Abstract
Bioprosthetic valves for tricuspid valve replacement (TVR) have become increasingly popular in recent years, but mechanical valves remain valuable, particularly for the patients who want to avoid reoperation for bioprostheses malfunction. The aim of this study was to review our 10-year experience in adult patients who underwent TVR with the St. Jude Medical (SJM) valve. From 2005 to 2015, 265 TVRs with SJM valves were performed at our institution. The mean age at operation was 44.1 ± 9.7 years, and 207 cases (78.1%) were female. The mean follow-up was 4.9 ± 2.7 years. Preoperative atrial fibrillation was present in 199 cases (75.1%) and ascites in 26 (9.8%). Of all cases, 88.7% were characterized as New York Heart Association class III or IV. The hospital mortality was 6.4%. There were 9 deaths (3.8%) during late follow-up. The overall survival rates were 89.2% ± 2.2% at 5 years and 86.6% ± 2.9% at 10 years. The linearized rates of valve thrombosis and bleeding events were 0.8%/patient-year and 1.5%/patient-year, respectively. Three cases (1.3%) were reoperated due to prosthetic valve thrombosis. There was no reoperation for sperivalvular leakage and structural failure. The freedom from reoperation was 98.6% ± 0.8% at 5 years and 98.6% ± 0.8% at 10 years. The SJM valve in the tricuspid position is a reliable mechanical prosthesis with a low rate of valve thrombosis and reoperation. It is a reasonable choice for the patients who require mechanical valve replacement in the tricuspid position.
Similar content being viewed by others
Introduction
In recent years, an increasing number of patients undergoing tricuspid valve replacement (TVR) have received bioprostheses due to the great durability in the tricuspid position and to the advantage of freeing patients from anticoagulant medication1,2,3. However, bioprostheses inevitably calcify and stenose, which may cause valve dysfunction. Therefore, the mechanical valve remains valuable in TVR, particularly for the patients who refuse to take on the risk of reoperation for bioprostheses malfunction.
The St. Jude Medical (SJM) valve (St. Jude Medical, Inc., St. Paul, MN), a low-profile bileaflet mechanical valve constructed of pyrolytic carbon, has been widely used in patients4. It is characterized by favorable hemodynamic properties, and a low incidence of thromboembolism5. As a result of excellent durability, it is preferred in young patients. Although its good clinical performances in the mitral and aortic positions have been reported4,6, assessment for follow-up results in the tricuspid position is limited. With this background, we reviewed our 10-year experience of 265 TVRs with SJM valves at our institution.
Results
Early results
Preoperative and intraoperative characteristics of the study patients are presented in Table 1. The mean age at operation was 44.1 ± 9.7 years (range, 19 to 68 years), and 207 cases (78.1%) were female. The etiology of tricuspid valve disease was as follows: rheumatic in 227 cases (85.7%), congenital in 22 (8.3%), degenerative in 7 (2.6%), endocarditis in 3 (1.1%), prosthetic dysfunction in 3 (1.1%), and traumatic in 3 (1.1%).
Compared with the none-mild pulmonary hypertension (PHT) group, the moderate-severe PHT group exhibited a greater prevalence of rheumatic valve disease (p < 0.001), larger preoperative left atrial diameter (LAD, p = 0.001) and lower preoperative left ventricular ejection fraction (LVEF, p = 0.026). More patients in the moderate-severe PHT group received TVR concomitantly with other procedures (p < 0.001) and required a longer extracorporeal circulation time (ECC, p = 0.001). However, the proportion of patients with a history of cardiac operation in the none-mild PHT group was significantly higher than the moderate-severe PHT group (p < 0.001).
The early postoperative results are presented in Table 2. The hospital mortality for patients undergoing TVR was 6.4%. The causes of early deaths were cardiac failure in 10 patients, multi-organ failure as a result of pulmonary infection in 4, arrhythmia (ventricular fibrillation and ventricular tachycardia) in 2, and acute renal failure in 1. The difference of hospital mortality between the none-mild PHT group (4.1%) and the moderate-severe PHT group (9.2%) was not statistically significant (p = 0.090).
There were 61 cases of early complications, including 22 low cardiac output syndrome, 17 respiratory infection, 10 re-exploration for excessive postoperative bleeding, 6 permanent pacemaker implant for atrioventricuiar block, 2 acute renal failure, 2 cerebral infarction, and 2 arrhythmia. These complications occurred in 24 TVRs (16.4%) of the none-mild PHT group and 30 (25.2%) of the moderate-severe PHT group, and the difference was not statistically significant (p = 0.078).
Thirty-nine cases (14.7%) experienced prolonged postoperative ventilator support for more than 72 hours. Multivariate logistic analysis showed that the age (p = 0.027), presence of ascites (p = 0.025), extended ECC time (p = 0.005) and low LVEF (p = 0.027) were the independent predictors of prolonged ventilator support (Table 3).
Ten years survival
Of the 235 survivors, 9 deaths occurred during follow-up, yielding a late mortality rate of 3.8%. The causes of late deaths were heart failure in 3 patients, cerebral hemorrhage in 1, and prosthetic valve endocarditis in 1. However, the specific causes had not been confirmed in the remaining 4 deaths and autopsy was not conducted. For the patients with a medical history of heart failure and peripheral edema, the cause of these deaths was considered to be heart failure. Overall survival rates were 89.2% ± 2.2% at 5 years and 86.6% ± 2.9% at 10 years (Fig. 1).
There were 4 late deaths (3.0%) in the none-mild PHT group and 5 (5.0%) in the moderate-severe PHT group. The 5 years and 10 years survival rates were 93.7 ± 2.2% and 89.0 ± 4.0% for the none-mild PHT group, and 83.7% ± 3.9% and 83.7% ± 3.9% for the moderate-severe PHT group, respectively. Although the survival rates in the none-mild PHT group were higher than the moderate-severe PHT group, the difference was not statistically significant (p = 0.055, Fig. 2).
Valve thrombosis
During follow-up, valveN thrombosis occurred in 9 cases (3.8%). Of them, 7 cases were associated with an irregular use of warfarin and unreasonable prolonging the intervals of international normalized ratio (INR) monitoring (more than 3 months). The other 2 cases were confirmed to have adequate anticoagulation with a therapeutic INR.
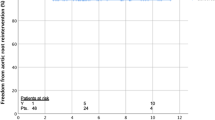
Valve replacement was successfully performed in 3 cases. As no overt symptoms related to the tricuspid valve thrombosis were observed in the remaining 6 cases, they accepted conservative management which increased the target range of INR to 2.5–3.0. Echocardiographic monitoring showed complete resolution of the thrombus within 6 months follow-up and normally functioning mechanical leaflets in 2 cases. Freedom from valve thrombosis was 96.0% ± 1.4% at 5 years and 94.1% ± 2.3% at 10 years (Fig. 3). The linearized rate of valve thrombosis was 0.8%/patient-year.
Bleeding events
Bleeding events that required inpatient management or transfusion was occurred in 17 cases (7.2%). Among them, 6 cases were gastrointestinal bleeding, 3 were cerebral bleeding (1 fatal), 3 were hematuria, 2 were leg hematomas, 2 were massive epistaxis, and 1 was retinal hemorrhage. Freedom from bleeding events was 91.8% ± 2.2% at 5 years and 87.5% ± 3.2% at 10 years (Fig. 4). The linearized rate of bleeding events was 1.5%/patient-year.
Reoperation
Reoperation was performed for 3 cases (1.3%) due to prosthetic valve thrombosis. A new SJM valve was re-implanted in 1 case, and bioprostheses were implanted in the other 2. All of them survived at the end of follow-up. The intervals to reoperation were 2 months, 4 months, and 2.8 years, respectively. Freedom from reoperation was 98.6% ± 0.8% at 5 years and 98.6% ± 0.8% at 10 years. The linearized rate of reoperation was 0.3%/patient-year. Another case of perivalvular leakage was detected after follow-up of 6.5 years, but it was unnecessary to undergo reoperation. In addition, no case of structural failure was observed.
Discussion
TVR is uncommon in clinical practice and is reserved for few cases in which repair of the tricuspid valve is not feasible or efforts to repair it have failed7. A high hospital mortality rate associated with TVR was reported universally in previous studies, ranging from 10.0% to 27.6%8,9,10. The present result of 6.4% is relatively favorable compared with them. However, it is still higher than researches on mitral or aortic valve replacement4,6.
The reasons for such a favorable hospital mortality are varied and could be summarized as follows. First, a younger patient population is an important factor, as age was identified to be a strong predictor of hospital mortality4,11,12. The average age of our patients was 44.1 ± 9.7 years, while other studies were commonly more than 50 or even 60 years9,11,12,13,14. Second, recent advances in myocardial protection, surgical techniques and perioperative management may have had a positive effect2,15. Third, a low proportion of patients (13.6%) received previous open heart operations in this study16. Re-entry is technically challenging and is associated with a high risk of catastrophic hemorrhage and death.
Like other studies, the main cause of hospital mortality in this study was heart failure. Tricuspid valve disease is primarily asymptomatic and can be tolerated for a long period. Patients often arrive for surgery with a long history of heart disease. However, when the symptoms of right ventricular malfunction, such as peripheral edema and ascites, are manifested, the clinical condition of these patients is already into a rapidly-deteriorated stage16,17. We observed that the presence of ascites and low LVEF were independent predictors for more than 72 hours of ventilator support. Topilsky and colleagues8 reported the early results of 189 patients who had received TVR for severe tricuspid regurgitation, and they indicated that an acceptable hospital mortality can derive from a surgical correction before the onset of advanced heart failure symptoms. In recent years, our attitude toward the surgical correction of tricuspid valve disease tend to be more aggressive than ever in an aim to prevent or at least retard the progress of heart failure. Therefore, the lower hospital mortality found in this study is also related to the earlier intervention for tricuspid valve disease.
The survival rate at 10 years in this study was 86.6% ± 2.9%, which is higher than that reported in other series, ranging from 59.9% to 84.3%10,16,18. Consistent with previously published studies8,11, we found that the main cause of late death was progressive heart failure and only 2 deaths occurred as a result of valve-related complications. Some authors5,16,19 have indicated that patient-related characteristics, such as heart failure and the presence of ascites, were independent predictors of long-term mortality, and the type of implanted prosthesis (mechanical valve and bioprosthesis) in the tricuspid position did not affect the early and long-term results.
Garatti and colleagues12 reviewed 90 patients who underwent TVR with a mechanical valve or a bioprosthesis during 25 years of follow-up. Nine of 13 late deaths were associated with heart failure and only 1 patient died from cerebral hemorrhage. The late deaths were dominantly dependent from non-valve-related events. Chang and colleagues16 revealed a similar long-term mortality of bioprosthetic and mechanical valves, and indicated that the progression of heart failure is the most frequent cause of late death. These data demonstrate that late deaths are more attributed to patient-related characteristics than valve-related factors by the implanted prosthesis in the tricuspid position. Although the literatures have demonstrated the elevated pulmonary hypertension was an independent predictor for pathetic long-term outcomes12,20, not so in this study. The reason might be due to a higher previous open heart surgery rate in the none-mild PHT group than moderate-severe PHT group.
Valve thrombosis is considered the Achilles’ heel of mechanical valves in the tricuspid position. Its linearized rate ranges from 0.5% to 6.8%/patient-year according to other studies16,18,21,22,23,24. The present result of 0.8%/patient-year is comparable with or even lower than these reports. A higher prevalence of valve thrombosis in caged ball and tilting disc prostheses has been generally mentioned21.
The SJM valve was introduced as an alternative to last-generation mechanical valves with preeminent hemodynamics and low incidence of thromboembolism4,5. In the case of valve dysfunction for thrombosis, the bileaflet SJM valve may present hemodynamic advantages over the caged ball and tilting disc prostheses: one of the leaflets may still partially open and close to avoid catastrophic outcomes25. Nakano and colleagues23 observed that valve thrombosis occurred in only 1 out of 39 patients with the SJM valve in the tricuspid position over a 13.8-year follow-up. The result from Singh and colleagues25 is more promising because there was no thrombosis in 14 patients with 7 to 10 years of follow-up. However, in a retrospective study by Kawano and his colleagues24, 6 of 19 SJM valves after TVR were detected with valve thrombosis (2.9%/patient-years), and they emphasized that thrombosis was more likely to occur in valves of the tricuspid position. In our view, the higher thrombogenicity of the SJM valve may have been caused by the setting of a lower target INR (1.5–2.0). The irregular use of warfarin and the unreasonable prolonging of the intervals of INR monitoring were the major causes of valve thrombosis in this study. Therefore, the strict control of the anticoagulation intensity and the regular education of patients are important to avoid thrombotic complications12,16.
Bleeding was the main valve-related complication in this study. The present linearized rate of bleeding events was 1.5%/patient-year, which is higher than a previous series with SJM in other valve positions (0.3–1.0%/patient-year)6,26. However, it seems to be a satisfactory result when compared with other mechanical valves in tricuspid valve position13,27. In China, after mechanical aortic valve replacement (AVR) and/or mitral valve replacement (MVR), low-intensity anticoagulation with a target INR less than 2.5 (AVR: 1.3–1.8; MVR: 1.8–2.3; AVR and MVR: 1.8–2.3) is recommended for decreasing the risk of bleeding28. Given the higher incidence of valve thrombosis in the tricuspid position, moderate-intensity anticoagulation (INR 2.0–3.0) is recommended in our hospital for patients who received TVR with a mechanical valve. The results of this study indicated that for Chinese TVR recipients, the target INR of 2.0–3.0 was concomitant with a low incidence of valve thrombosis and an acceptable occurrence of bleeding events, but further evaluations are required to confirm these findings.
Long-term durability is one of the creditable characteristics of the SJM valves. Structural failure due to the disruption of components of the prosthetic valve was not observed in this study or in other relevant studies23,24,25. In this study, 98.6% ± 0.8% of SJM valves were free from reoperation at 10 years. All reoperations were identified for valve thrombosis, rather than structural failure and perivalvular leakage. Similar to that of other studies23,25, excellent durability of the SJM valves was demonstrated in this study.
Several studies have reported better durability of bioprostheses in a low-pressure chamber of the tricuspid position than in the aortic and mitral position9,15. However, the deficiencies for bioprostheses are late valve calcification, stenosis, and dysfunction. Nakano and colleagues18 detected the subclinical prosthetic dysfunction of bioprosthetic valves in 35% of patients who were followed up for more than 5 years after TVR. Chang and colleagues16 compared the long-term outcomes between two types of valves. Freedom from reoperation for mechanical valves at 15 years was 86.0% ± 6.2%, while that of bioprosthetic valves was only 55.1% ± 13.8%. The reoperation of TVR would bring about a high operative risk and hospital expense. As the patients in this study were characterized by a younger age and a lower income distribution, they refuse to take on the risk of reoperation for bioprostheses malfunction. Therefore, they more preferable to mechanical valves at present.
In recent years, advances in the transcatheter valve-in-valve (VIV) technology is forcing more and more surgeons to implant bioprostheses, even in young patients. It is an attractive alternatives to redo conventional open heart surgery. However, most of the available studies are mainly focus on the treatment of dysfunctional aortic bioprostheses29. In our opinion, more experiences in transcatheter tricuspid VIV and longer follow-up are needed before the expansion of bioprosthesis used in tricuspid position30. The technology of transcatheter tricuspid VIV may open a new clinical prospect in the near future for patients.
Study limitations
There are also limitations in this study that must be realized. First, it was a retrospective observational study performed in a single institution. However, to our knowledge, it is the largest number of patients undergoing TVR with SJM valve to be studied. Second, 85.7% of patients had concomitant MVR and/or AVR, early complications such as low cardiac output syndrome, respiratory infection, reoperation for bleeding might not have been directly related to mechanical TVR, rather may be due to valve replacement in either aortic or mitral valves. Third, for an average duration of 4.9 ± 2.7 years of this study, the long-term results still need to be further followed up.
Conclusion
This study demonstrates the excellent mid-term results of SJM valve in the tricuspid position. The incidences of valve thrombosis and reoperation were low, and deaths were more attributed to the patient-related characteristics rather than valve-related complications. Therefore, the SJM valve is a reasonable choice for the patients who require mechanical valve replacement in the tricuspid position.
Materials and Methods
Patients
From January 2005 to December 2015, 10202 cardiac valve replacements were performed in West China Hospital, Sichuan University. Of these operations, 5574 (54.6%) were MVR, 2666 (26.1%) were MVR and AVR, 1630 (16.0%) were AVR, and 332 (3.3%) were TVR either as an isolated procedure or combined with surgery on other valves. After patients with bioprostheses (42 cases), non-SJM mechanical valves (GK valve in 11 cases and CarboMedics valve in 9) and younger than 18 years old (5 cases) were excluded, 265 cases of TVR with SJM valves were performed in 264 adult patients (see Supplementary Fig. 1). During the same period, there were 3658 cases of tricuspid valve repair in our hospital, and the ratio of replacement to repair was 1:11.
Surgical techniques
In our hospital, the first choice for patients with tricuspid valve disease is repair, and the replacement should only be considered as the last resort. A total of 261 (98.5%) TVRs were performed under cardiac arrest through median sternotomy in a conventional manner. The remaining 4 reoperative cases (1.5%) were performed while the heart was beating, and a right anterolateral thoracotomy was used to avoid retrosternal adhesions. Cardiopulmonary bypass and mild-moderate systemic hypothermia were initiated for all cases during the operations. The SJM valves were implanted with interrupted sutures. They were also used in other valve replacements, which were performed concomitantly with TVR. The prosthetic valve sizes of the SJM valves in TVR and MVR are shown in Fig. 5. Postoperative anticoagulation with warfarin was administered for all patients with the INR ranging from 2.0 to 3.0. Our anticoagulant management was monitored every month, but every 2–3 months for patients whose INR was consistently within the target range over 3 months.
None-mild PHT vs. moderate-severe PHT groups
The preoperative PHT was calculated through Doppler echocardiography by adding the systolic pressure gradient between the right ventricle and atrium to the right atrial pressure31. The patients were divided into the none-mild PHT (≤50 mm Hg) group and the moderate-severe PHT (>50 mm Hg) group according to the preoperative PHT condition. Both the preoperative and intraoperative data of the two groups are shown in Table 1.
Follow-up
Clinical follow-up was accomplished by a review of the medical records or telephone interviews with the patients themselves or their family members. The follow-up rate was 95.1% (252 of 265 cases), with an average duration of 4.9 ± 2.7 years ranging from 0 to 10.6 years. The cumulative follow-up was 1141.4 patient-years. Operative mortality was to be reported as all-cause mortality within 30 days of TVR or during the time of hospitalization32. The events that occurred within this time were defined as early complication. Valve-related complications associated with the prosthetic valve in the tricuspid position, including valve thrombosis, bleeding events, prosthetic valve endocarditis, and perivalvular leakage, were included in the data analysis2,32
Statistical analysis
Continuous variables were described as mean ± standard deviation (SD) and were analyzed with the Student’s t-test. Categorical data were reported as rates and were analyzed with the Chi-squared test. Independent predictors for ventilator support time more than 72 hours were evaluated with a logistic regression model. Variables with p value < 0.20 in univariate analysis were incorporated into multivariate analysis. The rates of overall survival, freedom from valve-related complications and reoperations were estimated with the Kaplan-Meier method respectively, and the log-rank test was used for intergroup comparison. The incidences of valve-related complications were reported as linearized rates. A two-sided p < 0.05 was regarded as statistically significant. All data were analyzed with Statistical Package for Social Sciences (SPSS V17.0, Chicago, Illinois, USA).
Ethics statement
This study followed the tenets of Declaration of Helsinki and was approved by the ethics review board of West China Hospital, Sichuan University. A waiver of consent was received from them at the same time.
Data Availability
The authors declare that all the data in this manuscript are available.
References
Vassileva, C. M., Shabosky, J., Boley, T., Markwell, S. & Hazelrigg, S. Tricuspid valve surgery: the past 10 years from the Nationwide Inpatient Sample (NIS) database. J Thorac Cardiovasc Surg. 143, (1043–1049 (2012).
Anselmi, A. et al. Appraisal of Long-Term Outcomes of Tricuspid Valve Replacement in the Current Perspective. Ann Thorac Surg. 101, 863–871 (2016).
Said, S. M. et al. When should a mechanical tricuspid valve replacement be considered? J Thorac Cardiovasc Surg. 148, 603–608 (2013).
Toole, J. M. et al. Twenty-five year experience with the St. Jude medical mechanical valve prosthesis. Ann Thorac Surg. 89, 1402–1409 (2010).
Kaplan, M., Kut, M. S., Demirtas, M. M., Cimen, S. & Ozler, A. Prosthetic replacement of tricuspid valve: bioprosthetic or mechanical. Ann Thorac Surg. 73, 467–73 (2002).
Minakata, K. et al. Twenty-year outcome of aortic valve replacement with St. Jude Medical mechanical valves in Japanese patients. Circ J. 79, 2380–2388 (2015).
Zhu, X., Li, Q. & Wu, Z. Long-Term Outcomes of Tricuspid Valve Replacement. Ann Thorac Surg. 102, 2134 (2016).
Topilsky, Y. et al. Preoperative factors associated with adverse outcome after tricuspid valve replacement. Circulation. 123, 1929–1939 (2011).
Carrier, M. et al. Tricuspid valve replacement: an analysis of 25 years of experience at a single center. Ann Thorac Surg. 75, 47–50 (2003).
Ratnatunga, C. P., Edwards, M. B., Dore, C. J. & Taylor, K. M. Tricuspid valve replacement: UK Heart Valve Registry mid-term results comparing mechanical and biological prostheses. Ann Thorac Surg 66, 1940–1947 (1998).
Filsoufi, F. et al. Long-term outcomes of tricuspid valve replacement in the current era. Ann Thorac Surg. 80, 845–850 (2005).
Garatti, A. et al. Twenty-five year outcomes of tricuspid valve replacement comparing mechanical and biologic prostheses. Ann Thorac Surg. 93, 1146–1153 (2012).
Mangoni, A. A., DiSalvo, T. G., Vlahakes, G. J., Polanczyk, C. A. & Fifer, M. A. Outcome following isolated tricuspid valve replacement. Eur J Cardiothorac Surg. 19, 68–73 (2001).
Alqahtani, F. et al. Contemporary trends in the use and outcomes of surgical treatment of tricuspid regurgitation. J Am Heart Assoc. 6, e007597 (2017).
Sung, K. et al. Is tricuspid valve replacement a catastrophic operation? Eur J Cardiothorac Surg. 36, 825–829 (2009).
Chang, B. C. et al. Long-term clinical results of tricuspid valve replacement. Ann Thorac Surg. 81, 1317–1324 (2006).
Buzzatti, N. et al. Long-term outcomes of tricuspid valve replacement after previous left-side heart surgery. Eur J Cardiothorac Surg. 46, 713–719 (2014).
Nakano, K., Ishibashi-Ueda, H., Kobayashi, J., Sasako, Y. & Yagihara, T. Tricuspid valve replacement with bioprostheses: long-term results and causes of valve dysfunction. Ann Thorac Surg 71, 105–109 (2001).
Glower, D. D. et al. In-hospital and long-term outcome after porcine tricuspid valve replacement. J Thorac Cardiovasc Surg. 109, 877–884 (1995).
Iscan, Z. H., Vural, K. M., Bahar, I., Mavioglu, L. & Saritas, A. What to expect after tricuspid valve replacement? Long-term results. Eur J Cardiothorac Surg. 32, 296–300 (2007).
Thorburn, C. W., Morgan, J. J., Shanahan, M. X. & Chang, V. P. Long-term results of tricuspid valve replacement and the problem of prosthetic valve thrombosis. Am J Cardiol 51, 1128–1132 (1983).
Boskovic, D. et al. Late thrombosis of the Bjork-Shiley tilting disc valve in the tricuspid position. Thrombolytic treatment with streptokinase. J Thorac Cardiovasc Surg. 91, 1–8 (1986).
Nakano, K., Koyanagi, H., Hashimoto, A., Ohtsuka, G. & Nojiri, C. Tricuspid valve replacement with the bileaflet St. Jude Medical valve prosthesis. J Thorac Cardiovasc Surg. 108, 888–892 (1994).
Kawano, H. et al. Tricuspid valve replacement with the St. Jude Medical valve: 19 years of experience. Eur J Cardiothorac Surg. 18, 565–569 (2000).
Singh, A. K., Feng, W. C. & Sanofsky, S. J. Long-term results of St. Jude Medical valve in the tricuspid position. Ann Thorac Surg. 54, 538–540 (1992).
Aoyagi, S. et al. Long-term results of valve replacement with the St. Jude Medical valve. J Thorac Cardiovasc Surg. 108, 1021–1029 (1994).
Hwang, H. Y., Kim, K. H., Kim, K. B. & Ahn, H. Mechanical tricuspid valve replacement is not superior in patients younger than 65 years who need long-term anticoagulation. Ann Thorac Surg. 93, 1154–1160 (2012).
Haibo, Z., Jinzhong, L., Yan, L. & Xu, M. Low-intensity international normalized ratio (INR) oral anticoagulant therapy in Chinese patients with mechanical heart valve prostheses. Cell Biochem Biophys 62, 147–151 (2012).
Gurvitch, R. et al. Transcatheter valve-in-valve implantation for failed surgical bioprosthetic valves. J Am Coll Cardiol. 58, 2196–2209 (2011).
Hon, J. K. et al. Transatrial transcatheter tricuspid valve-in-valve implantation of balloon expandable bioprosthesis. Ann Thorac Surg. 90, 1696–1697 (2010).
Berger, M., Haimowitz, A., Van Tosh, A., Berdoff, R. L. & Goldberg, E. Quantitative assessment of pulmonary hypertension in patients with tricuspid regurgitation using continuous wave Doppler ultrasound. J Am Coll Cardiol. 6, 359–365 (1985).
Akins, C. W. et al. Guidelines for reporting mortality and morbidity after cardiac valve interventions. J Thorac Cardiovasc Surg. 135, 732–738 (2008).
Acknowledgements
We acknowledge the generous assistance of Qian Li for data collection.
Author information
Authors and Affiliations
Contributions
Conceived and designed the experiments: E.Z., Q.A., X.X., and L.D. Performed the experiments: X.Z. and Y.L. Analyzed the data: X.Z., Y.L., Y.G. and K.D. Contributed reagents/materials/analysis tools: X.Z. Wrote the paper: Z.W.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhu, X., Luo, Y., Zhang, E. et al. Ten-year experience of tricuspid valve replacement with the St. Jude medical valve. Sci Rep 8, 16654 (2018). https://doi.org/10.1038/s41598-018-35142-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-35142-8
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.