Abstract
Orthokeratology (Ortho-K) works to reshape cornea and is the only non-surgical way to enable vision without corrective aids. However, its effect is only temporary, and successful stabilization requires ongoing Ortho-K wear to maintain the reshaping effect. Corneal crosslinking (CXL) is a commonly-used technique in clinical practice to stabilize corneal shape in keratoconic eyes. However, whether or not CXL can stabilize corneal shape after Ortho-K in normal cornea has not been reported. Therefore, this proof-of-concept study using 2 rhesus monkeys aimed to determine the efficacy of the combined procedure. One monkey wore Ortho-K bilaterally for 24 hours, and the other from 6 pm to 8 am for 7 days. The left eyes of both monkeys underwent CXL after Ortho-K while the contralateral eye served as control. Results showed a gradual regression of corneal shape in all eyes with or without CXL. However, eyes underwent CXL regressed more slowly than the control eyes. The control eyes and the CXL treatment eye in the 7-day Ortho-K monkey regressed completely at last, while the CXL treatment eye in the 24 h Ortho-K monkey maintained a corneal flattening of −1.48 D 27 days after procedure. These findings suggest CXL can slow the regression of Ortho-K for a short duration, but cannot sustain its effect according to the current protocol.
Similar content being viewed by others
Introduction
As a non-surgical vision correction and with the potential to reduce myopia progression1, Orthokeratology (Ortho-K) has received much attention in the past decades. Correction of myopia is achieved as Ortho-K thins and functionally flattens the central cornea of the wearer during sleeping. However, the effect is only temporary, thus successful stabilization requires ongoing Ortho-K wear to maintain the reshaping effect, which comes at an inconvenience and cost for users.
Corneal crosslinking (CXL) is a clinical procedure designed to slow down or halt the progression of keratoconus. While the precise mechanism is yet to be elucidated, the molecular mechanisms accounting for the corneal change may be attributable to the cross-linking of collagen fibrils through the photochemical reaction between ultraviolet A (UVA) light and photosensitizers2. Previous studies have shown a significant increase of up to 70–300% in corneal rigidity after CXL3,4, suggesting the potential of CXL to stabilize corneal shape. Though originally proposed as a treatment for keratoconus, the use of CXL has been recently extended in LASIK surgery. With proven evidence that CXL is able to achieve improved stabilization of corneal refraction after refractive surgeries5,6, its potential as a promising auxiliary treatment to stiffen corneal shape has invited much attention.
Ortho-K is able to reshape the cornea to successfully correct myopia, thus whether or not CXL is able to sustain its reshaping effect and maintain the correction of refractive errors in patients after Ortho-K is of substantial clinical value to investigate into. There have been efforts to apply this combined therapy in keratoconus patients7,8. Results showed that the visual acuity of keratoconus patients improved after this combined therapy, but no effects of corneal stabilization were observed. However, the abnormality of collagen structure and loss of collagen fibrils in keratoconus may have weakened the efficacy of both Ortho-K and CXL9. As the effect of this combined procedure remains unknown in normal corneas, in this proof-of-concept study we aimed to investigate whether CXL can stabilize corneal shape molded by Ortho-K lenses in normal cornea using rhesus monkeys.
Results
Slit lamp microscopy
Given the fact that the shapes of both eyes in our monkeys were not identical, optimal lenses were selected for each eye with only slight differences in fitting curve parameters. The Ortho-K lenses were well-fitted and well-tolerated by both monkeys. No epithelial fluorescein staining was observed after the removal of Ortho-K lenses in either eye of both monkeys. Corneal epithelial defects in the CXL treatment eyes were healed by the fifth day post CXL procedure. Mild to moderate corneal edema or stromal haze gradually improved after corneal epithelial healing and completely recovered 10 days following the procedure.
Corneal topography and refractive power change
The corneal tangential maps and corresponding subtractive maps of the 2 monkeys are presented in Figs. 1 and 2. Their corresponding value of change in mean keratometry within the reshape zone was shown in Fig. 3. In Monkey A that wore Ortho-K lens for 24 h, despite the small central reshape zone due to this short duration of lens wear, the right eye (control eye) achieved a mean keratometry change of −1.13 D within an irregular shape zone of 3.84 mm2 (length × width, 3.53 × 1.86 mm), versus −2.16 D within a nearly-circular zone of 3.16 mm2 (length × width, 2.00 × 2.04 mm) in the left eye (treatment eye). Corneal flattening was more obvious in Monkey B with overnight Ortho-K lens wear for 7 days, with a mean keratometry change of −3.48 D achieved in the right eye (control eye) within a round reshape zone of 9.27 mm2, versus −2.45 D within a round reshape zone of 6.87 mm2 in the left eye (treatment eye).
Tangential and subtractive maps of the control and crosslinking (CXL) eye from monkey A wearing Ortho-K lens for 24 h. Picture A–F2 are profiles for the control eye while picture a-g2 are profiles for the CXL eye. Picture (A),(a) are the baseline tangential maps of the control and treatment eye, respectively. Picture B1 and b1 are tangential maps after wearing Ortho-K lens for 24 h. Picture C1–F1 show corneal shape at 5 days, 8 days, 13 days and 19 days after lens removal while c1-g1 show corneal shape at 5 days, 8 days, 13 days, 19 days and 27 days after CXL. Picture B2–F2 and b2–g2 are corresponding tangential subtractive maps compared to their baseline (B2 was generated from B1 minus A and b2 was generated from b1 minus a, etc.), representing curvature change at each visit relative to original shape. Warm colors (red) indicate corneal steepening while cold colors (blue) indicate flattening in subtractive maps. Central corneal flattening was achieved in both eyes after wearing Ortho-K lenses (B2 and b2), followed by gradual regression (C2–F2 and c2–g2). The control eye regressed completely by 8 days (D2), while the CXL eye maintained a −1.48 D of corneal flattening at 27 days post-operatively (g2).
Tangential and subtractive maps of the control and crosslinking (CXL) eye from monkey B wearing Ortho-K lens for 7 day. Picture A–E2 are profiles for the control eye while picture a–e2 are profiles for the CXL eye. Picture (A),(a) are the baseline tangential maps of the control and treatment eye, respectively. Picture B1 and b1 are tangential maps after wearing Ortho-K lens for 7 days. Picture C1–E1 show corneal shape at 6 days, 14 days and 25 days after lens removal while c1–e1 show corneal shape at 6 days, 14 days and 25 days after CXL. Picture B2–E2 and b2–e2 are corresponding tangential subtractive maps compared to their baseline (B2 was generated from B1 minus A and b2 was generated from b1 minus a, etc.), representing curvature change at each visit relative to original shape. Warm colors (red) indicate corneal steepening while cold colors (blue) indicate flattening in subtractive maps. Central corneal flattening was achieved in both eyes after wearing Ortho-K lenses (B2 and b2), followed by gradual regression (C2–E2 and c2–e2). The control eye regressed completely by 6 days (C2), while the CXL eye regressed completely by 14 days post-operatively (d2).
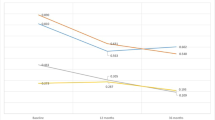
Mean keratometry changes of treatment zone in monkey A wearing Ortho-K lens for 24 h (top) and monkey B wearing Ortho-K lens for 7 days (bottom). The line chart shows the change of mean keratometry values (D) at each visit while the bar charts presents the difference of keratometry (D) at each visit compared to the baseline level. Reference line: y = 0 and y = −0.5. For monkey A, keratometry change in the control eye was less than −0.5 D at 8 days after lens removal, while the CXL eye maintained a −1.48 D of corneal flattening at 27 days post-operatively. For monkey B, keratometry change in the control eye was less than −0.5 D at 6 days after lens removal, while the CXL eye regressed completely at 10 days after post-operatively.
In Monkey A, regressions of corneal shape were observed in both CXL treatment and control eyes. By day 8, the control eye regressed to its original shape (mean keratometry change of −0.07 D compared to baseline in the reshape zone), while the central corneal area in the CXL treatment eye remained flat (mean change of −1.01 D in the reshape zone). At day 27, a change of −1.48 D of corneal flattening still remained in the treatment eye relative to its baseline status.
In Monkey B, the control eye had completely regressed to baseline level (mean change of −0.17 D in the reshape zone) by day 6, whereas the effect of central flattening in CXL treatment eye still remained (mean change of −1.28 D in the reshape zone) till day 14 when it returned to baseline shape (mean change of 0.21 D in the reshape zone).
The mean keratometry of reshape zone and the difference between follow-up and baseline for two monkeys are presented in detail in Fig. 3. After Ortho-K wear an abrupt decrease in corneal curvature of reshape zone occurred, followed by a gradual regression in all eyes. Eight days post CXL procedure in Monkey A, the mean keratometry of the control eye returned to baseline level, while that of CXL treatment eye decreased. In Monkey B, both eyes regressed to baseline level on day 10 post procedure, with a slower pace in the CXL treatment eye than the control eye.
Refraction
Figure 4 displays the retinoscopy refraction change in the two monkeys. No clinically significant refraction change was observed in Monkey A (left) while Monkey B displayed a hyperopic change of 3–3.75 D (right) as a result of corneal flattening. The refraction change was similar in the CXL treatment and control eyes during the regression phase.
Spherical equivalent (SE) changes before and post operation. The left one portrays the SE changes (D) in monkey A (24 h lens wear), while the right one shows the SE changes (D) in monkey B (7-day lens wear). Refraction change between control and corsslinking (CXL) eye showed similar trend within the same monkey.
Discussion
Our study demonstrates that the current standard CXL technique may slow the regression of corneal shape molded by Ortho-K in normal corneas in rhesus monkeys, however it appears that CXL cannot stabilize the Ortho-K effect longer than one month.
The combined therapy of Ortho-K and CXL has already been applied in some previous studies, but not for myopia treatment. In clinical experiments for keratoconus patients wearing Ortho-K lenses, only temporary effects of corneal flattening were observed following CXL10,11. It is difficult to draw direct comparisons of Ortho-K efficacy in keratoconic and non-keratoconic eyes due to the differences in stromal structure. Our study was supported by the contralateral eye as a control, and it showed that the standard CXL procedure failed to stabilize the corneal shape molded by Ortho-K in normal cornea. While residual corneal flattening in the treated eye with 24 h of Ortho-K lens wear was observed, the associated refraction changes warrants further validation in more samples.
We hypothesize that the failure of CXL to stabilize the corneal reshape effect by Ortho-K may be attributable to several possible reasons. Firstly, although it is yet conclusive that the effect of Ortho-K is mainly attributable to the corneal epithelial re-distribution12,13,14, other studies suggested the changes of corneal posterior surface flattening15, stromal thinning16 and shorter anterior chamber depth after Ortho-K17. On the other hand, one study suggested that CXL might bring about structural changes in the stroma but these changes were mainly on the anterior 200 μm thick portion18. This might also explain the insufficient stabilization effect of CXL.
Another possible explanation for this negative result is related to the intensity of crosslinking. In our experiment, we followed the most commonly used protocol of CXL for the treatment of keratoconus19. However, the effect of CXL is associated with total absorbed radiant exposure, concentration distribution, and treatment time20,21. Though the Dresden protocol is currently the most effective way to conduct UV-A mediated CXL, issues regarding efficacy, such as pulsing versus continuous wave light, accelerated versus conventional CXL, are still in debate. Besides, other novel CXL techniques including riboflavin concentration-controlled method which is more theoretically efficient than the Dresden protocol22, the rose bengal-green light CXL which was proved to have a sgreater density of CXL than UV-A CXL23, and the novel femtosecond laser CXL to correct vision24, have been investigated and developed. In light of this, the intensity of CXL in our study may fall short of adequacy, but with the potential to be improved to create long-term corneal changes. However, it must be noted that methods to strengthen CXL, such as using higher energy doses, may damage the underlying structures25,26, hence the appropriate trade-off between efficacy and safety of crosslinking when combined with Ortho-K requires further evaluation.
The topography showed clear profile of the changes in corneal shape from re-modelling to regression, but the refraction changes were not completely in line with the topographic measurements. Although measurement showed that a flattening of −1.13 D to −2.16 D was achieved in the reshape area in Monkey A, a lack of hyperopic shift was observed. One possible explanation is that the flattening area in monkey A was relatively small. Optometrists were easily misled by the surrounding areas where no curvature change occurred. Furthermore, measurement errors of retinoscopy should be noted for the discrepancy between topography and refraction measurement.
Although the effect of CXL treatment faded over time, corneal flattening of −1.48 D remained in the CXL treated eye in Monkey A. One of the confounding factor is the potential effect on corneal flattening solely by CXL itself, since previous studies have reported mild corneal flattening and myopia reduction in keratoconus patients after CXL treatment using the current protocol5,27,28, though most of which was observed in steeper cornea29. Elling et al.30 have performed CXL alone in myopic patients with normal corneas and observed the mean keratometry changed from 42.64 D at baseline to 42.11 D at 1 month post-op. However, the energy they used was 2–3 times higher than that in our study (10–15 J/cm2 vs. 5.4 J/cm2). Therefore, we do not think the effect of corneal flattening caused by CXL alone could be excluded, but it was of much less significance in the current protocol.
Interestingly, residual corneal flattening was only observed in Monkey A. It is conceivable that different Ortho-K modalities may influence the effect of CXL. Although high oxygen transmission materials are developed and applied in Ortho-K lenses, there is evidence that ocular surface is under additional hypoxic stress during overnight Ortho-K lens wear31. Therefore, we speculate that long-term wear of Ortho-K lenses may lead to more severe hypoxia and corneal swelling response, resulting in the diminished effect of CXL. Moreover, biomechanical changes with increasing duration of lens wear might also be attributable to the discrepancy in CXL effect32. Additional data is required to further elucidate the mechanistic hypotheses for this finding.
While the current study showed that CXL failed to sustain the corneal shape molded by Ortho-K lens, it was able to retard its regression. Therefore, reducing the frequency of lens wear while prolonging the effects of Ortho-K, especially for those with low compliance, is of substantial patient benefit. However, a more suitable protocol to achieve a better outcome and less complication is needed before its application in clinical practice.
The strengths of this study include the design of contralateral eye as a control, the use of customized Ortho-K lenses and a standardized protocol for CXL, and thorough quality control of the clinical measurements. A number of limitations must also be considered. Firstly, only two rhesus monkeys were included and assigned to different Ortho-K modalities, which may have limited the generalizability of our findings. However, given the similarities of structure, shape and size in monkey and human corneas, monkeys are the most relevant animal model available to investigate the combined treatment effects of Ortho-K and CXL. We observed consistent results in both monkeys with the application of various durations of Ortho-K wear, which would therefore provide strong evidence to support our conclusion. Another possible limitation was the short duration of follow-up that may have failed to capture the long-term effect of CXL, as some studies have observed the effects of CXL treatment on keratoconus eyes years after the procedure33. Although the latency and duration of CXL treatment effect remained unknown, our experiment confirmed that effect of CXL on corneal shape molded by Ortho-K faded within a month, hence treatment effect was unlikely even if follow-up duration was extended further.
Conclusions
In conclusion, standard CXL procedure failed to stabilize the corneal shape molded by short-term Ortho-K wear in rhesus monkeys. However, whether or not this combined therapy could achieve satisfactory outcome under other circumstances, including different Ortho-K modalities or CXL protocols, needs to be validated in further study. New research to develop a novel cross-linking technique for the stabilization of Ortho-K is ongoing.
Methods
Experimental design
This was a proof-of-concept study designed to establish the efficacy of CXL in stabilizing corneal shape following Ortho-K wear. Two male rhesus monkeys (Macaca mulatta) aged 2-year-old were used as subjects in these experiments. The monkeys were fitted with Ortho-K lenses bilaterally with different modalities to establish a transient or stable remolding status: Monkey A wore the Ortho-K lens continuously for 24 hours, while Monkey B wore the Ortho-K lens for 14 hours per day (6:00 PM to 8:00 AM) for 7 consecutive days to simulate habitual Ortho-K lens use in humans. This setting aims to test the efficay of CXL to stabilize the corneal shape at any time with any status. Ambient lighting was minimized and shade cloths were used on the cages in order to maximize adherence to the protocol and simulate the conditions most human users of Ortho K would experience.
Following contact lens removal, the left eye of each monkey was arbitrarily chosen to undergo CXL, while the fellow eye served as the control. Slit-lamp microscopy, corneal topography (Medmont E300 Corneal Topographer; Medmont Pty Ltd., Victoria, Australia) and retinoscopy refraction measurements (streak retinoscope; Lifecare Medical Equipments Co., Ltd., Zhejiang, China) were performed after the recovery of corneal epithelium in treated eyes and repeated at 1-week interval for a duration of 1 month. Differences between the treated and control eyes were observed.
The use of the animals in this study and protocols were approved by the Animal Ethics Committee of Sun Yat-sen University. The study was conducted in compliance with the Association for Research in Vision and Ophthalmology statement for the use of animals in ophthalmic and vision research.
Ortho-K lenses and lens fitting
Spherical reverse-geometry gas-permeable rigid contact lenses (E&E Optics Ltd, Hong Kong), with a refractive power of −6.00 diopters (D), an overall diameter of 10.6 mm, and an optic zone diameter of 6 mm, were used in this study. The radius of lens central curvature was chosen based on the corneal curvature map captured by a corneal topographer. Additional assessment of lens fitting was conducted with fluorescein staining under slit lamp biomicroscope by an Ortho-K expert (YX). Given that monkeys are more active than human and the lenses tend to drop out easily, mobility and stabilization of the lens were the primary consideration when selecting the lenses, hence those with optimal fluorescein patterns were selected as the final fitting lenses.
Corneal cross-linking
Standard CXL was conducted according to the Dresden Protocol19. The cornea underwent epithelial debridement with toothed forceps and sterile gauze, followed by 20 minutes’ soaking with 0.1% riboflavin (Avedro Inc., Waltham, MA, USA). Following this, the cornea was rinsed with a balanced salt solution prior to the application of UV-A irradiation. The cornea was exposed to UV-A light of 3 mW/cm2 intensity, emitted by a KXL I UV-A source (Avedro Inc., Waltham, MA, USA) for 30 minutes, receiving a total energy dose of 5.4 J/cm2. In addition, drops of riboflavin were added every 5 minutes during the exposure period to ensure sufficient supply to cornea. Antibiotic ointment (Tobradex®, Alcon, Fort Worth, USA) was administered prophylactically to the cornea directly after CXL treatment to prevent infection.
Corneal topography
Changes in the corneal shape were monitored with the Medmont E300 Corneal Topographer (Medmont Pty Ltd., Victoria, Australia). Only pictures with a systematic comprehensive score exceeding 85 points were considered acceptable. Tangential maps and subtractive maps were used to display changes in corneal shape, while the mean keratometry of the reshape zone was provided as a quantitative measurement.
Of note, the tear films of the monkey break up easily, especially in the condition of anesthesia, thus affecting the quality of topography images. Secondly, the fixation of the monkey was not stable and hard to modulate, making the comparisons between measurements unreliable. To minimize the variability of topographic measurements mentioned above, we used saline solution and artificial tears to wet the cornea and keep the integrity of the tear films before measurements. We also tried to adjust the head position of the monkeys to capture the images only when the fixation was at/near the center. In addition, we analyzed the curvature changes in central reshape zone where the measurements were most accurate and precise.
The calculation of mean keratometry of the reshape zone was performed as follows (See Supplementary Materials). Firstly, the reshape zone of Ortho-K was identified using the tangential subtractive maps before and after Ortho-K lens wear. In subtractive maps, the reshape zone is located in the central circular zone and surrounded by the ring of mid-peripheral corneal steepening. According to a previous study34, it can be effectively determined using a custom step size setting of 0.1 D in Medmont Studio 6 software (Medmont Pty Ltd., Victoria, Australia). The shape of the reshape zone was portrayed and copied in each tangential map with Adobe Photoshop software. Maps with painted reshape zones were then imported into Image-Pro Plus software (IPP; produced by Media Cybernetics Corporation, USA) and the reshape zone was set as the region of interest (ROI). Using the “counting tool” in IPP, the area ratio (ai) of each pseudo color (i) within the ROI was estimated separately and their corresponding keratometric reading (pi) was verified with the color scale. The mean keratometry of ROI (P) was calculated as:
Refraction
Refraction was performed following the instillation of tropicamide drops (1%) in each eye, using a streak retinoscope. Pupillary dilation and the absence of a pupillary light reflex was considered as successful cycloplegia. The refraction examination was conducted independently by two experienced optometrists. Results with a discrepancy ≤0.5 D between the optometrists were considered valid, otherwise a third examination was required.
All measurements including lens fitting were performed 15 minutes after general anesthesia with an intra-muscular injection of pentobarbital sodium (10 mg/kg) and topical administration of proxymetacaine hydrochloride 0.5% eyedrops (Alcaine; Alcon Laboratories Inc, Fort Worth, TX).
Description and calculations
Corneal topography profiles for baseline and each follow-up were stuck in alignment to reflect corneal shape change. The change of mean keratometry in the reshape zone was plotted with line charts and the difference in mean keratometry between follow-up examinations and baseline was plotted with bar charts. All calculations were performed using STATA Statistical Software: Release 12.0 (StataCorp LP, Colleage Station, TX).
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author upon reasonable request.
References
Hiraoka, T., Kakita, T., Okamoto, F., Takahashi, H. & Oshika, T. Long-term effect of overnight orthokeratology on axial length elongation in childhood myopia: a 5-year follow-up study. Invest. Ophthalmol. Vis. Sci. 53, 3913–3919, https://doi.org/10.1167/iovs.11-8453 (2012).
Wollensak, G. & Redl, B. Gel electrophoretic analysis of corneal collagen after photodynamic cross-linking treatment. Cornea 27, 353–356 (2008).
Wollensak, G., Spoerl, E. & Seiler, T. Stress-strain measurements of human and porcine corneas after riboflavin–ultraviolet-A-induced cross-linking. J. Cataract. Refractive Surg. 29, 1780–1785 (2003).
Wollensak, G. & Iomdina, E. Long-term biomechanical properties of rabbit sclera after collagen crosslinking using riboflavin and ultraviolet A (UVA). Acta Ophthalmol. 87, 193–198, https://doi.org/10.1111/j.1755-3768.2008.01229.x (2009).
Celik, H. U. et al. Accelerated corneal crosslinking concurrent with laser in situ keratomileusis. J. Cataract. Refract. Surg. 38, 1424–1431, https://doi.org/10.1016/j.jcrs.2012.03.034 (2012).
Kanellopoulos, A. J. & Kahn, J. Topography-guided hyperopic LASIK with and without high irradiance collagen cross-linking: initial comparative clinical findings in a contralateral eye study of 34 consecutive patients. J. Refract. Surg. 28, S837–840 (2012).
Calossi, A., Romano, F., Ferraioli, G. & Romano, V. Orthokeratology and riboflavin-UVA corneal collagen cross-linking in keratoconus. J. Emmetropia: J. Cataract, Refractive Corneal Surg. 1, 126–131 (2010).
Goyal, S., Hau, S. & Allan, B. & Rostron, C. Preoperative Orthokeratology and Corneal Collagen Cross-Linking in Keratoconus: An Exploratory Randomised Clinical Trial. Investig. Ophthalmol. Vis. Sci. 50, 5482–5482 (2009).
Swarbrick, H. A. Orthokeratology review and update. Clin. Exp. Optom. 89, 124–143, https://doi.org/10.1111/j.1444-0938.2006.00044.x (2006).
Nguyen, M. K. & Chuck, R. S. Corneal collagen cross-linking in the stabilization of PRK, LASIK, thermal keratoplasty, and orthokeratology. Curr. Opin. Ophthalmol. 24, 291–295, https://doi.org/10.1097/ICU.0b013e3283622d51 (2013).
Calossi, A., Romano, F., Ferraioli, G. & Romano, V. Orthokeratology and riboflavin-UVA corneal collagen crosslinking in keratoconus. J. Emmetropia 1, 126–131 (2010).
Qian, Y. et al. Pachymetry map of corneal epithelium in children wearing orthokeratology contact lenses. Curr. Eye Res. 39, 263–270, https://doi.org/10.3109/02713683.2013.841259 (2014).
Alharbi, A. & Swarbrick, H. A. The effects of overnight orthokeratology lens wear on corneal thickness. Invest. Ophthalmol. Vis. Sci. 44, 2518–2523 (2003).
Cheah, P. S. et al. Histomorphometric profile of the corneal response to short-term reverse-geometry orthokeratology lens wear in primate corneas: a pilot study. Cornea 27, 461–470, https://doi.org/10.1097/ICO.0b013e318165642c (2008).
Owens, H., Garner, L. F., Craig, J. P. & Gamble, G. Posterior corneal changes with orthokeratology. Optom. Vis. Sci. 81, 421–426 (2004).
Reinstein, D. Z., Gobbe, M., Archer, T. J., Couch, D. & Bloom, B. Epithelial, stromal, and corneal pachymetry changes during orthokeratology. Optom. Vis. Sci. 86, E1006–1014, https://doi.org/10.1097/OPX.0b013e3181b18219 (2009).
Gonzalez-Mesa, A., Villa-Collar, C., Lorente-Velazquez, A. & Nieto-Bona, A. Anterior segment changes produced in response to long-term overnight orthokeratology. Curr. Eye Res. 38, 862–870, https://doi.org/10.3109/02713683.2013.790977 (2013).
Kohlhaas, M. et al. Biomechanical evidence of the distribution of cross-links in corneas treated with riboflavin and ultraviolet A light. J. Cataract. Refract. Surg. 32, 279–283, https://doi.org/10.1016/j.jcrs.2005.12.092 (2006).
Wollensak, G., Spoerl, E. & Seiler, T. Riboflavin/ultraviolet-a–induced collagen crosslinking for the treatment of keratoconus. Am. J. Ophthalmol. 135, 620–627, https://doi.org/10.1016/s0002-9394(02)02220-1 (2003).
Schumacher, S., Mrochen, M., Wernli, J., Bueeler, M. & Seiler, T. Optimization model for UV-riboflavin corneal cross-linking. Invest. Ophthalmol. Vis. Sci. 53, 762–769, https://doi.org/10.1167/iovs.11-8059 (2012).
Aldahlawi, N. H. et al. Enzymatic Resistance of Corneas Crosslinked Using Riboflavin in Conjunction With Low Energy, High Energy, and Pulsed UVA Irradiation Modes. Invest. Ophthalmol. Vis. Sci. 57, 1547–1552, https://doi.org/10.1167/iovs.15-18769 (2016).
Lin, J. T. A Proposed Concentration-Controlled New Protocol for Optimal Corneal Crosslinking Efficacy in the Anterior Stroma. Invest. Ophthalmol. Vis. Sci. 59, 431–432, https://doi.org/10.1167/iovs.17-23414 (2018).
Bekesi, N. et al. Biomechanical Changes After In Vivo Collagen Cross-Linking With Rose Bengal-Green Light and Riboflavin-UVA. Invest. Ophthalmol. Vis. Sci. 58, 1612–1620, https://doi.org/10.1167/iovs.17-21475 (2017).
Wang, C., Fomovsky, M., Miao, G., Zyablitskaya, M. & Vukelic, S. Femtosecond laser crosslinking of the cornea for non-invasive vision correction. Nat. Photonics 12, 416 (2018).
Spoerl, E., Mrochen, M., Sliney, D., Trokel, S. & Seiler, T. Safety of UVA-riboflavin cross-linking of the cornea. Cornea 26, 385–389, https://doi.org/10.1097/ICO.0b013e3180334f78 (2007).
International Commission on Non-Ionizing Radiation, P. Guidelines on limits of exposure to ultraviolet radiation of wavelengths between 180 nm and 400 nm (incoherent optical radiation). Health Phys 87, 171–186 (2004).
Hersh, P. S., Greenstein, S. A. & Fry, K. L. Corneal collagen crosslinking for keratoconus and corneal ectasia: one-year results. J. Cataract. Refractive Surg. 37, 149–160 (2011).
Brooks, N. O., Greenstein, S., Fry, K. & Hersh, P. S. Patient subjective visual function after corneal collagen crosslinking for keratoconus and corneal ectasia. J. Cataract. Refractive Surg. 38, 615–619 (2012).
Koller, T., Pajic, B., Vinciguerra, P. & Seiler, T. Flattening of the cornea after collagen crosslinking for keratoconus. J. Cataract. refractive Surg. 37, 1488–1492, https://doi.org/10.1016/j.jcrs.2011.03.041 (2011).
Elling, M., Kersten-Gomez, I. & Dick, H. B. Photorefractive intrastromal corneal crosslinking for treatment of myopic refractive error: Findings from 12-month prospective study using an epithelium-off protocol. J. Cataract. refractive Surg. 44, 487–495, https://doi.org/10.1016/j.jcrs.2018.01.022 (2018).
Choy, C. K., Cho, P., Benzie, I. F. & Ng, V. Effect of one overnight wear of orthokeratology lenses on tear composition. Optom. Vis. Sci. 81, 414–420 (2004).
Chen, D., Lam, A. K. & Cho, P. A pilot study on the corneal biomechanical changes in short-term orthokeratology. Ophthalmic Physiol. Opt. 29, 464–471, https://doi.org/10.1111/j.1475-1313.2008.00625.x (2009).
Raiskup-Wolf, F., Hoyer, A., Spoerl, E. & Pillunat, L. E. Collagen crosslinking with riboflavin and ultraviolet-A light in keratoconus: long-term results. J. Cataract. Refractive Surg. 34, 796–801 (2008).
Mei, Y., Tang, Z., Li, Z. & Yang, X. Repeatability and Reproducibility of Quantitative Corneal Shape Analysis after Orthokeratology Treatment Using Image-Pro Plus Software. J. Ophthalmol. 2016, 1732476, https://doi.org/10.1155/2016/1732476 (2016).
Author information
Authors and Affiliations
Contributions
C.L. and X.L. carried out the experiments and performed data analysis. S.K. and J.H. supervised data analysis and revised the manuscript. X.Y. and M.H. developed the concept and supervised the experiments. All authors have revised the manuscript and approved the submission.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liao, C., Lin, X., Keel, S. et al. Effects of corneal crosslinking on corneal shape stabilization after orthokeratology. Sci Rep 10, 2357 (2020). https://doi.org/10.1038/s41598-020-59157-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-59157-2
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.