Abstract
Physical non-communicable diseases (NCDs) and mental health disorders are a rapidly increasing health burden in low-and middle-income countries. This study aims to examine the relationships between mental health disorders and cascade of care in managing four common physical NCDs (hypertension, diabetes, dyslipidemia, chronic kidney disease) in China. We utilized two waves of nationally-representative China Health and Retirement Longitudinal Study (CHARLS 2011, 2015) of older adult population aged 45 and above. A series of unadjusted and adjusted mixed-effect logistic regression was applied to evaluate the association between presence of mental health disorder and physical chronic disease awareness, treatment, and control. We found that the odds of dyslipidemia (AOR 1.81, 95% CI 1.36–2.39) and kidney disease awareness (AOR 2.88, 95% CI 2.12–3.92) were higher for individuals with mental chronic conditions, compared to those without mental chronic conditions. The odds of having hypertension treatment was higher for subjects with mental health disorder, compared to those without (AOR 1.32, 95% CI 1.02–1.70). The odds of having physical chronic conditions controlled was not significantly associated with having mental chronic conditions (P > 0.05). These results indicated that adults with mental health disorder have a greater likelihood of awareness of having dyslipidemia and kidney disease, and receiving treatment for hypertension. Strategies to address the growing burden of physical-mental NCDs in China should include efforts to improve management of patients with comorbid health condition and improve access to continual high-quality treatment after the first diagnosis.
Similar content being viewed by others
Introduction
The prevalence of the co-occurrence of physical non-communicable disease (NCDs) and mental health disorder is increasing rapidly in many low-and middle-income countries (LMIC)1. Evidence suggests that the relationship between physical NCDs and mental health disorders is bidirectional2. China, the most populous country, has seen rapid demographic and epidemiological transition over the last few decades. By 2050, the projected proportion of the older population, aged 60 years and over, will dramatically increase to 35.1% from 16.2% in 20173. The repaid aging population has led to substantial increase in the prevalence of physical NCDs. For example, a recent study, based on 11 physical NCDs, found that the prevalence of physical multimorbidity was 62% among those aged 45 years and older4. The prevalence of mental health disorders has also been increasing in recent decade5. Analysis using China Mental Health Survey, based on 32,552 participants in 31 provinces in China, found that the prevalence of any mental health disorders was 9.3% in 2013 among Chinese adults6. The rising prevalence of physical and mental chronic conditions is expected to post significant challenges to the health system in China.
The potential impact of mental health disorder on the cascade of care in managing physical NCDs is an emerging area of research interest. The UK National Institute from Health and Care Excellence (NICE) guidelines on multimorbidity have emphasized the challenge of poor management of chronic conditions in adults, which could subsequently be associated with higher treatment burden and poorer health-related quality of life (HRQoL)7,8. The literature on the impact of having multimorbidity on the management and control of each of the chronic conditions is scarce, with current studies largely from High-income countries (HICs) that use qualitative methods9,10,11,12,13. There is also some quantitative research in the literature that have investigated how having more comorbid NCDs influences management and control of specific conditions, primarily hypertension14,15. Furthermore, a limited number of studies, mostly from HICs as well, have focused on the differential impact of concordant versus discordant conditions on the quality of chronic disease management8,16,17,18,19,20. While it may be hypothesized that concordant conditions would facilitate the management of a NCD due to the similar pathophysiology and treatment regiments, and discordant NCDs would have opposite effects, existing studies demonstrate inconsistencies on how concordant and discordant NCDs influence the management of chronic diseases8,17,20.
To illustrate, a retrospective cohort study in the United States on hypertensive primary care patients examined the impact of concordant versus discordant NCDs of hypertension, on hyperlipidemia management16. This study showed that additional discordant conditions were associated with lower odds of hyperlipidemia management compared with no discordant NCDs, and additional concordant conditions were associated with increased odds of hyperlipidemia management16. Another study analyzed 15,000 patients from primary care practices in the United States who have multimorbidity and uncontrolled hypertension, and found that patients with more discordant NCDs to hypertension (28 conditions including arthritis and emphysema) were less likely to have their uncontrolled hypertension solved, compared to those with concordant conditions18. Our recent paper which also analyzed the World Health Organization study on global aging and adult health data (WHO SAGE) found that having more NCDs was associated with better odds of diagnosis but not better management and control of co-occurring NCDs21. Importantly, generating more research from LMICs is crucial as the findings from HICs may not able applicable, due to different health systems and access to healthcare for diagnostic testing and treatment9,13,17,22. In addition, impact of a broader range of NCDs needs to be investigated8,14,15,17,19,20.
This study examines individuals in China with multimorbidity that consists of both physical and mental health chronic conditions. Specifically, we investigate how having mental health conditions is associated with cascade of care in managing four common physical NCDs (e.g. hypertension, diabetes, dyslipidemia, chronic kidney disease) of the elder adult population in China.
Methods
Participants and sample
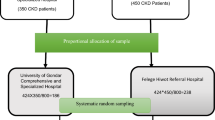
This study analysed pooled cross-sectional data of the first wave (2011) and third wave (2015) of China Health and Retirement Longitudinal Study (CHARLS). We have registered in CHARLS website and get the permission from Peking University of using this dataset. All participants of CHARLS have signed consent forms before face-to-face interview. Personal information, like ID, address, are removed from the dataset and coded as a series of numbers.
The CHARLS consists of nationally representative participants aged 45 or older from 450 randomly selected communities/villages in 28 provinces of China23. It collects information on demographics, family, health status and functioning, health care and insurance, income, work, and housing. Respondents of CHARLS are followed up every two years via face-to-face computer-assisted personal interview (CAPI)23. Biomarkers for chronic diseases were used in each wave, while blood tests were conducted every two waves24. Additional information about CHARLS are available on http://charls.ccer.edu.cn/.
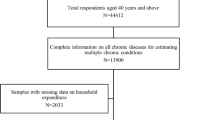
17,708 subjects participated in the first wave (2011) and 20,967 participated in the third wave (2015). For those participants, 14,574 participated in both the first and third wave (2015). For the purpose of the study, we only include those with biomarker and blood test result (63% of the total observations in the two waves). After removing subjects with missing information on covariates (30% of the sample), the final sample size in this study is 17,141, which include 8189 observations in the first wave and 8952 observations in the third wave.
Variables
Predictor variables
The predictor variable in this study is having a mental health disorder. Having mental health disorder was defined as the existence of any one of those following conditions (1) answer affirmatively to “have you been diagnosed with emotional, nervous, or psychiatric problem by a doctor?” (2) answered affirmatively to “have you been diagnosed with memory-related disease by a doctor?” (3) 10-item Center for Epidemiologic Studies Depression Scale (CES-D-10) higher than 1225. This study only included respondents that have answered at least 9 items on CES-D-10, and used the average of the remaining 9 items to impute the missing item.
Outcome variables
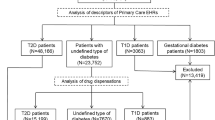
Awareness
Having awareness of the chronic condition is defined as being diagnosed by doctors or being self-aware of their chronic conditions. For hypertension, blood pressure was measured three times for each participant and this study only included participants with at least two results on systolic blood pressure and diastolic blood pressure to minimize measurement error. This study revised the WHO definition for hypertension to meet the questionnaire design26. Participants with hypertension are defined as the existence of one the following conditions: (1) average systolic blood pressure ≥ 140 mmHg; (2) average diastolic blood pressure ≥ 90 mmHg; (3) self-report hypertension diagnosed by a doctor or self-report aware of hypertension. Hypertension awareness is defined as respondents with hypertension and their hypertension is diagnosed by doctors or they are aware of their hypertension condition. Diabetes is defined as: (1) fasting blood glucose ≥ 126 mg/dl; (2) non-fasting blood glucose ≥ 200 mg/dl; (3) HbA1c concentration ≥ 6.5%; (4) self-report diabetes diagnosed by a doctor27. Dyslipidemia is defined as: (1) triglyceride ≥ 200 mg/ml; (2) HDL (high density lipoprotein cholesterol) < 40 mg/dl; (3) LDL (low density lipoprotein cholesterol) ≥ 160 mg/dl; (4) TC (total cholesterol) ≥ 240 mg/dl; (5) self-report dyslipidemia diagnosed by a doctor28. Kidney disease is defined as: (1) GFR (Glomerular Filtration Rate) < 90 ml/min/1.72m2; (2) with self-report kidney disease diagnosed by a doctor. GFR is calculated by using Levey’s method29. Diabetes, dyslipidemia, kidney disease awareness was defined as respondents with diabetes, dyslipidemia, or kidney disease and these conditions are diagnosed by doctors.
Treatment
Being treated for a NCD is defined as respondents with self-reported chronic conditions diagnosed by a doctor or being aware of their chronic condition and taking at least one treatment for this chronic condition. For hypertension, respondents answer affirmatively to “taking Chinese traditional medicine” or “taking western modern medicine” to the question “Are you taking any of the following treatments to treat hypertension or its complication?” are considered to be with hypertension treated. For diabetes and kidney disease, respondents choose any one of the following choices “taking Chinese traditional medicine”, “taking western modern medicine” or “other treatments” to question “are you taking any of the following treatment to treat (…) or its complications?” are considered to be with hypertension/kidney disease treatment. For diabetes, respondents choose any one of those choices “taking Chinese traditional medicine” “taking western modern medicine” or “taking insulin injections” to the question “are you taking any of the following treatments to treat or control your diabetes” are considered to be with diabetes treated.
Controlled
Being controlled for a NCD is defined as respondents with self-report chronic condition, with self-report treatment and with normal biomarker or blood test result. The clinical criteria for hypertension, dyslipidemia, diabetes, and kidney disease are mentioned in the part of awareness.
Covariates
Covariates are age (45–54, 55–64, 65–74, 75 +), sex (male, female), marital status (married, single), education level (primary school or below, middle or high school, college or above), consumption quantile (as a proxy for economic status, is calculated by dividing individual household consumption into 5 equal parts by using 20th, 40th, 60th, and 80th percentiles), residence type (rural, urban, migrates), health insurance status (no insurance, UEMI (Urban Employee Medical Insurance), URMI (Urban Resident Health Insurance), NCMI (New Cooperative Medical Insurance), others), region (eastern, central, western, and north–east), number of outpatient visits, and number of physical chronic conditions (0, 1, 2, 3 ,4+).
Statistical analysis
Demographic characteristics of participants for year 2011 and 2015 were calculated separately. The demographic characteristics of participants with hypertension, diabetes, dyslipidemia, and or kidney disease were calculated separately for subjects with mental health disorder and without mental health disorder.
We estimated the prevalence of NCD awareness, treatment, and control for subjects with and without mental health disorder separately. Pearson chi-square test was used to test the significance in the difference between subjects with mental health disorder and those without mental health disorder for their awareness, treatment, and control of physical chronic conditions.
A series of unadjusted and adjusted mixed-effects logistics regressions were used to evaluate the effect of mental health disorders on NCD awareness, treatment, and control. People who live in the same community are more likely to have similar living environments and medical conditions, which results in a similarity in chronic disease management. To reduce the impact of unobserved individual characteristics and community characteristics on the estimation of coefficients, this study used fixed effect on the level of individual ID and community IC, while using random effect to estimate the effect of other covariates30. First, we conducted unadjusted mixed effect logistics regression with NCD awareness, treatment, or control as the outcome variable and mental health disorder as the predicting variable. Subsequently, we fitted multiple mixed effect logistics regression with NCD awareness, treatment, or control as the outcome variable, mental health disorder as the exposure variable, and adjusted for the covariates mentioned above including frequency of outpatient visits.
All data analysis was performed by using Stata 14.0 and level of significance was set at 0.05.
Results
The number of observations in this study is 17,141, of which 8189 observations are from year 2011, and 8952 are from year 2015. The demographic characteristics of participants are presented in Table 1 separately for year 2011, year 2015, and overall. Among those observations, 7361 observations with hypertension, 2342 observations with diabetes, 7054 observations with dyslipidemia, and 9265 observations with kidney disease. The demographic characteristics of observations with hypertension, with diabetes, with dyslipidemia, and with kidney disease are presented in Appendix Table 1a,b,c,d.
The prevalence of NCD awareness, treatment, and control for subjects with and without mental health disorder are presented in Table 2. The prevalence of NCD awareness ranges from 74.47% for people with hypertension and with mental health disorder to 27.71% for people with kidney disease and without mental health disorder. For all of the four NCDs, the prevalence of NCD awareness is significantly higher for people with mental health disorder than people without mental health disorder (P < 0.05).
For hypertension, dyslipidemia, and kidney disease, the prevalence of those physical conditions being treated is higher for people with mental health disorder than without mental health disorder, while this difference is not significant for diabetes (P-value = 0.510). For diabetes, the prevalence of physical conditions being controlled is lower for people without mental health disorder than with mental health disorder (P-value = 0.020), however, this difference is not significant for the other three physical chronic conditions. Although the prevalence of physical conditions being controlled is lower for people without mental health disorder than people with mental health disorder, the difference is not significant at the 5% level.
Table 3 presents the univariate and multivariate mixed effect logistic regression result. The reference group is people without mental health disorder. Having mental health disorder was associated with increased odds of NCD awareness for dyslipidemia (AOR (Adjusted odds ratio) = 2.88, 95% CI (confidence interval) = 2.21–3.74) and kidney disease (AOR 4.14, 95% CI 2.95–5.81). However, there was not significant increase the odds of hypertension and diabetes awareness (P > 0.05). Having mental health disorder was associated with an increased odds of receiving hypertension treatment (AOR 1.32, 95% CI 1.02–1.70), but not diabetes treatment, dyslipidemia treatment, and kidney disease treatment (P > 0.05). Having mental health disorder is not associated with increased or decreased odds of being controlled for all four NCDs (P > 0.05). All regression results are listed in the appendix Table 1.
Discussion
Principle findings
We presented the first study that investigate the associations between having mental health disorder and cascade of care in managing four common physical NCDs in China among the older adult population. Our study revealed that having mental health disorder was associated with increased odds of being aware of having dyslipidemia, and kidney disease, after adjusting for covariates including frequency of outpatient visit. Additionally, having mental health disorder was associated with increased odds of receiving treatment of hypertension, but not for diabetes, dyslipidemia, and kidney disease. However, having mental health disorder was not associated with increased or decreased odds of being controlled for hypertension, diabetes, dyslipidemia and kidney disease.
Comparison with literature
The finding on the positive effect of having mental health conditions on better diagnosis of previously undiagnosed dyslipidemia and kidney disease is consistent with the small number of existing articles. Subjects with more comorbidities likely resulted in having more frequent visits to and interactions with multiple health providers8,20,31,32,33, such as dyslipidemia, and kidney disease in this particular study. Additionally, healthcare providers are likely to spend more time on consultation and suggest more examinations for patients with multiple chronic conditions. Third, healthcare providers often prescribe thyroid function and blook lipid tests for patients with mental health disorders, because they all believe thyroid function is strongly associated with emotional problems and patients with thyroid imbalance are more likely to develop lipid problems34. Fourth, for patients with long-term treatment of psychotropic drugs, healthcare providers often suggest them to do liver and kidney function tests regularly, because long-term use of medication may cause liver or kidney function damage35. An increased frequency of healthcare visits, having more comorbidities, and more interactions with healthcare providers were likely associated with a greater tendency for patients to self-report kidney pain and test blood liquid36,37.
Studies that have examined the relationship between comorbid health condition and NCD treatment, have shown conflicting results which may reflect complexity of the issue8,20,33,38,39,40. It is worth noting that our study considered only whether subjects were taking treatment or not, and did not if treatment was adequate, in terms of adherence to medication8,20,41. While our study showed that subjects with mental health disorder have higher odds of taking treatment, but in reality, with more co-occurring physical conditions, the odds of treatment adherence and having adequate treatment would decline8,20.
The finding on having mental health conditions not associated with increased or decreased odds of being controlled for hypertension, diabetes, dyslipidemia and kidney disease is not consistent with the little amount of existing literature. The difficulty in controlling NCDs tend to be exacerbated with having more co-occurring physical chronic conditions12,14,18.
There has been debate in the recent literature on how co-occurring conditions influence the management and control of NCDs8,20. Magnan et al. (2014) analyzed electronic health data records of 24,430 adults aged 18 to 75 years from the United States, and revealed that even though having more concordant NCDs were correlated with a higher likelihood of achieving diabetes control goals, this relationship was not present for the outcome on achieving blood pressure control19. Ricci-Cabello et al. (2015) investigated the prevalence of concordant and discordant NCDs of diabetes, and their impact on diabetes care in England8,17. The study revealed that only 2 of 8 discordant NCDs to diabetes were correlated with worse quality of diabetes care, and only 4 of 7 concordant NCDs with diabetes were correlated with better quality of diabetes care17.
Hence, this study along with our previous work and other papers, provide further evidence on the complexity of how co-occurring mental health conditions impact the management and control of NCDs, and the hypothesis that concordant comorbidities with mental illness facilitate the management of NCDs and discordant comorbidities with mental illness impede the management of NCDs may be over-simplified8,20.
Strengths and limitations
This is the first study that used a large population of adults from China with multimorbidity, to investigate the association between having mental health conditions with the odds of being undiagnosed, untreated and uncontrolled for co-occurring physical chronic condition.
However, several limitations need to be considered when drawing conclusion from this study. First, Self-reported diagnosis and treatment of chronic conditions may be under-reported due to recall bias42,43,44. Stigma could be another reason for under-reporting of depression in MICs45,46. Additionally, this survey only asked if subjects were taking treatment (medicines, lifestyle changes), but did not measure the adherence to treatment (i.e. dosage, frequency, duration, etc.)20,41. Biomarkers used to assess whether chronic conditions were controlled may not be sufficiently comprehensive. Supplemental assessment criteria may have been needed for better accuracy. Third, results from this study may not apply to those excluded from our study due to incomplete data of biomarkers or blood test results.
Future studies could expand on this study by examining more NCDs, especially conditions with high prevalence and morbidity8,20,47. The study’s cross-sectional design means that causality could not be determined, and studies that use cohort study designs could examine how mental health conditions lead to worse treatment and control of physical chronic diseases in subjects that are followed-up over a decade8,20,38.
Clinical, policy, and research implications
Clinical guidelines must be updated to include improved screening and treatment of physical chronic conditions that may occur in patients with mental health conditions8,20. Regarding poorer treatment and control of mental health conditions and physical chronic diseases associated with having more NCDs, clinical guidelines could incorporate more intentional monitoring of patients’ adherence to medication and treatments by clinicians8,20. Also proposed in our previous work, current clinical guidelines are based on evidence from controlled trials for treating single NCDs8,20,48,49,50, and treatments may no longer be effective and even have adverse effects when applying single-disease guidelines to patients with multimorbidity8,20,51. Hence, clinical guidelines should be tailored towards an approach to multimorbidity of co-occurring mental illness and physical chronic conditions, whereby clinicians review the effectiveness and risks of combining the medications and different treatments for mental illness and physical chronic diseases7,8,20,48.
Healthcare systems in LMICs like China may need to implement policies that improve access to care from the primary care system for continual treatment after first diagnosis52,53,54,55. Policies that prioritize NCD combinations that include mental health conditions that are more prevalent or associated with poorer management and control need be considered, such as reducing costs of medicines and clinic visits56,57. It is worth noting that health-care delivery in China is hospital-centered and fragmented, with little coordination among health-care providers across different tiers of the system57,58. Strong primary health care, underpinned by multidisciplinary teams lead by general practitioner, is also crucial for the improved prevention and treatment of patients with multiple NCDs. Health care delivery need to shift away from the current vertical approach of treating single-disease models to one that emphasize on horizontal integration that aims to provide more effectively management for patients with multiple NCDs, including co-existing physical and mental NCDs. Overall, our study provides evidence on the impact of comorbid mental health condition on the management of physical NCDs in China. Further research is required to better understand the epidemiology of co-existing mental-physical NCDs and associated impacts on management of the conditions and associated costs and health outcomes in LMIC settings.
References
Mendenhall, E., Kohrt, B. A., Norris, S. A., Ndetei, D. & Prabhakaran, D. Non-communicable disease syndemics: poverty, depression, and diabetes among low-income populations. Lancet 389, 951–963 (2017).
Momen, N. C. et al. Association between mental disorders and subsequent medical conditions. N. Engl. J. Med. 382, 1721–1731 (2020).
Day, J. C. Population projections of the United States, by age, sex, race, and Hispanic origin: 1992 to 2050. (US Department of Commerce, Economics and Statistics Administration, Bureau …, 1992).
Zhao, Y. et al. Physical multimorbidity, health service use, and catastrophic health expenditure by socioeconomic groups in China: an analysis of population-based panel data. Lancet Glob. Health 8, e840–e849. https://doi.org/10.1016/S2214-109X(20)30127-3 (2020).
Lu, S., Oldenburg, B., Li, W., He, Y. & Reavley, N. Population-based surveys and interventions for mental health literacy in China during 1997–2018: a scoping review. BMC Psychiatry 19, 1–12 (2019).
Huang, Y. et al. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatry 6, 211–224 (2019).
Eulenburg, C. et al. Propensity scoring after multiple imputation in a retrospective study on adjuvant radiation therapy in lymph-node positive vulvar cancer. PLoS ONE 11, e0165705. https://doi.org/10.1371/journal.pone.0165705 (2016).
Sum, G. Patient centric perspectives on the public health burden of multimorbidity: Out of pockey expenditure, work productivity, healthcare utilisation, quality of life, and disease management and control. SSHSPH NUS (2020).
Noel, P. H., Frueh, B. C., Larme, A. C. & Pugh, J. A. Collaborative care needs and preferences of primary care patients with multimorbidity. Health Expect 8, 54–63. https://doi.org/10.1111/j.1369-7625.2004.00312.x (2005).
Noel, P. H. et al. The challenges of multimorbidity from the patient perspective. J Gen Intern Med 22(Suppl 3), 419–424. https://doi.org/10.1007/s11606-007-0308-z (2007).
Bayliss, E. A., Steiner, J. F., Fernald, D. H., Crane, L. A. & Main, D. S. Descriptions of barriers to self-care by persons with comorbid chronic diseases. Ann. Fam. Med. 1, 15–21. https://doi.org/10.1370/afm.4 (2003).
Piette, J. D. & Kerr, E. A. The impact of comorbid chronic conditions on diabetes care. Diabetes Care 29, 725–731 (2006).
Bair, M. J. et al. Barriers and facilitators to chronic pain self-management: a qualitative study of primary care patients with comorbid musculoskeletal pain and depression. Pain Med 10, 1280–1290. https://doi.org/10.1111/j.1526-4637.2009.00707.x (2009).
Wong, M. C. et al. Factors associated with multimorbidity and its link with poor blood pressure control among 223,286 hypertensive patients. Int. J. Cardiol. 177, 202–208. https://doi.org/10.1016/j.ijcard.2014.09.021 (2014).
Li, Y. T. et al. Medication adherence and blood pressure control among hypertensive patients with coexisting long-term conditions in primary care settings: a cross-sectional analysis. Medicine 95, e3572. https://doi.org/10.1097/md.0000000000003572 (2016).
Lagu, T. et al. The impact of concordant and discordant conditions on the quality of care for hyperlipidemia. J. Gen. Int. Med. 23, 1208–1213. https://doi.org/10.1007/s11606-008-0647-4 (2008).
Ricci-Cabello, I. et al. Impact of the prevalence of concordant and discordant conditions on the quality of diabetes care in family practices in England. Ann. Fam. Med. 13, 514–522. https://doi.org/10.1370/afm.1848 (2015).
Turner, B. J., Hollenbeak, C. S., Weiner, M., Ten Have, T. & Tang, S. S. Effect of unrelated comorbid conditions on hypertension management. Ann. Int. Med. 148, 578–586 (2008).
Magnan, E. M. et al. The impact of a patient’s concordant and discordant chronic conditions on diabetes care quality measures. J. Diabetes Comp. 29, 288–294. https://doi.org/10.1016/j.jdiacomp.2014.10.003 (2015).
Sum, G. et al. Patients with more comorbidities have better detection of chronic conditions, but poorer management and control: findings from six middle-income countries. BMC Public Health 20, 9. https://doi.org/10.1186/s12889-019-8112-3 (2020).
Sum, G. et al. Patients with more comorbidities have better detection of chronic conditions, but poorer management and control: findings from six middle-income countries. BMC Public Health 20, 1–26 (2020).
Palladino, R., Tayu Lee, J., Ashworth, M., Triassi, M. & Millett, C. Associations between multimorbidity, healthcare utilisation and health status: evidence from 16 European countries. Age Age. 45, 431–435. https://doi.org/10.1093/ageing/afw044 (2016).
Zhao, Y. et al. China health and retirement longitudinal study–2011–2012 national baseline users’ guide. Beijing: National School of Development, Peking University, 1–56 (2013).
Zhao, Y., Hu, Y., Smith, J. P., Strauss, J. & Yang, G. Cohort profile: the China health and retirement longitudinal study (CHARLS). Int. J. Epidemiol. 43, 61–68 (2014).
Luo, H. et al. Obesity and the onset of depressive symptoms among middle-aged and older adults in China: evidence from the CHARLS. BMC Public Health 18, 909 (2018).
Alwan, A. Global status report on noncommunicable diseases 2010. (World Health Organization, 2011).
Zhao, Y. et al. Prevalence, diagnosis, and management of diabetes mellitus among older Chinese: results from the China Health and Retirement Longitudinal Study. Int. J. Public Health 61, 347–356 (2016).
Adults, I. Chinese guideline for the management of dyslipidemia in adults. Zhonghua Xin Xue Guan Bing Za Zhi 44, 833–853 (2016).
Levey, A. S. et al. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am. J. Kidney Dis. 39, 1–2 (2002).
Liu, Y., Dijst, M., Faber, J., Geertman, S. & Cui, C. Healthy urban living: residential environment and health of older adults in Shanghai. Health Place 47, 80–89 (2017).
Zhang, Y. & Moran, A. E. Trends in the prevalence, awareness, treatment, and control of hypertension among young adults in the United States, 1999 to 2014. Hypertension 70, 736–742. https://doi.org/10.1161/hypertensionaha.117.09801 (2017).
Mirza, A. A. & Elmorsy, S. A. Diagnosis and Control of Hypertension as Indicators of the Level of Awareness Among Relatives of Medical Students in Saudi Arabia. High Blood Pressure Cardiovasc. Prevent. Off. J. Italian Soc. Hypertension 23, 123–132. https://doi.org/10.1007/s40292-016-0145-4 (2016).
Pasina, L. et al. Medication non-adherence among elderly patients newly discharged and receiving polypharmacy. Drugs Aging 31, 283–289 (2014).
Kafle, B., Khadka, B. & Tiwari, M. L. Prevalence of thyroid dysfunction among depression patients in a tertiary care centre. JNMA J. Nepal Med. Assoc. 58, 654 (2020).
Lala, V., Goyal, A., Bansal, P. & Minter, D. Liver function tests. StatPearls (2020).
McConaghy, J. R. & Oza, R. Outpatient diagnosis of acute chest pain in adults. Am. Fam. Phys. 87, 177–182 (2013).
Shima, A. et al. Relationship between outpatient visit frequency and hypertension control: a 9-year occupational cohort study. Hypertens. Res. 39, 376–381 (2016).
Chow, C. K. et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA 310, 959–968. https://doi.org/10.1001/jama.2013.184182 (2013).
Gellad, W. F., Grenard, J. L. & Marcum, Z. A. A Systematic Review of Barriers to Medication Adherence in the Elderly: Looking Beyond Cost and Regimen Complexity. Am. J. Geriatr. Pharmacother. 9, 11–23. https://doi.org/10.1016/j.amjopharm.2011.02.004 (2011).
Sum, G. et al. Multimorbidity and out-of-pocket expenditure on medicines: a systematic review. BMJ Glob Health 3, e000505. https://doi.org/10.1136/bmjgh-2017-000505 (2018).
Brown, M. T. & Bussell, J. K. Medication adherence: WHO cares?. Mayo Clin. Proc. 86, 304–314. https://doi.org/10.4065/mcp.2010.0575 (2011).
Chatterji, S. & Kowal, P. (Inter-university Consortium for Political and Social Research [distributor], 2013).
Kowal, P. et al. Data resource profile: the World Health Organization Study on global AGEing and adult health (SAGE). Int. J. Epidemiol. 41, 1639–1649. https://doi.org/10.1093/ije/dys210 (2012).
Vellakkal, S. et al. Are estimates of socioeconomic inequalities in chronic disease artefactually narrowed by self-reported measures of prevalence in low-income and middle-income countries? Findings from the WHO-SAGE survey. J. Epidemiol. Commun. Health 69, 218–225. https://doi.org/10.1136/jech-2014-204621 (2015).
Busby Grant, J., Bruce, C. P. & Batterham, P. J. Predictors of personal, perceived and self-stigma towards anxiety and depression. Epidemiol. Psychiatr. Sci. 25, 247–254. https://doi.org/10.1017/s2045796015000220 (2016).
Jones, A. R., Cook, T. M. & Wang, J. Rural-urban differences in stigma against depression and agreement with health professionals about treatment. J. Affect. Disord. 134, 145–150. https://doi.org/10.1016/j.jad.2011.05.013 (2011).
Barnett, K. et al. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet 380, 37–43. https://doi.org/10.1016/s0140-6736(12)60240-2 (2012).
Kovacevic, S. V. et al. Evaluation of drug-related problems in older polypharmacy primary care patients. J. Eval. Clin. Pract. 23, 860–865. https://doi.org/10.1111/jep.12737 (2017).
Feng, X. Q., Zhu, L. L. & Zhou, Q. Opioid analgesics-related pharmacokinetic drug interactions: from the perspectives of evidence based on randomized controlled trials and clinical risk management. J. Pain Res. 10, 1225–1239. https://doi.org/10.2147/jpr.s138698 (2017).
Vrdoljak, D. & Borovac, J. A. Medication in the elderly - considerations and therapy prescription guidelines. Acta Med. Acad. 44, 159–168. https://doi.org/10.5644/ama2006-124.142 (2015).
Stewart, D. et al. Guidance to manage inappropriate polypharmacy in older people: systematic review and future developments. Expert Opin. Drug Saf. 16, 203–213. https://doi.org/10.1080/14740338.2017.1265503 (2017).
Frieden, T. R. A framework for public health action: the health impact pyramid. Am. J. Public Health 100, 590–595 (2010).
Waibel, S., Vargas, I., Coderch, J. & Vázquez, M.-L. Relational continuity with primary and secondary care doctors: a qualitative study of perceptions of users of the Catalan national health system. BMC Health Serv. Res. 18, 257 (2018).
Wright, M. & Mainous, A. G. III. Can continuity of care in primary care be sustained in the modern health system?. Aust. J. Gen. Pract. 47, 667 (2018).
Guthrie, B. Continuity in UK general practice: a multilevel model of patient, doctor and practice factors associated with patients seeing their usual doctor. Fam. Pract. 19, 496–499 (2002).
Chen, H., Chen, Y. & Cui, B. The association of multimorbidity with healthcare expenditure among the elderly patients in Beijing China. Arch. Gerontol. Geriatr. 79, 32–38 (2018).
Sum, G. et al. Multimorbidity and out-of-pocket expenditure on medicines: a systematic review. BMJ global health 3, e000505 (2018).
Wang, X. et al. People-centred integrated care in urban China. Bull. World Health Organ. 96, 843 (2018).
Author information
Authors and Affiliations
Contributions
Z.Z.: data analysis and drafted the manuscript; GS: draft writing and editing; V.M.Q.: check result and provide assistance in data analysis; Y.Z.: provide assistance for data analysis; T.N.H.: provide suggestions on writing manuscript; B.O.: edit draft; J.T.L.: design, coordinate the study and edit the draft.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhang, Z., Sum, G., Qin, V.M. et al. Associations between mental health disorder and management of physical chronic conditions in China: a pooled cross-sectional analysis. Sci Rep 11, 5731 (2021). https://doi.org/10.1038/s41598-021-85126-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-85126-4
This article is cited by
-
A situational analysis of human resource and non-communicable diseases management for community health workers in Chengdu, China: a cross-sectional study
BMC Health Services Research (2023)
-
The impact of depression and physical multimorbidity on health-related quality of life in China: a national longitudinal quantile regression study
Scientific Reports (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.