Abstract
Women-who-have-sex-with-women (WSW) are at increased risk of bacterial vaginosis (BV). We investigated the impact of practices and past BV on the vaginal microbiota within a two-year longitudinal cohort of Australian WSW. Self-collected vaginal swabs were used to characterise the vaginal microbiota using 16S-rRNA gene sequencing. Hierarchical clustering defined community state types (CSTs). Bacterial diversity was calculated using the Shannon diversity index and instability of the vaginal microbiota was assessed by change of CST and Bray-Curtis dissimilarity. Sex with a new partner increased the bacterial diversity (adjusted-coefficient = 0.41, 95%CI: 0.21,0.60, p < 0.001) and instability of the vaginal microbiota, in terms of both change of CST (adjusted-odds-ratio = 2.65, 95%CI: 1.34,5.22, p = 0.005) and increased Bray-Curtis dissimilarity (adjusted-coefficient = 0.21, 95%CI: 0.11,0.31, p < 0.001). Women reporting sex with a new partner were more likely than women reporting no new partner to have a vaginal microbiota characterised by Gardnerella vaginalis (adjusted-relative-risk-ratio[aRRR] = 3.45, 95%CI: 1.42,8.41, p = 0.006) or anaerobic BV-associated bacteria (aRRR = 3.62, 95%CI: 1.43,9.14, p = 0.007) relative to a Lactobacillus crispatus dominated microbiota. Sex with a new partner altered the vaginal microbiota of WSW by increasing the diversity and abundance of BV-associated bacteria. These findings highlight the influence of practices on the development of a non-optimal vaginal microbiota and provide microbiological support for the sexual exchange of bacteria between women.
Similar content being viewed by others
Introduction
The vaginal microbiota has an important role in protecting against a range of adverse obstetric and gynaecological outcomes including miscarriage, preterm birth, and transmission and acquisition of sexually transmitted diseases (STIs) and HIV1,2,3,4. The optimal vaginal microbiota of reproductive aged women is typically characterised by low bacterial diversity and high relative abundance of Lactobacillus spp., commonly Lactobacillus crispatus5,6,7.
Bacterial vaginosis (BV) is the most common vaginal dysbiosis and is characterised by a decrease in lactobacilli and increase in the diversity and abundance of facultative and strict anaerobic bacteria including Gardnerella vaginalis5,8,9. The pathogenesis of BV is complex and mounting epidemiological and microbiological evidence suggests that sexual activity has a role in both BV incidence and recurrence. Inconsistent condom use and new or increased numbers of sexual partners have been shown by meta-analysis to increase BV risk10. Other sexual practices associated with increased risk of BV include penile-vaginal sex11,12, vaginal sex after anal sex12, receptive oral sex with a female partner13,14, and shared use of sex toys between women13,15,16. BV prevalence is high amongst women who have sex with women (WSW) with estimates ranging from 25–52%16,17,18,19,20,21. Whether increased prevalence of BV in WSW is due to sexual practices or other factors is not known.
A number of studies have found sexual activity is associated with disturbance of the vaginal microbiota22,23,24,25, however there are limited data describing how specific sexual practices influence the vaginal microbiota in WSW. Mitchell et al.26 used culture methods and found that sharing of sex toys with female partners was associated with reduced concentration of Lactobacillus, and digital vaginal sex and sex toy use was associated with increased colonization of G. vaginalis.
Understanding how specific sexual practices influence the composition of the vaginal microbiota and contribute to vaginal dysbiosis and BV is important in order to develop effective treatment and prevention strategies. The primary objective of our study was to describe the impact of sexual practices on the vaginal microbiota of a subset of women participating in a cohort of Australian WSW.
Results
Description of participants at baseline and longitudinally
Baseline characteristics and sexual practices of participants are summarised in Table 1. Specimens from 102 women were initially selected for inclusion in the study; however two were removed post quality control of sequencing data (as described below), leaving 100 women in the study population. The median age of participants at enrolment was 28 years (interquartile range[IQR] 24–37 years). Most women were Australian born (86%), had tertiary level education (81%) and had a female sexual partner (FSP) at enrolment (72%). Twenty-two percent of women reported a past history of BV.
Longitudinally, most women reported receiving oral sex from an FSP (85%) and use of sex toys with an FSP (72%). Fourteen women (14%) reported vaginal sex with a male during the study period. Forty women (40%) reported sex with a new partner in one or more interval (25 women reported one new sexual partner and 15 women two or more new partners over the study period). New partners were predominantly female; 28 women reported a female new partner/s, three women reported having a male new partner/s and nine women reported both female and male new partners.
A total of 372 specimens from 102 women underwent sequencing and 5,061,171 sequence reads were generated. Following quality control, 4,942,634 reads representing 393 ASVs remained. Nine specimens had <1000 reads and were excluded; consequently two participants were excluded from analysis as one did not have an enrolment specimen and one did not have longitudinal specimens post quality control. Thus, a total of 360 specimens from 100 women were included in analyses. This included 100 enrolment specimens and 260 longitudinal specimens, 47 of which represented incident BV. The median number of reads per specimen was 12,504 (IQR 7,460–18,344).
Vaginal community state types
Hierarchical clustering identified eight community state types (CSTs), Fig. 1. Five CSTs were characterised by Lactobacillus: CST1-L. crispatus (n = 152 specimens), CST2-Lactobacillus mixed (comprised of L. crispatus and L. iners; n = 29), and CST3-L. iners (n = 93), CST6-L. gasseri (n = 5), CST8-L. jensenii/L. fornicalis (n = 10). The remaining three CSTs were: CST4-G. vaginalis and diverse (n = 40 specimens), CST5-anaerobic and diverse (n = 28), CST7-Bifidobacterium longum (n = 3). The five most prevalent taxa identified in specimens in CST5 were BV-associated bacteria Dialister spp., Prevotella spp., G. vaginalis, L. iners and Peptoniphilus spp. For analysis purposes, the two small Lactobacillus CSTs (CST6 and CST8) were combined with CST2-Lactobacillus mixed, and CST7-B. longum was combined with other anaerobic dominated specimens in CST5-anaerobic and diverse.
The vaginal microbiota of women who have sex with women. The heatmap displays the relative abundance of the 15 most abundant bacteria detected in women in this study. Hierarchical clustering of Euclidean distances with Ward linkage was used to determine eight community state types (CST): CST1-L. crispatus, CST2-Lactobacillus mixed, and CST3-L. iners (n = 93), CST4-G. vaginalis and diverse, CST5-anaerobic and diverse, CST6-L. gasseri, CST7-Bifidobacterium longum, CST8-L. jensenii/L. fornicalis. Exposure to a new sexual partner in the preceding 90 days is indicated above the heatmap.
All women at baseline had normal (Nugent Score [NS] = 0–3, n = 92/100) or intermediate microbiota (NS = 4–6, n = 8/100) by the NS method9. Most women (n = 90) clustered into a Lactobacillus dominated CST (CST1-L. crispatus (n = 41), CST2-Lactobacillus mixed (n = 19) and CST3-L. iners (n = 30)).
Of the longitudinal specimens with normal (NS = 0–3, n = 204) and intermediate (NS = 4–6, n = 9) microbiota, most (89%) clustered to a Lactobacillus CST [CST1-L. crispatus (n = 111/213, 52%), CST2-Lactobacillus mixed (n = 24/213; 11%) and CST3-L. iners (n = 55/213; 26%)]. The majority of incident BV specimens (NS = 7–10, n = 47) clustered with CST4-G. vaginalis and diverse (n = 26/47; 55%) and CST5-anaerobic and diverse (n = 12/47; 26%).
Factors associated with vaginal microbiota diversity
In univariate analyses, sex with a new partner compared with no sex or sex in an ongoing relationship (defined as relationship for >3 months) was significantly associated with increased bacterial diversity of the vaginal microbiota (coefficient = 0.49, 95%CI: 0.30,0.68, p < 0.001; Table 2). Other characteristics associated with increased microbiota diversity included self-reported past history of BV, smoking, having two or more sexual partners in a study interval (i.e. the period of time between two specimen collections), frequent sexual activity (several times/week), receptive oral sex from any FSP and self-report of BV symptoms (abnormal vaginal odour and/or vaginal discharge; Table 2). Douching and sharing of sex toys had a borderline association with increased diversity.
We included sex with a new partner, frequency of sex, smoking, oral sex and past history of BV in a multivariable model (Table 2). Digital anal sex was not included in adjusted analyses to limit over-fitting the model. Sex with a new partner (adjusted coefficient = 0.41, 95%CI: 0.21,0.60, p < 0.001), frequent sex (adj. coefficient = 0.20, 95%CI: 0.00,0.41, p = 0.049) and past history of BV (adj. coefficient = 0.26, 95%CI: 0.04,0.48, p = 0.018) were significantly associated with increased diversity of the vaginal microbiota. Smoking and receptive oral sex with an FSP were not associated with diversity adjusted analyses.
To explore the relationship between oral sex, exposure to a new sexual partner, and microbiota diversity, we investigated 1) the impact of new partner exposure on diversity stratified by receptive oral sex, and 2) investigated the interaction between new partner exposure and receptive oral sex. Although new partner exposure was significantly associated with microbiota diversity in women reporting oral sex and not in women who did not practice oral sex (Supplementary Table 1), the 95% confidence intervals overlapped, suggesting no statistical difference in the effect of new partner by oral sex, and furthermore there was no evidence of interaction when formally tested (p = 0.110).
Factors associated with instability of the vaginal microbiota
Compositional change (instability) was measured by change of CST and Bray-Curtis dissimilarity score, calculated between consecutive longitudinal specimens.
Eighty-three women (83%) experienced at least one change of CST during the study period, accounting for 138 instances of CST change. Interestingly, changing between different Lactobacillus CSTs (n = 66/138, 48% of all CST changes) was as common as changing from a Lactobacillus CST to CST4-G. vaginalis and diverse or CST5-anaerobic and diverse (n = 50/138, 36%).
Practices significantly associated with change of CST by univariate analysis (smoking and sex with a new partner) were included in a multivariable model with CST of index specimen (i.e. the first specimen of each consecutive pair; Table 3). In the adjusted analysis, sex with a new partner (adjusted odds ratio [AOR] 2.65, 95%CI: 1.34,5.22, p = 0.005) and smoking (AOR 1.79, 95%CI: 1.03,3.11, p = 0.039) were both associated with an increased odds of change of CST when adjusted for CST of index specimen. Additionally, women with a vaginal microbiota classified as CST2-Lactobacillus mixed (AOR = 6.65, 95%CI: 2.81,15.76, p < 0.001), CST3-L. iners (AOR = 3.13, 95%CI: 1.67,5.87, p < 0.001) or CST5-anaerobic and diverse (AOR 13.18, 95%CI: 2.83,61.31, p < 0.001) were more likely to change CST in the next interval compared with women with a vaginal microbiota of CST1-L. crispatus. Having a CST4-G. vaginalis and diverse microbiota was not significantly associated with change of CST, likely because the majority of CST4 samples represented an endpoint specimen i.e. incident BV (n = 26/40, 65%).
By multinomial regression, women reporting sex with a new partner were more likely than women without a new partner to change from a Lactobacillus CST (i.e. CST1/2/3) to a non-Lactobacillus dominated CST relative to not changing CST (relative risk ratio [RRR] = 4.18, 95%CI: 2.06,8.50, p < 0.001). Smokers were more likely than non-smokers to change between Lactobacillus CSTs (RRR = 2.21, 95%CI: 1.15,4.23, p = 0.017) or change from a Lactobacillus CST to a non-Lactobacillus dominated CST (i.e. CST4/5; RRR = 2.04, 95%CI: 1.11,3.75, p = 0.021) relative to not changing CST. Figure 2 summarises changes of CST in each participant longitudinally and indicates when sex with a new partner was reported.
Longitudinal changes of community state type in women reporting sex with a new partner. Each column represents a participant and sequential longitudinal specimens are ordered from baseline to endpoint. Boxes are coloured according to community state type (CST). *Indicates a report of sex with a new partner. Most women changed CST at least once during the study. Change of CST occurred in 36/40 (90%) women who reported exposure to a new partner and 47/60 (78%) women who did not report sex with a new partner.
Practices significantly associated with instability of the vaginal microbiota (i.e. increased Bray-Curtis scores between consecutive samples) by univariate analysis were included in a multivariable model that also included CST of the index specimen (Table 4). Sex with a new partner (adj. coefficient = 0.21, 95%CI: 0.11, 0.31, p < 0.001) and smoking (adj. coefficient = 0.09, 95%CI: 0.01, 0.18, p = 0.036) were associated with increased instability of the microbiota, adjusted for index specimen CST. Additionally, having a vaginal microbiota in the index specimen of CST3-L. iners (adj. coefficient = 0.25, 95%CI: 0.15,0.34, p < 0.001), CST4-G. vaginalis and diverse (adj. coefficient = 0.24, 95%CI: 0.05,0.43, p = 0.013) or CST5-anaerobic and diverse (adj. coefficient = 0.44, 95%CI: 0.30,0.60, p < 0.001) was associated with increased instability of the vaginal microbiota longitudinally compared to a L. crispatus (CST1) vaginal microbiota.
Practices impacting the vaginal microbiota composition
After considering factors that influence stability of the microbiota, we looked at specific characteristics and sexual practices that influenced the vaginal microbiota composition by multinomial logistic regression. In univariate analyses (Supplementary Table 2), we found women who reported sex with a new partner in the previous 90 days were more likely than women reporting no sex or sex in an ongoing relationship to have a vaginal microbiota of CST4-G. vaginalis abundant and diverse (RRR = 4.09, 95%CI: 1.69,9.92, p = 0.002) or CST5-anaerobic and diverse (RRR = 5.37, 95%CI: 2.18,13.20, p < 0.001) than one of CST1. Women who reported smoking were more likely than non-smokers to have anaerobic microbiota (CST5) relative to CST1 (RRR = 3.01,95%CI: 1.31,6.92, p = 0.009). Women who reported receptive oral vaginal sex from an FSP or sharing of unwashed sex toys with an FSP were more likely to have a CST4 microbiota, and women who douched or had a past history of BV were more likely to have a CST5 microbiota (Supplementary Table 2). Women reporting recent menses (defined as onset of menses within 7 days of specimen collection) were more likely than women not reporting recent menses (>7 days from specimen collection) to have a CST2-Lactobacillus-mixed or CST3-L. iners microbiota composition relative to CST1 microbiota, but were not more likely to have a G. vaginalis (CST4) or anaerobic microbiota (CST5).
We included past history of BV, receptive oral sex from a FSP, sex with a new partner, sharing of unwashed sex toys with an FSP smoking and recent menses in a multivariable multinomial regression model (Table 5). Women reporting sex with a new partner were more likely than women reporting no sex or sex in an ongoing relationship to have a CST4-G. vaginalis and diverse (adjusted-RRR = 3.45, 95%CI: 1.42,8.41, p = 0.006) or CST5-anerobic and diverse vaginal microbiota (adjusted-RRR = 3.62, 95%CI: 1.43,9.14, p = 0.007) relative to a CST1 vaginal microbiota. Women reporting that they shared unwashed sex toys with an FSP were more likely than women not reporting this practice to have a CST4 vaginal microbiota (adjusted-RRR = 2.49, 95%CI: 1.05,5.91, p = 0.038). Women reporting smoking were more likely than non-smokers to have a CST5-anaerobic and diverse vaginal microbiota relative to a CST1 vaginal microbiota (adjusted-RRR = 2.94, 95%CI: 1.16,7.43, p = 0.023). Women with a past-history of BV were more likely to have a CST5 vaginal microbiota (adjusted-RRR = 3.18, 95%CI: 1.13,8.91, p = 0.028), and women reporting recent menses were more likely to have a CST2 (adjusted-RRR = 3.89, 95%CI: 1.58,9.50, p = 0.003) or CST3 (adjusted-RRR = 2.37, 95%CI: 1.14,4.90, p = 0.020) vaginal microbiota.
Discussion
In this longitudinal cohort study of women who have sex with women, specific sexual practices influenced the bacterial diversity, stability and composition of the vaginal microbiota. Sex with a new partner (primarily representing new FSPs) was associated with an increase in bacterial diversity and an increase in compositional change (or instability) of the vaginal microbiota, both in terms of change of CST and increased Bray-Curtis dissimilarity. Furthermore, women who reported sex with a new partner were more likely than women reporting no sex/sex in an ongoing relationship to have a vaginal microbiota characterised by BV-associated anaerobic bacteria or G. vaginalis, relative to an optimal microbiota characterised by L. crispatus. This study highlights the influence of practices on the development of a non-optimal vaginal microbiota and provides microbiological support for the sexual exchange of bacteria between women. These microbiological findings complement the previously reported epidemiological data from the original cohort13,18 which showed sex with a new partner was associated with a 2.5-fold increased risk of BV acquisition.
There is increasing evidence to support the sexual transmission of vaginal bacteria between WSW. Longitudinal studies in this population have shown that one of the greatest risk factors for BV is having a sexual partner with a history of BV, BV symptoms or microbiologically confirmed BV13,14. A recent study demonstrated that incident BV occurred at a median of 4 days post sexual activity in 93% of WSW, indicating a similar incubation period to that of other STIs27. An early study looking at the transmission dynamics of BV demonstrated that transfer of vaginal secretions between women resulted in BV in 11 of 15 women28. Furthermore, high concordance of Nugent Score categories between FSP13,15,17,18,19 and evidence that women in monogamous relationships share Lactobacillus strains29 in their vaginas supports exchange of bacteria between women during sex. In our study, women who shared unwashed sex toys and/or received oral sex from an FSP were more likely than women not reporting these practices to have an anaerobic or G. vaginalis abundant vaginal microbiota than a microbiota dominated by L. crispatus. Sexual practices are frequently highly correlated, so it is difficult to determine whether one activity has a greater impact on the vaginal microbiota than others. However, both oral sex with an FSP and sex toy use involve exchange of bodily fluids to varying degrees and therefore promote exchange of bacteria between women. Additionally, both practices have been reported as a risk factor for BV10,13,14,16. Collectively, these data suggest that female partner treatment of women with BV may be an effective strategy to improve BV cure and warrants further investigation.
Change of CST was common in our study, in accordance with previous reports that show the vaginal microbiota can be highly dynamic22,23,30. Compositional change (or instability) of the vaginal microbiota between consecutive specimens was primarily influenced by the bacteria present in the index specimen. Collectively, women with a low diversity L. crispatus dominated vaginal microbiota were more likely to have a stable microbiota longitudinally and were less likely to experience change of CST than women with a diverse microbiota or a microbiota abundant in L. iners or G. vaginalis. Our findings are consistent with one study22 that analysed the vaginal microbiota of 32 women sampled twice-weekly for 16-weeks. Gajer et al.22 reported that L. crispatus and L. gasseri dominated microbiota appeared to be stable, and that sexual activity negatively impacted stability. Interestingly, practices and microbiological characteristics associated with change of CST were highly consistent with those associated with increasing instability of the microbiota (measured by Bray-Curtis), suggesting change of CST may be a useful measure of microbiota instability31.
Smoking had a broad ranging effect on the diversity, stability and composition of the vaginal microbiota, and past studies have shown an association between smoking and BV and/or vaginal microbiota composition that was dose dependent18,32,33,34. There are a number of possible explanations for this association. Smokers have been shown to have reduced oestradiol levels compared non-smokers35, and reduced oestrogen has been associated with non-optimal Lactobacillus-deficient vaginal microbiota36. Furthermore, it is well established that nicotine has detrimental effects on the immune system, including reduced production of inflammatory cytokines and decreased functionality of neutrophils and macrophages37, and nicotine and its derivatives have been detected in the vaginal metabolome38. It is possible that modulation of immune responses may result in reduced clearance of G. vaginalis and other BV-associated bacteria (similar to what has been observed for human papillomavirus39) or prevent maintenance of an optimal Lactobacillus vaginal microbiota. The association between smoking and vaginal microbiota instability seen in our study is interesting and may be because the microbiota composition that is found more commonly in smokers (i.e. anaerobic and diverse microbiota) is inherently more unstable than others, such as those dominated by L. crispatus. It is also possible that observed associations between smoking and adverse microbiota composition and instability are due to unmeasured confounding; however, the fact that this association has been shown to be dose dependent in some studies and persists in adjusted analysis provides evidence for a biological association.
A number of other factors were associated with vaginal microbiota composition, stability and/or diversity including past history of BV, menses and douching. The finding that past history of BV was associated with both increased bacterial diversity and an anaerobic microbiota may represent persistence or re-emergence of a polymicrobial BV-biofilm40,41, or alternatively the influence of other factors such as host genetics or immune function37, diet42 or contraceptive practices43. Both douching and menses have been shown in a number of studies to adversely alter vaginal microbiota composition and stability22,44,45, and consistent with this, we found that douching was associated with anaerobic and diverse vaginal microbiota and had a borderline adverse effect on microbiota stability in univariate analyses. While recent menses did not have an effect on microbiota diversity or stability in our study, it did influence microbiota composition. Women were more likely to have a vaginal microbiota abundant in L. iners (i.e. CST2 or CST3) if their specimen was collected within seven days of onset of menses, consistent with data that shows L. iners grows best on media containing blood46,47.
Hormonal contraception may have a beneficial impact on the vaginal microbiota48. However, we found no association between hormonal contraception and microbiota diversity, stability or composition, which may be because only a small number of women reported hormonal contraceptive use in the parent cohort.
There are a number of limitations to this study. The study population comprised highly educated women who were predominately Australian born and reported Australian or English ethnicity, which may limit the generalizability of our findings. Specimens were collected every three months which limited our ability to assess immediate effect of sexual practices behaviours on the vaginal microbiota and any short-term fluctuations in microbiota composition. Specimens included in the analysis were not selected randomly or from specified study time points which may have biased results. We did not include negative controls alongside specimens during sequencing, however we removed contaminants previously identified using the same extraction methodology, primer set up and sequencing instrument49 and the microbiota profiles are consistent with those previously published6,25,50. Finally, this study did not assess practices or the vaginal microbiota of the sexual partner/s of participants so we cannot definitively prove sexual transmission of BV-associated bacteria is occurring between women. Nevertheless, the microbiota data presented here is consistent with epidemiological data that supports sexual transmission of BV in WSW13,14.
This study shows that sex with a new partner is associated with changes in the vaginal microbiota of WSW, including increased diversity and increased abundance of bacteria commonly associated with a non-optimal vaginal microbiota. These findings suggest that sexual exchange of bacteria, including BV-associated bacteria, occurs between female sexual partners, and highlight the influence of specific practices on the development of a non-optimal vaginal microbiota. These data are important for informing strategies to promote a vaginal microbiota that is associated with optimal reproductive health, as well as new approaches to improve BV cure such as female partner treatment.
Methods
Participant and specimen selection
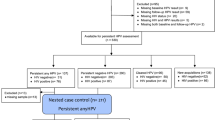
Participants were selected from the Women On Women’s (WOW) Health study, a two-year cohort of 298 WSW designed to examine epidemiological and microbiological factors associated with incident BV13,18. Women reported a FSP within 18 months prior to enrolment and were BV negative (NS < 79) on three consecutive baseline vaginal smears collected one week apart. Women self-collected a vaginal swab and smear, and completed a detailed questionnaire every three months until study endpoint (diagnosis of incident BV [NS = 7–10] or 24 months without BV). Women were instructed to avoid specimen collection on the heaviest days of their menstrual cycle13.
For the microbiota sub-study, we included all women who developed incident BV (n = 51) and an equal number of women who did not (initially controls were over-selected using a random sort command in Stata/IC (v14.2, StataCorp LP, College Station, USA)). Seven of the 51 women to develop incident BV co-enrolled in the original cohort with their FSP13. As such, controls were then frequency matched on co-enrolment status and age to ensure a similar distribution of both variables (for example, the last non co-enrolled control was replaced with the next randomly selected co-enrolled control). Each woman contributed a baseline specimen and an endpoint specimen (BV-specimen from women with incident BV or the 24 month specimen from women without BV). Up to three interim specimens were included for each woman (typically the last two specimens collected prior to the endpoint specimen). If a specimen could not be used/located, an earlier specimen from that participant was used.
Ethical approval was obtained from the Human Research Ethics Committees of Alfred Hospital, Melbourne, Australia and the University of Melbourne. All research was performed in accordance with the National Statement on Ethical Conduct in Human Research. Informed written consent was obtained from all participants for the use of their specimens in the current study.
Laboratory methods
Swabs were agitated in 1 mL RNAlater (Thermo Fisher Scientific, Waltham, USA) and stored at −80 °C prior to DNA extraction using the MagNA Pure 96 instrument and the DNA and Viral NA small volume kit (Roche Diagnostics, Mannheim, Germany). Dual index primers 341 F/805 R with heterogeneity spacers51,52,53 were used for PCR amplification of the V3-V4 hypervariable regions of the 16S rRNA gene. Libraries were sequenced by Micromon Genomics (Micromon, Monash University, Victoria, Australia) on the MiSeq platform (Illumina, San Diego, CA, USA). Sequence reads are available in the NCBI Sequence Read Archive under Bioproject PRJNA434520.
Sequence data analysis
Barcodes were extracted using QIIME v1.9.054 and demultiplexing was performed using idemp (https://github.com/yhwu/idemp). Primers and heterogeneity spacers were removed using TagCleaner standalone version 0.1655. Reads were processed using DADA2 v1.6.056. Reads were truncated based on quality profiles (at 250 bases for read 1 and 220 bases for read 2) and were discarded if they had ambiguous bases or exceeded the number of expected errors based on quality scores. Chimeras were identified and removed. Taxonomy was assigned using the default RDP Classifier implemented in DADA2 and the Silva reference database (v128)57. Species level assignment was performed using exact matching in the DADA2 package and taxonomy for Lactobacillus spp. was confirmed by a BLAST search against a database of 16S rRNA gene sequences from 158 type strains. Not all ASVs were able to be assigned to species level.
BV-associated bacteria (BVAB)−1 has previously been misclassified as Shuttleworthia58 and BVAB3 is named as Fastidiosiplia in the Silva database59. We aligned Shuttleworthia and Fastidiosiplia ASVs against BVAB1 (NCBI GenBank AY724739.1), BVAB2 (AY724740.1) and BVAB3 (AY724741.1) using Clustal Omega (EMBL-EBI)60,61. Shuttleworthia ASV had 100% identity to BVAB1. Two Fastidiosiplia ASVs had high identity to BVAB2 (99.50 and 100% identity, respectively), and a third Fastidiosiplia ASV had 100% identity to BVAB3. The ASVs were reclassified accordingly.
ASVs were removed if they had a total abundance of less than 0.001% or were present in only one specimen. The ASV table was screened for contaminants previously identified in negative controls49, as well as common sequencing contaminants (removed ASVs belonging to Facklamia and Shewanella genera and Halomonadaceae family)62,63. Specimens with fewer than 1000 reads were excluded from analysis. Participants were excluded if they did not have an enrolment specimen or did not have any follow-up specimens.
Diversity metrics and CST were generated using the Vegan package64 and R Studio [V 1.1.419, Boston, USA] employing R v3.4.3. Alpha diversity was calculated using the Shannon Diversity Index using ASV data. ASVs assigned to the same taxonomy were merged and the relative abundance of each taxon was used for CST identification. Hierarchical clustering of Euclidean distances with Ward linkage was performed on the relative abundance of each taxon and a scree plot of within cluster distances was used to inform the number of CSTs. Bray-Curtis dissimilarity scores were calculated between consecutive paired specimens from each participant. The heatmap was generated using the ComplexHeatmap package65 and the same metrics used to identify CSTs. Change of CST was defined as change or no change in CST between consecutive paired specimens.
Statistical analysis
Statistical models that accounted for repeated measures within individuals were fitted using generalised estimating equations (GEE) to investigate the impact of characteristics and practices on the diversity (Shannon-Diversity Index) and instability (change of CST or Bray-Curtis dissimilarity) of the vaginal microbiota. GEE linear regression analyses were used when the outcome was Shannon-Diversity Index or Bray-Curtis dissimilarity, with the regression coefficient representing the mean difference of each outcome between the reference and comparison group/s for each characteristic/practice investigated. GEE logistic regression was used when change of CST was the outcome. Characteristics and practices deemed significant in univariate analyses (p < 0.05) were included in multivariable analyses.
We also analysed the type of CST change observed. Specimens were allocated one of four change type between sequential specimens: (1) no change; (2) change from one Lactobacillus CST to another Lactobacillus CST; (3) change from one Lactobacillus CST to a non-Lactobacillus CST; or (4) change from a non-Lactobacillus CST to any other CST. Multinomial regression was used to investigate the relationship between practices and type of CST change relative to the risk of no change, generating relative risk ratios and 95% confidence intervals.
Multinomial regression was also used to assess associations between characteristics and microbiota composition (i.e. CST-classification of a sample). CST1-L. crispatus was the reference group for all analyses. This analysis calculated the risk of having a vaginal microbiota of a specific CST (details of CSTs provided in results below) compared to the risk of a vaginal microbiota of CST1, clustering for multiple samples from individual participants.
Characteristics and practices deemed significant in univariate analyses (p < 0.05) were included in multivariable analyses. Statistical analyses were performed using STATA v14.2, unless otherwise specified.
Data availability
The raw sequencing data are publicly available in the NCBI Sequence Read Archive (SRA) under the Bioproject number PRJNA434520.
References
Cohen, C. R. et al. Bacterial vaginosis associated with increased risk of female-to-male HIV-1 transmission: a prospective cohort analysis among African couples. PLoS Med 9, e1001251, https://doi.org/10.1371/journal.pmed.1001251 (2012).
Koumans, E. H., Markowitz, L. E., Berman, S. M. & St Louis, M. E. A public health approach to adverse outcomes of pregnancy associated with bacterial vaginosis. Int J Gynaecol Obstet 67(Suppl 1), S29–33 (1999).
Myer, L., Kuhn, L., Stein, Z. A., Wright, T. C. Jr. & Denny, L. Intravaginal practices, bacterial vaginosis, and women’s susceptibility to HIV infection: epidemiological evidence and biological mechanisms. Lancet Infect Dis 5, 786–794, https://doi.org/10.1016/S1473-3099(05)70298-X (2005).
Brotman, R. M. et al. Bacterial vaginosis assessed by Gram stain and diminished colonization resistance to incident gonococcal, chlamydial, and trichomonal genital infection. J Infect Dis 202, 1907–1915, https://doi.org/10.1086/657320 (2010).
Fredricks, D. N., Fiedler, T. L. & Marrazzo, J. M. Molecular identification of bacteria associated with bacterial vaginosis. N Engl J Med 353, 1899–1911, https://doi.org/10.1056/NEJMoa043802 (2005).
Ravel, J. et al. Vaginal microbiome of reproductive-age women. Proc Natl Acad Sci USA 108(Suppl 1), 4680–4687, https://doi.org/10.1073/pnas.1002611107 (2011).
Verhelst, R. et al. Comparison between Gram stain and culture for the characterization of vaginal microflora: definition of a distinct grade that resembles grade I microflora and revised categorization of grade I microflora. BMC Microbiol 5, 61, https://doi.org/10.1186/1471-2180-5-61 (2005).
Srinivasan, S. et al. Bacterial communities in women with bacterial vaginosis: high resolution phylogenetic analyses reveal relationships of microbiota to clinical criteria. PLoS One 7, e37818, https://doi.org/10.1371/journal.pone.0037818 (2012).
Nugent, R. P., Krohn, M. A. & Hillier, S. L. Reliability of diagnosing bacterial vaginosis is improved by a standardized method of Gram stain interpretation. J Clin Microbiol 29, 297–301 (1991).
Fethers, K. A., Fairley, C. K., Hocking, J. S., Gurrin, L. C. & Bradshaw, C. S. Sexual risk factors and bacterial vaginosis: a systematic review and meta-analysis. Clin Infect Dis 47, 1426–1435, https://doi.org/10.1086/592974 (2008).
Fethers, K. A. et al. Early sexual experiences and risk factors for bacterial vaginosis. J Infect Dis 200, 1662–1670, https://doi.org/10.1086/648092 (2009).
Cherpes, T. L., Hillier, S. L., Meyn, L. A., Busch, J. L. & Krohn, M. A. A delicate balance: risk factors for acquisition of bacterial vaginosis include sexual activity, absence of hydrogen peroxide-producing lactobacilli, black race, and positive herpes simplex virus type 2 serology. Sex Transm Dis 35, 78–83, https://doi.org/10.1097/OLQ.0b013e318156a5d0 (2008).
Vodstrcil, L. A. et al. Incident bacterial vaginosis (BV) in women who have sex with women is associated with behaviors that suggest sexual transmission of BV. Clin Infect Dis 60, 1042–1053, https://doi.org/10.1093/cid/ciu1130 (2015).
Marrazzo, J. M., Thomas, K. K., Fiedler, T. L., Ringwood, K. & Fredricks, D. N. Risks for acquisition of bacterial vaginosis among women who report sex with women: a cohort study. PLoS One 5, e11139, https://doi.org/10.1371/journal.pone.0011139 (2010).
Marrazzo, J. M. et al. Characterization of vaginal flora and bacterial vaginosis in women who have sex with women. J Infect Dis 185, 1307–1313, https://doi.org/10.1086/339884 (2002).
Marrazzo, J. M., Thomas, K. K., Agnew, K. & Ringwood, K. Prevalence and risks for bacterial vaginosis in women who have sex with women. Sex Transm Dis 37, 335–339 (2010).
Evans, A. L., Scally, A. J., Wellard, S. J. & Wilson, J. D. Prevalence of bacterial vaginosis in lesbians and heterosexual women in a community setting. Sex Transm Infect 83, 470–475, https://doi.org/10.1136/sti.2006.022277 (2007).
Bradshaw, C. S. et al. The influence of behaviors and relationships on the vaginal microbiota of women and their female partners: the WOW Health Study. J Infect Dis 209, 1562–1572, https://doi.org/10.1093/infdis/jit664 (2014).
Berger, B. J. et al. Bacterial vaginosis in lesbians: a sexually transmitted disease. Clin Infect Dis 21, 1402–1405 (1995).
Bailey, J. V., Farquhar, C. & Owen, C. Bacterial vaginosis in lesbians and bisexual women. Sex Transm Dis 31, 691–694 (2004).
McCaffrey, M., Varney, P., Evans, B. & Taylor-Robinson, D. Bacterial vaginosis in lesbians: evidence for lack of sexual transmission. Int. J. STD. AIDS. 10, 305–308 (1999).
Gajer, P. et al. Temporal dynamics of the human vaginal microbiota. Sci Transl Med 4, 132ra152, https://doi.org/10.1126/scitranslmed.3003605 (2012).
Schwebke, J. R., Richey, C. M. & Weiss, H. L. Correlation of behaviors with microbiological changes in vaginal flora. J Infect Dis 180, 1632–1636, https://doi.org/10.1086/315065 (1999).
Pepin, J. et al. The complex vaginal flora of West African women with bacterial vaginosis. PLoS One 6, e25082, https://doi.org/10.1371/journal.pone.0025082 (2011).
Vodstrcil, L. A. et al. The influence of sexual activity on the vaginal microbiota and Gardnerella vaginalis clade diversity in young women. PLoS One 12, e0171856, https://doi.org/10.1371/journal.pone.0171856 (2017).
Mitchell, C., Manhart, L. E., Thomas, K. K., Agnew, K. & Marrazzo, J. M. Effect of sexual activity on vaginal colonization with hydrogen peroxide-producing lactobacilli and Gardnerella vaginalis. Sex Transm Dis 38, 1137–1144, https://doi.org/10.1097/OLQ.0b013e31822e6121 (2011).
Muzny, C. A., Lensing, S. Y., Aaron, K. J. & Schwebke, J. R. Incubation period and risk factors support sexual transmission of bacterial vaginosis in women who have sex with women. Sex Transm Infect 0, 1–5, https://doi.org/10.1136/sextrans-2018-053824 (2019).
Gardner, H. L. & Dukes, C. D. Haemophilus vaginalis vaginitis: a newly defined specific infection previously classified non-specific vaginitis. Am J Obstet Gynecol 69, 962–976 (1955).
Marrazzo, J. M., Antonio, M., Agnew, K. & Hillier, S. L. Distribution of genital Lactobacillus strains shared by female sex partners. J Infect Dis 199, 680–683, https://doi.org/10.1086/596632 (2009).
Srinivasan, S. et al. Temporal variability of human vaginal bacteria and relationship with bacterial vaginosis. PLoS One 5, e10197, https://doi.org/10.1371/journal.pone.0010197 (2010).
Brooks, J. P. et al. Changes in vaginal community state types reflect major shifts in the microbiome. Microb Ecol Health Dis 28, 1303265, https://doi.org/10.1080/16512235.2017.1303265 (2017).
Brotman, R. M. et al. Association between cigarette smoking and the vaginal microbiota: a pilot study. BMC Infect Dis 14, 471, https://doi.org/10.1186/1471-2334-14-471 (2014).
Mehta, S. D. et al. The vaginal microbiota over an 8- to 10-year period in a cohort of HIV-infected and HIV-uninfected women. PLoS One 10, e0116894, https://doi.org/10.1371/journal.pone.0116894 (2015).
Hellberg, D., Nilsson, S. & Mardh, P. A. Bacterial vaginosis and smoking. International journal of STD & AIDS 11, 603–606, https://doi.org/10.1258/0956462001916461 (2000).
Westhoff, C., Gentile, G., Lee, J., Zacur, H. & Helbig, D. Predictors of ovarian steroid secretion in reproductive-age women. Am. J. Epidemiol. 144, 381–388 (1996).
Miller, E. A., Beasley, D. E., Dunn, R. R. & Archie, E. A. Lactobacilli Dominance and Vaginal pH: Why Is the Human Vaginal Microbiome Unique? Front Microbiol 7, 1936, https://doi.org/10.3389/fmicb.2016.01936 (2016).
Murphy, K. & Mitchell, C. M. The Interplay of Host Immunity, Environment and the Risk of Bacterial Vaginosis and Associated Reproductive Health Outcomes. J Infect Dis 214(Suppl 1), S29–35, https://doi.org/10.1093/infdis/jiw140 (2016).
Nelson, T. M. et al. Cigarette smoking is associated with an altered vaginal tract metabolomic profile. Sci Rep 8, 852, https://doi.org/10.1038/s41598-017-14943-3 (2018).
Giuliano, A. R. et al. Clearance of oncogenic human papillomavirus (HPV) infection: effect of smoking (United States). Cancer Causes Control 13, 839–846, https://doi.org/10.1023/a:1020668232219 (2002).
Machado, A. & Cerca, N. Influence of biofilm formation by Gardnerella vaginalis and other anaerobes on bacterial vaginosis. J Infect Dis 212, 1856–1861, https://doi.org/10.1093/infdis/jiv338 (2015).
Swidsinski, A. et al. Adherent biofilms in bacterial vaginosis. Obstet Gynecol 106, 1013–1023, https://doi.org/10.1097/01.AOG.0000183594.45524.d2 (2005).
Tuddenham, S. et al. Associations between dietary micronutrient intake and molecular-Bacterial Vaginosis. Reprod Health 16, 151, https://doi.org/10.1186/s12978-019-0814-6 (2019).
Joesoef, M. R. et al. High rate of bacterial vaginosis among women with intrauterine devices in Manado, Indonesia. Contraception 64, 169–172, https://doi.org/10.1016/s0010-7824(01)00246-3 (2001).
Brotman, R. M. et al. The effect of vaginal douching cessation on bacterial vaginosis: a pilot study. Am J Obstet Gynecol 198, 628 e621–627, https://doi.org/10.1016/j.ajog.2007.11.043 (2008).
van der Veer, C. et al. Effects of an over-the-counter lactic-acid containing intra-vaginal douching product on the vaginal microbiota. BMC Microbiol 19, 168, https://doi.org/10.1186/s12866-019-1545-0 (2019).
Srinivasan, S. et al. More Easily Cultivated Than Identified: Classical Isolation With Molecular Identification of Vaginal Bacteria. J Infect Dis 214(Suppl 1), S21–28, https://doi.org/10.1093/infdis/jiw192 (2016).
Falsen, E., Pascual, C., Sjoden, B., Ohlen, M. & Collins, M. D. Phenotypic and phylogenetic characterization of a novel Lactobacillus species from human sources: description of Lactobacillus iners sp. nov. Int J Syst Bacteriol 49(Pt 1), 217–221, https://doi.org/10.1099/00207713-49-1-217 (1999).
Brooks, J. P. et al. Effects of combined oral contraceptives, depot medroxyprogesterone acetate and the levonorgestrel-releasing intrauterine system on the vaginal microbiome. Contraception 95, 405–413, https://doi.org/10.1016/j.contraception.2016.11.006 (2017).
Plummer, E. L. et al. Combined oral and topical antimicrobial therapy for male partners of women with bacterial vaginosis: Acceptability, tolerability and impact on the genital microbiota of couples - A pilot study. PLoS One 13, e0190199, https://doi.org/10.1371/journal.pone.0190199 (2018).
Chaban, B. et al. Characterization of the vaginal microbiota of healthy Canadian women through the menstrual cycle. Microbiome 2, 23, https://doi.org/10.1186/2049-2618-2-23 (2014).
Fadrosh, D. W. et al. An improved dual-indexing approach for multiplexed 16S rRNA gene sequencing on the Illumina MiSeq platform. Microbiome 2, 6, https://doi.org/10.1186/2049-2618-2-6 (2014).
Shipitsyna, E. et al. Composition of the vaginal microbiota in women of reproductive age - sensitive and specific molecular diagnosis of bacterial vaginosis is possible? PLoS One 8, e60670 (2013).
Sinclair, L., Osman, O. A., Bertilsson, S. & Eiler, A. Microbial community composition and diversity via 16S rRNA gene amplicons: evaluating the illumina platform. PLoS One 10, e0116955, https://doi.org/10.1371/journal.pone.0116955 (2015).
Caporaso, J. G. et al. QIIME allows analysis of high-throughput community sequencing data. Nat Methods 7, 335–336, https://doi.org/10.1038/nmeth.f.303 (2010).
Schmieder, R., Lim, Y. W., Rohwer, F. & Edwards, R. TagCleaner: Identification and removal of tag sequences from genomic and metagenomic datasets. BMC Bioinformatics 11, 341, https://doi.org/10.1186/1471-2105-11-341 (2010).
Callahan, B. J. et al. DADA2: High-resolution sample inference from Illumina amplicon data. Nat Methods 13, 581–583, https://doi.org/10.1038/nmeth.3869 (2016).
Quast, C. et al. The SILVA ribosomal RNA gene database project: improved data processing and web-based tools. Nucleic Acids Res 41, D590–596, https://doi.org/10.1093/nar/gks1219 (2013).
Oakley, B. B., Fiedler, T. L., Marrazzo, J. M. & Fredricks, D. N. Diversity of human vaginal bacterial communities and associations with clinically defined bacterial vaginosis. Appl Environ Microbiol 74, 4898–4909, https://doi.org/10.1128/AEM.02884-07 (2008).
Van Der Pol, W. J. et al. In Silico and Experimental Evaluation of Primer Sets for Species-Level Resolution of the Vaginal Microbiota Using 16S Ribosomal RNA Gene Sequencing. J Infect Dis 219, 305–314, https://doi.org/10.1093/infdis/jiy508 (2019).
Sievers, F. et al. Fast, scalable generation of high-quality protein multiple sequence alignments using Clustal Omega. Mol Syst Biol 7, 539, https://doi.org/10.1038/msb.2011.75 (2011).
Chojnacki, S., Cowley, A., Lee, J., Foix, A. & Lopez, R. Programmatic access to bioinformatics tools from EMBL-EBI update: 2017. Nucleic Acids Res 45, W550–W553, https://doi.org/10.1093/nar/gkx273 (2017).
Jervis-Bardy, J. et al. Deriving accurate microbiota profiles from human samples with low bacterial content through post-sequencing processing of Illumina MiSeq data. Microbiome 3, 19, https://doi.org/10.1186/s40168-015-0083-8 (2015).
Salter, S. J. et al. Reagent and laboratory contamination can critically impact sequence-based microbiome analyses. BMC Biol 12, 87, https://doi.org/10.1186/s12915-014-0087-z (2014).
vegan: Community Ecology Package v. R package version 2.4-1 (2016).
Gu, Z., Eils, R. & Schlesner, M. Complex heatmaps reveal patterns and correlations in multidimensional genomic data. Bioinformatics 32, 2847–2849, https://doi.org/10.1093/bioinformatics/btw313 (2016).
Acknowledgements
This work was supported by The Australian National Health and Medical Research Council Project Grant (1020457) awarded to CSB and the Australian National Health and Medical Research Council Program (1071269) awarded to S.M.G., C.K.F. and M.G.L. E.L.P. was supported by an Australian Government Research Training Program (RTP) Scholarship. The authors thank Glenda Fehler, Susan Peterson, Dr. Marcus Chen, Dr. Sandra Walker, Dr. Jade Bilardi, and Clare Bellhouse for their contributions to the original WOW Cohort study, from which this microbiota sub-study arose. The authors thank Dr. Jimmy Twin for contributions to the laboratory work.
Author information
Authors and Affiliations
Contributions
C.S.B., L.A.V., S.N.T., C.K.F. and J.S.H. conceived and designed the study. C.S.B., C.K.F., L.A.V., M.G.L., K.A.F. and J.S.H. contributed to the original cohort study from which this microbiota analysis arose. SNT oversaw the laboratory work. E.L.P. and L.A.V. analysed the data, with statistical support from M.G.L., J.S.H. and C.S.B. L.A.V., S.M.G., C.K.F., D.M.B., S.N.T., G.L.M. and C.S.B. provided additional supervision and oversight. C.S.B., S.N.T., J.S.H., C.K.F., S.M.G. and M.G.L. acquired funding. E.L.P., L.A.V., G.L.M. and C.S.B. wrote the original draft. All authors critically revised the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Plummer, E.L., Vodstrcil, L.A., Fairley, C.K. et al. Sexual practices have a significant impact on the vaginal microbiota of women who have sex with women. Sci Rep 9, 19749 (2019). https://doi.org/10.1038/s41598-019-55929-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-55929-7
This article is cited by
-
Cysteine dependence of Lactobacillus iners is a potential therapeutic target for vaginal microbiota modulation
Nature Microbiology (2022)
-
Bacterial vaginosis: drivers of recurrence and challenges and opportunities in partner treatment
BMC Medicine (2021)
-
Vaginal microbiota and the potential of Lactobacillus derivatives in maintaining vaginal health
Microbial Cell Factories (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.