Abstract
Investigating COPD trends may help healthcare providers to forecast future disease burden. We estimated sex- and smoking-specific incidence trends of pre-bronchodilator airflow obstruction (AO) among adults without asthma from 11 European countries within a 20-year follow-up (ECRHS and SAPALDIA cohorts). We also quantified the extent of misclassification in the definition based on pre-bronchodilator spirometry (using post-bronchodilator measurements from a subsample of subjects) and we used this information to estimate the incidence of post-bronchodilator AO (AOpost-BD), which is the primary characteristic of COPD. AO incidence was 4.4 (95% CI: 3.5–5.3) male and 3.8 (3.1–4.6) female cases/1,000/year. Among ever smokers (median pack-years: 20, males; 12, females), AO incidence significantly increased with ageing in men only [incidence rate ratio (IRR), 1-year increase: 1.05 (1.03–1.07)]. A strong exposure-response relationship with smoking was found both in males [IRR, 1-pack-year increase: 1.03 (1.02–1.04)] and females [1.03 (1.02–1.05)]. The positive predictive value of AO for AOpost-BD was 59.1% (52.0–66.2%) in men and 42.6% (35.1–50.1%) in women. AOpost-BD incidence was 2.6 (1.7–3.4) male and 1.6 (1.0–2.2) female cases/1,000/year. AO incidence was considerable in Europe and the sex-specific ageing-related increase among ever smokers was strongly related to cumulative tobacco exposure. AOpost-BD incidence is expected to be half of AO incidence.
Similar content being viewed by others
Introduction
Chronic Obstructive Pulmonary Disease (COPD) is a major cause of chronic morbidity and mortality worldwide1, and it represents an important public health challenge, being both a preventable and treatable disease2. Globally, the COPD burden is projected to increase in coming decades because of continued exposure to risk factors and ageing of the population3.
COPD is characterised by a progressive airflow obstruction that is not fully reversible4. According to the Global Initiative for Chronic Obstructive Lung Disease guidelines2, the diagnosis of COPD requires post-bronchodilator spirometry, and the use of pre-bronchodilator measurements may lead to some misclassification of the disease5. However, post-bronchodilator spirometry has been adopted in epidemiological studies in recent years only.
Investigating how COPD rates could be affected by changes in major risk factors may help healthcare providers and decision makers to forecast the disease burden and to optimise clinical and public health strategies. In particular, tobacco smoking is the main preventable cause of COPD and it is still the most important health hazard in Europe6. Epidemiological tools for Health Impact Assessment7 are available to forecast changes in the COPD burden due to changes in a risk factor (e.g. the reduction in smoking after anti-tobacco interventions), but these tools need estimates of the COPD incidence and prevalence within a given population, among other information, as inputs.
In the present study, we evaluated incidence trends of pre-bronchodilator airflow obstruction (AO) by sex and lifetime smoking history, among adults without asthma. To fulfil this purpose, we analysed 20-year follow-up data from the European Community Respiratory Health Survey (ECRHS)8,9,10 and the Swiss Cohort Study on Air Pollution and Lung and Heart Diseases in Adults (SAPALDIA)11,12,13, and we identified AO using internally-derived equations of the lower limit of normal [LLN; 5th percentile of the distribution of the forced expiratory volume in 1 second (FEV1) and the forced vital capacity (FVC) ratio in normal subjects]. In addition, we quantified the extent of misclassification in the definition based on pre-bronchodilator spirometry (using post-bronchodilator measurements from a subsample of our subjects) and we used this information to estimate the overall incidence of post-bronchodilator airflow obstruction (AOpost-BD), which is the primary characteristic of COPD.
Results
Main characteristics of the subjects
At baseline, 5,900 men and 6,341 women without diagnosed asthma from 32 centres located in 11 European countries (listed in Supplementary Table S1) participated in the ECRHS and SAPALDIA studies, and were eligible for the present study (Fig. 1). Among these individuals, the prevalence of AO was 8.4% in males and 7.4% in females. We identified 3,076 men and 3,192 women (mean age at baseline: 36 years), who had reported not having been diagnosed with asthma at the follow-up, as subjects at risk for AO and we included them in the analyses (Fig. 1 and Table 1). About 60% of these subjects participated and provided valid lung function measurements at all three examinations. The mean duration of the follow-up was 15 years (range: 1–20 years) for both sexes. Among those at risk for AO, 65.9% of men and 56.5% of women were ever smokers at baseline and/or during the follow-up. The median number of pack-years among male and female ever smokers was 20 and 12, respectively. The selection of the subjects at risk for AO and their main characteristics are reported separately for the ECRHS and SAPALDIA studies in Supplementary Tables S2 and S3. The main characteristics of the eligible subjects included or excluded from the analyses are described separately for the two cohorts in Supplementary Tables S4 and S5.
Incidence of AO
During the follow-up, 208 incident cases of AO out of a total of 45,536 person-years were identified among males, whereas the new cases were 194 out of a total of 48,135 person-years among females (Table 2). The overall incidence rate (IR) of AO in subjects aged 25–64 was 4.4 cases/1,000/year [95% confidence interval (95% CI: 3.5–5.3)] for males and 3.8 (3.1–4.6) for females. The incidence of AO was higher for ever smokers compared to never smokers in both men [incidence rate ratio (IRR) for smoking (95% CI): 2.34 (1.65–3.32)] and women [1.78 (1.31–2.42)]. These estimates are reported separately for the ECRHS and SAPALDIA studies in Supplementary Table S6.
Trends in the incidence of AO
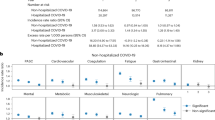
The incidence of AO greatly increased with ageing in men [IRR per 1-year increase (95% CI): 1.04 (1.02–1.06)], whereas a less steep, and statistically non-significant increase was observed in women [1.01 (0.99–1.03)] (Fig. 2). Among ever smokers, a positive trend in AO incidence was found in men as age increased [1.05 (1.03–1.07)], whereas this age trend was lees steep and did not reach statistical significance in women [1.02 (0.99–1.04)] (Fig. 3). In addition, a strong exposure-response relationship was found between lifetime pack-years and AO incidence for both males [IRR per 1-pack-year increase (95% CI): 1.03 (1.02–1.04)] and females [1.03 (1.02–1.05)] (Fig. 4). Among never smokers, no age trend in AO incidence was observed for either men [IRR per 1-year increase (95% CI): 1.00 (0.96–1.03)] or women [1.00 (0.97–1.03)] (Fig. 3).
Incidence of AOpost-BD
The positive predictive value of AO for AOpost-BD was 59.1% (95% CI: 52.0–66.2%) among the 212 men and 42.6% (35.1–50.1%) among the 184 women with AO and valid post-bronchodilator spirometry at the 3rd examination. Based on these figures, the estimated IR of AOpost-BD was 2.6 (95% CI: 1.7–3.4) cases/1,000/year in males and 1.6 (1.0–2.2) cases/1,000/year in females.
Discussion
This 20-year follow-up study of two large, population-based, European cohorts of young adults without asthma provided estimates of the incidence of AO over time. This information was used to evaluate the incidence of AOpost-BD. We found a considerable incidence of AO, quantified as 4.4 male and 3.8 female cases/1,000/year. AO incidence increased with ageing and these trends seem to be largely attributable to active smoking. The exposure-response relationship between lifetime pack-years and AO incidence could possibly be stronger in females. The incidence of AO was also high (2.3 male and 2.7 female cases/1,000/year) among lifetime non-smokers. The expected incidence of AOpost-BD was 2.6 and 1.6 cases/1,000/year for males and females, respectively.
Few spirometry-based studies have investigated the incidence of AO in large cohorts with long follow-up periods in Europe14,15. Our estimates of the overall incidence of AO are consistent with earlier results from the ECRHS I and II data14, in which the incidence of pre-bronchodilator FEV1/FVC <70% over 9 years was 3.2 and 2.4 cases/1,000/year in men and women aged 20–54, respectively. The present analyses add further and stronger evidence that AO is a major health problem in adults16, especially in males15. In respect to the previous analysis of the ECRHS data14, the longer follow-up and the inclusion of the SAPALDIA cohort in the present study (with the consequent higher sample size) enabled us to investigate incidence trends across all ages of adulthood. As a result, we found an increase of AO incidence up to 64 years in both sexes, even if this increase was less steep and did not reach statistical significance in women.
The higher incidence of AO with ageing is well known, even if it is unclear whether ageing-related biological mechanisms lead to COPD or if age reflects the accumulation of exposures during a lifetime17. In our study, we found that the incidence of AO increased with ageing among ever smokers only, which supports the concept that age reflects cumulative exposures (especially tobacco smoking) throughout life. Therefore, in the present analyses, the higher incidence of AO in men could be due to both the higher percentage of ever smokers and the higher level of tobacco exposure (pack-years) in the male cohort.
We found that female smokers reached the same level of AO incidence at a lower number of pack-years than male smokers, even if our study included a limited number of heavy smokers. Other studies have suggested that women may be at a greater risk of smoking-induced lung function impairment for the same level of exposure as men18. This may be related to a sex-specific predisposition for smoking-related lung damage or a dose-dependent effect due to smaller airways in women, with each cigarette smoked representing a proportionally greater exposure. It has been hypothesised that oestrogens could potentiate the oxidative stress due to smoking exposure, contributing to airway remodelling19,20. Sørheim and colleagues have also found that a greater lung function reduction and a more severe COPD was more common among female patients with a low smoking exposure21.
Current trends in smoking habits may have a complex effect on future trends in AO incidence. During the past decades, smoking initiation rates reduced or levelled off among late adolescents and young adults22, and smoking cessation rates increased23 across Europe. However, after 1990, smoking initiation rates markedly increased among early adolescents in different European regions22. In addition, subjects who start smoking before the age of 16 may be less likely to quit than those who start later23. Accordingly, we can speculate an increase in AO incidence during the next decades across Europe among the individuals who were in their early adolescence after the Nineties.
The high incidence of AO among never smokers, which was relatively constant with ageing, supports previous evidence that COPD also generates a substantial burden in the population not exposed to active smoking24,25. Early life insults, such as tobacco exposure in utero and childhood, low birth weight and childhood lung infections, may increase the risk of COPD26. Occupational exposures to chemicals, dust or fumes27, indoor exposure to biomass fuels28, outdoor air pollution29, chronic asthma30 and alpha-1-antitrypsin deficiency31 may also increase the risk of COPD in subjects who have never smoked.
The positive predictive value of AO for AOpost-BD was lower in women than in men in our sample, which could be explained by differences among the subjects with AO. As reported by Sawalha and colleagues5, we also found that the percentage of ever smokers (79.7% vs 73.4%), the median number of lifetime pack-years (25 vs 20), and the percentage of subjects with productive cough (21.0% vs 14.5%), factors that may predict the occurrence of COPD14, were higher in men than in women with AO and valid post-bronchodilator spirometry at the 3rd examination. In addition, our estimates of the positive predictive value (59.1% in males and 42.6% in females) were lower than the figure obtained by Schermer and colleagues (74.7% in both sexes) when the fixed cut-off definition of AO was used4. The fixed cut-off criterion leads to a substantial over-diagnosis of AO in middle-aged and elderly subjects4 and, consequently, to a higher positive predictive value.
We found that the expected overall incidence of AOpost-BD was half of the incidence of AO. We acknowledge that the expected incidence of AOpost-BD could still be an overestimate of the incidence of COPD in Europe, as AOpost-BD cases may include a non-negligible proportion of asymptomatic never smokers32 who would likely not be diagnosed with COPD in a clinical setting2.
The present study has several strengths. Firstly, it relies on the long follow-up of two large population-based cohorts of adults without asthma. In addition, the young age of our subjects at baseline enabled us to investigate AO in the early phases of COPD, which is crucial in identifying the group of individuals who could benefit from preventive interventions. The exclusion of the individuals who had reported a diagnosis of asthma at baseline or at the follow-up should have limited the bias due to the asthma-COPD misclassification. Asthma and COPD have a different aetiology, characteristics and clinical course33, and AOpost-BD in adulthood (even in smokers) should not be considered as COPD without giving consideration to earlier asthma34. However, among the incident cases of AO at the 2nd examination, 61.3% of males and 66.7% of females had either AO or key indicators of COPD2 or they reported a physician diagnosis of COPD at the 3rd examination (detailed description available in the Supplementary Information, page 7). This result suggests that a subgroup of AO cases in the present study could be patients with undiagnosed asthma. Further, the inclusion in the analyses of two large cohorts of subjects from 11 countries should have increased the generalizability of our results to the European population. Lastly, the computation of the LLN equations within our cohorts, by taking the heterogeneity of the spirometric measurements among centres into account35, should have reduced the misclassification due to the use of predictive equations generated from other populations36.
The main limitation of the present study is the lack of post-bronchodilator spirometry at all examinations, which did not enable us to directly estimate the incidence of AOpost-BD and to confirm the presence of AOpost-BD in subsequent spirometry tests37,38. In addition, having measured lung function only at three time points over 20 years could have affected the estimates of the incidence trends, as we could only predict the year of AO onset between two examinations. Further, only 60% of the subjects in our cohorts participated and had valid lung function measurements at all examinations, and attrition could have influenced our findings and limited their generalizability to some extent. However, in males, the overall IR of AO estimated from the subsample of subjects with data from all the examinations was comparable with the figure obtained from the whole cohort (4.5 vs 4.4 cases/1,000/year), whereas a lower value was found in females (3.0 vs 3.8 cases/1,000/year). The percentage of ever smokers was lower among the eligible subjects included in the study than among those excluded, for both cohorts and sexes (Supplementary Tables S4 and S5). Accordingly, we speculate that AO incidence could be underestimated in our analyses as a consequence of the lower percentage of ever smokers among the study subjects. Lastly, we acknowledge that ever smoking should be subdivided into current or past exposures, and that these two categories should be further subdivided based on pack-years (and time since smoking cessation for quitters), in order to better assess the impact of current and past smoking on AO incidence trends. Unfortunately, these analyses would require a high number of incident cases to obtain stable results.
In conclusion, the incidence of AO was considerable over 20 years among European adults without asthma, who were followed up between ages 25 and 64. The ageing-related increase in AO incidence among ever smokers was strongly related to cumulative tobacco exposure, which seems to largely explain the different age trends for men and women. The exposure-response relationship between lifetime pack-years and AO incidence could possibly be stronger in females. Although the incidence of AO was relatively constant with age, it was high even among lifetime non-smokers, which supports the fact that COPD also represents a substantial burden in the population not exposed to active smoking. The incidence of AOpost-BD is expected to be half of the incidence of AO and the extent of misclassification (when using pre-bronchodilator as opposed to post-bronchodilator spirometry) was higher in women.
Methods
Study design
The ECRHS and SAPALDIA studies share a comparable research protocol with information collected at three examinations. ECRHS (www.ecrhs.org) is an international, population-based, cohort study on respiratory health on random samples of subjects aged 20–44 years in 1991–1993 (ECRHS I; 1st examination)8. Each participant was sent a brief screening questionnaire (stage 1) and, from those who responded, a 20% random sample was invited to undergo a more detailed clinical examination (stage 2). The participants in the ECRHS I - stage 2 were followed up in 1998–2002 (ECRHS II; 2nd examination)9 and in 2010–2013 (ECRHS III; 3rd examination)10. SAPALDIA (www.sapaldia.ch/en/) is a Swiss, population-based, cohort study on the long-term health effects of air pollutants in subjects aged 18–60 years in 1991, who were randomly selected from local registries of inhabitants to undergo standardized clinical tests (SAPALDIA I; 1st examination)11,39. The participants in SAPALDIA I were re-examined in the clinical centres in 2001–2003 (SAPALDIA II; 2nd examination)12 and in 2010–2011 (SAPALDIA III; 3rd examination)13.
The subjects in both the ECRHS and SAPALDIA studies underwent a detailed clinical interview and pre-bronchodilator spirometry at each examination, and post-bronchodilator spirometry was also measured at the last follow-up contact. The maximum FEV1 and the maximum FVC from at least two technically satisfactory manoeuvres were measured according to the American Thoracic Society criteria for repeatability39,40. Biomedin, Jaeger Masterscope, SensorMedics or Vitalograph spirometers were used at the 1st and 2nd examinations, whereas NDD EasyOne was used in almost all centres at the 3rd examination (see Supplementary Table S1). In both the studies, the lung function measurements were corrected for the change in spirometer, according to Bridevaux and colleagues41.
Selection of the subjects and definitions
The eligible subjects (Fig. 1) were those who:
were at least 25 years old in the ECRHS - stage 2 or SAPALDIA I, in order to exclude those who may still not have reached the plateau phase of lung function growth at baseline42;
were born in 1945 or later, in order to have the same age range in the ECRHS and SAPALDIA cohorts;
had provided valid lung function measurements at baseline;
had reported never having been diagnosed with asthma at baseline.
The subjects at risk for AO (Fig. 1) were the eligible participants who:
had pre-bronchodilator FEV1/FVC ≥LLN at baseline (internally-derived LLN equations were computed, which take the variation in the spirometric measurements due to differences among centres into account35,43; detailed description available in the Supplementary Information, pages 3–4);
had provided valid lung function measurements during at least two consecutive examinations (ECRHS/SAPALDIA I-II or ECRHS/SAPALDIA I-II-III);
had reported not having been diagnosed with asthma at the follow-up.
The subjects at risk who had pre-bronchodilator FEV1/FVC <LLN at one of the follow-up contacts were considered to be incident cases of AO. For each new case, the year of age at AO onset was estimated by linear interpolation, (i) assuming that the decline in FEV1/FVC between two examinations was constant and (ii) taking into account the change in the LLN cut-off with ageing (detailed description available in the Supplementary Information, page 5). Based on these assumptions, we obtained the year of age when the FEV1/FVC had reached a level below the LLN for each individual. The end of the follow-up was the calendar year of AO onset (obtained by summing the estimated year of age at onset to the birth year) for the incident cases, and the calendar year of the last examination for the remaining subjects.
Smoking was classified as “never” (i.e. never smoking at baseline and follow-up) and “ever” (i.e. past or current smoking at baseline or follow-up). Lifetime pack-years were quantified at the end of the follow-up.
Statistical analyses
The ECRHS and SAPALDIA data were pooled to estimate the IRs of AO and their trends, within age 25–64 years during 1991–2011. Data pooling was justified due to the fact that the AO rates were similar in the two studies for both sexes (see Supplementary Table S6). Age was right-censored at 64 years in order to avoid data sparseness, whereas the time period was right-censored at 2011 in order to analyse the data from the same period for both the studies. The sex-specific pooled datasets were reshaped by age to estimate AO incidence (detailed description available in the Supplementary Information, page 6).
Incidence of AO
The overall IRs of AO were computed separately in males and females using two-level Poisson models (subject = level 1 unit; centre = level 2 unit). All the models had log person-years as the offset, a random intercept term at level 2 and study (0 = ECRHS, 1 = SAPALDIA) as a fixed effect. The smoking-specific IRs of AO were estimated adding smoke (ever vs never) and the smoke × study interaction term to the fixed part of the models. All the rates were obtained by setting the indicator of the study equal to the proportion of person-years in SAPALDIA (0.44 for males and 0.46 for females), in order to account for the different overall time at risk in the two cohorts.
Trends in the incidence of AO
Age trends in AO incidence were estimated separately in males and females using two-level Poisson models with log person-years as the offset, a random intercept term at level 2 and age, study and the age × study interaction term as fixed effects. Age was included as a linear factor in the models since higher degree polynomials or spline interpolations did not improve goodness-of-fit. Age trends were computed according to smoking history adding smoke and the age × smoke interaction term to the fixed part of the models. Lastly, AO incidence was evaluated according to lifetime pack-years among ever smokers, using sex-specific reshaped datasets by pack-years and two-level Poisson models with pack-years, study and the pack-years × study interaction term as fixed effects. The number of pack-years was right-censored at 60 for men and 45 for women to avoid data sparseness.
Incidence of AOpost-BD
The expected IR of AOpost-BD (post-bronchodilator FEV1/FVC <LLN) was estimated from the overall IR of AO, separately in men and women. Firstly, the positive predictive value of AO for AOpost-BD was computed for each sex among those with pre-bronchodilator FEV1/FVC ≥LLN and valid post-bronchodilator lung function measurements in the ECRHS/SAPALDIA III. Secondly, the expected IR of AOpost-BD was obtained as the product of the sex-specific estimates of the AO rate and the positive predictive value. The 95% confidence interval of the AOpost-BD rate was computed by using the delta method and assuming that the sex-specific estimates of the AO rate and of the positive predictive value have a perfect positive correlation.
The statistical analyses were carried out using STATA 15 (StataCorp, College Station, TX).
Ethics statement
Ethics approval was obtained by all centres from the appropriate ethics committees in ECRHS [Antwerp City and Antwerp South: Adviescommissie Medische Ethiek UZA-UA (CME); Tartu: Research Ethics Committee of the University of Tartu, Estland (N° 209T-17); French centres: Comite de protection des personnes, Sud V Est (N° 2011-A00013-38); German centres: Ethik-Kommission der Bayerischen Landesarztekammer (N° 10015); Reykjavik: National Biotecs Committe of Iceland (NBCI) (N° VSNb2011090016/03.11); Pavia: Fondazione IRCCS Policlinico ‘San Matteo’ (N° P-20110024215); Turin: Comitato Etico dell’Azienda Sanitaria Locale TO/2 di Torino (N° 569/09/08); Verona: Comitato Etico per la Sperimentazione dell’Azienda Ospedaliera Istituti Ospitalieri di Verona (N° 1393); Bergen: Universitetet i Bergen, Regional komité for medisinsk og helsefaglig forskningsetikk, Vest-Norge (REK Vest) (N° 2010/759); Albacete: Comité de Ética e Investigación de Complejo Hospitalario de Albacete (N° 04/09); Barcelona: Comité Ético de Investigación Clínica del Instituto Municipal de Asistencia Sanitaria, Barcelona, Spain (N° PS09/00716); Galdakao: Comité Ético de Investigación del Hospital de Galdakao, Spain (N° 20101104); Huelva: Comisión de Investigación del Hospital Juan Ramón Jiménez de Huelva (N° 20090417); Oviedo: Comité Ético de Investigación Clínica Regional, Hospital Universitario Central de Asturias (N° 20110415); Swedish centres: Ethics Committee at the Medical Faculty, Uppsala University (N° 1999/313 and 2010/068); Basel: Swiss Academy of Medical Sciences and the ethics committee of Basel (N° PV123/00,157/00); UK centres: NRES Committee London - Stanmore (REC Reference 11/LO/0965 IRAS number 70769)] and in SAPALDIA [Swiss Academy of Medical Sciences and the regional committees for each study centre; ethics approval is coordinated by the lead ethical agency EKNZ in Basel, Switzerland]. In both the studies, written informed consent was obtained from the participants and all experiments were performed in accordance with relevant guidelines and regulations.
Data availability
Due to data protection reasons, the datasets analysed in the present study cannot be made publicly available. The datasets are available to interested researchers from the corresponding author on reasonable request.
References
Lozano, R. et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380, 2095–2128 (2012).
Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease. NHLBI/WHO Workshop Report. Bethesda, MD: National Institutes of Health Publication No. 2701; revised (2018).
Mathers, C. D. & Loncar, D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 3, e442, https://doi.org/10.1371/journal.pmed.0030442 (2006).
Schermer, T. R. et al. Current clinical guideline definitions of airflow obstruction and COPD overdiagnosis in primary care. Eur. Respir. J. 32, 945–952 (2008).
Sawalha, S., Hedman, L., Rönmark, E., Lundbäck, B. & Lindberg, A. Pre- and post-bronchodilator airway obstruction are associated with similar clinical characteristics but different prognosis - report from a population-based study. Int. J. Chron. Obstruct. Pulmon. Dis. 12, 1269–1277 (2017).
Chapter 9: Tobacco smoking in The European Lung White Book (eds. Gibson, J., Loddenkemper, R., Sibille, Y. & Lundbäck, B.) 98–111 (European Respiratory Society, 2013).
Lhachimi, S. K. et al. DYNAMO-HIA–a Dynamic Modeling tool for generic Health Impact Assessments. PLoS One 7, e33317, https://doi.org/10.1371/journal.pone.0033317 (2012).
Burney, P. G., Luczynska, C., Chinn, S. & Jarvis, D. The European Community Respiratory Health Survey. Eur. Respir. J. 7, 954–960 (1994).
European Community Respiratory Health Survey II Steering Committee. The European Community Respiratory Health Survey II. Eur. Respir. J. 20, 1071–1079 (2002).
Amaral, A. F. S. et al. Changes in IgE sensitization and total IgE levels over 20 years of follow-up. J. Allergy Clin. Immunol. 137, 1788–1795 (2016).
Ackermann-Liebrich, U. et al. Lung function and long term exposure to air pollutants in Switzerland. Study on Air Pollution and Lung Diseases in Adults (SAPALDIA) Team. Am. J. Respir. Crit. Care Med. 155, 122–129 (1997).
Ackermann-Liebrich, U. et al. Follow-up of the Swiss Cohort Study on Air Pollution and Lung Diseases in Adults (SAPALDIA 2) 1991–2003: methods and characterization of participants. Soz. Praventivmed. 50, 245–263 (2005).
Hansen, S. et al. Gender differences in adult-onset asthma: results from the Swiss SAPALDIA cohort study. Eur. Respir. J. 46, 1011–1020 (2015).
de Marco, R. et al. Incidence of chronic obstructive pulmonary disease in a cohort of young adults according to the presence of chronic cough and phlegm. Am. J. Respir. Crit. Care Med. 175, 32–39 (2007).
Terzikhan, N. et al. Prevalence and incidence of COPD in smokers and non-smokers: the Rotterdam Study. Eur. J. Epidemiol. 31, 785–792 (2016).
de Marco, R. et al. An international survey of chronic obstructive pulmonary disease in young adults according to GOLD stages. Thorax 59, 120–125 (2004).
Mercado, N., Ito, K. & Barnes, P. J. Accelerated ageing of the lung in COPD: new concepts. Thorax 70, 482–489 (2015).
Han, M. K. et al. Gender and chronic obstructive pulmonary disease: why it matters. Am. J. Respir. Crit. Care Med. 176, 1179–1184 (2007).
Tam, A. et al. Sex-related differences in pulmonary function following 6 months of cigarette exposure: implications for sexual dimorphism in mild COPD. PLoS One 11, e0164835, https://doi.org/10.1371/journal.pone.0164835 (2016).
Amaral, A. F. S., Strachan, D. P., Burney, P. G. J. & Jarvis, D. L. Female smokers are at greater risk of airflow obstruction than male smokers. UK Biobank. Am. J. Respir. Crit. Care Med. 195, 1226–1235 (2017).
Sørheim, I. C. et al. Gender differences in COPD: are women more susceptible to smoking effects than men? Thorax 65, 480–485 (2010).
Marcon, A. et al. Trends in smoking initiation in Europe over 40 years: A retrospective cohort study. PLoS One 13, e0201881, https://doi.org/10.1371/journal.pone.0201881 (2018).
Pesce, G. et al. Time and age trends in smoking cessation in Europe. PLoS One 14, e0211976, https://doi.org/10.1371/journal.pone.0211976 (2019).
Tan, W. C. et al. Characteristics of COPD in never-smokers and ever-smokers in the general population: Results from the CanCOLD study. Thorax 70, 822–829 (2015).
Lamprecht, B. et al. COPD in never smokers: results from the population-based burden of obstructive lung disease study. Chest 139, 752–763 (2011).
Savran, O. & Ulrik, C. S. Early life insults as determinants of chronic obstructive pulmonary disease in adult life. Int. J. Chron. Obstruct. Pulmon. Dis. 13, 683–693 (2018).
Hagstad, S. et al. Prevalence and risk factors of COPD among never-smokers in two areas of Sweden - Occupational exposure to gas, dust or fumes is an important risk factor. Respir. Med. 109, 1439–1445 (2015).
Assad, N. A., Balmes, J., Mehta, S., Cheema, U. & Sood, A. Chronic obstructive pulmonary disease secondary to household air pollution. Semin. Respir. Crit. Care Med. 36, 408–421 (2015).
Andersen, Z. J. et al. Chronic obstructive pulmonary disease and long-term exposure to traffic-related air pollution: a cohort study. Am. J. Respir. Crit. Care Med. 183, 455–461 (2011).
Salvi, S. S. & Barnes, P. J. Chronic obstructive pulmonary disease in non-smokers. Lancet 374, 733–743 (2009).
Stoller, J. K. & Aboussouan, L. S. Alpha1-antitrypsin deficiency. Lancet 365, 2225–2236 (2005).
de Marco, R. et al. Long-term outcomes in mild/moderate chronic obstructive pulmonary disease in the European Community Respiratory Health Survey. Am. J. Respir. Crit. Care Med. 180, 956–963 (2009).
Rogliani, P., Ora, J., Puxeddu, E. & Cazzola, M. Airflow obstruction: is it asthma or is it COPD? Int. J. Chron. Obstruct. Pulmon. Dis. 11, 3007–3013 (2016).
Sears, M. R. Smoking, asthma, chronic airflow obstruction and COPD. Eur. Respir. J. 45, 586–588 (2015).
Roca, J. et al. References values for forced spirometry. Eur. Respir. J. 11, 1354–1362 (1998).
Swanney, M. P. et al. Using the lower limit of normal for the FEV1/FVC ratio reduces the misclassification of airway obstruction. Thorax 63, 1046–1051 (2008).
Schermer, T. R. et al. Should the diagnosis of COPD be based on a single spirometry test? NPJ Prim. Care Respir. Med. 26, 16059, https://doi.org/10.1038/npjpcrm.2016.59 (2016).
Aaron, S. D. et al. Diagnostic instability and reversals of chronic obstructive pulmonary disease diagnosis in individuals with mild to moderate airflow obstruction. Am. J. Respir. Crit. Care Med. 196, 306–314 (2017).
Martin, B. W. et al. SAPALDIA: methods and participation in the cross-sectional part of the Swiss Study on Air Pollution and Lung Diseases in Adults. Soz. Praventivmed. 42, 67–84 (1997).
Miller, M. R. et al. Standardisation of spirometry. Eur. Respir. J. 26, 319–338 (2005).
Bridevaux, P. O. et al. Spirometer replacement and serial lung function measurements in population studies: results from the SAPALDIA study. Am. J. Epidemiol. 181, 752–761 (2015).
Knudson, R. J., Lebowitz, M. D., Holberg, C. J. & Burrows, B. Changes in the normal maximal expiratory flow-volume curve with growth and aging. Am. Rev. Respir. Dis. 127, 725–734 (1983).
Cerveri, I. et al. Underestimation of airflow obstruction among young adults using FEV1/FVC <70% as a fixed cut-off: a longitudinal evaluation of clinical and functional outcomes. Thorax 63, 1040–1045 (2008).
Acknowledgements
The present analyses are part of the ALEC Study (www.alecstudy.org). The ALEC project leader is Deborah Jarvis. The manuscript was done with ALEC Workpackage 6 led by Cosetta Minelli. Other Workpackage leaders in ALEC are Cecilie Svanes, John Henderson (University of Bristol, Bristol, UK), Judith Garcia-Aymerich [ISGlobal, Centre for Research in Environmental Epidemiology (CREAL), Barcelona, Spain] and Nicole Probst-Hensch. ALEC has received funding from the European Union’s Horizon 2020 research and innovation programme [Grant Agreement No. 633212]. The co-ordination of the ECRHS was supported by the European Commission (phases 1 and 2) and the Medical Research Council (phase 3). The SAPALDIA cohort was funded by The State Secretariat for Education, Research and Innovation (SERI), Switzerland. The principal investigators and team members of the ECRHS and SAPALDIA studies, and the national funders who supported data collection in the ECRHS and SAPALDIA studies are listed in the appendix available in the Supplementary Information.
Author information
Authors and Affiliations
Contributions
S.A., L.C. and A.M. conceived the study. S.A. designed the study and drafted the analysis plan and the first version of the manuscript. L.C., S.A. and G.P. performed the statistical analysis. All the authors contributed in the collection of data in/from the original studies, discussion of the statistical analysis plan and interpretation of study results. All the authors critically reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Accordini, S., Calciano, L., Marcon, A. et al. Incidence trends of airflow obstruction among European adults without asthma: a 20-year cohort study. Sci Rep 10, 3452 (2020). https://doi.org/10.1038/s41598-020-60478-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-60478-5
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.