes, and metabolic syndrome in Nepal. Int J Hypertens 2011, 821971 (2011).
Chowdhury, M. Z. I. et al. Prevalence of metabolic syndrome in Bangladesh: a systematic review and meta-analysis of the studies. BMC Public Health 18, 308 (2018).
Pandit, K., Goswami, S., Ghosh, S., Mukhopadhyay, P. & Chowdhury, S. Metabolic syndrome in South Asians. Indian J Endocrinol Metab 16, 44–55 (2012).
Aryal, N. & Wasti, S. P. The prevalence of metabolic syndrome in South Asia: a systematic review. International Journal of Diabetes in Developing Countries 36, 255–262 (2016).
Yousefzadeh, G. & Sheikhvatan, M. Age and gender differences in the clustering of metabolic syndrome combinations: A prospective cohort research from the Kerman Coronary Artery Disease Risk Study (KERCADRS). Diabetes Metab Syndr 9, 337–342 (2015).
Zhao, Y. et al. Prevalence and determinants of metabolic syndrome among adults in a rural area of Northwest China. PLoS One 9, e91578 (2014).
Chu, A. H. & Moy, F. M. Association between physical activity and metabolic syndrome among Malay adults in a developing country, Malaysia. J Sci Med Sport 17, 195–200 (2014).
Kim, J., Tanabe, K., Yokoyama, N., Zempo, H. & Kuno, S. Association between physical activity and metabolic syndrome in middle-aged Japanese: a cross-sectional study. BMC Public Health 11, 624 (2011).
Lakka, T. A. & Laaksonen, D. E. Physical activity in prevention and treatment of the metabolic syndrome. Appl Physiol Nutr Metab 32, 76–88 (2007).
Salonen, M. K. et al. Physical activity, body composition and metabolic syndrome in young adults. PLoS One 10, e0126737 (2015).
Shin, J. Y., Kim, J. Y., Kang, H. T., Han, K. H. & Shim, J. Y. Effect of fruits and vegetables on metabolic syndrome: a systematic review and meta-analysis of randomized controlled trials. Int J Food Sci Nutr 66, 416–425 (2015).
Li, M., Fan, Y., Zhang, X., Hou, W. & Tang, Z. Fruit and vegetable intake and risk of type 2 diabetes mellitus: meta-analysis of prospective cohort studies. BMJ Open 4, e005497 (2014).
Katano, S. et al. Relationship among physical activity, smoking, drinking and clustering of the metabolic syndrome diagnostic components. J Atheroscler Thromb 17, 644–650 (2010).
Oh, S. W. et al. Association between cigarette smoking and metabolic syndrome: the Korea National Health and Nutrition Examination Survey. Diabetes Care 28, 2064–2066 (2005).
Onat, A. et al. Prospective epidemiologic evidence of a “protective” effect of smoking on metabolic syndrome and diabetes among Turkish women–without associated overall health benefit. Atherosclerosis 193, 380–388 (2007).
Ronksley, P. E., Brien, S. E., Turner, B. J., Mukamal, K. J. & Ghali, W. A. Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ 342, d671 (2011).
Howard, A. A., Arnsten, J. H. & Gourevitch, M. N. Effect of alcohol consumption on diabetes mellitus: a systematic review. Ann Intern Med 140, 211–219 (2004).
Friedman, L. A. & Kimball, A. W. Coronary heart disease mortality and alcohol consumption in Framingham. Am J Epidemiol 124, 481–489 (1986).
Perez-Martinez, P. et al. Lifestyle recommendations for the prevention and management of metabolic syndrome: an international panel recommendation. Nutr Rev 75, 307–326 (2017).
Bajaj, H. S. et al. Comparison of relative waist circumference between Asian Indian and US adults. J Obes 461956 (2014).
Cameron, A. J. et al. Cut-points for waist circumference in Europids and South Asians. Obesity (Silver Spring) 18, 2039–2046 (2010).
Katzmarzyk, P. T., Janssen, I., Ross, R., Church, T. S. & Blair, S. N. The Importance of Waist Circumference in the Definition of Metabolic Syndrome. Prospective analyses of mortality in men 29, 404–409 (2006).
Tan, C. E., Ma, S., Wai, D., Chew, S. K. & Tai, E. S. Can we apply the National Cholesterol Education Program Adult Treatment Panel definition of the metabolic syndrome to Asians? Diabetes Care 27, 1182–86 (2004).
Shen, H. et al. Uncoupling protein 2 promoter polymorphism−866G/A, central adiposity, and metabolic syndrome in Asians. Obesity 14, 656–61 (2006).
Aryal, K. K. et al. Communicable Diseases Risk Factors: STEPS Survey Nepal 2013. (Nepal Health Research Council, Kathmandu, 2014).
World Health Organization. The WHO STEPwise approach to noncommunicable disease risk factor surveillance. STEPs Surveillance manual. (last updated 2017. available from, http://www.who.int/ncds/surveillance/steps/manual/en/).
Huang, P. L. A comprehensive definition for metabolic syndrome. Dis Model Mech 2, 231–237 (2009).
World Health Organization. Non communicable disease and their risk factors. Global Physical Activity Surveillance. Available from, http://www.who.int/ncds/surveillance/steps/GPAQ/en/. (accessed on 1/4/2018).
World Health Organization. Global recommendations on physical activity for health. (2010. Available from, http://www.who.int/dietphysicalactivity/publications/9789241599979/en/).
World Health Organization. The STEPS Instrument and Support Materials. Available from, http://www.who.int/ncds/surveillance/steps/instrument/en/. (accessed on 1/4/2018).
Omech, B. et al. Prevalence and determinants of metabolic syndrome: a cross-sectional survey of general medical outpatient clinics using National Cholesterol Education Program-Adult Treatment Panel III criteria in Botswana. Diabetes Metab Syndr Obes 9, 273–279 (2016).
Acknowledgements
The data used in this study were obtained from NHRC the open access dataset of STEPS 2013. The opinions expressed in this article are those of the authors and do not necessarily reflect the views of the organisations they are affiliated to.
Author information
Authors and Affiliations
Contributions
S.M., S.R.M., N.S., R.K.M., B.B. and A.R.P. had the concept of the paper. N.S., R.K.M., S.R.M. and S.M. conducted literature review, carried out the data analysis and prepared the first draft. S.R.M., N.S., S.M., B.B. and A.R.P. suggested on the methodology and reviewed the manuscript. All authors read and agreed on the final version of paper.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mehata, S., Shrestha, N., Mehta, R.K. et al. Prevalence of the Metabolic Syndrome and its determinants among Nepalese adults: Findings from a nationally representative cross-sectional study. Sci Rep 8, 14995 (2018). https://doi.org/10.1038/s41598-018-33177-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-33177-5
Keywords
This article is cited by
-
Prevalence of metabolic syndrome among breast cancer survivors in East Coast of Peninsular Malaysia
BMC Public Health (2021)
-
Prevalence and associated factors of metabolic syndrome among a national population-based sample of 18–108-year-olds in Iraq: results of the 2015 STEPS survey
International Journal of Diabetes in Developing Countries (2021)
-
Cardiometabolic risk factors among patients with tuberculosis attending tuberculosis treatment centers in Nepal
BMC Public Health (2020)
-
Burden of Diabetes and Prediabetes in Nepal: A Systematic Review and Meta-Analysis
Diabetes Therapy (2020)
-
Prevalence, patterns, and correlates of physical activity in Nepal: findings from a nationally representative study using the Global Physical Activity Questionnaire (GPAQ)
BMC Public Health (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.