Abstract
Fanconi anemia (FA) is a genetically heterogeneous disorder with 22 disease-causing genes reported to date. In some FA genes, monoallelic mutations have been found to be associated with breast cancer risk, while the risk associations of others remain unknown. The gene for FA type C, FANCC, has been proposed as a breast cancer susceptibility gene based on epidemiological and sequencing studies. We used the Oncoarray project to genotype two truncating FANCC variants (p.R185X and p.R548X) in 64,760 breast cancer cases and 49,793 controls of European descent. FANCC mutations were observed in 25 cases (14 with p.R185X, 11 with p.R548X) and 26 controls (18 with p.R185X, 8 with p.R548X). There was no evidence of an association with the risk of breast cancer, neither overall (odds ratio 0.77, 95%CI 0.44–1.33, p = 0.4) nor by histology, hormone receptor status, age or family history. We conclude that the breast cancer risk association of these two FANCC variants, if any, is much smaller than for BRCA1, BRCA2 or PALB2 mutations. If this applies to all truncating variants in FANCC it would suggest there are differences between FA genes in their roles on breast cancer risk and demonstrates the merit of large consortia for clarifying risk associations of rare variants.
Similar content being viewed by others
Introduction
Fanconi Anemia (FA) is a rare recessively inherited disorder characterized by congenital malformations, progressive bone marrow failure and predisposition to cancer. Twenty-two different FA causative genes have now been identified whose products act in concert to mediate DNA interstrand crosslink repair1,2,3. At least seven of them (BRCA2/FANCD2, PALB2/FANCN, RAD51C/FANCO, RAD51/FANCR, BRCA1/FANCS, XRCC2/FANCU, and RFWD3/FANCW) are involved in different stages of homology-directed recombinational DNA repair (HRR), a pathway for error-free maintenance of the genome during replication and after DNA damage. A number of FA genes (including BRCA1/FANCS, BRCA2/FANCD1 and PALB2/FANCN) have been shown to be breast cancer susceptibility genes3. The products of BRCA1, BRCA2, and PALB2 are central to early stages of HRR. Further interactors in this pathway, in particular BRIP1/FANCJ, mainly have been linked to ovarian cancer risk4,5. It is less known to what extent other FA gene products may play a role in the inherited component of breast cancer susceptibility. Few of these other FA genes have been tested for mutations in relatively small breast cancer case-control studies, thus far6,7,8,9.
Early studies suggested that blood relatives of FA patients show an increased risk of breast cancer, although these findings have not been corroborated in a replication study and could not assess distinct FA complementation groups due to lack of genetic information at that time10,11,12,13. After FA was stratified into subsets defined by complementation assays, an increased risk of breast cancer was attributed to heterozygous carriers of FANCC mutations13. Historically, this was the first of the FA genes to be identified and accounts for 8–15% of FA cases14,15,16. More recently, FANCC has been suggested as a candidate breast cancer susceptibility gene in an exome sequencing study of 33 familial breast cancer cases and extension to another 438 cases17. However, the evidence for an association between FANCC and breast cancer risk is limited by the low prevalence of mutations17,18, and much larger numbers of individuals are needed to provide sufficient power to detect associations of plausible magnitude19.
In the present study, we genotyped two truncating variants of FANCC (p.R185X and p.R548X) using the Oncoarray (see Methods) in 64,760 female breast cancer cases and 49,793 female population controls of European descent. Both mutations are disease-causing in European FA patients and are recurrent in the FA mutation database20.
Results
We identified the truncating FANCC variants p.R185X (rs121917783) and p.R548X (rs104886457) in 40 of 153,899 individuals and 20 of 153,904 individuals, respectively. All mutation carriers were heterozygotes. Carrier distributions per study and intensity cluster plots for Europeans (which included the majority of mutation carriers) are shown in Supplementary Table 1 and Supplementary Fig. 1, respectively. Since the majority of carriers were women of European ancestry, we restricted the subsequent case-control association analysis to participants from this population. Logistic regression analyses were adjusted for study and 15 principal components21.
In Europeans, the two FANCC variants were observed in 25/64,760 cases (14 with p.R185X, 11 with p.R548X) and in 26/49,793 controls (18 with p.R185X, 8 with p.R548X). There was no evidence of association between the FANCC variants and breast cancer risk, either for carriers of both variants combined (OR 0.77, 95%CI 0.44–1.33, p = 0.35), or for either variant individually (Table 1). Similarly, we found no evidence for an association with estrogen receptor (ER)-negative (OR 0.91, 0.35–2.37) or ER-positive (OR 0.67, 0.37–1.28) disease, nor for subsets of disease defined by age at diagnosis (<50 years), bilaterality, family history, histological morphology, grade or nodal status (Table 2).
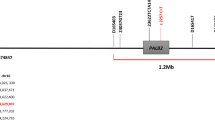
For comparison, we also analysed the PALB2/FANCN*p.R414X truncating variant that was genotyped in parallel on the same array. This variant was detected in 22/64,780 cases and 3/49,825 controls and was significantly associated with risk of breast cancer (OR 5.89, 95%CI 1.76–19.74, p = 0.004). The variant carriers were markedly enriched among cases with ER-negative tumours (p = 9.4 × 10−6; pdiff = 0.0006 in a log-likelihood ratio test) and specifically triple-negative breast tumours (p = 3.8 × 10−7; pdiff = 0.0001). The p.R414X truncating variant was also associated with ductal morphology, a positive first-degree family history of breast cancer, early age at diagnosis (<50 years), and low-differentiated tumours (grade 3) (Suppl. Table 1). Hence, by contrast with the two tested FANCC variants, p.R185X and p.R548X, the FANCN/PALB2 variant p.R414X was strongly associated with overall and with ER-negative disease under the same genotyping and analysis conditions.
Discussion
Functional defects of DNA repair are a hallmark of genomic instability syndromes as well as of carcinogenesis. FA is a genome instability and cancer prone disorder that has been investigated for breast cancer predisposition in homozygotes and heterozygotes for more than three decades11,12. Monoallelic mutations in five FA genes (BRCA1, BRCA2, PALB2, RAD51C, BRIP1) have now been confirmed to predispose to breast or ovarian cancer while biallelic mutations in these genes cause FA3. However, the role of the FA genes most commonly mutated, FANCA and FANCC, in the risk of developing breast cancer has remained uncertain. Epidemiological and segregation studies have provided some evidence of an increased breast cancer risk for grandmothers of FA patients, particularly those who carry the FANCC mutation13.
A previous sequencing study of Australian multiple-case breast cancer families had identified truncating variants in FANCC in 3 of 438 multiple-case breast cancer families but in none of 464 healthy controls, suggestive of a predisposing role for FANCC variants in breast cancer17. One of these variants, p.R185X, was also screened in our study. p.R185X was first reported shortly after the identification of the FANCC gene, and thus is one of the earliest recognized FA-causing mutations. Although representing an apparent nonsense mutation in exon 6, it also results in exon 6 being spliced out of a proportion of transcripts, suggesting this variant may alter splice site selection, with the aberrant transcript retaining the reading frame22. p.R548X, also an early-detected FANCC truncating variant23, is an authentic stop mutation in exon 14, and although in the last exon, it proved to be clearly pathogenic for FA24.
The fact that these two disease-causing variants have been frequently observed in European patients with FA20 prompted us to investigate their association with breast cancer in a large case-control study. However, we did not observe a significant difference between their frequency among breast cancer cases and controls. The upper 95% confidence limit was 1.33, thus excluding a two-fold or greater increase in risk found for moderate- or high-penetrance alleles in predisposition genes such as CHEK2 and ATM. Moreover, we found no evidence of association in subgroups defined by earlier age at onset, a positive family history of breast cancer, bilateral occurrence, or defined tumor parameters (histology, grade or hormone receptor status). However, confidence intervals for those estimates for subsets were wider as numbers were small – in particular we could not rule out a 2-fold increased risk for ER-negative or triple-negative breast cancer.
In contrast, we observed a clear association between the PALB2/FANCN variant p.R414X and breast cancer risk. PALB2 is an established breast cancer susceptibility gene, and the investigated mutation p.R414X25 occurred at a similar frequency to the tested FANCC mutations. The observed six-fold enrichment of p.R414X in breast cancer patients is in line with previous findings for other PALB2 founder mutations26,27,28 and in the upper range of the overall mutational effect size in PALB2 case-control sequencing studies29,30. We confirmed stronger associations with ER-negative breast cancer, with familial breast cancer and with a high tumor grade31. While genotyping arrays such as the Oncoarray are primarily used for evaluating common variants, these data confirm that the array provides a robust platform for evaluating even very rare alleles.
Although PALB2 and FANCC are both FA genes, their products exert different roles in the recognition and repair of DNA damage. FANCC is a component of the FA core complex which is thought to recognize an inter-strand crosslink. FANCL, an E3 ubiquitin ligase in the core complex, ubiquitinates FANCI and FANCD2. After many nuclease and translesion polymerase steps, a DNA double stranded intermediate is formed and its repair requires proteins from the homology-directed repair pathway, including FANCD1/BRCA2 and FANCN/PALB2. While truncating variants in BRCA2 and PALB2 confer a substantial risk of breast cancer, our study suggests that truncating FANCC variants do not confer a comparable risk. It is possible that members of the FA core complex that act upstream of HRR are less relevant for breast cancer due to their more specialized function in the repair of crosslinks while BRCA1, BRCA2, and PALB2 function more globally at DNA double-strand breaks. On the other hand, there is some evidence that truncating mutations in another gene involved in the early detection of intra-strand crosslinks, FANCM, are associated with both breast and ovarian cancer risk32,33,34, though FANCM is part of an anchor complex rather than the FA core complex and is not considered a classical FA gene35,36. It is also possible that the two prototype FANCC truncating variants analysed here, despite being FA-causing, have reduced penetrance for breast cancer due to some residual function, and other particular FANCC variants may confer a more substantial risk. More work will be required to clarify the role of each FA core complex member for breast cancer susceptibility.
In conclusion, our study findings suggest important differences between FA genes, indicating that truncating variants in FANCC do not confer a high overall risk of breast cancer unlike PALB2, BRCA1 and BRCA2. Our study does not exclude a role of monoallelic FANCC variants as low-penetrance alleles for breast cancer or as a genetic risk factor for certain breast cancer subgroups. Very large datasets, such as those generated through the BCAC, are critical to evaluate such rare mutations.
Methods
Patients
A total of 87 studies from the Breast Cancer Association Consortium (BCAC), of which 78 were case-control studies (some nested within prospective cohort studies) and 9 were case-only studies, contributed data as summarized in Supplementary Table 1. All studies provided data on disease status and age at diagnosis/observation, and the majority provided information on clinico-pathological and epidemiological factors, which have been curated and incorporated into the BCAC database (version 6). All participating studies were approved by their appropriate ethics review boards and all subjects provided informed consent. A list of the ethics review boards by study is provided in Supplementary Table 3.
Genotyping
The Illumina OncoArray design and genotyping procedure have been described previously21,37. In brief, approximately 72,000 variants were selected, among others, for inclusion on the array specifically for their potential relevance to breast cancer, based on prior evidence of association with overall or subtype-specific disease, with breast density or with breast tissue specific gene expression. After genotype calling and quality control of the cluster file, variants with a call rate <95% in any consortium, not in Hardy-Weinberg equilibrium (P < 10−7 in controls or P < 10−12 in cases) or with concordance <98% among 5,280 duplicate pairs were excluded. We also excluded samples with extreme heterozygosity (>4.89 standard deviations [SD] from the mean for the respective ethnicity). The final dataset, before restriction based on ethnicity, consisted of 153,673 samples of which 89,733 were cases and 63,940 were controls.
Statistical analyses
Per-allele odds ratios and 95% confidence intervals were generated using logistic regression with adjustment for principal components and study. Principal component analysis was performed using data for 33,661 uncorrelated SNPs (which included 2,318 markers of continental ancestry) with a MAF ≥ 0.05 and maximum correlation of 0.1, using purpose-written PCcalc software (written by Jonathan Tyrer and available at http://ccge.medschl.cam.ac.uk/software/pccalc/).
We also estimated subtype-specific per-allele ORs after restricting the cases by hormone receptor and/or HER2/neu status, by tumor grade, by ductal or lobular morphology, by nodal status, by bilateral occurrence of the tumor, by early diagnosis (<50 years), and by first-degree family history of breast cancer, using available BCAC data for the cases. Since we analysed 3 variants across 10 subgroups, a two-sided p-value ≤ 0.016 for the overall analyses and a two-sided p-value ≤ 0.0016 for the subgroup analyses were considered nominally significant.
Ethical approval
All experimental protocols were approved by the respective ethical institutions of participating BCAC centers. The study was carried out in accordance with the Declaration of Helsinki, and informed consent was obtained from all study participants.
Data Availability
The genotyping results from the Oncoarray are available in the dbGAP repository. The FANCC variants analysed in the current study are deposited in the NCBI SNP database as rs121917783 and rs104886457. The datasets analysed during the current study are available from the corresponding author upon reasonable request and with permission of the Data Access Committee of the Breast Cancer Association Consortium.
References
Ceccaldi, R., Sarangi, P. & D’Andrea, A. D. The Fanconi anaemia pathway: new players and new functions. Nat. Rev. Mol. Cell Biol. 17, 337–349 (2016).
Knies, K. et al. Biallelic mutations in the ubiquitin ligase RFWD3 cause Fanconi anemia. J. Clin. Invest. 127, 3013–3027 (2017).
Nalepa, G. & Clapp, D. W. Fanconi anaemia and cancer: an intricate relationship. Nat. Rev. Cancer 18, 168–185 (2018).
Ramus, S. J. et al. Germline Mutations in the BRIP1, BARD1, PALB2, and NBN Genes in Women With Ovarian Cancer. J. Natl. Cancer Inst. 107, 11 (2015).
Easton, D. F. et al. No evidence that protein truncating variants in BRIP1 are associated with breast cancer risk: implications for gene panel testing. J. Med. Genet. 53, 298–309 (2016).
García, M. J. et al. Mutational analysis of FANCL, FANCM and the recently identified FANCI suggests that among the 13 known Fanconi Anemia genes, only FANCD1/BRCA2 plays a major role in high-risk breast cancer predisposition. Carcinogenesis 30, 1898–1902 (2009).
Bakker, J. L. et al. Analysis of the novel fanconi anemia gene SLX4/FANCP in familial breast cancer cases. Hum. Mutat. 34, 70–73 (2013).
Osorio, A. et al. Evaluation of rare variants in the new fanconi anemia gene ERCC4 (FANCQ) as familial breast/ovarian cancer susceptibility alleles. Hum. Mutat. 34, 1615–1618 (2013).
Lhota, F. et al. Hereditary truncating mutations of DNA repair and other genes in BRCA1/BRCA2/PALB2-negatively tested breast cancer patients. Clin. Genet. 90, 324–333 (2016).
Swift, M. Fanconi’s anaemia in the genetics of neoplasia. Nature 230, 370–373 (1971).
Swift, M., Caldwell, R. J. & Chase, C. Reassessment of cancer predisposition of Fanconi anemia heterozygotes. J. Natl. Cancer Inst. 65, 863–867 (1980).
Jacobs, P. & Karabus, C. Fanconi’s anemia. A family study with 20-year follow-up including associated breast pathology. Cancer 54, 1850–1853 (1984).
Berwick, M. et al. Genetic heterogeneity among Fanconi anemia heterozygotes and risk of cancer. Cancer Res. 67, 9591–9596 (2007).
Strathdee, C. A. et al. Cloning of cDNAs for Fanconi’s anaemia by functional complementation. Nature 356, 763–767 (1992).
Gibson, R. A. et al. Genetic mapping of the FACC gene and linkage analysis in Fanconi anaemia families. J. Med. Genet. 31, 868–871 (1994).
Verlander, P. C. et al. Mutation analysis of the Fanconi anemia gene FACC. Am. J. Hum. Genet. 54, 595–601 (1994).
Thompson, E. R. et al. Exome sequencing identifies rare deleterious mutations in DNA repair genes FANCC and BLM as potential breast cancer susceptibility alleles. PLoS Genet. 8, e1002894 (2012).
Seal, S. et al. Evaluation of Fanconi Anemia genes in familial breast cancer predisposition. Cancer Res. 63, 8596–8599 (2003).
Ellis, N. A. & Offit, K. Heterozygous mutations in DNA repair genes and hereditary breast cancer: a question of power. PLoS Genet. 8, e1003008 (2012).
Fanconi anemia mutation database, http://www2.rockefeller.edu/fanconi/.
Michailidou, K. et al. Association analysis identifies 65 new breast cancer risk loci. Nature 551, 92–94 (2017).
Gibson, R. A. et al. A nonsense mutation and exon skipping in the Fanconi anaemia group C gene. Hum Mol Genet. 2, 797–799 (1993).
Murer-Orlando, M., Llerena, J. C. Jr. & Birjandi, F. FACC gene mutations and early prenatal diagnosis of Fanconi’s anaemia. Lancet. p. 686 (1993).
Lo ten Foe, J. R. et al. Sequence variations in the Fanconi anaemia gene, FAC: pathogenicity of 1806insA and R548X and recognition of D195V as a polymorphic variant. Hum Genet. 98, 522–523 (1996).
Bogdanova, N. et al. PALB2 mutations in German and Russian patients with bilateral breast cancer. Breast Cancer Res. Treat. 126, 545–550 (2011).
Erkko, H. et al. A recurrent mutation in PALB2 in Finnish cancer families. Nature 446, 316–319 (2007).
Southey, M. C. et al. A PALB2 mutation associated with high risk of breast cancer. Breast Cancer Res. 12, R109 (2010).
Noskowicz, M. et al. Prevalence of PALB2 mutation c.509_510delGA in unselected breast cancer patients from Central and Eastern Europe. Fam. Cancer 13, 137–142 (2014).
Rahman, N. et al. PALB2, which encodes a BRCA2-interacting protein, is a breast cancer susceptibility gene. Nat. Genet. 39, 165–167 (2007).
Tischkowitz, M. et al. Rare germline mutations in PALB2 and breast cancer risk: a population-based study. Hum. Mutat. 33, 674–680 (2012).
Heikkinen, T. et al. The breast cancer susceptibility mutation PALB2 1592delT is associated with an aggressive tumor phenotype. Clin. Cancer Res. 15, 3214–3222 (2009).
Kiiski, J. I. et al. Exome sequencing identifies FANCM as a susceptibility gene for triple-negative breast cancer. Proc. Natl. Acad. Sci. USA 111, 15172–15177 (2014).
Peterlongo, P. et al. FANCM c.5791C > T nonsense mutation (rs144567652) induces exon skipping, affects DNA repair activity and is a familial breast cancer risk factor. Hum. Mol. Genet. 24, 5345–5355 (2015).
Dicks, E. et al. Germline whole exome sequencing and large-scale replication identifies FANCM as a likely high grade serous ovarian cancer susceptibility gene. Oncotarget 8, 50930–50940 (2017).
Catucci, I. et al. Individuals with FANCM biallelic mutations do not develop Fanconi anemia, but show risk for breast cancer, chemotherapy toxicity and may display chromosome fragility. Genet. Med. 20, 452–457 (2018).
Bogliolo, M. et al. Biallelic truncating FANCM mutations cause early-onset cancer but not Fanconi anemia. Genet. Med. 20, 458–463 (2018).
Milne, R. L. et al. Identification of ten variants associated with risk of estrogen-receptor-negative breast cancer. Nat. Genet. 49, 1767–1778 (2017).
Acknowledgements
We thank all the individuals who took part in these studies and all the researchers, clinicians, technicians and administrative staff who have enabled this work to be carried out. We acknowledge all contributors to the COGS and OncoArray study design, chip design, genotyping, and genotype analyses. ABCFS thank Maggie Angelakos, Judi Maskiell, Gillian Dite. ABCS thanks the Blood bank Sanquin, The Netherlands. ABCTB Investigators: C.L.C., Rosemary Balleine, Robert Baxter, Stephen Braye, Jane Carpenter, Jane Dahlstrom, John Forbes, Soon Lee, Deborah Marsh, Adrienne Morey, Nirmala Pathmanathan, Rodney Scott, Allan Spigelman, Nicholas Wilcken, Desmond Yip. Samples are made available to researchers on a non-exclusive basis. The ACP study wishes to thank the participants in the Thai Breast Cancer study. Special Thanks also go to the Thai Ministry of Public Health (MOPH), doctors and nurses who helped with the data collection process. Finally, the study would like to thank Dr Prat Boonyawongviroj, the former Permanent Secretary of MOPH and Dr Pornthep Siriwanarungsan, the Department Director-General of Disease Control who have supported the study throughout. BBCS thanks Eileen Williams, Elaine Ryder-Mills, Kara Sargus. BCEES thanks Allyson Thomson, Christobel Saunders, Terry Slevin, BreastScreen Western Australia, Elizabeth Wylie, Rachel Lloyd. The BCINIS study would not have been possible without the contributions of Dr. K. Landsman, Dr. N. Gronich, Dr. A. Flugelman, Dr. W. Saliba, Dr. E. Liani, Dr. I. Cohen, Dr. S. Kalet, Dr. V. Friedman, Dr. O. Barnet of the NICCC in Haifa, and all the contributing family medicine, surgery, pathology and oncology teams in all medical institutes in Northern Israel. The BREOGAN study would not have been possible without the contributions of the following: Jose Esteban Castelao, Angel Carracedo, Victor Muñoz Garzón, Alejandro Novo Domínguez, Sara Miranda Ponte, Carmen Redondo Marey, Maite Peña Fernández, Manuel Enguix Castelo, Maria Torres, Manuel Calaza (BREOGAN), José Antúnez, Máximo Fraga and the staff of the Department of Pathology and Biobank of the University Hospital Complex of Santiago-CHUS, Instituto de Investigación Sanitaria de Santiago, IDIS, Xerencia de Xestion Integrada de Santiago-SERGAS; Joaquín González-Carreró and the staff of the Department of Pathology and Biobank of University Hospital Complex of Vigo, Instituto de Investigacion Biomedica Galicia Sur, SERGAS, Vigo, Spain. BSUCH thanks Peter Bugert, Medical Faculty Mannheim. The CAMA study would like to recognize CONACyT for the financial support provided for this work and all physicians responsible for the project in the different participating hospitals: Dr. Germán Castelazo (IMSS, Ciudad de México, DF), Dr. Sinhué Barroso Bravo (IMSS, Ciudad de México, DF), Dr. Fernando Mainero Ratchelous (IMSS, Ciudad de México, DF), Dr. Joaquín Zarco Méndez (ISSSTE, Ciudad de México, DF), Dr. Edelmiro Pérez Rodríguez (Hospital Universitario, Monterrey, Nuevo León), Dr. Jesús Pablo Esparza Cano (IMSS, Monterrey, Nuevo León), Dr. Heriberto Fabela (IMSS, Monterrey, Nuevo León), Dr. Fausto Hernández Morales (ISSSTE, Veracruz, Veracruz), Dr. Pedro Coronel Brizio (CECAN SS, Xalapa, Veracruz) and Dr. Vicente A. Saldaña Quiroz (IMSS, Veracruz, Veracruz). CBCS thanks study participants, co-investigators, collaborators and staff of the Canadian Breast Cancer Study, and project coordinators Agnes Lai and Celine Morissette. CCGP thanks Styliani Apostolaki, Anna Margiolaki, Georgios Nintos, Maria Perraki, Georgia Saloustrou, Georgia Sevastaki, Konstantinos Pompodakis. CGPS thanks staff and participants of the Copenhagen General Population Study. For the excellent technical assistance: Dorthe Uldall Andersen, Maria Birna Arnadottir, Anne Bank, Dorthe Kjeldgård Hansen. The Danish Cancer Biobank is acknowledged for providing infrastructure for the collection of blood samples for the cases. COLBCCC thanks all patients, the physicians Justo G. Olaya, Mauricio Tawil, Lilian Torregrosa, Elias Quintero, Sebastian Quintero, Claudia Ramírez, José J. Caicedo, and Jose F. Robledo, the researchers Ignacio Briceno, Fabian Gil, Angela Umana, Angela Beltran and Viviana Ariza, and the technician Michael Gilbert for their contributions and commitment to this study. Investigators from the CPSII cohort thank the participants and Study Management Group for their invaluable contributions to this research. They also acknowledge the contribution to this study from central cancer registries supported through the Centers for Disease Control and Prevention National Program of Cancer Registries, as well as cancer registries supported by the National Cancer Institute Surveillance Epidemiology and End Results program. CTS Investigators include Leslie Bernstein, S.L.N., James Lacey, Sophia Wang, and Huiyan Ma at the Beckman Research Institute of City of Hope, Jessica Clague DeHart at the School of Community and Global Health Claremont Graduate University, Dennis Deapen, Rich Pinder, and Eunjung Lee at the University of Southern California, Pam Horn-Ross, Christina Clarke Dur and David Nelson at the Cancer Prevention Institute of California, Peggy Reynolds, at the Department of Epidemiology and Biostatistics, University of California San Francisco, H.A-C, A.Z., and Hannah Park at the University of California Irvine, and Fred Schumacher at Case Western University. DIETCOMPLYF thanks the patients, nurses and clinical staff involved in the study. We thank the participants and the investigators of EPIC (European Prospective Investigation into Cancer and Nutrition). ESTHER thanks Hartwig Ziegler, Sonja Wolf, Volker Hermann, Christa Stegmaier, Katja Butterbach. FHRISK thanks NIHR for funding. GC-HBOC thanks Stefanie Engert, Heide Hellebrand, Sandra Kröber and LIFE - Leipzig Research Centre for Civilization Diseases (Markus Loeffler, Joachim Thiery, Matthias Nüchter, Ronny Baber). The GENICA Network: Dr. Margarete Fischer-Bosch-Institute of Clinical Pharmacology, Stuttgart, and University of Tübingen, Germany [H.B., W-Y.L.], German Cancer Consortium (DKTK) and German Cancer Research Center (DKFZ) [H.B.], Deutsche Forschungsgemeinschaft (DFG, German Research Foundation) under Germany’s Excellence Strategy - EXC 2180 - 390900677, Department of Internal Medicine, Evangelische Kliniken Bonn gGmbH, Johanniter Krankenhaus, Bonn, Germany [Yon-Dschun Ko, Christian Baisch], Institute of Pathology, University of Bonn, Germany [Hans-Peter Fischer], Molecular Genetics of Breast Cancer, Deutsches Krebsforschungszentrum (DKFZ), Heidelberg, Germany [UH], Institute for Prevention and Occupational Medicine of the German Social Accident Insurance, Institute of the Ruhr University Bochum (IPA), Bochum, Germany [Thomas Brüning, Beate Pesch, Sylvia Rabstein, Anne Lotz]; and Institute of Occupational Medicine and Maritime Medicine, University Medical Center Hamburg-Eppendorf, Germany [Volker Harth]. HABCS thanks Michael Bremer and Johann H. Karstens. HEBCS thanks Sofia Khan, Johanna Kiiski, Kristiina Aittomäki, Rainer Fagerholm, Kirsimari Aaltonen, Karl von Smitten, Irja Erkkilä. HKBCS thanks Hong Kong Sanatorium and Hospital, Dr Ellen Li Charitable Foundation, The Kerry Group Kuok Foundation, National Institute of Health 1R03CA130065 and the North California Cancer Center for support. HMBCS thanks Johann H. Karstens. HUBCS thanks Shamil Gantsev. KARMA thanks the Swedish Medical Research Counsel. KBCP thanks Eija Myöhänen, Helena Kemiläinen. We thank all investigators of the KOHBRA (Korean Hereditary Breast Cancer) Study. LMBC thanks Gilian Peuteman, Thomas Van Brussel, EvyVanderheyden and Kathleen Corthouts. MABCS thanks Milena Jakimovska (RCGEB “Georgi D. Efremov), Emilija Lazarova (University Clinic of Radiotherapy and Oncology), Katerina Kubelka-Sabit, Mitko Karadjozov (Adzibadem-Sistina Hospital), Andrej Arsovski and Liljana Stojanovska (Re-Medika Hospital) for their contributions and commitment to this study. MARIE thanks Petra Seibold, Dieter Flesch-Janys, Judith Heinz, Nadia Obi, Alina Vrieling, Sabine Behrens, Ursula Eilber, Muhabbet Celik, Til Olchers and Stefan Nickels. MBCSG (Milan Breast Cancer Study Group): Bernard Peissel, Jacopo Azzollini, Dario Zimbalatti, Daniela Zaffaroni, Bernardo Bonanni, Mariarosaria Calvello, Davide Bondavalli, Aliana Guerrieri Gonzaga, Monica Marabelli, Irene Feroce, and the personnel of the Cogentech Cancer Genetic Test Laboratory. We thank the coordinators, the research staff and especially the MMHS participants for their continued collaboration on research studies in breast cancer. MSKCC thanks Marina Corines, Lauren Jacobs. MTLGEBCS would like to thank Martine Tranchant (CHU de Québec– Université Laval Research Center), Marie-France Valois, Annie Turgeon and Lea Heguy (McGill University Health Center, Royal Victoria Hospital; McGill University) for DNA extraction, sample management and skillful technical assistance. J.S. is Chair holder of the Canada Research Chair in Oncogenetics. MYBRCA thanks study participants and research staff (particularly Patsy Ng, Nurhidayu Hassan, Yoon Sook-Yee, Daphne Lee, Lee Sheau Yee, Phuah Sze Yee and Norhashimah Hassan) for their contributions and commitment to this study. The NBCS Collaborators would like to thank the Oslo Breast Cancer Research Consortium, OSBREAC (breastcancerresearch.no/osbreac/), for providing samples and phenotype data. NBHS and SBCGS thank study participants and research staff for their contributions and commitment to the studies. We would like to thank the participants and staff of the Nurses’ Health Study and Nurses’ Health Study II for their valuable contributions as well as the following state cancer registries for their help: AL, AZ, AR, CA, CO, CT, DE, FL, GA, ID, IL, IN, IA, KY, LA, ME, MD, MA, MI, NE, NH, NJ, NY, NC, ND, OH, OK, OR, PA, RI, SC, TN, TX, VA, WA, WY. The authors assume full responsibility for analyses and interpretation of these data. OFBCR thanks Teresa Selander, Nayana Weerasooriya. ORIGO thanks E. Krol-Warmerdam, and J. Blom for patient accrual, administering questionnaires, and managing clinical information. The ORIGO survival data were retrieved from the Leiden hospital-based cancer registry system (ONCDOC) with the help of Dr. J. Molenaar. PBCS thanks Louise Brinton, Mark Sherman, Neonila Szeszenia-Dabrowska, Beata Peplonska, Witold Zatonski, Pei Chao, Michael Stagner. The ethical approval for the POSH study is MREC /00/6/69, UKCRN ID: 1137. We thank staff in the Experimental Cancer Medicine Centre (ECMC) supported Faculty of Medicine Tissue Bank and the Faculty of Medicine DNA Banking resource. PREFACE thanks Sonja Oeser and Silke Landrith. PROCAS thanks NIHR for funding. RBCS thanks Petra Bos, Jannet Blom, Ellen Crepin, Elisabeth Huijskens, Anja Kromwijk-Nieuwlaat, Annette Heemskerk, the Erasmus MC Family Cancer Clinic. We thank the SEARCH and EPIC teams. SGBCC thanks the participants and research coordinator Ms Tan Siew Li. SKKDKFZS thanks all study participants, clinicians, family doctors, researchers and technicians for their contributions and commitment to this study. We thank the SUCCESS Study teams in Munich, Duessldorf, Erlangen and Ulm. SZBCS thanks Ewa Putresza. UCIBCS thanks Irene Masunaka. UKBGS thanks Breast Cancer Now and the Institute of Cancer Research for support and funding of the Breakthrough Generations Study, and the study participants, study staff, and the doctors, nurses and other health care providers and health information sources who have contributed to the study. We acknowledge NHS funding to the Royal Marsden/ICR NIHR Biomedical Research Centre. BCAC is funded by Cancer Research UK [C1287/A16563, C1287/A10118], the European Union’s Horizon 2020 Research and Innovation Programme (grant numbers 634935 and 633784 for BRIDGES and B-CAST respectively), and by the European Community’s Seventh Framework Programme under grant agreement number 223175 (Grant Number HEALTH-F2-2009-223175) (COGS). The EU Horizon 2020 Research and Innovation Programme funding source had no role in study design, data collection, data analysis, data interpretation or writing of the report. Genotyping of the OncoArray was funded by the NIH Grant U19 CA148065, and Cancer UK Grant C1287/A16563 and the PERSPECTIVE project supported by the Government of Canada through Genome Canada and the Canadian Institutes of Health Research (grant GPH-129344) and, the Ministère de l’Économie, Science et Innovation du Québec through Genome Québec and the PSR-SIIRI-701 grant, and the Quebec Breast Cancer Foundation. Funding for the iCOGS infrastructure came from: the European Community’s Seventh Framework Programme under grant agreement No. 223175 (HEALTH-F2-2009-223175) (COGS), Cancer Research UK (C1287/A10118, C1287/A10710, C12292/A11174, C1281/A12014, C5047/A8384, C5047/A15007, C5047/A10692, C8197/A16565), the National Institutes of Health (CA128978) and Post-Cancer GWAS initiative (1U19 CA148537, 1U19 CA148065 and 1U19 CA148112 - the GAME-ON initiative), the Department of Defence (W81XWH-10-1-0341), the Canadian Institutes of Health Research (CIHR) for the CIHR Team in Familial Risks of Breast Cancer, and Komen Foundation for the Cure, the Breast Cancer Research Foundation, and the Ovarian Cancer Research Fund. The DRIVE Consortium was funded by U19 CA148065. The Australian Breast Cancer Family Study (ABCFS), BCFR-NY, BCFR-PA, BCFR-UTAH, the Northern California Breast Cancer Family Registry (NC-BCFR) and Ontario Familial Breast Cancer Registry (OFBCR) were supported by grant UM1 CA164920 from the National Cancer Institute (USA). The content of this manuscript does not necessarily reflect the views or policies of the National Cancer Institute or any of the collaborating centers in the Breast Cancer Family Registry (BCFR), nor does mention of trade names, commercial products, or organizations imply endorsement by the USA Government or the BCFR. The ABCFS was also supported by the National Health and Medical Research Council of Australia, the New South Wales Cancer Council, the Victorian Health Promotion Foundation (Australia) and the Victorian Breast Cancer Research Consortium. J.L.H. is a National Health and Medical Research Council (NHMRC) Senior Principal Research Fellow. M.C.S. is a NHMRC Senior Research Fellow. The ABCS study was supported by the Dutch Cancer Society [grants NKI 2007-3839; 2009 4363]. The Australian Breast Cancer Tissue Bank (ABCTB) was supported by the National Health and Medical Research Council of Australia, The Cancer Institute NSW and the National Breast Cancer Foundation. C.L.C is a NHMRC Principal Research Fellow. The ACP study is funded by the Breast Cancer Research Trust, UK and KM and AL are supported by the NIHR Manchester Biomedical Research Centre and by the ICEP (“This work was also supported by CRUK [grant number C18281/A19169]”). The AHS study is supported by the intramural research program of the National Institutes of Health, the National Cancer Institute (grant number Z01-CP010119), and the National Institute of Environmental Health Sciences (grant number Z01-ES049030). The work of the BBCC was partly funded by ELAN-Fond of the University Hospital of Erlangen. The BBCS is funded by Cancer Research UK and Breast Cancer Now and acknowledges NHS funding to the NIHR Biomedical Research Centre, and the National Cancer Research Network (NCRN). The BCEES was funded by the National Health and Medical Research Council, Australia and the Cancer Council Western Australia and acknowledges funding from the National Breast Cancer Foundation (J.S.). The BREast Oncology GAlician Network (BREOGAN) is funded by Acción Estratégica de Salud del Instituto de Salud Carlos III FIS PI12/02125/Cofinanciado FEDER; Acción Estratégica de Salud del Instituto de Salud Carlos III FIS Intrasalud (PI13/01136); Programa Grupos Emergentes, Cancer Genetics Unit, Instituto de Investigacion Biomedica Galicia Sur. Xerencia de Xestion Integrada de Vigo-SERGAS, Instituto de Salud Carlos III, Spain; Grant 10CSA012E, Consellería de Industria Programa Sectorial de Investigación Aplicada, PEME I + D e I + D Suma del Plan Gallego de Investigación, Desarrollo e Innovación Tecnológica de la Consellería de Industria de la Xunta de Galicia, Spain; Grant EC11-192. Fomento de la Investigación Clínica Independiente, Ministerio de Sanidad, Servicios Sociales e Igualdad, Spain; and Grant FEDER-Innterconecta. Ministerio de Economia y Competitividad, Xunta de Galicia, Spain. The BSUCH study was supported by the Dietmar-Hopp Foundation, the Helmholtz Society and the German Cancer Research Center (DKFZ). The CAMA study was funded by Consejo Nacional de Ciencia y Tecnología (CONACyT) (SALUD-2002-C01-7462). Sample collection and processing was funded in part by grants from the National Cancer Institute (NCI R01CA120120 and K24CA169004). CBCS is funded by the Canadian Cancer Society (grant #313404) and the Canadian Institutes of Health Research. CCGP is supported by funding from the University of Crete. The CECILE study was supported by Fondation de France, Institut National du Cancer (INCa), Ligue Nationale contre le Cancer, Agence Nationale de Sécurité Sanitaire, de l’Alimentation, de l’Environnement et du Travail (ANSES), Agence Nationale de la Recherche (ANR). The CGPS was supported by the Chief Physician Johan Boserup and Lise Boserup Fund, the Danish Medical Research Council, and Herlev and Gentofte Hospital. COLBCCC is supported by the German Cancer Research Center (DKFZ), Heidelberg, Germany. Diana Torres was in part supported by a postdoctoral fellowship from the Alexander von Humboldt Foundation. The American Cancer Society funds the creation, maintenance, and updating of the CPSII cohort. The CTS was supported by the California Breast Cancer Act of 1993, the California Breast Cancer Research Fund (contract 97-10500) and the National Institutes of Health (R01 CA77398, K05 CA136967, UM1 CA164917, and U01 CA199277). Collection of cancer incidence data was supported by the California Department of Public Health as part of the statewide cancer reporting program mandated by California Health and Safety Code Section 103885. HAC receives support from the Lon V Smith Foundation (LVS39420). The University of Westminster curates the DietCompLyf database funded by the charity Against Breast Cancer (Registered Charity No. 1121258) and the NCRN. The coordination of EPIC is financially supported by the European Commission (DG-SANCO) and the International Agency for Research on Cancer. The national cohorts are supported by: Ligue Contre le Cancer, Institut Gustave Roussy, Mutuelle Générale de l’Education Nationale, Institut National de la Santé et de la Recherche Médicale (INSERM) (France); German Cancer Aid, German Cancer Research Center (DKFZ), Federal Ministry of Education and Research (BMBF) (Germany); the Hellenic Health Foundation, the Stavros Niarchos Foundation (Greece); Associazione Italiana per la Ricerca sul Cancro-AIRC-Italy and National Research Council (Italy); Dutch Ministry of Public Health, Welfare and Sports (VWS), Netherlands Cancer Registry (NKR), LK Research Funds, Dutch Prevention Funds, Dutch ZON (Zorg Onderzoek Nederland), World Cancer Research Fund (WCRF), Statistics Netherlands (The Netherlands); Health Research Fund (FIS), PI13/00061 to Granada, PI13/01162 to EPIC-Murcia, Regional Governments of Andalucía, Asturias, Basque Country, Murcia and Navarra, ISCIII RETIC (RD06/0020) (Spain); Cancer Research UK (14136 to EPIC-Norfolk; C570/A16491 and C8221/A19170 to EPIC-Oxford), Medical Research Council (1000143 to EPIC-Norfolk, MR/M012190/1 to EPIC-Oxford) (United Kingdom). The ESTHER study was supported by a grant from the Baden Württemberg Ministry of Science, Research and Arts. Additional cases were recruited in the context of the VERDI study, which was supported by a grant from the German Cancer Aid (Deutsche Krebshilfe). FHRISK is funded from NIHR grant PGfAR 0707-10031. DGE is supported by the all Manchester NIHR Biomedical Research Centre (IS-BRC-1215-20007). The GC-HBOC (German Consortium of Hereditary Breast and Ovarian Cancer) is supported by the German Cancer Aid (grant no 110837, coordinator: R.K.S., Cologne). This work was also funded by the European Regional Development Fund and Free State of Saxony, Germany (LIFE - Leipzig Research Centre for Civilization Diseases, project numbers 713-241202, 713-241202, 14505/2470, 14575/2470). The GENICA was funded by the Federal Ministry of Education and Research (BMBF) Germany grants 01KW9975/5, 01KW9976/8, 01KW9977/0 and 01KW0114, the Robert Bosch Foundation, Stuttgart, Deutsches Krebsforschungszentrum (DKFZ), Heidelberg, the Institute for Prevention and Occupational Medicine of the German Social Accident Insurance, Institute of the Ruhr University Bochum (IPA), Bochum, as well as the Department of Internal Medicine, Evangelische Kliniken Bonn gGmbH, Johanniter Krankenhaus, Bonn, Germany. The GEPARSIXTO study was conducted by the German Breast Group GmbH. The GESBC was supported by the Deutsche Krebshilfe e. V. [70492] and the German Cancer Research Center (DKFZ). The HABCS study was supported by the Claudia von Schilling Foundation for Breast Cancer Research, by the Lower Saxonian Cancer Society, by the Friends of Hannover Medical School and by the Rudolf Bartling Foundation. The HEBCS was financially supported by the Helsinki University Central Hospital Research Fund, Academy of Finland (266528), the Finnish Cancer Society, and the Sigrid Juselius Foundation. The HERPACC was supported by MEXT Kakenhi (No. 170150181 and 26253041) from the Ministry of Education, Science, Sports, Culture and Technology of Japan, by a Grant-in-Aid for the Third Term Comprehensive 10-Year Strategy for Cancer Control from Ministry Health, Labour and Welfare of Japan, by Health and Labour Sciences Research Grants for Research on Applying Health Technology from Ministry Health, Labour and Welfare of Japan, by National Cancer Center Research and Development Fund, and “Practical Research for Innovative Cancer Control (15ck0106177h0001)” from Japan Agency for Medical Research and development, AMED, and Cancer Bio Bank Aichi. The HMBCS and HUBCS were funded by the German Research Foundation (Do761/10-1) and by the Rudolf Bartling Foundation. The HUBCS was further supported by a grant from the German Federal Ministry of Research and Education (RUS08/017), and by the Russian Foundation for Basic Research and the Federal Agency for Scientific Organizations for support the Bioresource collections and RFBR grants 14-04-97088, 17-29-06014 and 17-44-020498. Financial support for KARBAC was provided through the regional agreement on medical training and clinical research (ALF) between Stockholm County Council and Karolinska Institutet, the Swedish Cancer Society, The Gustav V Jubilee foundation and Bert von Kantzows foundation. The KARMA study was supported by Märit and Hans Rausings Initiative Against Breast Cancer. The KBCP was financially supported by the special Government Funding (EVO) of Kuopio University Hospital grants, Cancer Fund of North Savo, the Finnish Cancer Organizations, and by the strategic funding of the University of Eastern Finland. The KOHBRA study was partially supported by a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), and the National R&D Program for Cancer Control, Ministry of Health & Welfare, Republic of Korea (HI16C1127; 1020350; 1420190). LMBC is supported by the ‘Stichting tegen Kanker’. DL is supported by the FWO. The MABCS study is funded by the Research Centre for Genetic Engineering and Biotechnology “Georgi D. Efremov” and supported by the German Academic Exchange Program, DAAD. The MARIE study was supported by the Deutsche Krebshilfe e.V. [70-2892-BR I, 106332, 108253, 108419, 110826, 110828], the Hamburg Cancer Society, the German Cancer Research Center (DKFZ) and the Federal Ministry of Education and Research (BMBF) Germany [01KH0402]. MBCSG is supported by grants from the Italian Association for Cancer Research (AIRC) and by funds from the Italian citizens who allocated the 5/1000 share of their tax payment in support of the Fondazione IRCCS Istituto Nazionale Tumori, according to Italian laws (INT-Institutional strategic projects “5 × 1000”). The MCBCS was supported by the NIH grants CA192393, CA116167, CA176785 an NIH Specialized Program of Research Excellence (SPORE) in Breast Cancer [CA116201], and the Breast Cancer Research Foundation and a generous gift from the David F. and Margaret T. Grohne Family Foundation. MCCS cohort recruitment was funded by VicHealth and Cancer Council Victoria. The MCCS was further supported by Australian NHMRC grants 209057 and 396414, and by infrastructure provided by Cancer Council Victoria. Cases and their vital status were ascertained through the Victorian Cancer Registry (VCR) and the Australian Institute of Health and Welfare (AIHW), including the National Death Index and the Australian Cancer Database. The MEC was supported by NIH grants CA63464, CA54281, CA098758, CA132839 and CA164973. The MISS study is supported by funding from ERC-2011-294576 Advanced grant, Swedish Cancer Society, Swedish Research Council, Local hospital funds, Berta Kamprad Foundation, Gunnar Nilsson. The MMHS study was supported by NIH grants CA97396, CA128931, CA116201, CA140286 and CA177150. MSKCC is supported by grants from the Breast Cancer Research Foundation and Robert and Kate Niehaus Clinical Cancer Genetics Initiative. The work of MTLGEBCS was supported by the Quebec Breast Cancer Foundation, the Canadian Institutes of Health Research for the “CIHR Team in Familial Risks of Breast Cancer” program – grant #CRN-87521 and the Ministry of Economic Development, Innovation and Export Trade – grant #PSR-SIIRI-701. MYBRCA is funded by research grants from the Malaysian Ministry of Higher Education (UM.C/HlR/MOHE/06) and Cancer Research Malaysia. MYMAMMO is supported by research grants from Yayasan Sime Darby LPGA Tournament and Malaysian Ministry of Higher Education (RP046B-15HTM). The NBCS has received funding from the K.G. Jebsen Centre for Breast Cancer Research; the Research Council of Norway grant 193387/V50 (to A-L Børresen-Dale and V.N.K.) and grant 193387/H10 (to A-L Børresen-Dale and V.N.K.), South Eastern Norway Health Authority (grant 39346 to A-L Børresen-Dale) and the Norwegian Cancer Society (to A-L Børresen-Dale and V.N.K.). The NBHS was supported by NIH grant R01CA100374. Biological sample preparation was conducted the Survey and Biospecimen Shared Resource, which is supported by P30 CA68485. The Carolina Breast Cancer Study (NCBCS) was funded by Komen Foundation, the National Cancer Institute (P50 CA058223, U54 CA156733, U01 CA179715), and the North Carolina University Cancer Research Fund. The NGOBCS was supported by the National Cancer Center Research and Development Fund. The NHS was supported by NIH grants P01 CA87969, UM1 CA186107, and U19 CA148065. The NHS2 was supported by NIH grants UM1 CA176726 and U19 CA148065. The ORIGO study was supported by the Dutch Cancer Society (RUL 1997-1505) and the Biobanking and Biomolecular Resources Research Infrastructure (BBMRI-NL CP16). The PBCS was funded by Intramural Research Funds of the National Cancer Institute, Department of Health and Human Services, USA. Genotyping for PLCO was supported by the Intramural Research Program of the National Institutes of Health, NCI, Division of Cancer Epidemiology and Genetics. The PLCO is supported by the Intramural Research Program of the Division of Cancer Epidemiology and Genetics and supported by contracts from the Division of Cancer Prevention, National Cancer Institute, National Institutes of Health. The POSH study is funded by Cancer Research UK (grants C1275/A11699, C1275/C22524, C1275/A19187, C1275/A15956 and Breast Cancer Campaign 2010PR62, 2013PR044. PROCAS is funded from NIHR grant PGfAR 0707-10031. The RBCS was funded by the Dutch Cancer Society (DDHK 2004-3124, DDHK 2009-4318). The SASBAC study was supported by funding from the Agency for Science, Technology and Research of Singapore (A*STAR), the US National Institute of Health (NIH) and the Susan G. Komen Breast Cancer Foundation. The SBCGS was supported primarily by NIH grants R01CA64277, R01CA148667, UMCA182910, and R37CA70867. Biological sample preparation was conducted the Survey and Biospecimen Shared Resource, which is supported by P30 CA68485. The scientific development and funding of this project were, in part, supported by the Genetic Associations and Mechanisms in Oncology (GAME-ON) Network U19 CA148065. SEARCH is funded by Cancer Research UK [C490/A10124, C490/A16561] and supported by the UK National Institute for Health Research Biomedical Research Centre at the University of Cambridge. The University of Cambridge has received salary support for PDPP from the NHS in the East of England through the Clinical Academic Reserve. SEBCS was supported by the BRL (Basic Research Laboratory) program through the National Research Foundation of Korea funded by the Ministry of Education, Science and Technology (2012-0000347). SGBCC is funded by the NUS start-up Grant, National University Cancer Institute Singapore (NCIS) Centre Grant and the NMRC Clinician Scientist Award. Additional controls were recruited by the Singapore Consortium of Cohort Studies-Multi-ethnic cohort (SCCS-MEC), which was funded by the Biomedical Research Council, grant number: 05/1/21/19/425. The Sister Study (SISTER) is supported by the Intramural Research Program of the NIH, National Institute of Environmental Health Sciences (Z01-ES044005 and Z01-ES049033). The Two Sister Study (2SISTER) was supported by the Intramural Research Program of the NIH, National Institute of Environmental Health Sciences (Z01-ES044005 and Z01-ES102245), and, also by a grant from Susan G. Komen for the Cure, grant FAS0703856. SKKDKFZS is supported by the DKFZ. The SMC is funded by the Swedish Cancer Foundation. The SZBCS was supported by Grant PBZ_KBN_122/P05/2004. The TNBCC was supported by: a Specialized Program of Research Excellence (SPORE) in Breast Cancer (CA116201), a grant from the Breast Cancer Research Foundation, a generous gift from the David F. and Margaret T. Grohne Family Foundation and the Ohio State University Comprehensive Cancer Center. The TWBCS is supported by the Taiwan Biobank project of the Institute of Biomedical Sciences, Academia Sinica, Taiwan. The UCIBCS component of this research was supported by the NIH [CA58860, CA92044] and the Lon V Smith Foundation [LVS39420]. The UKBGS is funded by Breast Cancer Now and the Institute of Cancer Research (ICR), London. ICR acknowledges NHS funding to the NIHR Biomedical Research Centre. The UKOPS study was funded by The Eve Appeal (The Oak Foundation) and supported by the National Institute for Health Research University College London Hospitals Biomedical Research Centre. The USRT Study was funded by Intramural Research Funds of the National Cancer Institute, Department of Health and Human Services, USA. The WAABCS study was supported by grants from the National Cancer Institute of the National Institutes of Health (R01 CA89085 and P50 CA125183 and the D43 TW009112 grant), Susan G. Komen (SAC110026), the Dr. Ralph and Marian Falk Medical Research Trust, and the Avon Foundation for Women.
Author information
Authors and Affiliations
Author notes
A comprehensive list of consortium members appears at the end of the paper.
Consortia
Contributions
Study design: Thilo Dörk, Alison M. Dunning, Paul D.P. Pharoah, Detlev Schindler, and Douglas F. Easton. Data management: Manjeet K. Bolla, Qin Wang, Joe Dennis. Data and material contributions: Thilo Dörk, Paolo Peterlongo, Arto Mannermaa, Manjeet K. Bolla, Qin Wang, Joe Dennis, Thomas Ahearn, Irene L. Andrulis, Hoda Anton-Culver, Volker Arndt, Kristan J. Aronson, Annelie Augustinsson, Laura E. Beane Freeman, Matthias W. Beckmann, Alicia Beeghly, Sabine Behrens, Marina Bermisheva, Carl Blomqvist, Natalia V. Bogdanova, Stig E. Bojesen, Hiltrud Brauch, Hermann Brenner, Barbara Burwinkel, Federico Canzian, Tsun L. Chan, Jenny Chang-Claude, Stephen J. Chanock, Ji-Yeob Choi, Hans Christiansen, Christine L. Clarke, Fergus J. Couch, Kamila Czene, Mary B. Daly, Isabel dos-Santos-Silva, Miriam Dwek, Diana M. Eccles, Arif B. Ekici, Mikael Eriksson, D. Gareth Evans, Peter A. Fasching, Jonine Figueroa, Henrik Flyger, Lin Fritschi, Marike Gabrielson, Manuela Gago-Dominguez, Chi Gao, Susan M. Gapstur, Montserrat García-Closas, José A. García-Sáenz, Mia M. Gaudet, Graham G. Giles, Mark S. Goldberg, David E. Goldgar, Pascal Guénel, Lothar Haeberle, Christopher A. Haiman, Niclas Håkansson, Per Hall, Ute Hamann, Mikael Hartman, Jan Hauke, Alexander Hein, Peter Hillemanns, Frans B.L. Hogervorst Maartje J. Hooning, John L. Hopper, Tony Howell, Dezheng Huo, Hidemi Ito, Motoki Iwasaki, Anna Jakubowska, Wolfgang Janni, Esther M. John, Audrey Jung, Rudolf Kaaks, Daehee Kang, Pooja Middha Kapoor, Elza Khusnutdinova, Sung-Won Kim, Cari M. Kitahara, Stella Koutros, Peter Kraft, Vessela N. Kristensen, Ava Kwong, Diether Lambrechts, Loic Le Marchand, Jingmei Li, Sara Lindström, Martha Linet, Wing-Yee Lo, Jirong Long, Artitaya Lophatananon, Jan Lubiński, Mehdi Manoochehri, Siranoush Manoukian, Sara Margolin, Elena Martinez, Keitaro Matsuo, Dimitris Mavroudis, Alfons Meindl, Usha Menon, Roger L. Milne, Nur Aishah Mohd Taib, Kenneth Muir, Anna Marie Mulligan, Susan L. Neuhausen, Heli Nevanlinna, Patrick Neven, William G. Newman, Kenneth Offit, Olufunmilayo I. Olopade, Andrew F. Olshan, Janet E. Olson, Håkan Olsson, Sue K. Park, Tjoung-Won Park-Simon, Julian Peto, Dijana Plaseska-Karanfilska, Esther Pohl-Rescigno, Nadege Presneau, Brigitte Rack, Paolo Radice, Muhammad U. Rashid, Gad Rennert, Hedy S. Rennert, Atocha Romero, Matthias Ruebner, Emmanouil Saloustros, Marjanka K. Schmidt, Rita K. Schmutzler, Michael O. Schneider, Minouk J. Schoemaker, Christopher Scott, Chen-Yang Shen, Xiao-Ou Shu, Jacques Simard, Susan Slager, Snezhana Smichkoska, Melissa C. Southey, John J. Spinelli, Jennifer Stone, Harald Surowy, Anthony J. Swerdlow, Rulla M. Tamimi, William J. Tapper, Soo H. Teo, Mary Beth Terry, Amanda E. Toland, Rob A.E.M. Tollenaar, Diana Torres, Gabriela Torres-Mejía, Melissa A. Troester, Thérèse Truong, Shoichiro Tsugane, Michael Untch, Celine M. Vachon, Ans M.W. van den Ouweland, Elke M. van Veen, Joseph Vijai, Camilla Wendt, Alicja Wolk, Jyh-Cherng Yu, Wei Zheng, Argyrios Ziogas, Elad Ziv, ABCTB Investigators, NBCS Collaborators, Alison M. Dunning, Paul D.P. Pharoah, Peter Devilee, Douglas F. Easton. Data analyses: Thilo Dörk, Joe Dennis; Manuscript writing: Thilo Dörk, Paolo Peterlongo, Arto Mannermaa, M.K.B., Detlev Schindler, Peter Devilee and Douglas F. Easton; Manuscript correction and approval: all authors.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dörk, T., Peterlongo, P., Mannermaa, A. et al. Two truncating variants in FANCC and breast cancer risk. Sci Rep 9, 12524 (2019). https://doi.org/10.1038/s41598-019-48804-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-48804-y
This article is cited by
-
A comprehensive analysis of Fanconi anemia genes in Chinese patients with high-risk hereditary breast cancer
Journal of Cancer Research and Clinical Oncology (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.